Unlock your full potential by mastering the most common Exercise Physiology Principles interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Exercise Physiology Principles Interview
Q 1. Explain the concept of VO2 max and its significance in exercise prescription.
VO2 max, or maximal oxygen consumption, represents the maximum rate at which your body can utilize oxygen during intense exercise. It’s a crucial indicator of cardiorespiratory fitness, reflecting the efficiency of your heart, lungs, and muscles in delivering and using oxygen. A higher VO2 max signifies greater endurance capacity.
In exercise prescription, VO2 max helps determine training intensity. For example, training at 70-80% of your VO2 max promotes significant improvements in aerobic capacity. Knowing your VO2 max allows for personalized training plans, ensuring workouts are challenging enough to elicit adaptation but not so intense as to cause overtraining. Imagine a marathon runner: their high VO2 max enables them to sustain high-intensity running for extended periods. Conversely, someone with a lower VO2 max might need to start with lower-intensity training and gradually increase intensity to avoid injury and burnout.
Q 2. Describe the physiological responses to acute exercise.
Acute exercise elicits numerous physiological changes. Immediately, your heart rate and respiratory rate increase to meet the increased oxygen demand of working muscles. Blood pressure rises as blood is redirected from non-essential organs to the muscles. Your body temperature increases, and you begin to sweat to regulate temperature. Metabolic rate increases significantly, with a corresponding rise in energy expenditure. These changes reflect the body’s immediate response to the stress of physical activity. Think about sprinting – your heart pounds, you breathe heavily, you get warmer, and you feel your muscles working hard.
Furthermore, blood glucose levels increase initially to fuel working muscles, followed by mobilization of stored glycogen for prolonged activity. Lactate production increases with higher intensity exercise, reflecting the shift towards anaerobic metabolism. After exercise, the body gradually returns to homeostasis, although recovery time varies based on exercise intensity and duration.
Q 3. What are the key adaptations to endurance training?
Endurance training, such as running or cycling, brings about several key adaptations aimed at improving oxygen delivery and utilization. These include:
- Increased VO2 max: The body becomes more efficient at extracting and using oxygen.
- Increased capillary density in muscles: More blood vessels deliver oxygen and nutrients to muscle cells, improving their function.
- Increased mitochondrial density: Mitochondria are the powerhouses of cells, and more mitochondria mean increased capacity for aerobic ATP production.
- Improved cardiac output: The heart becomes stronger and more efficient at pumping blood, increasing the amount of oxygen delivered to muscles.
- Increased blood volume: A greater blood volume improves oxygen transport capacity.
- Increased fat oxidation: The body becomes more efficient at burning fat for fuel during prolonged exercise.
These adaptations work synergistically to enhance endurance performance. For instance, a runner who trains regularly will notice they can run longer distances at a faster pace, showcasing these adaptations in action.
Q 4. What are the key adaptations to strength training?
Strength training leads to significant adaptations primarily within the musculoskeletal system. Key changes include:
- Increased muscle fiber size (hypertrophy): Muscle fibers grow larger and stronger in response to the training stimulus.
- Increased muscle fiber recruitment: The nervous system becomes more efficient at activating more muscle fibers simultaneously, leading to greater force production.
- Increased bone density: Weight-bearing exercises stimulate bone growth, leading to stronger bones and reduced risk of osteoporosis.
- Increased tendon and ligament strength: Connective tissues surrounding the muscles and joints adapt to the increased forces they experience.
- Changes in muscle fiber type composition: While not a dramatic shift, some individuals may see a shift towards a more balanced ratio of fast-twitch and slow-twitch fibers, depending on their training.
These adaptations result in improved strength, power, and muscle mass. A weightlifter, for instance, will gain significant muscle mass and strength due to these physiological changes, allowing them to lift heavier weights.
Q 5. Explain the role of ATP, PCr, and glycogen in energy production during exercise.
ATP (adenosine triphosphate) is the primary energy currency of the body. PCr (phosphocreatine) serves as a rapid source of energy to regenerate ATP during high-intensity exercise. Glycogen, stored glucose in the muscles and liver, provides a longer-lasting energy source during prolonged exercise.
During exercise, ATP is broken down to release energy. PCr quickly donates a phosphate group to ADP (adenosine diphosphate) to reform ATP. However, PCr stores are limited, lasting only for a few seconds of intense activity. Once PCr is depleted, the body relies on the breakdown of glycogen (glycolysis) for ATP production. Glycolysis produces ATP relatively quickly but less efficiently than the PCr system, and also produces lactate as a byproduct.
Q 6. Describe the different energy systems and their contributions during various intensities of exercise.
The body uses three main energy systems, each contributing differently depending on exercise intensity and duration:
- ATP-PCr System (Phosphagen System): This system is dominant during short, high-intensity activities like sprinting or weightlifting. It’s extremely fast but has limited fuel reserves (ATP and PCr).
- Glycolytic System: This system becomes the primary source of ATP during moderately intense exercise lasting several minutes. It breaks down glycogen (and glucose) into pyruvate, producing ATP relatively quickly but less efficiently and creating lactate as a byproduct.
- Oxidative System (Aerobic System): This system is used for prolonged, low-to-moderate intensity exercise. It uses oxygen to completely break down carbohydrates and fats, producing large amounts of ATP but at a slower rate. This system supports activities like marathon running or long-distance cycling.
During a typical workout, all three systems are involved, although their contributions vary depending on the activity. A 100m sprint is primarily fueled by the ATP-PCr system, while a marathon relies heavily on the oxidative system.
Q 7. Explain the lactate threshold and its importance in exercise performance.
The lactate threshold (LT) is the exercise intensity at which blood lactate concentration begins to increase exponentially. It’s a critical indicator of endurance performance because it reflects the point at which the body can no longer efficiently clear lactate produced during exercise. Beyond the LT, fatigue sets in more rapidly due to lactate accumulation and its associated effects (e.g., muscle acidosis).
A higher lactate threshold indicates better endurance capacity. Athletes train to increase their LT, allowing them to sustain higher exercise intensities for longer periods without experiencing excessive fatigue. For example, a cyclist with a high LT can maintain a faster pace for a longer duration during a race compared to a cyclist with a lower LT. Training strategies to raise the LT often involve interval training and tempo runs that push athletes to and slightly beyond their current LT.
Q 8. What are the factors affecting exercise prescription?
Exercise prescription, the process of designing a safe and effective exercise program, is influenced by a multitude of factors. It’s not a one-size-fits-all approach; instead, it requires careful consideration of the individual’s unique characteristics and goals.
- Individual’s Goals: Are they aiming for weight loss, improved cardiovascular health, increased muscle strength, or a combination? Their goals dictate the intensity, duration, and type of exercise.
- Health Status: Pre-existing conditions like hypertension, diabetes, or arthritis significantly influence exercise prescription. Certain exercises might be contraindicated, requiring modifications or alternative activities.
- Fitness Level: Beginners require different programs compared to experienced athletes. A gradual progression is crucial to avoid injury and ensure adherence.
- Age: Age-related changes in musculoskeletal and cardiovascular systems necessitate adaptations to training programs. Older adults, for example, may benefit from lower-impact activities.
- Available Resources: Access to facilities, equipment, and qualified instructors all play a role. A program designed for a gym setting may not be feasible for someone without gym access.
- Personal Preferences: Enjoyment is key to adherence. Incorporating activities the individual likes increases the likelihood of long-term success. Forcing someone to run if they hate running is a recipe for failure.
- Environmental Factors: Weather, safety concerns, and accessibility of exercise locations impact program design.
For example, an exercise program for a sedentary 50-year-old with hypertension will be vastly different from a program for a young, healthy marathon runner. The former would emphasize low-impact aerobic activities, strength training, and gradual intensity increases, while the latter might focus on high-intensity interval training and endurance building.
Q 9. How do you assess an individual’s fitness level?
Assessing an individual’s fitness level involves a combination of methods, encompassing both subjective and objective measures. A comprehensive assessment provides a baseline to guide exercise prescription and monitor progress.
- Subjective Assessments: These involve questionnaires and interviews to gather information about the individual’s health history, lifestyle, activity levels, and exercise goals. Examples include the Physical Activity Readiness Questionnaire (PAR-Q) and medical history forms.
- Objective Assessments: These involve physical tests to measure various fitness components. Common tests include:
- Cardiovascular Fitness: Resting heart rate, blood pressure, and tests like the graded exercise test (GXT) or submaximal exercise tests (e.g., using a cycle ergometer or treadmill) to measure VO2 max (maximal oxygen consumption).
- Muscular Strength and Endurance: 1-repetition maximum (1RM) tests for major muscle groups, push-up tests, sit-up tests.
- Flexibility: Sit-and-reach test, shoulder flexibility tests.
- Body Composition: Measurements of body fat percentage, lean mass, etc., using methods discussed in the next question.
Integrating both subjective and objective assessments provides a holistic understanding of the individual’s fitness status. For example, a high resting heart rate coupled with a poor performance on a submaximal exercise test may indicate a need for a carefully designed cardiovascular training program.
Q 10. Describe the methods for measuring body composition.
Several methods exist to measure body composition, each with its advantages and limitations. Accurate measurement is crucial for assessing health risks and tracking progress in weight management programs.
- Hydrostatic Weighing (Underwater Weighing): This gold standard method measures body density by comparing weight on land to weight underwater. Archimedes’ principle is applied to calculate body fat percentage. However, it requires specialized equipment and trained personnel.
- Air Displacement Plethysmography (Bod Pod): This method uses air displacement to measure body volume, which is then used to calculate body density and body fat percentage. It’s less invasive than underwater weighing but still requires specialized equipment.
- Dual-Energy X-ray Absorptiometry (DEXA): This highly accurate technique uses low-dose X-rays to measure bone mineral density, lean mass, and fat mass. It’s more expensive than other methods but provides detailed information on body composition.
- Bioelectrical Impedance Analysis (BIA): This readily available method uses a small electrical current passed through the body to estimate body fat percentage based on resistance to the current. Hydration levels can affect accuracy, so it’s crucial for consistent hydration practices during testing.
- Skinfold Calipers: This relatively inexpensive method measures skinfold thickness at various body sites using calipers. Accuracy depends on the skill of the technician and may not be as precise as other methods.
The choice of method depends on factors such as cost, availability of equipment, and desired level of precision. For clinical settings, DEXA is often preferred for its accuracy, while BIA is more common in home-use fitness trackers due to ease of access.
Q 11. Explain the principles of training: overload, progression, specificity, individualization, reversibility.
The principles of training are fundamental to designing effective and safe exercise programs. They guide the progression and intensity of training to optimize results while minimizing injury risk.
- Overload: To improve fitness, the body must be progressively stressed beyond its current capacity. This can be achieved by increasing the intensity, duration, or frequency of exercise.
- Progression: Training loads should be gradually increased over time to avoid plateaus and injuries. This principle emphasizes a systematic and gradual increase in training volume and intensity.
- Specificity: Training adaptations are specific to the type of training performed. If one wants to improve running performance, running-specific training is necessary. This is often summarized as, “what you train is what you gain”.
- Individualization: Training programs must be tailored to the individual’s unique characteristics, goals, and limitations. There’s no one-size-fits-all approach to exercise.
- Reversibility: The positive adaptations from training are lost if training ceases or is significantly reduced. This highlights the importance of maintaining a consistent exercise routine to sustain gains.
Consider a weightlifter trying to increase their bench press. Overload might involve increasing the weight lifted, progression would involve gradually increasing the weight over weeks, specificity involves focusing on bench press exercises, individualization considers their current strength level and any injuries, and reversibility means that stopping training will lead to a decrease in their bench press strength.
Q 12. What are the common cardiovascular risk factors?
Cardiovascular risk factors are conditions and lifestyle choices that increase the likelihood of developing heart disease. Identifying and managing these factors is crucial for maintaining cardiovascular health.
- High Blood Pressure (Hypertension): Persistently elevated blood pressure strains the heart and blood vessels.
- High Blood Cholesterol: High levels of LDL (“bad”) cholesterol contribute to the buildup of plaque in arteries (atherosclerosis).
- Smoking: Damages blood vessels and increases the risk of blood clots.
- Diabetes: High blood sugar levels damage blood vessels and increase the risk of heart disease.
- Obesity: Excess body fat increases the risk of hypertension, high cholesterol, and diabetes.
- Physical Inactivity: Lack of regular exercise contributes to many cardiovascular risk factors.
- Family History: A family history of heart disease increases individual risk.
- Age: The risk of cardiovascular disease increases with age.
- Unhealthy Diet: A diet high in saturated fats, sodium, and processed foods increases risk.
It’s important to note that these risk factors often interact, increasing the overall risk. For example, a person with high blood pressure, high cholesterol, and a sedentary lifestyle has a significantly higher risk of cardiovascular disease than someone with none of these factors.
Q 13. How do you design an exercise program for a patient with hypertension?
Designing an exercise program for a patient with hypertension requires careful consideration to avoid sudden increases in blood pressure. The focus is on improving cardiovascular fitness gradually and safely.
- Initial Assessment: A thorough medical evaluation, including a stress test, is crucial before initiating any exercise program. This helps assess the patient’s current fitness level and identifies any limitations.
- Aerobic Exercise: Moderate-intensity aerobic activities like brisk walking, swimming, or cycling are recommended. Intensity should be gradually increased based on the patient’s tolerance and response.
- Resistance Training: Strength training is beneficial for improving blood pressure control but should be performed with lighter weights and higher repetitions to avoid excessive strain on the cardiovascular system.
- Frequency and Duration: Start with shorter sessions (e.g., 20-30 minutes) and gradually increase duration and frequency. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, spread across several days.
- Monitoring Blood Pressure: Regular monitoring of blood pressure before, during, and after exercise is essential to ensure safety and adjust the program as needed.
- Medication Considerations: The program should be coordinated with the patient’s physician, particularly concerning medication, especially those that can affect heart rate or blood pressure response to exercise.
For instance, an initial exercise program might involve 20 minutes of brisk walking three times per week, gradually increasing to 30-45 minutes as tolerated. Resistance training might start with 1-2 sets of 12-15 repetitions, using weights that allow for proper form and controlled movement. The program’s intensity should always be tailored to the individual’s response, ensuring that blood pressure does not rise excessively.
Q 14. How do you design an exercise program for a patient with diabetes?
Exercise is crucial for managing diabetes, improving insulin sensitivity, and reducing the risk of complications. However, specific considerations are necessary due to the potential for hypoglycemia (low blood sugar).
- Medical Evaluation: A thorough assessment by a physician is essential, especially to evaluate the patient’s current glycemic control and any other co-morbidities.
- Blood Glucose Monitoring: Regular monitoring of blood glucose levels before, during, and after exercise is critical to prevent hypoglycemia. Adjustments in timing, type, and intensity of exercise might be needed based on monitoring.
- Type of Exercise: A combination of aerobic and resistance training is recommended. Aerobic exercises improve insulin sensitivity, while resistance training increases muscle mass, which helps regulate blood sugar levels.
- Intensity and Duration: Moderate-intensity aerobic exercise is generally recommended. The duration and intensity should be tailored to the individual’s fitness level and glucose response. Starting with shorter durations and gradually increasing is key.
- Timing of Exercise: Exercise is often best performed after a meal or snack to prevent hypoglycemia. However, this depends on the individual’s blood glucose response to exercise and diet.
- Foot Care: Diabetic patients often have decreased sensation in their feet, so proper footwear and monitoring for blisters or injuries during exercise are crucial.
For example, a patient might start with 15-20 minutes of brisk walking after breakfast, carefully monitoring their blood glucose levels. As tolerance increases, the duration and intensity can be gradually adjusted. Incorporating strength training exercises 2-3 times per week can further improve glucose control and muscle strength.
Q 15. How do you design an exercise program for a patient with obesity?
Designing an exercise program for an obese patient requires a holistic approach, prioritizing safety and gradual progression. We start with a thorough assessment, including medical history, body composition analysis, and a functional movement screen to identify any limitations. The program needs to be individualized, considering factors like age, comorbidities, and current fitness level.
The initial phase focuses on building a foundation of aerobic fitness. Low-impact activities like walking, cycling, or water aerobics are ideal, starting with short durations and gradually increasing intensity and duration. Strength training is crucial for building muscle mass, which boosts metabolism and improves functional capacity. We use bodyweight exercises initially, progressing to resistance training with light weights or resistance bands.
Flexibility and balance exercises are also incorporated to improve range of motion and reduce the risk of injury. The entire program should be enjoyable and sustainable to encourage long-term adherence. For example, a patient might start with 15 minutes of walking three times a week, gradually increasing to 30-45 minutes, five times a week. We might start with two sets of 10 repetitions of bodyweight squats and progress to using dumbbells. Regular check-ins are vital to monitor progress, make adjustments, and provide support.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the role of exercise in weight management.
Exercise plays a multifaceted role in weight management. It directly burns calories, creating a calorie deficit necessary for weight loss. But its impact extends beyond simple calorie expenditure. Exercise increases resting metabolic rate (RMR), meaning your body burns more calories even at rest. It also helps build muscle mass, which further boosts metabolism.
Moreover, exercise improves insulin sensitivity, helping your body use glucose more effectively and reducing fat storage. It also aids in appetite regulation, potentially reducing cravings and promoting feelings of satiety. Consider a scenario where someone combines a reduced-calorie diet with regular exercise: the exercise will not only contribute to direct calorie burning but also enhance the body’s metabolic efficiency, making weight loss more sustainable and less reliant solely on dietary restriction.
Q 17. What are the benefits of exercise for mental health?
The benefits of exercise for mental health are substantial and well-documented. Physical activity stimulates the release of endorphins, natural mood elevators that reduce stress, anxiety, and depression. It improves sleep quality, which directly impacts mood and cognitive function. Exercise also enhances self-esteem and body image, contributing to overall psychological well-being.
Regular exercise can be as effective as some forms of therapy in managing mild to moderate depression and anxiety. For instance, a patient experiencing anxiety might find that a daily 30-minute walk helps to reduce their symptoms more effectively than medication alone. The social interaction inherent in group exercise classes can also combat feelings of loneliness and isolation, promoting a sense of community and support.
Q 18. How do you assess exercise capacity in a clinical setting?
Assessing exercise capacity in a clinical setting involves a combination of methods tailored to the individual’s condition. A thorough medical history and physical examination are crucial to identify any potential limitations or contraindications. Common tests include:
- Graded Exercise Test (GXT): This involves gradually increasing the intensity of exercise on a treadmill or cycle ergometer while monitoring heart rate, blood pressure, and ECG. It determines the individual’s peak oxygen uptake (VO2 max), a measure of cardiovascular fitness.
- 6-Minute Walk Test (6MWT): A simpler, less-resource-intensive test that measures the distance covered in six minutes. It is particularly useful for individuals with limited mobility.
- Submaximal Exercise Tests: These tests estimate VO2 max using less intensive exercise protocols, suitable for individuals unable to tolerate maximal exertion. Examples include the YMCA cycle ergometer test or the Rockport walk test.
The choice of test depends on the patient’s health status and available resources. The results help determine an appropriate exercise intensity and prescribe a safe and effective exercise program.
Q 19. What are the safety considerations when prescribing exercise?
Safety considerations are paramount when prescribing exercise. A thorough medical history is crucial to identify any pre-existing conditions that may impact exercise tolerance. Patients with cardiovascular disease, respiratory problems, or musculoskeletal issues require careful monitoring and modified exercise programs.
Environmental factors also play a role. Exercise should be performed in a safe environment, avoiding extreme temperatures and ensuring proper hydration. Individuals should be educated about recognizing signs and symptoms of exertion and when to stop exercising. Proper warm-up and cool-down periods are essential to prepare the body for exercise and prevent injury. The exercise prescription must always consider individual limitations and risks to minimize potential harm.
Q 20. How do you monitor and evaluate the effectiveness of an exercise program?
Monitoring and evaluating the effectiveness of an exercise program involves regular assessments of both physiological and subjective measures. Physiological measures include tracking heart rate, blood pressure, body composition (e.g., body mass index, waist circumference), and fitness levels (e.g., VO2 max, strength, flexibility).
Subjective measures involve assessing the patient’s perceived exertion, mood, and adherence to the program. These can be collected through questionnaires, self-monitoring logs, or regular discussions. Progress is reviewed regularly, usually every 4-8 weeks, allowing for adjustments to intensity, duration, or type of exercise. For instance, if a patient’s weight loss plateaus, we might adjust the program by increasing the intensity or duration of exercise or modifying the dietary plan. Consistent monitoring ensures the program remains effective, safe, and enjoyable, leading to better adherence and long-term success.
Q 21. Describe the different types of muscle contractions.
Muscle contractions are categorized based on their length and tension changes. There are three main types:
- Isometric Contraction: Muscle tension increases, but the muscle length remains the same. Think of holding a weight in a static position—the muscle is working, but not shortening or lengthening. Example: A plank.
- Isotonic Contraction: Muscle tension remains relatively constant, but the muscle length changes. This is further divided into:
- Concentric Contraction: Muscle shortens while generating force. Example: Lifting a weight during a bicep curl.
- Eccentric Contraction: Muscle lengthens while generating force. Example: Lowering a weight during a bicep curl.
- Isokinetic Contraction: Muscle contracts at a constant speed, regardless of the force applied. This type of contraction typically requires specialized equipment. Example: Using an isokinetic dynamometer.
Understanding these different types of contractions is critical for designing effective exercise programs that target specific muscle adaptations and functional improvements.
Q 22. Explain the concept of muscle hypertrophy and hyperplasia.
Muscle growth, or skeletal muscle mass increase, happens through two primary mechanisms: hypertrophy and hyperplasia. Hypertrophy refers to an increase in the size of individual muscle fibers (cells), while hyperplasia refers to an increase in the number of muscle fibers.
Think of it like this: hypertrophy is like inflating a balloon (making the existing muscle fibers larger), while hyperplasia is like getting more balloons (increasing the number of muscle fibers). Most muscle growth in adult humans is primarily due to hypertrophy. Hyperplasia, while possible, plays a less significant role and is more often seen in animal models and certain specific situations.
In practical terms, resistance training, where muscles are repeatedly challenged against a significant load, primarily stimulates hypertrophy. The mechanical tension, metabolic stress, and muscle damage caused by this type of exercise trigger cellular signaling pathways that lead to protein synthesis, resulting in larger muscle fibers. While the exact extent to which hyperplasia contributes is debated, evidence suggests that it may play a more significant role in certain individuals or specific training protocols, such as those involving very high volumes of training.
Q 23. Describe the role of hormones in exercise adaptation.
Hormones play a crucial role in mediating the body’s response to exercise, influencing adaptations such as muscle growth, strength gains, and improvements in cardiovascular function. Key hormones involved include:
- Testosterone: Crucial for muscle protein synthesis and hypertrophy, particularly in men. Exercise, especially resistance training, stimulates testosterone production.
- Growth Hormone (GH): Promotes muscle growth, protein synthesis, and fat breakdown. Exercise, particularly high-intensity interval training (HIIT) and resistance training, stimulates GH release.
- Insulin-like Growth Factor 1 (IGF-1): Mediates many of the effects of GH, including promoting muscle protein synthesis and hypertrophy.
- Cortisol: A catabolic hormone that breaks down muscle protein. While elevated cortisol can be detrimental, moderate levels can also play a role in tissue repair and adaptation. Overtraining or excessive stress can lead to chronically elevated cortisol, hindering muscle growth and recovery.
- Insulin: Essential for glucose uptake into muscle cells, fueling muscle growth and recovery. Exercise can temporarily increase insulin sensitivity.
The interplay of these hormones during and after exercise determines the extent and nature of the adaptations. For example, well-balanced training with adequate rest and nutrition will lead to a favourable hormonal environment (high testosterone, GH, IGF-1, and controlled cortisol), while overtraining leads to a negative hormonal profile (low testosterone, high cortisol).
Q 24. What are the common biomechanical considerations in exercise programming?
Biomechanical considerations are vital for designing safe and effective exercise programs. Ignoring them can lead to injuries. Key factors include:
- Joint Alignment: Exercises should be performed with proper form to minimize stress on joints. For instance, incorrect squat form can stress the knees. Proper coaching is critical.
- Range of Motion (ROM): Exercises should be performed through a full, controlled ROM to maximize muscle activation and improve flexibility. However, it is important not to force it beyond a comfortable range.
- Force Production: The amount of force generated during exercise influences muscle activation and adaptation. Progressive overload (gradually increasing weight or resistance) is crucial for continuous improvement. The application of this principle needs to be nuanced, considering the individual’s strength level.
- Muscle Activation: Different exercises activate different muscles. A well-designed program targets all major muscle groups, ensuring balanced development. This often implies a combination of compound and isolation exercises.
- Muscle Balance: Strength imbalances between opposing muscle groups (e.g., hamstrings and quadriceps) can lead to injuries. A balanced program trains opposing muscle groups equally.
For example, a poorly designed program neglecting proper joint alignment while performing deadlifts may increase the risk of lower back injury. A well-designed program will teach and emphasize correct form and incorporate exercises to support postural stability.
Q 25. Explain the concept of overtraining and how to avoid it.
Overtraining is a state of excessive training that leads to impaired performance, fatigue, and other negative health consequences. It’s a critical issue for athletes and fitness enthusiasts alike.
Signs of overtraining include:
- Decreased performance despite increased training volume
- Persistent fatigue and muscle soreness
- Loss of motivation and enthusiasm for exercise
- Increased resting heart rate
- Disturbed sleep
- Irritability and mood changes
Preventing overtraining requires a multi-pronged approach:
- Progressive Overload: Gradually increase training volume and intensity. Avoid sudden or significant increases in training.
- Adequate Rest and Recovery: Ensure sufficient sleep, nutrition, and rest days. Active recovery can also be beneficial.
- Periodization: Plan training cycles with periods of high intensity followed by periods of reduced intensity. This allows for optimal adaptation without leading to overtraining.
- Listen to Your Body: Pay attention to signs of fatigue and reduce training volume or intensity if needed. Don’t push yourself beyond your limits.
- Individualization: Training programs should be tailored to an individual’s fitness level, goals, and recovery capacity.
A coach plays a crucial role by closely monitoring the athlete’s training progress and response to training. Careful observation of performance, feedback, and any signs of overtraining are essential.
Q 26. Describe the importance of proper nutrition in exercise performance and recovery.
Proper nutrition is fundamental to optimal exercise performance and recovery. It provides the fuel for exercise, supports muscle growth and repair, and boosts the immune system.
Before exercise: Consume a carbohydrate-rich meal or snack 1-3 hours before exercise to provide energy. This is critical to replenish glycogen stores.
During exercise (for longer sessions): Consume carbohydrates and electrolytes to maintain energy levels and hydration.
After exercise: Consume a meal or snack containing protein and carbohydrates within 1-2 hours after exercise to promote muscle protein synthesis and replenish glycogen stores. The optimal protein intake depends on the individual’s training volume and goals.
Macronutrients:
- Carbohydrates: The primary energy source during exercise.
- Protein: Essential for muscle growth, repair, and recovery.
- Fats: Provide energy and support hormone production.
Micronutrients: Vitamins and minerals are also crucial for optimal function.
A well-planned nutrition strategy is as critical as a well-structured training program. An individual’s dietary needs vary greatly depending on factors such as activity level, training goals, body composition, and individual preferences.
Q 27. How do you handle a client who is experiencing exercise-induced symptoms?
When a client experiences exercise-induced symptoms, a systematic approach is crucial:
- Assess the Situation: Determine the nature, severity, and location of the symptoms. Is it chest pain, dizziness, shortness of breath, or muscle cramps? The location, intensity and duration are important details.
- Immediate Action: If the symptoms are severe or life-threatening (e.g., chest pain, loss of consciousness), call emergency medical services immediately.
- Stop the Exercise: Have the client stop exercising immediately.
- Monitor Vital Signs: If appropriate, check the client’s heart rate, blood pressure, and respiration rate.
- Provide First Aid: If appropriate, provide basic first aid, such as administering water or ice for muscle cramps.
- Refer to Medical Professional: Refer the client to a physician or other appropriate healthcare professional for evaluation and treatment.
- Document the Incident: Document the incident, including the symptoms, actions taken, and any referrals made.
Prevention is key. Thorough health screenings before beginning an exercise program and continuous monitoring are necessary. Knowing the client’s medical history and any pre-existing conditions is crucial. Educating clients on the importance of listening to their bodies and recognizing early warning signs of problems is essential.
Q 28. How do you adapt exercise programs to accommodate for different populations and needs?
Adapting exercise programs for different populations and needs involves careful consideration of individual factors. This could involve:
- Age: Older adults may require modifications to account for decreased bone density, joint mobility, and cardiovascular fitness. Exercise programs should prioritize functional fitness, balance and incorporate lower impact activities.
- Medical Conditions: Individuals with chronic diseases (e.g., diabetes, heart disease) require programs tailored to their specific condition and limitations. This may involve exercise mode adaptations, intensity modifications or collaboration with other healthcare professionals.
- Physical Limitations: Individuals with disabilities or injuries may require modified exercises or assistive devices to ensure safe and effective participation.
- Fitness Level: Programs should start at a level appropriate to the client’s fitness level and progress gradually to avoid injury and maintain motivation.
- Goals: Programs should be designed to align with the client’s individual goals, whether it’s weight loss, strength gain, improved cardiovascular health, or stress reduction.
- Preferences: Incorporate the client’s personal preferences to enhance adherence. Some people prefer group classes, while others prefer individual training. Exercise selection can be catered to an individual’s preferences to maximize enjoyment.
For example, an older adult with osteoarthritis might benefit from low-impact exercises like swimming or cycling, whereas a younger individual training for a marathon might require a high-intensity running program. A client with knee pain might need modifications to exercises that put significant stress on the knee joint.
Key Topics to Learn for Exercise Physiology Principles Interview
- Energy Systems: Understand the interplay of ATP-PCr, glycolytic, and oxidative systems during exercise of varying intensities and durations. Consider how these systems influence training program design.
- Cardiorespiratory Physiology: Master concepts like VO2 max, lactate threshold, and their practical applications in assessing fitness and prescribing exercise. Be prepared to discuss the physiological responses to aerobic and anaerobic training.
- Muscle Physiology: Explore muscle fiber types, their metabolic characteristics, and how they adapt to different training stimuli. Discuss the principles of muscle hypertrophy and strength gains.
- Exercise Prescription: Demonstrate a strong understanding of the principles of exercise prescription, including FITT (Frequency, Intensity, Time, Type) and its application across various populations and fitness goals. Be ready to discuss adaptations to training and detraining.
- Bioenergetics: Understand the metabolic processes involved in energy production and utilization during exercise. Be able to explain how nutritional factors influence performance.
- Thermoregulation: Explain the physiological mechanisms involved in regulating body temperature during exercise and the implications for exercise in different environmental conditions.
- Assessment and Testing: Be familiar with various methods used to assess cardiorespiratory fitness, muscular strength and endurance, body composition, and flexibility. Understand the limitations and interpretations of these assessments.
- Exercise and Health: Discuss the role of exercise in preventing and managing chronic diseases such as cardiovascular disease, type 2 diabetes, and obesity. Be prepared to discuss the evidence-based benefits of exercise.
Next Steps
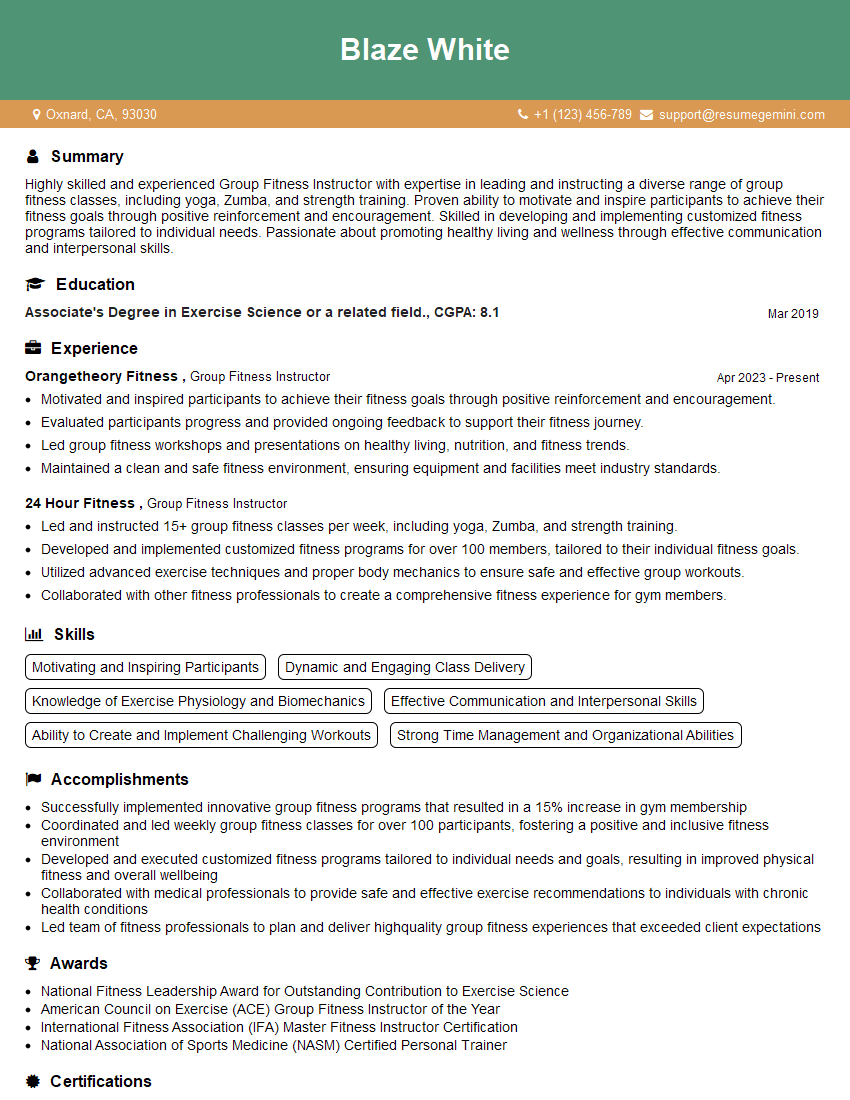
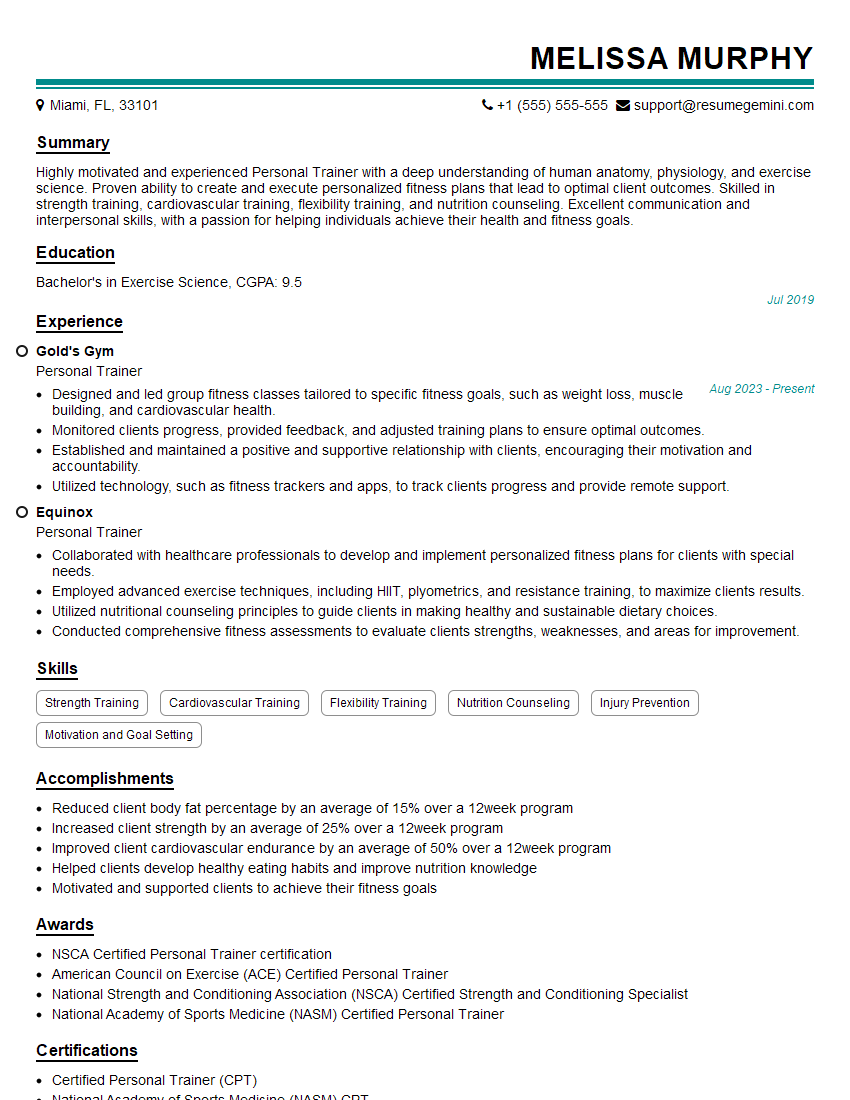
Mastering Exercise Physiology Principles is crucial for career advancement in the fitness and health fields. A strong understanding of these concepts will differentiate you from other candidates and demonstrate your expertise. To maximize your job prospects, create a compelling and ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume tailored to the specific demands of Exercise Physiology positions. They provide examples of resumes specifically designed for Exercise Physiology Principles roles to help guide your process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.