Cracking a skill-specific interview, like one for Exercise Prescription for Chronic Conditions, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Exercise Prescription for Chronic Conditions Interview
Q 1. Explain the principles of exercise prescription for individuals with cardiovascular disease.
Exercise prescription for individuals with cardiovascular disease (CVD) centers on improving cardiovascular fitness while minimizing risk. The goal is to increase the heart’s efficiency, strengthen the heart muscle, and improve blood flow. We use a phased approach, starting with low-intensity activities and gradually increasing intensity and duration as tolerated.
- Phase 1: Inpatient Rehabilitation: This phase focuses on bed mobility, range of motion exercises, and low-intensity activities such as chair sits and stands. It’s crucial to monitor vital signs closely.
- Phase 2: Outpatient Cardiac Rehabilitation: This phase involves supervised exercise training, typically including aerobic exercise (like walking or cycling), resistance training, and flexibility exercises. Intensity is carefully monitored using methods like the Borg Scale or heart rate monitoring.
- Phase 3: Community-Based Exercise: Once patients are stable, they transition to maintaining their fitness through self-directed exercise programs. Continuing to monitor progress is essential.
Key Principles:
- Individualization: Programs must be tailored to the patient’s specific condition, functional capacity, and risk factors.
- Gradual Progression: Intensity, duration, and frequency are increased gradually to avoid overexertion and potential complications.
- Monitoring: Regular monitoring of vital signs, symptoms, and perceived exertion is critical to ensure safety and effectiveness.
- Risk Stratification: Patients are categorized based on risk levels to guide exercise prescription and safety precautions.
For example, a patient post-myocardial infarction might start with short, low-intensity walks, gradually increasing the duration and intensity over weeks and months, under the supervision of a cardiac rehabilitation team.
Q 2. Describe the appropriate exercise intensity, duration, and frequency for patients with type 2 diabetes.
Exercise prescription for type 2 diabetes aims to improve insulin sensitivity, manage blood glucose levels, and reduce cardiovascular risk. The focus is on both aerobic and resistance training.
Intensity: Moderate intensity, generally 50-70% of maximum heart rate (MHR) or perceived exertion (Borg Scale 12-14), is recommended for aerobic exercise. Resistance training should be performed at a level that allows for 10-15 repetitions with moderate exertion.
Duration: At least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week is recommended. Resistance training should be performed at least two days per week.
Frequency: Most days of the week are ideal for aerobic exercise, while resistance training should be performed at least two days per week, with rest days in between.
Example: A patient with type 2 diabetes might engage in 30 minutes of brisk walking most days of the week, along with two days of resistance training using bodyweight or light weights.
Important Considerations: Blood glucose monitoring before, during, and after exercise is crucial. Proper nutrition and medication management are essential components of the overall diabetes management plan. Exercise should be tailored to the individual’s current fitness level and any co-morbidities.
Q 3. What are the contraindications and precautions for exercise in individuals with hypertension?
Exercise is generally beneficial for managing hypertension, but there are contraindications and precautions to consider.
Absolute Contraindications: These are situations where exercise should be avoided altogether, such as an uncontrolled hypertensive crisis (systolic blood pressure consistently over 200 mmHg or diastolic over 120 mmHg), acute myocardial infarction, severe aortic stenosis, or unstable angina.
Relative Contraindications: These require careful monitoring and possibly modification of the exercise program. They include severe left ventricular hypertrophy, uncontrolled arrhythmias, severe orthostatic hypotension, and recent stroke or transient ischemic attack (TIA).
Precautions:
- Monitoring Blood Pressure: Regular blood pressure monitoring is essential, both before and after exercise sessions.
- Gradual Progression: Intensity should be gradually increased to avoid sudden blood pressure spikes.
- Medication Management: Patients should be advised to take their medications as prescribed.
- Avoiding Valsalva Maneuver: Patients should be instructed on proper breathing techniques during exercise to avoid this maneuver, which can dramatically increase blood pressure.
- Hydration: Adequate hydration is important to maintain blood volume and prevent hypotension.
For instance, a patient with well-controlled hypertension might start with low-intensity aerobic exercise and gradually increase intensity, with careful monitoring of their blood pressure response. If blood pressure significantly rises during exercise, the intensity needs to be lowered or the session stopped.
Q 4. How would you modify an exercise program for a patient with osteoarthritis?
Modifying an exercise program for a patient with osteoarthritis (OA) requires careful consideration of joint pain and limitations. The focus should be on maintaining joint mobility, strengthening surrounding muscles, and improving overall fitness without exacerbating joint pain.
Modifications:
- Low-Impact Activities: Prioritize low-impact exercises such as walking, cycling, swimming, or water aerobics, which minimize stress on affected joints.
- Range of Motion Exercises: Regular range of motion exercises are crucial to maintain joint flexibility and reduce stiffness.
- Strengthening Exercises: Focus on strengthening muscles surrounding the affected joints to provide support and stability. Use lighter weights or resistance bands to avoid excessive stress on the joints.
- Proper Technique: Ensure correct exercise technique is used to avoid further joint damage.
- Pain Management: Incorporate strategies for pain management, such as ice or heat therapy, medication, and rest.
- Avoid High-Impact Activities: Activities that put significant stress on the affected joints, such as running or jumping, should be avoided.
Example: A patient with OA in the knee might benefit from a program incorporating low-impact exercises like stationary cycling, aquatic exercises, and strengthening exercises for the quadriceps and hamstrings using light weights or resistance bands. The program should be tailored to their specific pain levels and functional capabilities.
Q 5. Discuss the role of exercise in managing chronic obstructive pulmonary disease (COPD).
Exercise plays a vital role in managing chronic obstructive pulmonary disease (COPD). It helps improve lung function, increase exercise tolerance, and enhance quality of life. The focus is on improving respiratory muscle strength and endurance, as well as overall cardiovascular fitness.
Exercise Prescription:
- Pursed-Lip Breathing: Teach pursed-lip breathing techniques to control breathing and improve oxygenation.
- Diaphragmatic Breathing: Encourage diaphragmatic breathing to optimize lung capacity and reduce dyspnea (shortness of breath).
- Aerobic Exercise: Incorporate low-to-moderate intensity aerobic exercise, such as walking, cycling, or swimming. Intensity should be adjusted based on the patient’s tolerance and oxygen saturation levels.
- Strength Training: Incorporate resistance training to improve muscle strength and endurance, which assists with breathing and daily activities.
- Pulmonary Rehabilitation: A comprehensive pulmonary rehabilitation program involving exercise training, education, and psychosocial support is highly beneficial for managing COPD.
Monitoring: Oxygen saturation levels should be monitored during exercise to ensure that the patient is not overexerting themselves. Listen carefully to the patient’s symptoms and adjust the exercise intensity accordingly.
Example: A patient with COPD might start with short intervals of walking, interspersed with rest periods, gradually increasing the duration and intensity of the walks over time. Incorporating pursed-lip breathing techniques throughout the exercise session can help improve breathing efficiency.
Q 6. Explain how you would assess a patient’s readiness for exercise before starting a program.
Assessing a patient’s readiness for exercise before starting a program involves a thorough evaluation of their physical and medical history. This ensures exercise is safe and effective. The process involves several steps:
- Medical History: Obtain a detailed medical history, including current conditions, medications, allergies, and prior surgeries. Look for any contraindications to exercise.
- Physical Examination: Perform a physical examination to assess the patient’s overall health, including cardiovascular and musculoskeletal systems. Check for any limitations or risk factors.
- Risk Stratification: Categorize the patient based on their risk level using validated risk stratification tools. This helps determine appropriate exercise intensity and type.
- Functional Capacity Testing: Assess the patient’s functional capacity through tests such as a 6-minute walk test, a graded exercise test, or other relevant assessments depending on the condition. This determines the starting point of their exercise program.
- Symptom Assessment: Assess the patient’s current symptoms and how they are impacted by physical activity. This informs the choice of exercise and the intensity levels.
- Patient Education and Goals: Educate the patient about the importance of exercise, potential benefits, and risks. Collaborate to set realistic and achievable goals. Their compliance is crucial to success.
For example, before starting an exercise program for a patient with heart failure, a graded exercise test would be performed to assess their functional capacity and guide exercise prescription. This ensures their safety and determines the intensity and type of exercise to start with.
Q 7. What are the common signs and symptoms of exercise intolerance, and how would you respond?
Exercise intolerance manifests in various ways. Recognizing these signs is crucial to prevent complications.
Common Signs and Symptoms:
- Chest pain or discomfort: This can indicate cardiac problems and requires immediate cessation of exercise.
- Shortness of breath (dyspnea): Excessive breathlessness might signal respiratory issues or cardiovascular problems.
- Dizziness or lightheadedness: These could indicate orthostatic hypotension or other cardiovascular issues.
- Nausea or vomiting: These could be related to overexertion or other medical conditions.
- Muscle cramps or pain: Severe or persistent muscle pain might require rest or modification of the exercise.
- Excessive fatigue: Unusual or severe fatigue is a cause for concern.
- Changes in heart rate or rhythm: Abnormally high or low heart rate, or irregular rhythms, warrant immediate attention.
Response to Exercise Intolerance:
- Stop the exercise immediately: If any of these symptoms occur, immediately stop the exercise.
- Assess the situation: Monitor vital signs, such as heart rate and blood pressure.
- Seek medical attention if necessary: If symptoms are severe or persistent, contact emergency medical services or a healthcare professional.
- Modify exercise program as needed: After evaluation, adjust the exercise program based on the patient’s tolerance and any identified underlying issues. This might involve reducing intensity, duration, or frequency.
For example, if a patient experiences chest pain during exercise, the exercise must be stopped immediately. Vital signs should be assessed, and if the pain persists, they should seek medical attention. Their exercise program would likely need to be modified to a lower intensity level.
Q 8. Describe the process of developing an individualized exercise program for a patient with multiple chronic conditions.
Developing an individualized exercise program for a patient with multiple chronic conditions is a complex process requiring a holistic approach. It’s not a one-size-fits-all solution; we need to consider the interplay of each condition and the patient’s overall functional capacity.
The process typically involves these steps:
- Comprehensive Assessment: This includes a thorough medical history review, assessment of current functional abilities (e.g., walking distance, ability to perform ADLs), and identification of any limitations imposed by their conditions. This might involve reviewing medical records, conducting physical exams, and utilizing validated assessment tools. For example, I might use the Berg Balance Scale for assessing fall risk in a patient with Parkinson’s disease and osteoarthritis.
- Goal Setting: Collaboratively establish realistic, measurable, achievable, relevant, and time-bound (SMART) goals with the patient. These goals might focus on improving strength, endurance, balance, flexibility, or reducing pain. For instance, a goal might be to increase walking distance from 50 meters to 100 meters within 8 weeks.
- Exercise Prescription: Based on the assessment and goals, I carefully select appropriate exercise modalities, intensity, frequency, and duration. This may involve a combination of aerobic exercise (e.g., walking, cycling), resistance training (e.g., using weights or resistance bands), flexibility exercises (e.g., stretching, yoga), and balance training (e.g., tai chi). The intensity and type of exercise are tailored to the patient’s capabilities and limitations. For example, a patient with heart failure might start with low-intensity interval training, gradually increasing the intensity over time.
- Monitoring and Modification: Regular monitoring of the patient’s progress is crucial. This involves tracking their response to the exercise program, adjusting the program as needed based on their feedback and progress, and addressing any adverse effects. Frequent communication and feedback loops with the patient and their healthcare providers are essential for effective program adjustment.
- Education and Support: Patient education is vital to ensure adherence and long-term success. This includes instruction on proper exercise techniques, the importance of consistency, and strategies to overcome barriers to exercise. Providing support and encouragement is essential, fostering a positive and motivating environment for the patient.
Example: A patient with diabetes, hypertension, and osteoarthritis might benefit from a program combining low-impact aerobic exercise (water aerobics), gentle resistance training (using light weights), and range-of-motion exercises for the joints. The program’s intensity would be carefully monitored to avoid exacerbating any condition.
Q 9. How would you adapt exercise programming for patients with neurological conditions (e.g., stroke, multiple sclerosis)?
Adapting exercise programming for patients with neurological conditions like stroke or multiple sclerosis requires a highly individualized and cautious approach. Safety and functional improvement are paramount.
Key Considerations:
- Severity and Stage of the Condition: The program must consider the patient’s specific deficits and limitations. For example, a patient recovering from a stroke might have hemiparesis (weakness on one side of the body), requiring exercises to improve strength and coordination on the affected side. A patient with MS might experience fatigue and balance problems, necessitating modifications to exercise intensity and duration.
- Cognitive Impairment: Patients with neurological conditions may have cognitive deficits that affect their ability to understand and follow instructions. Clear, concise, and simple instructions, along with visual aids or demonstrations, are necessary. Regular feedback and reinforcement are also crucial.
- Spasticity and Muscle Weakness: Exercises should address muscle imbalances and spasticity (increased muscle tone). Stretching exercises, strengthening exercises for weak muscles, and specific techniques like neurodevelopmental treatment (NDT) may be incorporated.
- Balance and Coordination: Impaired balance and coordination increase fall risk. Exercises focusing on improving balance, posture, and coordination, such as tai chi or balance board exercises, are vital. The environment should be safe and supportive, and assistive devices (e.g., canes, walkers) might be used.
- Fatigue Management: Fatigue is a common symptom in neurological conditions. The exercise program should avoid overexertion and incorporate rest periods as needed. Energy conservation techniques might also be taught.
Example: A patient post-stroke might benefit from a program including task-specific training (e.g., practicing walking and reaching for objects), strengthening exercises for the affected limb using resistance bands, and balance training using a wobble board. The program’s intensity would be carefully monitored to avoid fatigue or further injury.
Q 10. What are the benefits and risks of resistance training for individuals with osteoporosis?
Resistance training offers significant benefits for individuals with osteoporosis, but it also carries some risks that must be carefully managed.
Benefits:
- Increased Bone Density: Weight-bearing and resistance exercises stimulate bone remodeling, leading to increased bone mineral density and reduced fracture risk. This is particularly important in preventing osteoporotic fractures.
- Improved Muscle Strength and Balance: Stronger muscles improve functional abilities, enhancing daily activities and reducing fall risk—a major concern in osteoporosis.
- Reduced Fall Risk: Improved strength and balance directly translate to fewer falls, thus reducing the risk of fractures.
- Improved Posture: Resistance training can help strengthen postural muscles, improving posture and reducing back pain.
Risks:
- Fractures: While resistance training strengthens bones, improper technique or excessive loading can increase fracture risk. This risk can be mitigated through careful exercise selection, proper form, and gradual progression of intensity.
- Muscle Strains or Sprains: Overexertion can lead to muscle injuries. It’s essential to begin with lighter weights and gradually increase the load as strength improves.
- Vertebral Fractures: Certain exercises, such as heavy lifting, may increase the risk of vertebral fractures. Careful selection of exercises and avoiding high-impact activities are important.
Recommendations:
- Weight-bearing exercises: Walking, jogging, stair climbing
- Resistance exercises: Using resistance bands, light weights, body weight exercises (squats, lunges)
- Focus on proper form and technique: To minimize injury risk
- Gradual progression: Starting with low weight and repetitions, slowly increasing as tolerated
- Avoid high-impact activities: Running, jumping
A healthcare professional should always supervise resistance training programs for individuals with osteoporosis.
Q 11. Explain the importance of monitoring vital signs during exercise.
Monitoring vital signs during exercise is crucial for ensuring patient safety and effectively managing chronic conditions. Vital signs provide valuable insights into the body’s response to physical stress.
Key Vital Signs to Monitor:
- Heart Rate (HR): Monitors cardiovascular response. Significant increases or irregularities can indicate potential problems.
- Blood Pressure (BP): Tracks cardiovascular strain. Excessive increases in systolic or diastolic pressure can be alarming.
- Respiratory Rate (RR): Assesses respiratory function. Increased or labored breathing could signify respiratory distress.
- Oxygen Saturation (SpO2): Measures the percentage of oxygen in the blood. Decreased SpO2 levels suggest inadequate oxygenation.
- Rate of Perceived Exertion (RPE): Subjective measure of how hard the patient feels they are working. It provides crucial feedback about individual tolerance.
Importance of Monitoring:
- Early Detection of Problems: Changes in vital signs can signal potential complications such as angina, arrhythmias, or respiratory issues, allowing for prompt intervention.
- Adjusting Exercise Intensity: Monitoring enables tailoring exercise intensity to individual tolerance and ensuring the exercise remains within safe limits.
- Tracking Progress: Changes in vital signs over time can indicate improvements in fitness and cardiovascular health.
- Ensuring Safety: Close monitoring is essential for patients with chronic conditions like heart disease, hypertension, or respiratory conditions, minimizing the risks of adverse events during exercise.
Example: If a patient’s blood pressure significantly increases during exercise, it might indicate a need to reduce the intensity or duration of the activity. Similarly, a drop in oxygen saturation would necessitate pausing the exercise and assessing the patient’s condition.
Q 12. How would you handle a patient who experiences chest pain during an exercise session?
Chest pain during an exercise session is a serious medical emergency and requires immediate action. It could indicate a range of conditions, including myocardial ischemia (reduced blood flow to the heart) or other cardiovascular problems.
Immediate Actions:
- Stop the Exercise Immediately: The patient should cease all physical activity immediately.
- Assess the Patient: Check vital signs (heart rate, blood pressure, respiratory rate), note the character and location of the chest pain, and assess their overall condition.
- Administer Oxygen (if available and trained): Oxygen can improve blood oxygen levels, aiding in myocardial oxygenation.
- Call Emergency Medical Services (EMS): This is crucial if the pain is severe, prolonged, or accompanied by other symptoms such as shortness of breath, dizziness, or nausea.
- Monitor Vital Signs Continuously: Continue to monitor the patient’s vital signs until EMS arrives.
- Provide Comfort and Support: Reassure the patient and make them as comfortable as possible.
Post-Emergency Care:
Once the patient is stable, a thorough medical evaluation is necessary to determine the cause of the chest pain. This may involve cardiac testing such as electrocardiograms (ECGs) or cardiac enzyme tests. The exercise program will be reassessed and potentially modified or stopped, depending on the findings.
Important Note: Never ignore chest pain during exercise. It is always better to err on the side of caution and seek immediate medical attention.
Q 13. Describe your experience with different types of exercise modalities (e.g., aerobic, resistance, flexibility).
My experience encompasses a wide range of exercise modalities, each tailored to specific needs and conditions. I have extensive experience in prescribing and supervising:
Aerobic Exercise: This is crucial for cardiovascular health and includes activities like walking, jogging, swimming, cycling, and elliptical training. I adapt intensity and duration based on individual fitness levels and health conditions. For example, I’ve successfully used interval training to improve cardiovascular fitness in patients with heart failure, carefully monitoring heart rate and oxygen saturation.
Resistance Training: This is vital for building and maintaining muscle mass, strength, and bone density. This includes exercises using free weights, resistance bands, weight machines, or even bodyweight exercises. I always prioritize proper form and technique to avoid injuries, tailoring programs to individual capabilities and pre-existing conditions. For example, I’ve worked with elderly patients with osteoarthritis, modifying resistance exercises to accommodate joint limitations.
Flexibility and Balance Training: These components are essential for maintaining joint mobility, improving balance, and preventing falls. I incorporate stretching, yoga, Pilates, and tai chi into exercise programs. Flexibility exercises help prevent muscle stiffness, especially relevant for patients with conditions like multiple sclerosis or Parkinson’s disease. Balance exercises are crucial for preventing falls in patients with neurological or orthopedic conditions.
Other Modalities: Depending on individual patient needs, I may incorporate other modalities such as aquatic therapy (beneficial for patients with joint pain or limited mobility) or functional training (focused on improving daily living activities). For example, aquatic therapy allows for low-impact cardiovascular exercise and resistance training without stressing weight-bearing joints.
Q 14. Discuss your knowledge of exercise testing and its applications in chronic disease management.
Exercise testing plays a vital role in chronic disease management. It helps us objectively assess a patient’s functional capacity, identify potential risks, and tailor exercise programs safely and effectively.
Types of Exercise Tests:
- Graded Exercise Test (GXT): This involves gradually increasing the intensity of exercise while monitoring vital signs (heart rate, blood pressure, ECG) to assess cardiovascular response and identify any limitations. It’s valuable for patients with cardiovascular disease or respiratory conditions.
- 6-Minute Walk Test (6MWT): A simple, widely used test measuring the distance a patient can walk in 6 minutes. It assesses functional capacity and endurance, especially helpful for patients with pulmonary or cardiac limitations.
- Balance Tests: Various balance tests (e.g., Berg Balance Scale, Timed Up and Go test) evaluate balance and fall risk, crucial for patients with neurological conditions or older adults.
- Muscle Strength and Endurance Tests: These tests assess muscular strength and endurance using dynamometers or manual muscle testing. They are important for patients recovering from injuries or with muscular dystrophy.
Applications in Chronic Disease Management:
- Risk Stratification: Exercise testing helps identify patients at high risk for cardiovascular events during exercise, allowing for careful planning and monitoring.
- Exercise Prescription: Test results guide the development of individualized exercise programs tailored to each patient’s capabilities and limitations.
- Monitoring Progress: Repeat testing over time helps track improvements in functional capacity and cardiovascular fitness.
- Intervention Planning: Test results might influence decisions regarding medical management, such as medication adjustments or surgical interventions.
Example: A patient with coronary artery disease undergoing a GXT might show limitations in their exercise capacity, informing the development of a low-intensity aerobic training program. Regular 6MWT assessments can then track their progress and guide program adjustments.
Q 15. How do you incorporate patient education into your exercise prescription?
Patient education is the cornerstone of successful exercise prescription. It’s not just about handing someone a workout plan; it’s about empowering them to understand why they’re exercising and how the exercise benefits their specific condition.
My approach involves a collaborative discussion, explaining the rationale behind each exercise, its impact on their condition, and addressing any misconceptions or fears they might have. For example, a patient with osteoarthritis might fear worsening joint pain. I’d explain how specific low-impact exercises, like aquatic therapy or cycling, can strengthen supporting muscles and improve joint stability, thus reducing pain in the long run. I use visual aids, handouts, and simple language tailored to their health literacy level. I also encourage questions and actively listen to their concerns, making the learning process interactive and empowering.
I also provide education on proper exercise technique, including warm-up and cool-down procedures, to minimize injury risk and maximize the benefits. Furthermore, I educate them on recognizing and responding to their body’s signals, emphasizing the importance of listening to their body and modifying the exercise as needed. Finally, I provide education on lifestyle modifications that complement the exercise program, such as nutrition and stress management, promoting holistic well-being.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your approach to motivating patients with low adherence to exercise programs.
Low adherence is a common challenge. My strategy focuses on building a strong therapeutic alliance and understanding the underlying barriers. This often involves open discussions to identify personal obstacles – time constraints, lack of motivation, social support, or even fear of failure.
I use motivational interviewing techniques to explore their intrinsic motivations and help them set realistic, achievable goals. Small, incremental successes build confidence and foster a sense of accomplishment, increasing motivation. I incorporate strategies like goal setting using the SMART method (Specific, Measurable, Achievable, Relevant, Time-bound). For example, instead of ‘exercise more,’ we might aim for ‘walk for 15 minutes three times a week.’
I tailor exercise programs to their preferences and lifestyle. If they enjoy dancing, we incorporate dance classes. If they prefer walking, we create routes that are convenient and enjoyable. Building social support is crucial, so I might encourage them to find a workout buddy or join a group fitness class. Regular check-ins and positive reinforcement help maintain momentum. Technology, like fitness trackers and apps, can provide feedback and encouragement.
Q 17. How would you modify an exercise program based on patient feedback and progress?
Regular monitoring of patient feedback and progress is essential for program adaptation. I actively solicit feedback during each session, using both structured questionnaires and open-ended questions to gauge their experience and identify any difficulties.
Progress is tracked through various methods, including subjective measures like pain scales and perceived exertion, and objective measures like strength tests, range of motion assessments, and functional fitness tests. This data helps me understand if the program is effective and identify areas needing modification. For instance, if a patient reports increased joint pain during a particular exercise, I might reduce the intensity, duration, or modify the exercise technique. If they are progressing well, I can gradually increase the intensity and duration to challenge them further, preventing plateaus.
This iterative process ensures the program remains safe, effective, and enjoyable, promoting long-term adherence. It’s important to remember that exercise prescription is not a static process. It’s dynamic and should evolve with the patient’s progress, feedback, and changing needs.
Q 18. How familiar are you with different exercise prescription guidelines (e.g., ACSM, AHA)?
I am very familiar with the exercise prescription guidelines published by organizations such as the American College of Sports Medicine (ACSM) and the American Heart Association (AHA). These guidelines provide evidence-based recommendations for safe and effective exercise programming across various populations, including those with chronic conditions.
I regularly consult the ACSM’s guidelines for exercise testing and prescription, using them to determine appropriate exercise modalities, intensity, duration, and frequency based on individual patient characteristics and medical history. Similarly, I utilize the AHA’s guidelines for cardiovascular health and rehabilitation, especially when working with patients with heart conditions. Understanding these guidelines ensures that my exercise prescriptions are aligned with best practices and minimize the risk of adverse events.
My understanding extends beyond simply following guidelines; I understand the underlying rationale and scientific evidence behind the recommendations, allowing me to make informed decisions and adapt the guidelines to individual patient needs. I am also aware of other relevant guidelines, such as those from the National Institute of Health (NIH) and other reputable organizations.
Q 19. Explain the importance of considering psychological factors in exercise prescription.
Ignoring psychological factors is a critical oversight in exercise prescription. Motivation, self-efficacy (belief in one’s ability to succeed), mood, and stress levels all significantly impact a patient’s adherence and overall response to exercise.
For example, a patient with depression might find it challenging to initiate and maintain an exercise program due to low energy levels and lack of motivation. Addressing these psychological barriers is as crucial as addressing the physical aspects of the condition. I use techniques like motivational interviewing, cognitive behavioral therapy (CBT) principles, and stress management strategies to build self-efficacy and foster a positive mindset towards exercise.
I regularly assess psychological factors through conversations, validated questionnaires (like the Exercise Motivation Inventory), and observation of their behavior and emotional responses during exercise. I then tailor the exercise program to address these factors and build their confidence. This might involve setting smaller, more attainable goals, providing positive feedback and reinforcement, and celebrating their successes. Collaboration with mental health professionals is sometimes necessary for patients with significant psychological challenges.
Q 20. What are your strategies for assessing and managing patient safety during exercise?
Patient safety is paramount. My approach to assessing and managing risk begins with a thorough health history and physical examination, including reviewing their medical records and any pre-existing conditions. This helps identify potential risks and contraindications to exercise.
I conduct a baseline assessment of their physical fitness, including cardiovascular fitness, muscular strength and endurance, and flexibility. This helps me design a safe and appropriate exercise program. During exercise sessions, I closely monitor their vital signs (heart rate, blood pressure) and observe their response to the exercise. I teach patients to recognize signs of overexertion, such as chest pain, dizziness, or extreme fatigue, and to immediately stop exercising and report these symptoms.
I emphasize proper exercise technique and provide individualized instruction to reduce the risk of injury. Emergency procedures are in place and clearly communicated, including access to emergency medical services. The exercise environment is also carefully considered, ensuring it is safe and appropriate for the patient’s abilities and needs. Regular communication with their physician ensures a coordinated approach to their care.
Q 21. How do you utilize technology (e.g., wearable sensors, telehealth) in exercise prescription?
Technology plays a crucial role in enhancing exercise prescription and adherence. Wearable sensors, such as fitness trackers and smartwatches, provide objective data on activity levels, heart rate, sleep patterns, and other physiological parameters. This data offers valuable insights into the patient’s response to the exercise program and helps me tailor the program accordingly.
Telehealth platforms enable remote monitoring and support, especially beneficial for patients with limited mobility or geographical constraints. I utilize telehealth for virtual consultations, exercise demonstrations, and progress tracking. Mobile applications offer structured exercise programs, reminders, and progress monitoring tools, enhancing patient engagement. For example, I might use a telehealth platform to demonstrate proper exercise form and provide immediate feedback to a patient with arthritis, ensuring they are performing the exercises correctly and safely.
Data from wearable sensors and telehealth platforms are integrated into the overall assessment and program modification process. This objective data, combined with subjective feedback, provides a more comprehensive understanding of patient progress and response to treatment, leading to more effective and personalized exercise interventions.
Q 22. Explain your understanding of the relationship between exercise and the immune system.
The relationship between exercise and the immune system is complex and bidirectional. Moderate exercise has been shown to boost the immune system, improving its ability to fight off infection. This is partly due to increased circulation of immune cells and the release of cytokines, which are signaling molecules that regulate immune responses. However, excessive or high-intensity exercise can actually suppress the immune system, making individuals more susceptible to illness. Think of it like a Goldilocks effect – too little exercise isn’t beneficial, but too much can be detrimental.
For example, regular moderate-intensity exercise can increase the number of natural killer cells (NK cells), which are crucial for early immune defense against viruses and cancer cells. Conversely, marathon running, for instance, has been linked to temporary immunosuppression, increasing the risk of upper respiratory tract infections in the days following the race. Therefore, appropriate exercise prescription must consider intensity, duration, and frequency to optimize immune function without compromising it.
Q 23. How would you address the barriers to exercise adherence in diverse populations?
Addressing barriers to exercise adherence requires a multifaceted approach tailored to the specific needs of diverse populations. Understanding the unique challenges faced by different groups is paramount.
- Socioeconomic factors: Lack of access to safe exercise facilities, financial constraints, and transportation limitations are significant barriers. Solutions might include subsidized programs, community-based initiatives, and home-based exercise plans.
- Cultural factors: Cultural norms, beliefs, and values can influence exercise participation. Culturally sensitive programs delivered by individuals from the same cultural background can be highly effective.
- Health literacy: Individuals with limited health literacy may struggle to understand exercise recommendations and their benefits. Clear, concise, and culturally appropriate communication strategies are essential.
- Comorbidities: Existing health conditions can limit exercise capacity. Careful assessment, individualized exercise prescriptions, and collaboration with other healthcare professionals are necessary.
- Personal preferences: Individual preferences for exercise types and settings are crucial. Offering a variety of options—from group fitness classes to solitary walks—can increase adherence.
For instance, I’ve worked with a low-income community by partnering with a local community center to offer free exercise classes and providing transportation assistance. Another example involved adapting exercise programs for individuals with limited mobility by focusing on chair exercises and aquatic therapy.
Q 24. Describe your experience with creating and implementing exercise programs in various settings (e.g., hospital, clinic, community).
My experience spans various settings, each presenting unique opportunities and challenges. In hospital settings, I’ve focused on early mobilization and cardiac rehabilitation programs, carefully monitoring patients’ vital signs and tailoring exercise to their specific cardiac conditions. This involves a gradual increase in intensity and duration under close medical supervision. In clinics, I’ve designed and implemented weight management and diabetes management programs, emphasizing behavioral change and incorporating both aerobic and resistance training. In community settings, I’ve led group fitness classes, organized walking groups, and developed educational workshops on healthy lifestyles.
A memorable experience involved creating a chair exercise program for elderly individuals in a senior center. It proved immensely popular, fostering socialization and improving their physical function and balance, significantly reducing fall risks.
Q 25. How do you tailor exercise programs to consider age-related physiological changes?
Age-related physiological changes necessitate significant adjustments to exercise programs. Older adults experience declines in muscle mass (sarcopenia), bone density (osteoporosis), cardiovascular function, and flexibility.
- Reduced intensity and duration: Exercise intensity and duration should be lower than for younger individuals to prevent injury and fatigue.
- Emphasis on functional fitness: Focus should be on exercises that improve balance, coordination, and strength, relevant to activities of daily living.
- Warm-up and cool-down: Thorough warm-up and cool-down periods are essential to prepare the body and prevent injury.
- Progressive overload: Gradually increasing exercise intensity and duration over time to avoid plateaus and promote adaptation.
- Multimodal approach: Combining aerobic exercise, resistance training, flexibility exercises, and balance training provides comprehensive benefits.
For example, for an older adult with osteoarthritis, I’d recommend low-impact aerobic exercises like swimming or cycling, combined with resistance training using light weights or resistance bands, and exercises to improve balance and flexibility, like tai chi.
Q 26. Discuss the ethical considerations involved in exercise prescription for individuals with chronic conditions.
Ethical considerations in exercise prescription for individuals with chronic conditions are paramount.
- Informed consent: Patients must fully understand the benefits and risks of exercise and provide informed consent before starting any program. This necessitates clear and transparent communication.
- Beneficence and non-maleficence: Exercise programs should maximize benefits while minimizing risks of injury or exacerbation of existing conditions.
- Autonomy: Respecting patients’ preferences, choices, and limitations is essential. The exercise plan should be collaboratively developed, empowering patients to actively participate in their care.
- Justice: Equitable access to exercise programs, regardless of socioeconomic status, ethnicity, or other factors, is vital.
- Confidentiality: Protecting patients’ privacy and confidentiality is mandatory.
For example, it would be unethical to prescribe high-intensity interval training (HIIT) to a patient with severe heart failure without appropriate medical clearance and careful monitoring.
Q 27. How would you collaborate with other healthcare professionals (e.g., physicians, physical therapists) to provide comprehensive care?
Collaboration with other healthcare professionals is crucial for providing holistic care. Effective communication and shared decision-making are key.
- Physicians: Physicians provide medical clearance, manage comorbidities, and monitor overall health status. Regular communication ensures exercise prescription aligns with medical goals.
- Physical therapists: Physical therapists address functional limitations and provide hands-on interventions such as manual therapy and gait training. Joint planning maximizes rehabilitation outcomes.
- Registered dietitians: Dietitians ensure proper nutrition to support exercise and overall health goals.
- Occupational therapists: Occupational therapists focus on improving daily living skills. This is particularly important in patients with chronic diseases affecting upper extremity function.
For instance, I’ve worked closely with a physician to tailor an exercise program for a patient with diabetes, integrating strategies to manage blood glucose levels effectively. Collaborative care ensures a comprehensive and integrated approach to patient wellbeing.
Q 28. Describe your experience with documenting patient progress and communicating with healthcare providers.
Accurate documentation of patient progress and clear communication with healthcare providers are essential components of effective care.
- Progress notes: Detailed progress notes should document initial assessments, exercise prescription, adherence, progress, and any modifications made to the program. These notes should include objective measures such as changes in weight, blood pressure, or functional capacity.
- Communication methods: Various communication methods, such as electronic health records (EHRs), progress reports, and direct communication with healthcare providers, facilitate effective information sharing.
- Data tracking: Tracking patient data, including exercise intensity, duration, and response, allows for objective monitoring of progress and timely adjustments to the program. This can involve using wearable technology or self-report methods.
- Feedback mechanisms: Regular feedback sessions with patients allow for addressing concerns, modifying the program as needed, and maintaining patient motivation.
For example, I use a standardized format for documenting patient progress, including specific measurements like resting heart rate, blood pressure, and functional fitness tests. I regularly share this information with the patient’s physician through the EHR system to ensure coordinated care.
Key Topics to Learn for Exercise Prescription for Chronic Conditions Interview
- Needs Analysis & Assessment: Understanding client history, medical conditions, functional limitations, and goals to create a safe and effective exercise plan.
- Exercise Program Design: Applying principles of exercise physiology and adapting exercise modalities (aerobic, resistance, flexibility) for various chronic conditions (e.g., cardiovascular disease, diabetes, arthritis).
- Program Progression & Modification: Adapting exercise intensity, duration, and type based on client response, progress, and potential setbacks. Understanding the importance of periodization and deloading.
- Risk Stratification & Safety: Identifying and mitigating potential risks associated with exercise in individuals with chronic conditions. Understanding contraindications and precautions.
- Behavioral Modification & Adherence: Strategies to promote long-term adherence to exercise programs, including motivational interviewing and goal setting techniques.
- Communication & Collaboration: Effectively communicating with clients, physicians, and other healthcare professionals regarding exercise prescription and progress.
- Legal & Ethical Considerations: Understanding scope of practice, informed consent, and professional liability related to exercise prescription.
- Monitoring & Evaluation: Utilizing appropriate assessment tools to track client progress, modify programs as needed, and demonstrate the efficacy of interventions.
- Specific Chronic Conditions: Deep understanding of exercise prescription guidelines for specific conditions such as coronary artery disease, type 2 diabetes, osteoarthritis, obesity, and chronic obstructive pulmonary disease.
- Technology & Exercise: Utilizing technology (wearable devices, telehealth) to enhance exercise prescription, adherence, and monitoring.
Next Steps
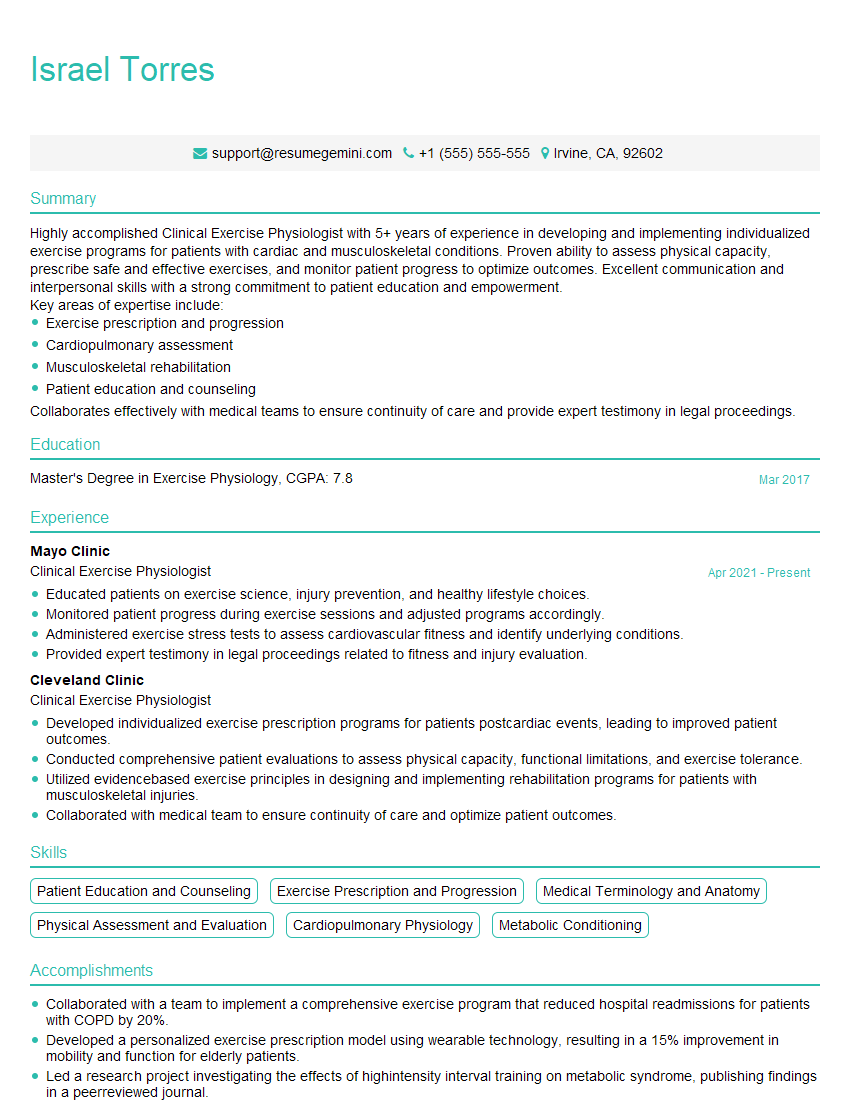
Mastering Exercise Prescription for Chronic Conditions is crucial for career advancement in healthcare and fitness settings. It demonstrates a high level of expertise and opens doors to specialized roles with greater responsibility and earning potential. To maximize your job prospects, creating a strong, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. Examples of resumes tailored to Exercise Prescription for Chronic Conditions are available to guide you through the process, ensuring your application stands out.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.