Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Eye Emergencies interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Eye Emergencies Interview
Q 1. Describe the immediate management of a patient presenting with a chemical burn to the eye.
Immediate management of a chemical burn to the eye is crucial to minimize permanent damage. Time is of the essence! The first step involves copious irrigation with sterile water or saline. Think of it like washing away a dangerous spill – the more you wash, the better the outcome. This should be done for at least 20-30 minutes, ideally under a continuous stream of fluid. We’re aiming to dilute and remove the offending chemical. Simultaneously, we would assess the patient’s visual acuity, using a Snellen chart if possible. Any associated injuries, like burns to the face or body, should also be addressed. After irrigation, we’d administer topical anesthetic drops for pain relief and assess the extent of the burn. The patient would then be immediately referred to an ophthalmologist for specialized assessment and potential surgical intervention.
Example: Imagine a construction worker gets lime splashed in their eye. Immediate, prolonged irrigation with water at the site, followed by urgent ophthalmology referral, is paramount.
Q 2. Explain the difference between a corneal abrasion and a corneal ulcer.
Both corneal abrasions and corneal ulcers are conditions affecting the cornea, the transparent front part of the eye, but they differ in severity and cause. A corneal abrasion is a superficial scratch or scrape on the corneal surface. Think of it like a minor road rash on your eye. It usually heals quickly without complications. A corneal ulcer, however, is a deeper, more serious infection or damage involving the corneal layers. It’s like a deep wound that requires medical attention. This can lead to scarring and vision loss if not treated promptly. The key difference lies in the depth of the injury and the presence of infection. Corneal abrasions are typically caused by trauma (like a scratch from a fingernail or a foreign body), while corneal ulcers often result from bacterial, viral, or fungal infections.
Example: A patient rubbing their eye with a dirty hand might develop a corneal abrasion. Conversely, a patient with compromised immunity might develop a corneal ulcer due to an untreated infection.
Q 3. How would you assess visual acuity in a patient with a suspected retinal detachment?
Assessing visual acuity in a suspected retinal detachment requires a cautious approach. Since any manipulation could worsen the detachment, we’d avoid any tests that might put stress on the eye. We’d begin with a basic assessment of the patient’s ability to see using a simple hand motion test, checking their light perception, and asking them to count fingers at a distance. If possible, a simple near vision assessment could be performed using a small print card. Detailed visual acuity tests like the Snellen chart are often postponed until the retinal detachment is addressed by an ophthalmologist. It’s critical to prioritize immediate referral to prevent irreversible vision loss. Remember that this assessment is part of the emergency evaluation to determine urgency and doesn’t replace the detailed assessment done later by a specialist.
Q 4. What are the key features of a hyphema, and how would you manage it?
A hyphema is a collection of blood in the anterior chamber of the eye, the space between the cornea and the iris. This typically presents as a visible layer of blood obscuring the iris. Key features include pain, decreased vision, and the presence of blood in the anterior chamber, easily visible on examination. Management involves immediate bed rest with the head elevated to 30-45 degrees to reduce intraocular pressure. We would avoid any straining activities and monitor the intraocular pressure closely. Topical cycloplegic agents (to dilate the pupils and reduce pain) might be used. If the hyphema is significant, or if there are other complications such as secondary glaucoma (increased eye pressure), surgical intervention might be necessary.
Example: A patient presenting with blurry vision and a reddish hue in their eye after blunt trauma to the face could be exhibiting a hyphema.
Q 5. Describe the appropriate initial management of a penetrating eye injury.
Initial management of a penetrating eye injury focuses on preventing further damage and preserving vision. The absolute priority is to stabilize the injured eye, protecting it from further trauma. We absolutely avoid any pressure or attempts to remove any penetrating object. Cover both eyes with a sterile shield to minimize movement and prevent further injury. Immediate analgesia (pain relief) and tetanus prophylaxis are given as needed. Then, the patient needs rapid transfer to an ophthalmology center or trauma unit. In the Emergency Department, the focus is on stabilizing the patient’s general condition and preventing any further damage to the eye while awaiting specialist assessment.
Example: Imagine a patient with a piece of metal embedded in their eye. The focus is immediate eye stabilization and protection, avoiding any attempts to remove the object in the field.
Q 6. How would you differentiate between a foreign body on the cornea and a corneal ulcer?
Differentiating between a foreign body on the cornea and a corneal ulcer requires a careful examination. A foreign body is typically visible as a discrete object on the corneal surface. The patient will often report a sensation of something in their eye, along with irritation and potential foreign body sensation. A corneal ulcer, in contrast, may not be visibly obvious initially. It may present with pain, redness, blurred vision, and photophobia (sensitivity to light). Fluorescein staining (a dye that highlights corneal defects) is a critical diagnostic tool. A foreign body will stain intensely at the location of the object, while a corneal ulcer shows a more diffuse and often irregular staining pattern, indicating a deeper lesion. Clinical judgement and appropriate use of staining are essential in making a distinction. If you are unsure, always err on the side of caution and refer to an ophthalmologist.
Q 7. Explain the process of irrigating a chemical burn to the eye.
Irrigating a chemical burn to the eye requires a methodical approach. The process involves using a copious amount of sterile saline or water, ideally under continuous irrigation. We typically use a Morgan lens or similar device, directing the flow of fluid across the eye’s surface. The goal is to neutralize and wash away the chemical agent as quickly as possible to reduce the extent of corneal damage. Irrigation should continue for a minimum of 20-30 minutes, with regular evaluation of the pH of the tear fluid to ensure neutralization. Irrigation is often carried out in the emergency department or under controlled conditions. The patient’s eyelids should be kept open during irrigation to ensure that the entire ocular surface is adequately flushed. After irrigation, the patient will be thoroughly examined for any remaining chemical injury, assessed for pain, and referred to an ophthalmologist for further evaluation and management.
Important Note: Never use neutralizers. Using substances like baking soda can cause further injury.
Q 8. What are the signs and symptoms of acute angle-closure glaucoma?
Acute angle-closure glaucoma is a serious eye emergency characterized by a sudden increase in intraocular pressure (IOP) due to blockage of the aqueous humor outflow pathway. Imagine your eye as a water balloon; normally, the fluid (aqueous humor) circulates and drains smoothly. In angle-closure glaucoma, this drainage is blocked, causing a build-up of pressure that can damage the optic nerve.
- Signs and Symptoms: The most common symptoms include sudden onset of severe eye pain, often described as a throbbing headache, blurred vision, halos around lights (seeing rainbows around lights), nausea, and vomiting. Patients may also experience eye redness and a feeling of pressure in the eye. It’s crucial to remember that these symptoms can develop rapidly, sometimes over just a few hours.
- Important Note: The presentation can vary, especially in elderly patients, who may not experience the characteristic severe pain but rather present with more subtle vision changes and reduced visual acuity. It’s essential to maintain a high index of suspicion for acute angle-closure glaucoma in any patient presenting with these symptoms, especially if there’s a family history of glaucoma or a history of prolonged near work.
Q 9. How would you manage a patient presenting with sudden vision loss?
Sudden vision loss is a true ophthalmic emergency requiring immediate action. The approach must be rapid and systematic to preserve vision. The initial assessment should rule out life-threatening conditions before focusing on the eyes.
- Immediate Assessment: First, obtain a detailed history, focusing on the onset, nature, and character of the vision loss. Is it unilateral or bilateral? Was the onset sudden or gradual? Was there associated trauma, pain, headache, or other symptoms? A thorough neurological examination is crucial to rule out stroke or other neurological causes.
- Visual Acuity: Assess visual acuity in each eye using a Snellen chart or hand-held visual acuity card.
- Ophthalmoscopy: Perform a thorough ophthalmoscopic examination to evaluate the optic disc, retinal vessels, and retina for any abnormalities like hemorrhage, edema, or ischemia.
- Pupil Examination: Examine pupils for size, shape, reactivity, and symmetry. A dilated or poorly reactive pupil may suggest serious pathology.
- Imaging: Based on the initial findings, urgent imaging, such as optical coherence tomography (OCT) or fluorescein angiography, may be necessary to determine the cause of the vision loss.
- Management: Depending on the suspected cause, management strategies vary from emergency treatment of acute angle-closure glaucoma (with medications to lower IOP), addressing vascular occlusion (like retinal artery occlusion), to initiating further investigations to rule out serious neurological causes.
Example: A patient presents with sudden painless loss of vision in one eye. Fundoscopy reveals a pale retina with a cherry-red spot, suggestive of central retinal artery occlusion. This requires immediate management with measures to improve retinal perfusion.
Q 10. Describe the use of fluorescein staining in diagnosing corneal injuries.
Fluorescein staining is a simple yet powerful diagnostic tool used to detect corneal abrasions and other corneal injuries. Fluorescein sodium, a water-soluble dye, stains damaged areas of the cornea, making them readily visible under a cobalt blue light (Wood’s lamp).
Mechanism: Fluorescein dye binds to damaged corneal epithelial cells. Intact epithelial cells are hydrophobic (water-repelling) and prevent dye uptake. However, damaged cells are permeable to the dye, leading to staining and visualization. The dye is non-toxic and will be washed away with the body’s natural processes.
Procedure: A strip of fluorescein is applied to the lower eyelid. The patient blinks several times, ensuring that the dye is evenly distributed over the cornea. The cornea is then examined under a cobalt blue light, allowing for the clear visualization of any stained areas. This allows for precise location and assessment of the injury’s size and severity.
Clinical Significance: Fluorescein staining aids in differentiating between various corneal conditions. A clearly defined stained area indicates a superficial abrasion. Diffuse staining might suggest a more significant corneal injury like a corneal ulcer or infection. The pattern and extent of staining guide the treatment strategy.
Q 11. What are the contraindications for topical anesthetic use in eye injuries?
Topical anesthetics, while helpful for pain relief in eye injuries, carry significant contraindications and risks, especially in the context of corneal injuries. Their use should be approached cautiously and strategically.
- Delayed Healing: The most significant risk is delayed corneal epithelial healing. Anesthesia masks the pain which would normally warn the patient to avoid rubbing their eyes. Rubbing, which can cause further damage, is a common cause of complications.
- Increased Risk of Infection: The loss of corneal sensation impairs the eye’s natural defense mechanisms, making it more vulnerable to bacterial, fungal, or viral infections. The lack of pain may mask the progression of these infections.
- Toxicity: Prolonged or repeated use of topical anesthetics can lead to corneal toxicity, causing damage to the corneal epithelium and even potentially corneal ulceration.
- Poor Patient Cooperation: Because patients cannot feel pain, they may not realize that they’re touching or rubbing their eyes, which can worsen the injury.
In Summary: Topical anesthetics should be used sparingly and only when absolutely necessary, typically for brief periods and under strict medical supervision. They are not a substitute for proper assessment, diagnosis, and management of the injury.
Q 12. How would you stabilize a globe perforation until surgical intervention?
Globe perforation is a severe eye injury requiring immediate surgical intervention. Stabilization before surgery aims to minimize further damage and protect the eye from further trauma.
- Do Not Apply Pressure: The first and foremost principle is to avoid applying pressure to the injured eye. This can worsen the perforation and damage delicate intraocular structures.
- Gentle Cleansing: If necessary, gently cleanse the surrounding area with sterile saline solution to remove any loose debris or foreign bodies. Avoid any forceful rubbing or scrubbing.
- Eye Shield: Apply a rigid eye shield to protect the eye from further injury during transport to a specialist ophthalmologist or emergency room. This should be done carefully, avoiding any pressure to the globe itself.
- Positioning: Position the patient comfortably, preferably with the injured eye slightly elevated to reduce intraocular pressure. This helps to minimize potential further damage.
- Systemic Support: Assess for systemic injuries and provide any necessary supportive care, including intravenous fluids and pain management, while awaiting definitive surgical repair. Antibiotic prophylaxis may be administered.
Example: A patient presents with a penetrating injury to the eye following a high-velocity trauma. The eye is immediately covered with a rigid shield, minimizing pressure, and the patient is rushed to the operating room. The goal is to quickly preserve the eyeball.
Q 13. Explain your understanding of the visual pathways and how damage impacts vision.
The visual pathways are a complex network of neural structures responsible for transmitting visual information from the retina to the visual cortex in the brain. Understanding these pathways is critical for interpreting the effects of damage to the visual system.
- Retina: The visual journey begins at the retina, where light is converted into neural signals by photoreceptor cells (rods and cones).
- Optic Nerve: These signals travel through the optic nerve to the optic chiasm.
- Optic Chiasm: Here, fibers from the nasal (inner) halves of each retina cross over to the opposite side of the brain. This allows the right visual field to be processed by the left hemisphere and vice-versa.
- Optic Tract: After the chiasm, the fibers continue as the optic tract to the lateral geniculate nucleus (LGN) of the thalamus.
- Lateral Geniculate Nucleus (LGN): The LGN acts as a relay station, processing and refining visual signals before sending them to the visual cortex.
- Visual Cortex: Finally, the signals reach the visual cortex in the occipital lobe, where visual information is interpreted and consciously perceived.
Impact of Damage: Damage at any point in this pathway can result in specific visual field defects. For example, damage to the optic nerve results in monocular vision loss (loss of vision in one eye). Damage to the optic chiasm can cause bitemporal hemianopsia (loss of the temporal visual fields in both eyes). Damage to the optic tract results in homonymous hemianopsia (loss of the same visual field in both eyes). The location of the damage dictates the type of visual loss.
Q 14. What are the potential complications of a corneal abrasion?
A corneal abrasion is a scratch on the surface of the cornea, the clear front part of the eye. While often minor and self-healing, complications can arise if not properly managed.
- Infection: The most significant risk is infection, particularly from bacteria like Pseudomonas aeruginosa, which can lead to a corneal ulcer, potentially causing permanent vision loss. A delay in healing or worsening symptoms are red flags for infection.
- Delayed Healing: Factors such as contact lens wear, dryness, or underlying conditions can delay healing, increasing the risk of infection and scarring.
- Corneal Ulcer: A severe infection that penetrates beyond the surface epithelium can lead to a corneal ulcer, characterized by significant pain, reduced vision, and potential perforation.
- Scarring: Significant abrasions or infections can result in corneal scarring, which can distort vision and lead to astigmatism.
- Symblepharon: In severe cases, adhesions may form between the eyelids and the cornea, leading to symblepharon. This requires surgical intervention to restore normal eyelid mobility.
Prevention and Management: Prompt diagnosis and treatment are key to preventing complications. This includes appropriate antibiotic eye drops, pain relief, and avoidance of contact lenses until healing is complete. Patients should be instructed on proper eye hygiene to minimize the risk of infection.
Q 15. Discuss the management of a patient with orbital cellulitis.
Orbital cellulitis is a serious infection of the tissues surrounding the eye. It requires immediate medical attention because it can lead to serious complications like blindness or meningitis. Management begins with a thorough history and physical exam focusing on the severity of the infection and any potential source, such as a recent sinusitis or trauma.
- Imaging: CT or MRI scans are crucial to assess the extent of the infection and rule out complications like abscess formation or cavernous sinus thrombosis.
- Intravenous Antibiotics: Broad-spectrum intravenous antibiotics, targeting both Gram-positive and Gram-negative bacteria, are the cornerstone of treatment. The choice of antibiotic will depend on the suspected pathogen and local antibiotic sensitivities.
- Pain Management: Analgesics, such as acetaminophen or ibuprofen, are provided to manage pain and discomfort.
- Hospitalization: Patients with severe cellulitis, significant orbital involvement, or evidence of systemic illness generally require hospitalization for close monitoring and intravenous antibiotic administration.
- Surgical Intervention: In cases of abscess formation or lack of response to antibiotics, surgical drainage may be necessary.
For instance, I recently managed a patient with orbital cellulitis secondary to a dental infection. Early diagnosis and aggressive intravenous antibiotic treatment led to a successful outcome, avoiding the need for surgery. The key is prompt recognition and intervention.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with ophthalmic medications and their potential side effects.
My experience encompasses a wide range of ophthalmic medications, from topical agents like artificial tears and glaucoma medications to injectable medications for macular degeneration and other retinal conditions. I’m familiar with the administration techniques, potential side effects, and drug interactions for each.
- Topical Medications: These are commonly used for conditions like glaucoma, dry eye disease, and conjunctivitis. Side effects can include burning, stinging, redness, and allergic reactions. For example, some glaucoma medications can cause blurred vision or affect heart rate.
- Injectable Medications: Intravitreal injections are used to treat macular degeneration and other retinal conditions. Potential side effects include increased intraocular pressure, bleeding, infection, and retinal detachment. Careful patient selection and meticulous sterile technique are crucial.
- Oral Medications: Oral medications may be used to treat certain inflammatory conditions affecting the eye. The potential side effects vary depending on the drug but can include gastrointestinal disturbances and allergic reactions.
I always discuss potential side effects with patients before initiating treatment, empowering them to report any adverse reactions promptly. Careful monitoring and adjustment of medication are important aspects of my practice.
Q 17. How do you assess for intraocular pressure?
Intraocular pressure (IOP) is the pressure inside the eye. Elevated IOP is a significant risk factor for glaucoma. We assess IOP using various methods, the most common being tonometry.
- Applanation Tonometry: This is the gold standard, using a slit lamp to flatten the cornea with a calibrated force. The reading directly reflects IOP.
- Non-Contact Tonometry: This method uses a puff of air to indent the cornea. It’s less accurate than applanation but convenient and suitable for patients who may be apprehensive about contact tonometry.
- Rebound Tonometry: This is a portable device that provides an IOP measurement via a small probe. Its accuracy varies slightly compared to applanation but is useful in situations where portability is beneficial.
Accurate IOP measurement is crucial for diagnosing and monitoring glaucoma. Variations in technique and calibration can affect results, hence regular calibration of equipment is mandatory.
Q 18. Explain the differences in treatment between open-angle and angle-closure glaucoma.
Open-angle glaucoma and angle-closure glaucoma are both types of glaucoma, characterized by elevated IOP leading to optic nerve damage. However, the underlying mechanisms differ significantly, leading to contrasting treatment approaches.
- Open-Angle Glaucoma: This is the most common type, where the drainage angle of the eye remains open, but the outflow of aqueous humor is impaired. Treatment primarily focuses on lowering IOP using medication (e.g., prostaglandin analogues, beta-blockers, alpha-agonists), laser trabeculoplasty, or surgery (e.g., trabeculectomy).
- Angle-Closure Glaucoma: This is a less common, but more urgent type where the iris blocks the drainage angle, causing a sudden spike in IOP. Treatment is often more aggressive, aiming for rapid IOP reduction. This might involve medications, laser peripheral iridotomy (to create an opening in the iris), or surgery in acute cases. Immediate medical attention is critical as this can lead to rapid vision loss.
The key difference lies in the urgency of intervention. Open-angle glaucoma is generally managed gradually, while angle-closure glaucoma demands immediate action to prevent irreversible vision loss. Patient education regarding medication compliance, lifestyle modifications, and regular follow-up appointments are crucial for both types.
Q 19. What are the common causes of optic neuritis?
Optic neuritis is inflammation of the optic nerve, leading to vision loss, often affecting one eye. The most common cause is multiple sclerosis (MS).
- Multiple Sclerosis (MS): This autoimmune disease is the leading cause of optic neuritis in young adults, and often precedes a diagnosis of MS.
- Infections: Viral infections (e.g., herpes zoster, influenza) can cause optic neuritis.
- Autoimmune Diseases: Besides MS, other autoimmune diseases like lupus and sarcoidosis can also cause optic neuritis.
- De-myelinating disorders: Conditions such as neuromyelitis optica can lead to optic nerve damage.
- Neuropathies: Certain neurological disorders or nerve disorders can impact the optic nerve as well.
- Other less common causes: These include medications, toxins and in rare instances, tumors.
A thorough evaluation is essential to identify the underlying cause and implement appropriate management, which may include corticosteroids to reduce inflammation.
Q 20. How would you counsel a patient with a diagnosis of macular degeneration?
Macular degeneration is a leading cause of vision loss, affecting the central part of the retina responsible for sharp, detailed vision. Counseling focuses on managing expectations, optimizing remaining vision, and promoting quality of life.
- Understanding the Disease: Explaining the different types (dry and wet) and their progression is paramount. Using simple analogies helps patients grasp the impact on their vision.
- Vision Rehabilitation: Referral to low-vision specialists for training in adaptive strategies to maximize remaining vision, such as using magnifiers or adaptive devices.
- Lifestyle Modifications: Encouraging a healthy diet rich in antioxidants, regular exercise, and smoking cessation helps in slowing disease progression, especially in the case of dry AMD.
- Treatment Options: Depending on the type, discussing potential treatments like anti-VEGF injections for wet AMD and nutritional supplements for dry AMD is crucial. Managing expectations is important, emphasizing the limitations of current treatments.
- Emotional Support: Vision loss can be emotionally challenging. Providing emotional support, facilitating access to support groups, and connecting with relevant resources is vital.
For example, I counsel patients with wet AMD about the importance of regular anti-VEGF injections to prevent further vision loss. I explain the potential side effects and the need for close monitoring. I also help them adjust to their vision changes and maintain their independence.
Q 21. Explain your experience with different types of eye patching techniques.
Eye patching techniques are crucial for various ophthalmic conditions, requiring proper application for efficacy and patient comfort.
- Simple Patching: This involves applying a sterile patch directly over the eye, securing it with surgical tape. It’s used for conditions like corneal abrasions or post-operative care. The key is ensuring complete coverage and comfortable placement avoiding pressure on the eye.
- Pressure Patching: This technique applies a firm pressure patch over the eye, sometimes used after eye surgery to minimize bleeding or swelling. The patch must be appropriately tight to exert the necessary pressure but must not compromise circulation or cause excessive discomfort.
- Sterile Technique: Maintaining sterile technique during patching is crucial to prevent infection. This includes using sterile gloves, ensuring clean hands, and avoiding contamination of the patch material.
- Patch Removal: Patches should be removed as instructed by the ophthalmologist, gently peeling the edges. Gentle cleansing of the eyelid area is usually recommended.
My experience highlights the importance of teaching patients proper patching techniques. Incorrect application can compromise healing and increase the risk of complications. I always demonstrate the procedure, answer any questions, and provide clear instructions before discharge, ensuring they can effectively manage their eye patch at home.
Q 22. Discuss the importance of proper documentation in eye emergency cases.
Proper documentation in eye emergencies is paramount for several reasons. It forms the cornerstone of patient care, legal protection, and facilitates effective communication among healthcare providers. Think of it as a detailed roadmap of the patient’s journey through the emergency.
- Legal Protection: Comprehensive documentation protects both the patient and the medical team from potential legal issues. It demonstrates that appropriate care was provided, and if any errors occurred, they can be identified and addressed.
- Continuity of Care: Accurate records ensure seamless transitions of care between different specialists or facilities. For instance, if a patient needs to be transferred to a specialized ophthalmology center, a thorough record facilitates immediate understanding of the situation.
- Improved Patient Outcomes: Detailed documentation enables a more precise diagnosis and facilitates appropriate treatment planning. It also helps track the patient’s progress and response to treatment.
- Research and Quality Improvement: Aggregated data from detailed patient records contributes significantly to ophthalmic research and helps to identify areas for improvement in emergency eye care protocols.
For example, meticulously documenting the time of injury, the mechanism of injury (e.g., chemical splash, blunt trauma), visual acuity measurements, and findings during ophthalmoscopy and slit-lamp examination are critical. Any interventions performed, such as irrigation or administration of medications, should be precisely recorded.
Q 23. How do you ensure accurate communication during eye emergency situations with both patients and other medical personnel?
Effective communication is the lifeblood of successful emergency care. In eye emergencies, miscommunication can have severe consequences. My strategy involves a multi-pronged approach:
- Clear and Concise Language: I use simple, non-medical jargon when communicating with patients, ensuring they understand the situation and the necessary steps. For example, instead of saying ‘We need to perform fluorescein staining,’ I might explain, ‘We’ll put a few drops in your eye to see if there’s any damage to the surface.’
- Active Listening: I actively listen to the patient’s concerns and answer their questions patiently and comprehensively. Building trust fosters cooperation and helps alleviate anxiety.
- Structured Reporting to Medical Personnel: When communicating with other healthcare professionals, I use a structured format, often following the SBAR (Situation, Background, Assessment, Recommendation) method. This provides a clear and concise summary of the patient’s condition, history, my assessment, and my recommendations for further management.
- Use of Technology: Electronic health records (EHRs) provide a platform for efficient and secure information sharing among the healthcare team.
For instance, if a patient presents with a suspected corneal abrasion, I would clearly communicate to the ophthalmologist the details of the injury, the patient’s visual acuity, and my initial findings from the slit-lamp examination using SBAR format. This ensures efficient triage and treatment.
Q 24. Describe your experience using ophthalmoscopy and slit-lamp biomicroscopy.
Ophthalmoscopy and slit-lamp biomicroscopy are essential tools in my practice. I’ve used them extensively throughout my career to diagnose and manage a wide range of eye conditions.
Ophthalmoscopy: I’m proficient in both direct and indirect ophthalmoscopy. Direct ophthalmoscopy allows for a magnified view of the retina, optic nerve, and blood vessels, enabling the detection of conditions like retinal detachments, hemorrhages, and papilledema. Indirect ophthalmoscopy provides a wider field of view, useful for evaluating the peripheral retina.
Slit-lamp Biomicroscopy: This instrument allows for detailed examination of the anterior segment of the eye, including the cornea, conjunctiva, iris, and lens. It’s invaluable for diagnosing conditions such as corneal ulcers, iritis, and cataracts. I am comfortable using various slit-lamp techniques, including magnification, illumination adjustments, and gonioscopy (examining the angle of the anterior chamber).
Over the years, my proficiency has grown through continuous practice, participation in workshops and training sessions, and by regularly reviewing ophthalmic images and case studies. I’m also adept at interpreting the findings obtained from these techniques and correlating them with the patient’s clinical presentation to arrive at an accurate diagnosis.
Q 25. What are your strategies for managing a patient who is anxious or in pain during an eye examination?
Managing anxious or painful patients requires a compassionate and empathetic approach. My strategy focuses on building rapport, providing reassurance, and employing pain management techniques.
- Empathy and Reassurance: I begin by acknowledging the patient’s anxiety and pain, validating their feelings. I explain the examination procedure clearly and simply, answering their questions patiently. A calm and reassuring demeanor goes a long way.
- Pain Management: For patients experiencing significant pain, I may use topical anesthetic drops to numb the eye. In cases of severe pain or discomfort, I may consider systemic analgesics, collaborating with other medical personnel as needed.
- Distraction Techniques: For anxious patients, I may use distraction techniques like engaging them in conversation or offering them something to focus on, such as a photograph or a calming object.
- Involving Support Personnel: If necessary, I involve family members or support personnel to provide emotional support and comfort to the patient.
For instance, a child with a painful corneal abrasion might benefit from a combination of topical anesthetic, distraction techniques (like engaging them in a simple game), and reassurance from a parent.
Q 26. Describe a time you had to make a critical decision under pressure in an eye emergency situation.
One instance that stands out involved a patient who presented with sudden vision loss and intense eye pain. Initial examination suggested a possible acute angle-closure glaucoma, a time-sensitive emergency. The patient’s intraocular pressure was dangerously elevated.
The challenge was that the patient was also severely claustrophobic, making it difficult to perform a thorough examination and administer necessary medications. Under pressure, I quickly decided to administer topical medications to lower intraocular pressure while simultaneously providing reassurance and using distraction techniques to minimize distress. I then immediately contacted the ophthalmology consultant and facilitated an expedited transfer to a surgical facility for laser peripheral iridotomy to prevent permanent vision loss. The quick response and collaborative effort ensured the patient maintained their eyesight.
This situation highlighted the critical role of rapid assessment, decisive action, and effective communication in managing time-sensitive eye emergencies. The experience reinforced the importance of adaptability and resourcefulness when dealing with complex situations.
Q 27. How do you stay current with the latest advancements and best practices in eye emergency care?
Staying current in eye emergency care requires continuous professional development. My strategies include:
- Regular Participation in Continuing Medical Education (CME): I actively attend conferences, workshops, and online courses focusing on advances in ophthalmology and emergency medicine.
- Membership in Professional Organizations: Membership in professional organizations like the American Academy of Ophthalmology provides access to the latest research, guidelines, and educational resources.
- Review of Peer-Reviewed Literature: I regularly review leading ophthalmic journals to stay informed about new research findings and best practices.
- Collaboration with Colleagues: Discussions and collaborations with colleagues, especially ophthalmologists, provide valuable insights and learning opportunities.
- Online Resources: I utilize reputable online resources such as UpToDate and PubMed to access the latest evidence-based information.
Staying abreast of advancements ensures I can provide the most up-to-date and effective care to my patients.
Q 28. How would you handle a situation where you are unsure of the diagnosis or treatment for a specific eye emergency?
When faced with diagnostic uncertainty, my approach is structured and methodical.
- Thorough Re-evaluation: I meticulously review the patient’s history, perform a comprehensive eye examination, and reassess the initial findings. I may repeat certain tests or utilize additional diagnostic tools to gain a clearer picture.
- Consultation with Specialists: If I remain uncertain, I immediately consult with an ophthalmologist or other relevant specialists. This ensures that the patient receives expert advice and appropriate management.
- Evidence-Based Literature Review: I conduct a thorough literature review to examine relevant case reports and studies, seeking to find similar cases and their management strategies.
- Conservative Management: In many situations, I may opt for conservative management, focusing on symptomatic relief and close monitoring, while waiting for diagnostic clarity.
It’s crucial to remember that seeking expert advice is not a sign of weakness but rather demonstrates a commitment to ensuring optimal patient care. It’s always better to err on the side of caution and seek help than to delay potentially life-changing treatment.
Key Topics to Learn for Eye Emergencies Interview
- Acute Red Eye Syndromes: Differentiating between infectious (e.g., conjunctivitis, keratitis) and non-infectious causes (e.g., corneal abrasions, iritis). Practical application: Developing a systematic approach to history taking and examination to arrive at a differential diagnosis.
- Trauma: Management of penetrating and blunt ocular trauma, including initial assessment, stabilization, and appropriate referral pathways. Practical application: Understanding the indications for immediate surgical intervention versus conservative management.
- Chemical Burns: Immediate first aid and subsequent management of alkali and acid burns, emphasizing irrigation techniques and appropriate follow-up care. Practical application: Calculating irrigation time and understanding the long-term complications.
- Glaucoma: Recognizing acute angle-closure glaucoma and its management. Practical application: Understanding the importance of rapid intervention to prevent vision loss.
- Orbital Emergencies: Identifying and managing conditions like orbital cellulitis, retrobulbar hemorrhage, and other orbital pathologies. Practical application: Understanding the signs and symptoms that require immediate referral to an ophthalmologist.
- Foreign Body Removal: Safe and effective techniques for removing foreign bodies from the cornea, conjunctiva, and other ocular structures. Practical application: Knowing when to refer a patient for removal due to complexity or risk.
- Assessment and Documentation: Thorough documentation of patient history, examination findings, and management plan. Practical application: Utilizing standardized terminology and clear communication with other healthcare professionals.
Next Steps
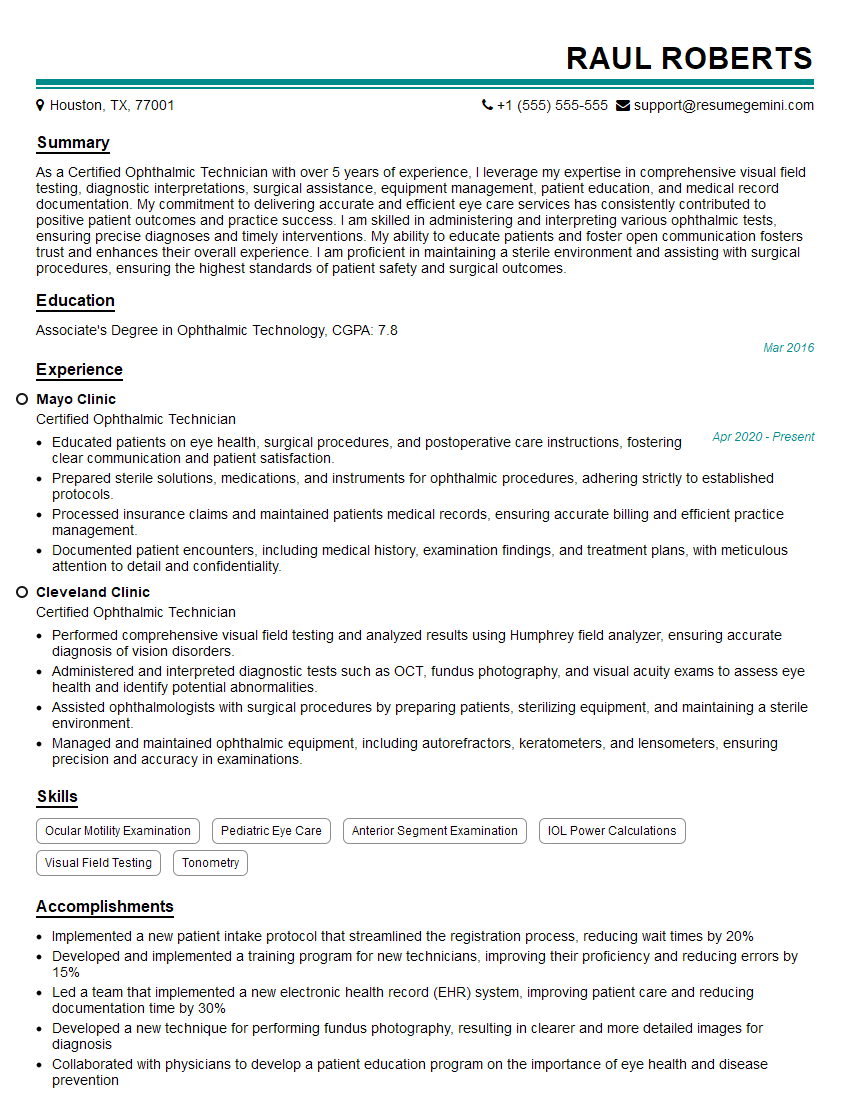
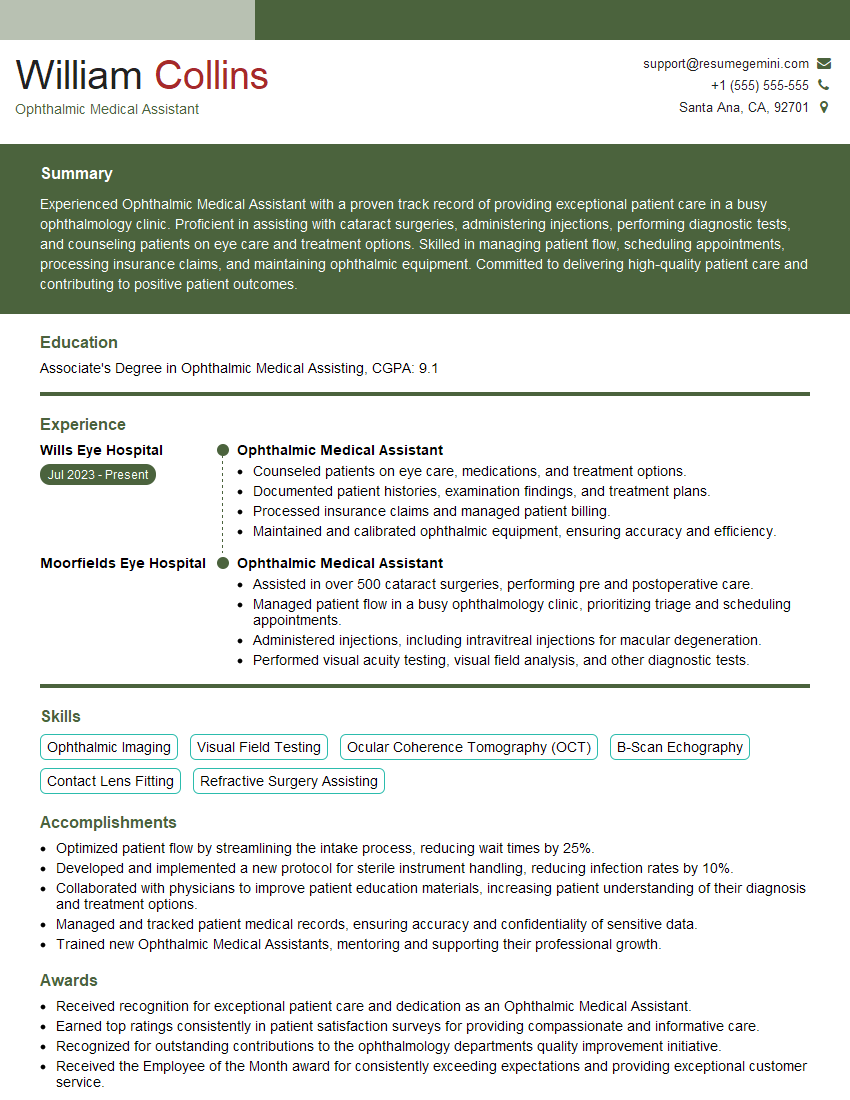
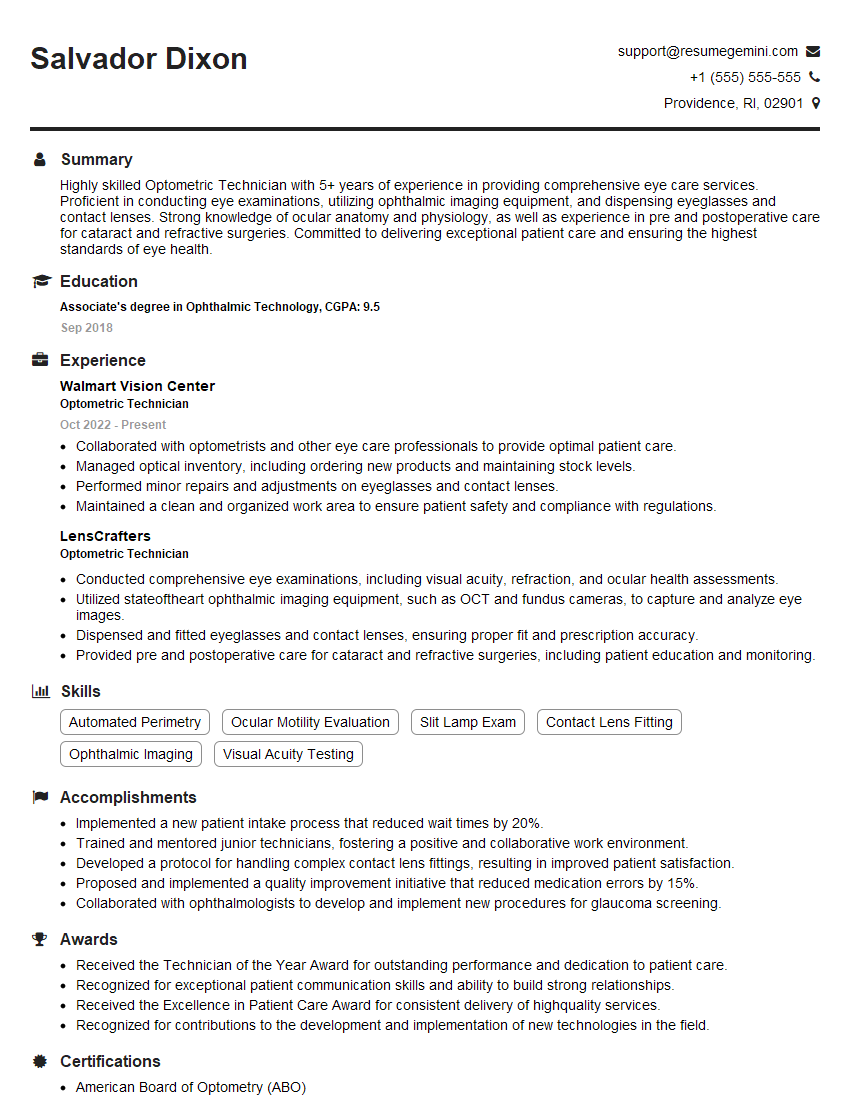
Mastering the management of eye emergencies is crucial for career advancement in ophthalmology and related fields. Demonstrating a solid understanding of these critical concepts will significantly enhance your interview performance and job prospects. To further strengthen your application, creating an ATS-friendly resume is essential for getting your qualifications noticed by recruiters. ResumeGemini is a trusted resource that can help you build a professional and effective resume, tailored to highlight your expertise in eye emergencies. Examples of resumes tailored to this specialization are available within the ResumeGemini platform.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.