Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Facial Nerve Evoked Response interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Facial Nerve Evoked Response Interview
Q 1. Explain the principles behind Facial Nerve Evoked Response (FNER) testing.
Facial Nerve Evoked Response (FNER) testing is a neurophysiological technique used to assess the integrity of the facial nerve. It works by stimulating the facial nerve with a brief electrical pulse and recording the resulting electrical activity in the facial muscles. The principles are based on the fact that a healthy facial nerve will conduct this electrical signal efficiently, resulting in a specific pattern of electrical activity detected at the muscle. Deviations from this pattern can indicate damage or dysfunction within the nerve pathway.
Imagine it like sending a signal down a wire. In FNER, we send an electrical ‘pulse’ along the facial nerve ‘wire’. If the wire is intact and working correctly, we get a clear and predictable signal at the other end (the muscle). A weak, delayed, or absent signal suggests a problem somewhere along the wire.
Q 2. Describe the different types of FNER stimuli used and their applications.
Several types of stimuli are used in FNER, each with its own advantages and applications:
- Electrical stimulation: This is the most common method, using brief electrical pulses delivered through surface electrodes placed near the stylomastoid foramen (where the facial nerve exits the skull) or directly to the nerve itself (for example, during surgery). It’s reliable and easy to apply.
- Acoustic stimulation: This involves using clicks or other sounds to stimulate the facial nerve via the acoustic reflex pathway. It’s useful for assessing the auditory-facial reflex and potentially identifying lesions affecting this pathway.
- Magnetic stimulation: This utilizes magnetic pulses to non-invasively stimulate the facial nerve. It’s relatively new but offers potential advantages over electrical stimulation, especially in cases where surface stimulation is difficult.
The choice of stimulus depends on the clinical question. For example, electrical stimulation is commonly used to evaluate Bell’s palsy, while acoustic stimulation might be more helpful in diagnosing certain types of hearing loss with associated facial nerve involvement.
Q 3. What are the common recording montages used in FNER studies?
Common recording montages in FNER involve placing surface electrodes over the facial muscles innervated by the facial nerve. The specific placement varies depending on the clinical question and the area of interest. However, some common configurations include:
- Active electrode over the orbicularis oculi muscle (eye closure): This helps evaluate the upper branch of the facial nerve.
- Active electrode over the orbicularis oris muscle (lip pursing): This assesses the lower branch of the facial nerve.
- Reference electrode: A reference electrode is placed on a non-active site, such as the earlobe or forehead, to minimize interference.
- Ground electrode: A ground electrode is placed on a neutral point, such as the forehead, to reduce noise.
The choice of montage aims to maximize the signal-to-noise ratio and obtain the clearest representation of the facial nerve’s response.
Q 4. How do you interpret latency and amplitude measurements in FNER?
Latency refers to the time it takes for the electrical signal to travel from the stimulation site to the muscle. Increased latency indicates slowed conduction, suggesting damage to the nerve. Amplitude refers to the size of the recorded electrical response. Reduced amplitude indicates decreased muscle activation or nerve fiber loss.
For example, a prolonged latency in the orbicularis oculi muscle response suggests a lesion along the upper branch of the facial nerve, while a reduced amplitude in the orbicularis oris response could indicate denervation of the lower branch.
Think of it like measuring the time and strength of a relay race. A slow time (latency) indicates a runner (nerve) is struggling, while a weak finish (amplitude) suggests a problem with the runner or the team (muscle).
Q 5. Explain the significance of different FNER waveforms.
FNER waveforms consist of several peaks and troughs reflecting different stages of signal transmission along the facial nerve. The significance of each waveform component can provide detailed information about the location and extent of nerve damage.
- Early components: These reflect the proximal parts of the facial nerve near the stimulation site. Changes here may indicate lesions closer to the brainstem.
- Later components: These reflect distal parts and terminal branches of the facial nerve, providing insight into the condition of peripheral nerve segments.
By analyzing the different components of the waveform (e.g., presence or absence of certain peaks, their amplitude and latency), neurologists can better localize the pathology and diagnose different facial nerve conditions more accurately.
Q 6. What are the normal values and ranges for FNER parameters?
Normal values for FNER parameters vary depending on factors like age, stimulus intensity, and recording technique. There is no universally accepted ‘normal’ range, but typical values are usually established by the specific lab performing the test and are usually given in a range. Generally, however, latencies are expected to be within a certain timeframe (e.g., below a certain threshold) and amplitudes are expected to be above a certain level for each corresponding muscle response. Significant deviations from these established ranges would indicate abnormality.
It is crucial to consult the specific normative data provided by the laboratory conducting the study for accurate interpretation of results. Each lab may have its own established normal values obtained from a study of healthy individuals.
Q 7. Describe the common artifacts encountered during FNER recording and how to mitigate them.
Several artifacts can interfere with FNER recordings, including:
- Electrode movement: Poor electrode contact or movement during recording causes noise and unstable waveforms. Careful electrode placement and securing are essential.
- Muscle activity: Patient movement or spontaneous muscle contractions can create unwanted signals. Relaxation techniques and appropriate patient instructions can minimize this. Often, averaging multiple trials helps to reduce this effect.
- Electrical interference: Electrical noise from surrounding equipment can corrupt the signal. Shielding the recording setup and using appropriate filtering techniques is important.
- Eye blinks: Eye blinks generate strong electrical signals that can contaminate facial nerve responses. Asking the patient to minimize blinking is key. This often requires the use of careful instruction and potentially even anesthetic eye drops.
Mitigation strategies involve careful patient preparation, meticulous electrode placement, proper grounding, and utilizing appropriate filtering techniques during signal processing. Experience in artifact identification and correction is crucial for obtaining reliable results. Sometimes, repeating the test is necessary when significant artifact contaminates the data.
Q 8. How does FNER differ from other electrodiagnostic techniques such as EMG and NCS?
Facial Nerve Evoked Response (FNER) is a specialized electrodiagnostic technique used to assess the function of the facial nerve. Unlike electromyography (EMG), which primarily evaluates muscle activity, and nerve conduction studies (NCS), which measure the speed of nerve impulse conduction along peripheral nerves, FNER specifically focuses on the nerve’s response to electrical stimulation.
In essence, FNER measures the electrical activity of the facial nerve itself in response to a stimulus, usually delivered near the stylomastoid foramen. This differs from EMG, which assesses the result of facial nerve activity in the muscles of facial expression, and NCS which assesses the speed of nerve impulse transmission across longer stretches of nerve. EMG can reveal muscle damage, while NCS detects problems along the nerve pathway. FNER provides direct insight into the nerve’s ability to transmit signals.
Think of it this way: EMG is like checking if a lightbulb is shining, NCS is like checking the wire connecting the lightbulb to the power source, and FNER is like checking the electrical signal itself at the switch controlling the lightbulb.
Q 9. Explain the clinical applications of FNER in diagnosing facial nerve disorders.
FNER plays a crucial role in diagnosing various facial nerve disorders. It’s invaluable in identifying the location and nature of lesions affecting the facial nerve, whether they are caused by Bell’s palsy, trauma, tumors, or other pathologies. For example, in Bell’s palsy, FNER helps differentiate between mild, moderate, and severe nerve involvement.
- Bell’s Palsy: FNER helps assess the severity and prognosis of Bell’s palsy by measuring the amplitude and latency of the evoked response. A reduced response suggests nerve damage.
- Facial Nerve Tumors: FNER can help localize tumors compressing the facial nerve by showing slowing or absence of responses.
- Trauma: Post-traumatic facial nerve damage can be assessed, differentiating between neuropraxia (temporary conduction block) and axonotmesis (axonal damage).
- Surgical Planning & Monitoring: FNER is used before and after surgery to evaluate the facial nerve’s health and guide surgical decisions.
FNER helps clinicians objectively quantify facial nerve function, leading to more accurate diagnoses and better treatment strategies.
Q 10. How would you differentiate between axonal and demyelinating lesions using FNER?
FNER can differentiate between axonal and demyelinating lesions based on the characteristics of the evoked response.
- Axonal Lesions: In axonal lesions (damage to the nerve fibers themselves), the amplitude of the FNER response will be significantly reduced or absent, while latency might be relatively normal or slightly prolonged. This is because fewer nerve fibers are functioning to generate a response.
- Demyelinating Lesions: In demyelinating lesions (damage to the myelin sheath surrounding the nerve fibers), the amplitude might be relatively preserved, but the latency will be significantly prolonged. This is because the myelin sheath is crucial for rapid signal conduction, and its damage slows the transmission of electrical impulses.
Therefore, a reduced amplitude with a relatively normal latency strongly suggests axonal damage, while a prolonged latency with a relatively normal amplitude indicates demyelination. However, it’s important to note that these are not always clear-cut distinctions, and complex lesions might show a combination of these findings.
Q 11. Describe the role of FNER in pre- and post-surgical evaluation of facial nerve function.
FNER plays a vital role in both pre- and post-surgical evaluation of facial nerve function.
Pre-surgical Evaluation: FNER helps assess the baseline function of the facial nerve before procedures like acoustic neuroma removal or parotid gland surgery, which may involve the facial nerve. This establishes a benchmark against which postoperative recovery can be measured.
Post-surgical Evaluation: Postoperatively, serial FNER studies monitor the recovery of facial nerve function. Improved amplitude and latency indicate a positive response to the surgery. Conversely, a lack of improvement or worsening of results can indicate complications or nerve damage that requires further intervention. FNER helps guide decisions on rehabilitation strategies and prognosis.
In essence, FNER acts as a valuable tool for surgeons to plan their approach, monitor the impact of their interventions, and optimize postoperative management.
Q 12. Discuss the limitations of FNER in assessing facial nerve function.
While FNER is a valuable diagnostic tool, it does have limitations.
- Technical Challenges: Obtaining a good quality recording can be challenging due to factors like patient cooperation, electrode placement, and interference from muscle artifacts. This is particularly true in patients with significant muscle spasms or limited mobility.
- Interpretation Complexity: Interpretation of FNER results can be subjective and requires considerable expertise. Abnormal findings must always be correlated with the clinical picture.
- Limited Sensitivity to Mild Lesions: FNER might not detect very mild or subtle lesions affecting the facial nerve; other electrophysiological techniques or imaging modalities might be needed.
- Absence of Anatomical Specificity: FNER can show that a lesion exists, but it often doesn’t specify the exact anatomical location within the facial nerve pathway without being complemented by other imaging tests like MRI.
Therefore, FNER results should be considered in conjunction with the patient’s clinical presentation, other diagnostic tests, and the clinical judgment of the physician.
Q 13. How do you interpret abnormal FNER findings in the context of clinical presentation?
Interpreting abnormal FNER findings requires careful consideration of the clinical presentation. For instance, a prolonged latency with a reduced amplitude in a patient presenting with symptoms of Bell’s palsy would suggest significant axonal damage, possibly indicating a poor prognosis for spontaneous recovery. In contrast, a prolonged latency with a preserved amplitude might suggest a primarily demyelinating process, often associated with a better potential for recovery.
The clinical picture provides the context for the electrophysiological data. For example, a patient with a history of trauma and a completely absent FNER response would strongly suggest a complete nerve transection, while the same finding in a patient with a slowly progressive facial weakness might raise concerns about a tumor compressing the nerve. The interaction between clinical findings and FNER results is critical for accurate diagnosis and management.
Q 14. What are the ethical considerations involved in conducting FNER studies?
Ethical considerations in conducting FNER studies are primarily related to patient safety and informed consent.
- Informed Consent: Patients must be fully informed about the procedure, including its purpose, risks (e.g., minor discomfort from electrical stimulation, skin irritation at electrode sites), and benefits. They should be given the opportunity to ask questions and withdraw their consent at any time.
- Patient Safety: Appropriate safety precautions should be taken to minimize any risks associated with electrical stimulation. The intensity of the stimulation should be carefully adjusted to ensure patient comfort.
- Data Confidentiality: FNER results, like any other medical information, must be kept confidential and handled in accordance with relevant privacy regulations.
- Competent Personnel: The procedure should be performed by trained and qualified professionals who are competent in the interpretation of FNER results.
By adhering to these ethical principles, clinicians can ensure that FNER studies are conducted responsibly and ethically, safeguarding the well-being and rights of their patients.
Q 15. Explain the technical aspects of FNER equipment setup and calibration.
Setting up for a Facial Nerve Evoked Response (FNER) study involves meticulous attention to detail. The equipment typically includes:
- Stimulator: A device delivering brief electrical pulses to the facial nerve. Calibration ensures consistent pulse amplitude and duration, usually measured in milliamperes (mA) and microseconds (µs). We need to verify its output using a calibrated oscilloscope to ensure accurate stimulation intensity. Too low, and we might not elicit a response; too high, and we risk discomfort or even injury.
- Electrodes: Surface electrodes are placed strategically on the face (near the stylomastoid foramen, for example) to record the evoked responses. Proper placement is crucial for signal quality. Impedance should be checked and maintained below 5 kΩ to minimize artifacts. We use conductive gel to enhance signal transmission.
- Amplifier: This increases the amplitude of the weak electrical signals generated by the nerve. It needs to be carefully calibrated to avoid signal distortion and noise amplification. A crucial step here is setting the amplifier’s gain and filter settings to effectively isolate the FNER signals from background noise.
- Computer system and software: This system digitally records, averages, and analyzes the evoked responses. Calibration involves verifying the correct sampling rate and ensuring proper signal representation. Incorrect settings could lead to misinterpretations.
Calibration procedures usually involve using known input signals to verify the accurate performance of each component of the system and ensure that the entire system produces accurate and reliable measurements. Regular checks are necessary to maintain optimal performance.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the patient preparation and positioning for an FNER study.
Patient preparation for FNER is key. First, a detailed explanation of the procedure is provided to alleviate anxiety. The patient should be comfortably seated or supine, their head supported to minimize movement artifacts. The area of stimulation and recording is then cleaned using an alcohol swab. The facial nerve is generally stimulated at the stylomastoid foramen, and electrodes are placed on the face and mastoid process according to a standardized montage (e.g., using a standard 10-20 system adapted for facial nerve recording). We instruct the patient to remain still during the test. Clear communication throughout the process is crucial. For example, I’d explain that they might experience slight tingling or twitching around the face during stimulation—this is normal. However, significant discomfort should be immediately reported.
Q 17. How do you ensure patient comfort and safety during FNER testing?
Patient comfort and safety are paramount. We start by clearly explaining the procedure, addressing any concerns. Stimulation intensity is carefully adjusted; it should be sufficient to evoke a response but not cause discomfort. We monitor the patient closely throughout the testing to observe for any adverse reactions. If the patient reports discomfort, we immediately reduce the stimulation intensity or pause the testing. Adequate breaks are provided if needed. Good communication and empathy significantly contribute to a positive experience.
For instance, if a patient expresses anxiety, I might use relaxation techniques, offer a comforting blanket, or simply chat with them to distract them during the test. A positive and calm atmosphere is as important as the technical aspect of the testing.
Q 18. Discuss the quality control measures used in FNER recording and analysis.
Quality control is essential for reliable results. We start with visual inspection of the recorded waveforms to identify artifacts such as eye blinks or muscle movements. We use averaging techniques to improve the signal-to-noise ratio, enhancing the clarity of the actual FNER responses. Regular checks on electrode impedance, stimulus output, and amplifier gain are performed throughout the study. A well-defined quality control checklist should be followed to ensure consistency and accuracy of the data. The use of a standardized methodology reduces variability between studies and increases the reliability of results.
For example, if we observe excessive noise in the recordings, we may check electrode placement, adjust the amplifier settings, or even repeat the stimulation. Consistent adherence to these protocols ensures high-quality data that is reliable and allows for accurate interpretation.
Q 19. What software packages are commonly used for FNER data analysis?
Several software packages are used for FNER data analysis. Examples include commercially available electrodiagnostic software like Neuro-MEP or specialized packages designed for evoked potential studies. These packages allow for waveform averaging, latency and amplitude measurements, and often offer advanced features like artifact rejection and statistical analysis tools.
The choice of software depends on the specific needs of the lab and the research questions being addressed. However, it’s crucial that any package used meets clinical standards for accuracy and reliability.
Q 20. How do you interpret FNER results in the presence of other neurological disorders?
Interpreting FNER results in the presence of other neurological disorders requires careful consideration. The results might be affected by factors such as demyelination (as seen in multiple sclerosis), axonal damage (as in peripheral neuropathies), or medication effects. A thorough clinical history and neurological examination are essential. We must correlate the FNER findings with other clinical and electrophysiological data to arrive at a comprehensive diagnosis.
For example, if we observe prolonged latencies in an FNER study of a patient with a history of multiple sclerosis, this finding needs to be interpreted in context. It’s not just the FNER result we consider. The patient’s clinical presentation, MRI scans, and other electrophysiological findings also factor into our overall interpretation. A purely isolated FNER abnormality might not be diagnostic.
Q 21. What are the potential complications associated with FNER testing?
While generally safe, FNER testing does carry some potential complications, although these are rare. The most common is discomfort during stimulation, which can usually be managed by adjusting the stimulation intensity. In rare cases, minor skin irritation at the electrode sites may occur. Significant complications are extremely uncommon and usually associated with improper technique. It’s crucial to carefully screen patients for conditions that might increase the risk of complications, such as bleeding disorders or skin infections, before proceeding with the test. Thorough patient education and meticulous technique are vital for ensuring safety.
Q 22. How do you interpret FNER results in children compared to adults?
Interpreting Facial Nerve Evoked Response (FNER) results in children differs from adults primarily due to developmental variations in the facial nerve and its conduction properties. In children, the facial nerve is still maturing, leading to potentially lower amplitude responses and longer latencies compared to adults. We also need to consider that smaller children might have difficulty maintaining stillness during the test, resulting in more artifact in the recordings. We often use age-adjusted normative data, meaning we compare the child’s results to a database of FNER results specifically collected from children of similar age groups. This is crucial because a response that might be considered abnormal in an adult might be perfectly normal in a young child. We also need to be mindful of the possibility of incomplete myelination and the influence of factors like medication, illness, and developmental stage. For instance, a child with an infection might exhibit delayed latencies that would resolve after recovery. Therefore, a longitudinal approach, where we monitor the FNER responses over time, is valuable in assessing true neurological injury as opposed to temporary physiological fluctuations.
Q 23. What is the role of FNER in monitoring the recovery of facial nerve function following injury?
FNER plays a crucial role in objectively monitoring facial nerve recovery following injury, such as from Bell’s palsy or trauma. By repeatedly measuring the electrical responses of the facial nerve, we can track the changes in nerve conduction velocity and amplitude over time. Improvements in these parameters indicate that the nerve is regenerating and recovering. For example, let’s say a patient with Bell’s palsy has an initial FNER showing absent responses. As the nerve heals, subsequent FNERs may reveal an increasing amplitude, indicating improved nerve function and suggesting the return of voluntary movement. The serial monitoring allows for a more precise evaluation of recovery compared to solely relying on clinical examination, which can be subjective. We can even use the FNER to guide decisions regarding interventions like surgery or corticosteroids. If the FNER shows little to no improvement despite treatment, this information can be used to adapt management strategies. In essence, FNER provides quantitative data which improves our understanding of recovery and helps us to personalize patient care.
Q 24. Describe the role of FNER in research settings.
In research settings, FNER contributes significantly to our understanding of facial nerve physiology and pathology. It’s a valuable tool for investigating the effects of various treatments, such as steroids or surgical decompression, on nerve regeneration. For instance, researchers might compare the FNER results of patients treated with different therapies to determine which is most effective in restoring facial nerve function. Furthermore, FNER can be used in pre-clinical studies on animal models to evaluate the efficacy of new drugs or surgical techniques before they’re used in human trials. Beyond treatment efficacy, FNER helps researchers understand the underlying mechanisms of facial nerve disorders. By analyzing the changes in nerve conduction parameters, researchers can gain insights into the nature and extent of nerve damage. The potential for high-resolution data analysis, combined with technological advances allowing more precise measurements and data processing, makes FNER a powerful research tool.
Q 25. Discuss the latest advancements in FNER technology and techniques.
Recent advancements in FNER technology include improvements in electrode design for better signal acquisition, minimizing artifacts. Advanced signal processing algorithms help to more effectively eliminate noise and isolate the true FNER responses. This leads to higher sensitivity and specificity in detecting subtle changes in nerve function. There’s also a move towards using more sophisticated stimulus patterns to elicit more information-rich responses from the nerve. This can include varying stimulus intensity and frequency, to explore a wider range of nerve fiber conduction properties. The integration of machine learning techniques allows for automated analysis of FNER data, increasing the efficiency and accuracy of interpretation. This also helps to create more robust normative databases, further enhancing the reliability of comparisons across patients and studies. Finally, portable FNER devices are being developed, allowing for more convenient testing in a variety of settings, improving access and making the technology more widely available.
Q 26. Compare and contrast FNER with other methods of assessing facial nerve function.
FNER offers a more objective and quantitative assessment of facial nerve function compared to methods relying on subjective clinical examination. While clinical exams assess muscle movement visually, FNER directly measures nerve conduction, revealing subtle changes missed by observation. Electromyography (EMG) is another technique examining muscle activity, but it focuses on the muscle response rather than the nerve itself. FNER complements EMG, with EMG providing information on the end-organ, while FNER provides information on the nerve’s integrity. For example, EMG might show muscle denervation, while FNER could pinpoint the location and severity of the nerve damage. Other methods include assessing the House-Brackmann grading scale, a subjective clinical score; however, this scale is not as sensitive to subtle changes in nerve function as FNER. The key difference lies in the level of assessment—FNER provides physiological data, while clinical evaluations and EMG primarily assess functional outcomes.
Q 27. How do you determine the appropriate number of trials for a reliable FNER study?
Determining the appropriate number of trials for a reliable FNER study involves a balance between achieving sufficient statistical power and minimizing testing time. We typically aim for a minimum number of trials to ensure the signal is distinguishable from background noise. Factors influencing the necessary number of trials include the expected signal-to-noise ratio, the variability within the patient population, and the desired statistical power. Smaller trials might suffice when dealing with a homogenous population with a strong expected signal, while larger trials are needed for populations with greater variability or expected weaker signals. This often entails performing a power analysis before starting the study to estimate the number of trials required to detect a clinically significant difference between groups with a specified level of confidence (e.g., 80% power, 5% significance level). Furthermore, we should consider practical factors, including participant fatigue and potential discomfort during prolonged testing, when determining the number of trials.
Q 28. How would you explain complex FNER results to a patient and their family?
Explaining complex FNER results requires careful consideration of the patient’s and family’s understanding of medical concepts. I start by avoiding technical jargon, explaining that FNER is a test measuring the electrical activity of the facial nerve to assess its health. I then explain the key findings in simple terms. For instance, if the FNER shows a delayed response, I might say, “The test shows that the nerve signals are a little slower than normal, which could be due to some inflammation or damage.” If the amplitude is low, I might explain, “The signal is weaker than usual, suggesting the nerve may not be working as efficiently.” I use analogies to make the concepts easier to grasp; comparing the nerve to a wire carrying electrical signals, where slower speed and decreased strength indicate possible issues. I ensure they understand that FNER findings contribute to the overall diagnosis and treatment plan but don’t represent the entire picture. I also explain the next steps in their care, emphasizing the collaborative nature of treatment, emphasizing hope and appropriate expectations based on their specific FNER findings and overall clinical picture. Open communication, using simple language and visual aids if necessary, ensures better understanding and alleviates patient anxiety.
Key Topics to Learn for Facial Nerve Evoked Response Interview
- Electrophysiology Principles: Understand the underlying principles of nerve conduction studies and evoked potentials, including the generation and propagation of action potentials.
- Facial Nerve Anatomy and Physiology: Demonstrate a thorough knowledge of the facial nerve’s pathway, branches, and function. Be prepared to discuss its relationship to other cranial nerves.
- FNER Methodology: Master the technical aspects of performing FNER testing, including stimulus placement, electrode placement, and data acquisition. Understand different recording techniques and their advantages/disadvantages.
- Waveform Interpretation: Develop proficiency in interpreting FNER waveforms. Be able to identify normal and abnormal patterns, and correlate findings with potential pathologies.
- Clinical Applications: Discuss the clinical utility of FNER in diagnosing various conditions affecting the facial nerve, such as Bell’s palsy, acoustic neuroma, and other facial nerve lesions.
- Differential Diagnosis: Be prepared to discuss how FNER findings contribute to the differential diagnosis of facial nerve disorders and distinguish them from other neurological conditions.
- Limitations and Artifacts: Understand the limitations of FNER and potential sources of artifacts that can affect test interpretation. Be able to critically evaluate the reliability of FNER results.
- Emerging Technologies: Familiarize yourself with advancements in FNER technology and techniques, and their impact on clinical practice.
Next Steps
Mastering Facial Nerve Evoked Response significantly enhances your expertise in neurophysiology and opens doors to specialized roles in clinical neurophysiology labs, research facilities, and academic institutions. A strong foundation in FNER is highly valued by employers seeking skilled and knowledgeable professionals.
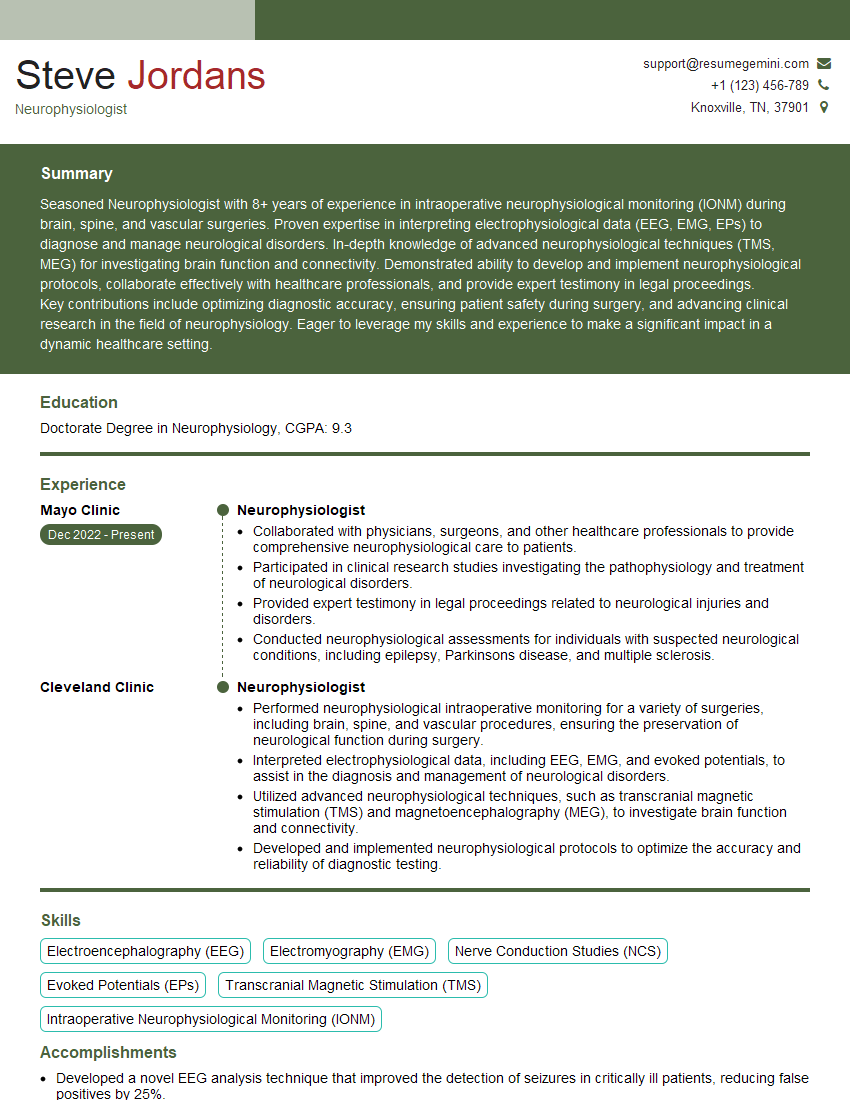
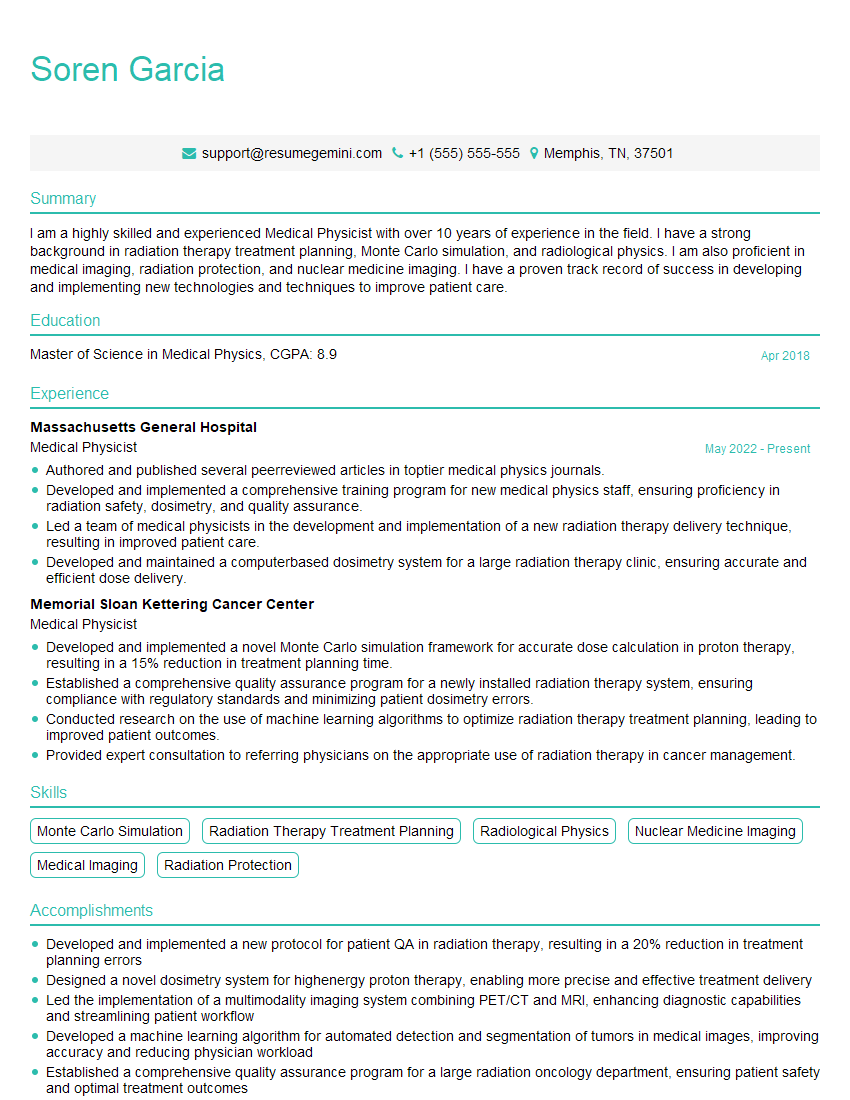
To maximize your job prospects, it’s crucial to present your skills effectively. Building an ATS-friendly resume is essential for getting your application noticed by recruiters and hiring managers. ResumeGemini is a trusted resource that can help you create a compelling and effective resume tailored to highlight your FNER expertise. Examples of resumes tailored to Facial Nerve Evoked Response are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.