Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Gerontology Counseling interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Gerontology Counseling Interview
Q 1. Describe your experience working with individuals experiencing age-related cognitive decline.
My experience working with individuals experiencing age-related cognitive decline is extensive. I’ve worked with patients across the spectrum of cognitive impairment, from mild cognitive impairment (MCI) to advanced dementia. My approach is always person-centered, focusing on the individual’s strengths and remaining abilities. This involves carefully assessing their current cognitive function, understanding their past life and interests, and tailoring interventions to maximize their quality of life. For example, I worked with a patient experiencing early-stage Alzheimer’s who was a talented gardener. We incorporated gardening activities into our sessions, adapting the tasks to her changing abilities and maintaining a sense of purpose and accomplishment. This contrasted sharply with another patient in the later stages who benefited most from calming, sensory-based activities. The key is flexibility and constant reassessment of their needs.
I often work closely with caregivers to provide education and support, ensuring that the patient receives consistent and compassionate care. This includes strategies for communication, safety, and maintaining a stimulating but supportive environment.
Q 2. Explain your understanding of the different stages of dementia and how you would adapt your counseling approach to each stage.
Dementia is an umbrella term encompassing several progressive neurocognitive disorders. Understanding the different stages is crucial for adapting counseling approaches. These stages are generally described as mild, moderate, and severe, although the progression varies significantly among individuals.
- Mild Stage: In this stage, individuals may experience subtle memory lapses, difficulty with complex tasks, and changes in personality. Counseling focuses on education, support for caregivers, and strategies for maintaining independence. This could involve memory aids, organizing routines, and problem-solving techniques.
- Moderate Stage: As the disease progresses, more significant cognitive impairments emerge. Individuals may need more assistance with daily activities, experience increased confusion, and have difficulty with communication. Counseling shifts to focus on emotional support for both the patient and their family, promoting adaptive coping mechanisms, and utilizing simple, clear communication strategies.
- Severe Stage: In the advanced stages, individuals require extensive care and support, their ability to communicate may be severely limited, and they experience significant memory loss. Counseling focuses on providing comfort and emotional support to the patient and family, managing challenging behaviors, and facilitating peaceful end-of-life care. Often, non-verbal communication and sensory stimulation become paramount.
Throughout all stages, my approach prioritizes respect, empathy, and a holistic understanding of the individual’s unique circumstances. Regular reassessment and flexibility are essential in adapting interventions to meet their ever-changing needs.
Q 3. How would you address the emotional needs of a patient facing end-of-life care?
Addressing the emotional needs of a patient facing end-of-life care is profoundly important. This involves creating a safe and supportive space where they can express their fears, anxieties, regrets, and hopes. Active listening, validation of their feelings, and unconditional positive regard are fundamental. I work to help them find meaning and purpose in their remaining time, exploring their spiritual or religious beliefs, and fostering connections with loved ones.
Practical strategies include reminiscence therapy, helping them create a legacy or life review, and assisting in advanced care planning. It is crucial to acknowledge the patient’s autonomy and preferences regarding end-of-life decisions, working collaboratively with the patient, their family, and the healthcare team.
A significant part of my role involves supporting the family during this difficult period. This includes providing education about the dying process, coping strategies for grief and loss, and facilitating family discussions around end-of-life care choices.
Q 4. Outline your approach to working with families of elderly patients.
Working with families of elderly patients requires sensitivity and a collaborative approach. I view the family as an integral part of the care team. My initial sessions often involve family meetings to assess the family dynamics, understand their concerns, and collaboratively develop realistic goals for care. I offer education on age-related changes, coping strategies for dealing with challenging behaviors, and practical techniques for providing care. I facilitate open communication within the family, promoting mutual support and understanding.
I also recognize the emotional toll caregiving can take on family members. I provide support groups, individual counseling, and resources for respite care. The focus is on empowering family members to care for themselves while also providing the best possible care for their loved one.
For instance, I’ve facilitated family meetings where siblings have conflicting ideas about care options. By creating a safe space for open discussion and helping them understand each other’s perspectives, we’ve collaboratively developed a plan that meets the patient’s needs while respecting family dynamics.
Q 5. Explain your knowledge of relevant legislation protecting the rights of the elderly.
My knowledge of relevant legislation protecting the rights of the elderly is thorough. I am familiar with laws addressing elder abuse, neglect, and exploitation, including mandatory reporting requirements. I understand the legal framework around advance directives, such as living wills and durable powers of attorney for healthcare, ensuring patients’ wishes are respected and honored. I am also knowledgeable about legislation related to long-term care facilities, including regulations pertaining to resident rights and quality of care. This understanding ensures I can advocate effectively for my patients and educate their families on their legal rights and protections.
For example, I am aware of the differences in state and federal laws regarding mandatory reporting of elder abuse and how those legal parameters influence my actions and responsibilities in specific situations. My familiarity with the Patient Self-Determination Act is critical to ensuring informed consent and respect for individual autonomy.
Q 6. How would you handle a situation where a patient is refusing necessary medical treatment?
When a patient refuses necessary medical treatment, a careful and nuanced approach is crucial. It’s important to first understand the reasons behind their refusal. This might involve exploring their fears, concerns, and beliefs. Respect for patient autonomy is paramount. I would engage in open and empathetic communication, exploring their understanding of the treatment, potential benefits and risks, and alternative options.
If the refusal poses a significant risk to their health and safety, I would collaborate with the medical team and the patient’s family to develop a plan that balances their autonomy with their well-being. This may involve involving other healthcare professionals, such as a psychiatrist or ethicist, to further assess the situation and explore options for ensuring the patient’s safety while respecting their choices.
Documentation of the entire process is critical, ensuring a clear record of the discussions, the patient’s decision-making capacity, and any collaborative efforts undertaken.
Q 7. Describe your experience in developing and implementing care plans for elderly individuals.
Developing and implementing care plans for elderly individuals is a collaborative process involving the patient, family, and healthcare team. My approach begins with a thorough assessment of the patient’s physical, cognitive, emotional, and social needs. This involves gathering information from medical records, interviews, and observations. The care plan is then developed collaboratively, focusing on realistic and achievable goals. It outlines specific interventions, timelines, and strategies for monitoring progress.
Care plans are not static; they are regularly reviewed and updated as the patient’s needs change. I use various methods for monitoring progress, including regular check-ins with the patient and family, review of medical records, and assessments of functional ability. This iterative process ensures that the plan remains relevant and effective, promoting the patient’s well-being and quality of life.
For example, a care plan for a patient with mobility limitations might include physical therapy, occupational therapy, assistive devices, and home modifications. Regular reassessments would adjust the plan to account for any changes in the patient’s condition, ensuring the interventions remain appropriate and effective.
Q 8. How would you identify and address potential elder abuse or neglect?
Identifying and addressing elder abuse or neglect requires a multifaceted approach, combining keen observation, skillful questioning, and a thorough understanding of the signs. Elder abuse encompasses physical, emotional, financial, and neglect. Neglect, a form of abuse, involves the failure to provide necessary care or protection.
My approach begins with building trust and rapport. I’d carefully observe the elder for physical signs like unexplained bruises, injuries, or malnutrition. I would also look for behavioral indicators such as withdrawal, fear, anxiety, or changes in personality.
I would then conduct a thorough assessment, asking open-ended questions about their living situation, relationships, and financial management. I’d be sensitive to the power dynamics involved, ensuring the elder feels safe to disclose any abuse. If suspicions are raised, I would document my observations meticulously and report my concerns to the appropriate authorities, such as Adult Protective Services, following mandated reporting guidelines.
For instance, if an elderly client consistently shows up with unexplained bruises and expresses fear of a caregiver, I would immediately escalate the situation. Similarly, if I notice significant weight loss or poor hygiene despite adequate resources, I would investigate potential neglect. The key is a proactive and collaborative approach, involving other healthcare professionals and social workers when necessary to ensure the elder’s safety and well-being.
Q 9. Explain your understanding of the various types of long-term care facilities and their suitability for different needs.
Long-term care facilities offer a range of services catering to diverse needs. The most common types include:
- Nursing Homes (Skilled Nursing Facilities): Provide 24-hour medical care for individuals needing significant assistance with daily activities and medical treatments. Suitable for those with chronic conditions requiring intensive care, such as Alzheimer’s disease in advanced stages or after major surgery.
- Assisted Living Facilities: Offer personal care assistance with activities like bathing, dressing, and medication management, along with social activities and supportive services. Best suited for individuals who need help with some daily tasks but don’t require 24-hour medical supervision.
- Independent Living Facilities: Provide housing and amenities tailored to active seniors who want a supportive community environment but can manage their daily needs independently. This is ideal for those who want social interaction and convenience but still retain their autonomy.
- Continuing Care Retirement Communities (CCRCs): Offer a range of services from independent living to skilled nursing care within one location. These are best for individuals who anticipate needing a continuum of care as their health changes over time. The ability to transition seamlessly within the same community offers great peace of mind.
Selecting the right facility involves a comprehensive assessment of the individual’s physical, cognitive, and social needs. Factors such as the level of medical care required, the person’s personality, and financial resources should be carefully considered. Engaging the family and the elder in the decision-making process is crucial for a positive outcome.
Q 10. How would you assess the psychosocial needs of an elderly patient?
Assessing the psychosocial needs of an elderly patient requires a holistic approach, integrating several assessment tools and methods. It’s not just about physical health but also understanding their emotional, cognitive, and social well-being.
My assessment would begin with a thorough interview, employing active listening techniques to understand their life story, current challenges, and support systems. I would use standardized questionnaires and scales, like the Geriatric Depression Scale or the Mini-Mental State Examination (MMSE), to screen for cognitive impairment and mental health issues.
Furthermore, I would observe their behavior during interactions, assessing their mood, affect, and overall engagement. This also includes considering their social network – the quality and frequency of contact with family and friends. Any indication of social isolation or loneliness would be a key area of concern. Finally, I would explore their coping mechanisms, resilience, and overall sense of purpose and meaning in life.
For example, a client expressing feelings of isolation and hopelessness might require referral to social groups or counseling. Someone with memory problems might benefit from cognitive stimulation activities and supportive care. A personalized approach, tailored to the individual’s unique circumstances, is vital for effective intervention.
Q 11. Describe your experience in grief and loss counseling in the elderly population.
Grief and loss counseling with the elderly presents unique challenges and rewards. Older adults often experience multiple losses concurrently— loss of loved ones, health, independence, and social roles. This accumulation of losses can be profoundly impactful.
My approach emphasizes empathy, active listening, and validation of their feelings. I recognize that grief is not linear; it’s a highly individualized process. I use a variety of therapeutic techniques tailored to the client’s needs, such as reminiscence therapy (exploring positive memories), life review (examining life experiences to find meaning), and narrative therapy (helping them construct a coherent story of their life).
One particularly challenging case involved a client grieving the loss of her spouse after 60 years of marriage. Through reminiscence therapy, we explored their shared memories, celebrating their love story and fostering a sense of continuity. It highlighted the importance of acknowledging the unique aspects of grief in later life, understanding that the loss resonates deeply within the context of their lived experiences.
Q 12. How do you maintain professional boundaries while building rapport with elderly clients?
Maintaining professional boundaries while building rapport with elderly clients is a delicate balance. While warmth and empathy are essential, it’s crucial to avoid blurring the professional relationship.
I achieve this through clear communication, establishing the therapeutic contract early in the therapeutic process which outlines the roles, responsibilities, and limits of the relationship. I avoid dual relationships, such as socializing outside of therapy sessions or accepting gifts that could be perceived as compromising my objectivity. I adhere strictly to confidentiality rules, maintaining appropriate professional distance while remaining compassionate and understanding.
For example, a client might offer a heartfelt gift of baked goods. I’d graciously express appreciation, but reiterate my professional boundaries, explaining that gifts could complicate our therapeutic relationship. Similarly, I’d maintain professional demeanor, avoiding overly familiar language or actions while still conveying genuine care and respect for their experiences.
Q 13. How familiar are you with different types of assistive devices and technologies for the elderly?
My familiarity with assistive devices and technologies for the elderly is extensive. This knowledge is critical in empowering older adults to maintain independence and quality of life.
I’m knowledgeable about a wide range of devices, including mobility aids (walkers, canes, wheelchairs), hearing aids, visual aids (magnifying glasses, large-print materials), medication reminders, telehealth systems, and assistive technologies for daily living (adaptive eating utensils, grab bars).
I also understand the importance of considering the individual’s needs and preferences when recommending assistive technology. A thorough assessment of their functional abilities, cognitive status, and living environment is crucial for selecting the most appropriate and user-friendly devices. I also provide training and support to ensure proper and safe usage. For example, I would assess a client’s mobility limitations before recommending a specific type of walker or wheelchair, taking into account factors like their strength, balance, and the terrain they navigate.
Q 14. Describe your understanding of ageism and how you mitigate its impact in your practice.
Ageism is a pervasive societal prejudice that negatively impacts older adults. It involves stereotyping and discrimination based on age, often leading to reduced opportunities, social exclusion, and diminished self-esteem.
In my practice, I actively combat ageism by promoting a person-centered approach that emphasizes individual strengths and capabilities, rather than relying on age-based stereotypes. I challenge ageist language and attitudes both in my interactions with clients and within broader professional settings.
For instance, I avoid making assumptions about cognitive abilities based solely on age, using appropriate assessment tools instead. I actively celebrate the wisdom and experience that older adults bring and promote their continued contributions to society. Education and awareness-raising about ageism among healthcare professionals and the wider community are crucial to fostering a more inclusive and equitable environment for all.
Q 15. What resources would you utilize to support an elderly patient and their family?
Supporting elderly patients and their families requires a multifaceted approach, drawing on a wide range of resources. My strategy centers around assessing individual needs and tailoring support accordingly. This includes:
Formal Support Systems: I would connect them with relevant agencies like Medicare, Medicaid, Social Security Administration, and local senior centers. These organizations offer crucial financial assistance, healthcare services, and social programs.
Community Resources: Accessing community-based services is vital. This could involve referring them to home healthcare agencies, adult day care centers, meal delivery services, or transportation assistance programs tailored to seniors’ mobility needs. For example, I might connect a family struggling with transportation to Meals on Wheels and a local senior transportation service.
Therapeutic Interventions: Depending on the patient’s needs, I might recommend individual or group therapy, focusing on areas such as grief counseling, coping with loss, or managing stress. Cognitive behavioral therapy (CBT) or other evidence-based approaches would be employed as appropriate.
Family Support and Education: A critical aspect is supporting the family. This involves educating them about the aging process, potential challenges, and available resources. Family therapy can strengthen family dynamics and improve communication, aiding in the patient’s overall well-being. I often facilitate family meetings to help address shared concerns and expectations.
Technology and Online Resources: I would explore the use of technology to improve access to information and support. This could involve recommending apps for medication reminders, telehealth appointments, or online support groups for both patients and caregivers.
The key is to create a personalized care plan, carefully considering the patient’s and family’s unique circumstances and preferences. It’s about empowering them to navigate the challenges of aging with dignity and resilience.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of the ethical considerations involved in gerontology counseling.
Ethical considerations in gerontology counseling are paramount. They revolve around the principles of autonomy, beneficence, non-maleficence, and justice. Specifically:
Respect for Autonomy: Older adults have the right to self-determination and making their own choices, even if those choices differ from what I might recommend. This includes respecting their wishes regarding treatment, lifestyle, and end-of-life care. For instance, if an elderly patient chooses not to pursue aggressive medical treatment, I must respect that decision.
Beneficence: I have a duty to act in the best interests of my clients. This means providing them with the most effective and compassionate care possible, always considering their individual needs and preferences. This could involve advocating for their rights or connecting them with additional support.
Non-Maleficence: I must avoid causing harm, both physical and psychological. This requires careful consideration of the potential risks and benefits of any interventions or recommendations. For example, I would carefully weigh the risks and benefits of medication before suggesting it.
Justice: All clients deserve fair and equitable access to care, regardless of their socioeconomic status, race, ethnicity, or other factors. This is especially crucial in gerontology counseling, where older adults may face disparities in access to healthcare and social services.
Confidentiality: Maintaining client confidentiality is of utmost importance, adhering to professional ethical guidelines and legal regulations. I would always obtain informed consent before sharing any information with third parties.
Navigating these ethical considerations requires careful reflection, consultation with colleagues, and a commitment to acting ethically in all aspects of my practice.
Q 17. How do you ensure confidentiality and client privacy in your practice?
Confidentiality and client privacy are cornerstones of my practice. I adhere strictly to the following:
HIPAA Compliance: I ensure complete compliance with the Health Insurance Portability and Accountability Act (HIPAA), safeguarding electronic health information (EHI) and personal health information (PHI). This includes secure storage of records, restricted access protocols, and adherence to data breach procedures.
Informed Consent: Before initiating any services, I obtain informed consent, thoroughly explaining the limits of confidentiality and any potential exceptions (e.g., mandated reporting of abuse).
Secure Record Keeping: All client records, both paper and electronic, are stored securely and only accessible to authorized personnel. I utilize password-protected electronic systems and locked filing cabinets for physical records.
Professional Boundaries: I maintain strict professional boundaries with my clients, avoiding dual relationships or situations that could compromise confidentiality. This includes avoiding personal contact outside of the therapeutic relationship.
Data Encryption and Disposal: I utilize data encryption for electronic records and follow secure disposal procedures for paper records, shredding them appropriately.
Client trust is essential; therefore, maintaining confidentiality is not merely a legal obligation, but a foundational aspect of building a strong therapeutic alliance.
Q 18. Describe a time you had to navigate a difficult ethical dilemma in your practice.
I once worked with an elderly patient who was experiencing significant cognitive decline and lacked capacity to make decisions about their own care. The family was deeply divided on the best course of action, with some advocating for placement in a nursing home and others preferring home care. This created a significant ethical dilemma: respecting the patient’s autonomy (to the extent possible), while also ensuring their safety and well-being.
My approach involved:
Careful Assessment: I thoroughly assessed the patient’s cognitive abilities and their expressed wishes (to the extent they could be understood). I also considered their physical health and support system at home.
Mediation and Family Meetings: I facilitated several family meetings, guiding them through respectful communication and helping them explore different options. The goal was to find common ground and a solution that best served the patient’s interests.
Legal Consultation: I consulted with a lawyer specializing in elder law to better understand the legal implications of decision-making for individuals lacking capacity. This provided guidance on guardianship or power of attorney options.
Collaboration with Other Professionals: I worked closely with the patient’s physician and social worker, developing a comprehensive care plan that balanced the family’s concerns with the patient’s best interests. Ultimately, the family reached a consensus on a plan that allowed for home care with enhanced support services.
This experience highlighted the importance of ethical decision-making in situations involving diminished capacity, emphasizing the need for collaboration, careful assessment, and respect for all involved parties.
Q 19. How do you stay up-to-date on current research and best practices in gerontology counseling?
Staying current in gerontology counseling requires ongoing professional development. My approach involves:
Professional Journals and Publications: I regularly read journals such as the “Journal of Gerontological Social Work,” “The Gerontologist,” and other relevant publications in the field of aging. I specifically seek out peer-reviewed articles on new therapies and research findings.
Conferences and Workshops: I actively attend professional conferences and workshops to learn about the latest research, best practices, and emerging trends in the field. This provides opportunities to network with other professionals and share insights.
Continuing Education Courses: I participate in continuing education courses to maintain my license and expand my knowledge. This ensures my skills remain updated, particularly in areas like neurocognitive disorders or palliative care.
Professional Organizations: I am a member of professional organizations such as the Gerontological Society of America (GSA), which provides access to resources, publications, and networking opportunities.
Online Resources: I utilize reputable online resources such as the National Institute on Aging (NIA) and other government websites for reliable information on aging-related topics.
Lifelong learning is essential in this ever-evolving field. By staying updated, I can provide my clients with the most effective and evidence-based interventions.
Q 20. Explain your experience in collaborating with interdisciplinary teams.
Interdisciplinary collaboration is vital in gerontology counseling. My experience encompasses working closely with:
Physicians: I regularly collaborate with physicians to ensure the patient’s medical and psychological needs are addressed comprehensively. For instance, I might work with a physician to manage medication side effects that are impacting a patient’s mental health.
Social Workers: Social workers provide invaluable support in navigating social services and resource allocation. Joint efforts can be critical in managing financial concerns, accessing home healthcare, or coordinating community resources.
Nurses: Nurses frequently play a vital role in the patient’s day-to-day care. Collaboration ensures that my counseling addresses their holistic needs, particularly when there are physical health complications.
Occupational Therapists and Physical Therapists: These therapists address functional limitations, and I integrate their recommendations into my counseling, addressing the psychological impact of physical challenges.
Pharmacists: Working with pharmacists helps to manage medication-related issues or address side effects that might interfere with the patient’s mental and emotional well-being.
Effective teamwork ensures comprehensive and patient-centered care, leading to better outcomes. Clear communication, regular meetings, and shared decision-making are key to successful interdisciplinary collaboration.
Q 21. How would you address a patient exhibiting signs of depression or anxiety?
Addressing depression or anxiety in an elderly patient requires a sensitive and comprehensive approach. My strategy involves:
Thorough Assessment: I begin with a comprehensive assessment to determine the severity of the symptoms, identifying potential contributing factors such as medical conditions, social isolation, or recent losses. This includes using standardized screening tools for depression and anxiety.
Differential Diagnosis: It’s crucial to rule out any underlying medical conditions that could be mimicking depression or anxiety. This often involves close collaboration with the patient’s physician.
Psychotherapy: Depending on the assessment findings, I might employ various therapeutic approaches, such as cognitive behavioral therapy (CBT), which helps patients identify and modify negative thought patterns and behaviors, or psychodynamic therapy, which explores unconscious conflicts contributing to mental health challenges. I might also incorporate supportive therapy to build resilience and coping mechanisms.
Medication Management: In cases where psychotherapy alone is insufficient, I would collaborate with the patient’s physician to consider medication options. This requires careful monitoring and management of side effects.
Social Support: Enhancing social support is vital. This could involve connecting the patient with support groups, encouraging social activities, and working with family members to foster a supportive environment.
Lifestyle Interventions: Lifestyle modifications, such as regular exercise, improved nutrition, and adequate sleep, can significantly improve mood and reduce anxiety. I work with the patient to implement realistic lifestyle changes.
The overall goal is to create a collaborative and empowering therapeutic relationship, fostering hope, and helping the patient regain a sense of purpose and well-being.
Q 22. Describe your approach to conducting thorough geriatric assessments.
A thorough geriatric assessment goes beyond simply checking vital signs. It’s a holistic evaluation considering the individual’s physical, cognitive, emotional, and social well-being. My approach involves a multi-faceted strategy:
- Comprehensive Health History: I begin by gathering a detailed medical history, including current medications, past illnesses, surgeries, and family history. This helps identify potential risk factors and underlying health conditions that may impact their current state.
- Physical Examination: A physical assessment is crucial to assess their functional abilities, such as mobility, dexterity, and balance. This informs care planning and identifies areas needing support. For instance, I might assess their ability to dress themselves or walk without assistance.
- Cognitive Assessment: I use standardized tests like the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) to evaluate cognitive function, including memory, attention, and executive function. This helps differentiate age-related cognitive changes from more serious conditions like dementia.
- Psychological Assessment: Understanding their emotional state, including mood, anxiety, and depression, is vital. I employ validated tools and engage in open-ended conversations to gauge their emotional wellbeing. This might involve identifying signs of depression masked by physical complaints.
- Social Assessment: This component focuses on their social support network, living situation, financial stability, and access to community resources. Knowing their social context is critical in determining their overall well-being and identifying potential support needs. For example, I would assess if they live alone, have family nearby, and if they have access to transportation for appointments.
- Functional Assessment: This assesses their ability to perform Activities of Daily Living (ADLs) like bathing, dressing, and eating, and Instrumental Activities of Daily Living (IADLs) like managing finances and medication. This assessment helps determine the level of assistance required.
By integrating these aspects, I build a comprehensive profile that allows for individualized care planning and intervention.
Q 23. How do you handle challenging communication situations with elderly patients with cognitive impairments?
Communicating with elderly patients experiencing cognitive impairment requires patience, understanding, and adaptation. My approach focuses on building rapport and utilizing effective communication strategies:
- Simplicity and Clarity: I use simple language, avoiding jargon or complex sentence structures. I break down information into smaller, manageable chunks. For example, instead of saying “Your medication regimen needs to be adjusted,” I might say, “Let’s talk about how to make your medicine easier to take.”
- Non-Verbal Communication: I pay close attention to nonverbal cues, such as body language and facial expressions, which can be more informative than verbal responses. Maintaining eye contact, using a calm and reassuring tone, and employing gentle touch (if appropriate) can significantly enhance communication.
- Environmental Modifications: Reducing distractions, ensuring good lighting, and using visual aids can enhance comprehension. A quiet space free from interruptions greatly improves the interaction.
- Validation and Empathy: I approach each interaction with empathy, acknowledging their feelings and experiences, even if I don’t fully understand them. This creates a safe space where they feel valued and respected.
- Structured Communication Techniques: Using techniques like reminiscing therapy or focusing on concrete topics they are familiar with can stimulate engagement and provide a point of connection. Engaging them with photos or familiar objects is often helpful.
- Collaboration with Caregivers: I involve family members or caregivers in the communication process, ensuring consistency and understanding across all interactions. Sharing information and developing strategies together is essential.
Remember, patience is paramount. Building trust takes time, and adapting to individual communication styles is essential.
Q 24. What are some common communication challenges you encounter with families of elderly clients?
Communication challenges with families of elderly clients are common and often stem from a variety of factors, including:
- Differing Perspectives on Care: Family members may have differing opinions on the best course of treatment or level of care needed, leading to conflict and tension. Some may advocate for aggressive interventions while others prefer a more conservative approach.
- Emotional Strain: Caring for an elderly parent can be emotionally draining, resulting in burnout and impacting communication dynamics. Understanding and acknowledging their emotional toll is crucial.
- Lack of Information and Understanding: Family members may lack knowledge about the aging process, specific conditions, or available resources, which can lead to misunderstandings and frustration. Providing clear, concise information is paramount.
- Role Conflicts: Family dynamics and power struggles can complicate decision-making processes, making consensus difficult to achieve. Facilitating open dialogue and mediating conflicting perspectives is often necessary.
- Guilt and Resentment: Feelings of guilt or resentment may arise due to the demands of caregiving or perceived inequities in responsibilities within the family. Addressing these underlying emotions in a safe and empathetic environment can aid resolution.
Addressing these challenges involves active listening, clear communication, empathy, and collaborative problem-solving. I often use family meetings to facilitate open communication and address concerns.
Q 25. How would you adapt your communication style to meet the specific needs of different elderly clients?
Adapting my communication style is fundamental to effective geriatric counseling. It involves recognizing that each individual has unique needs and preferences based on their personality, cognitive abilities, sensory impairments, and cultural background. This requires a flexible and personalized approach.
- Sensory Impairments: For individuals with hearing or vision loss, I adjust my communication accordingly. This might involve speaking clearly and slowly, using larger font sizes, or ensuring adequate lighting. The use of assistive devices is also carefully considered.
- Cognitive Impairments: As mentioned earlier, this requires simplified language, visual aids, and patience. I avoid abstract concepts and focus on concrete, relatable examples.
- Cultural Differences: I consider cultural beliefs, values, and communication styles when interacting with clients. Understanding their cultural background informs my approach and ensures sensitivity and respect.
- Personality Differences: Some individuals are more reserved, while others are outgoing. I adapt my communication style to their personality, creating a comfortable and safe environment.
- Emotional State: The client’s mood and emotional state greatly influence communication. If they are anxious or distressed, creating a calm and supportive environment is crucial.
Effective communication necessitates a genuine effort to understand and respect the individual’s unique needs and communication preferences.
Q 26. Explain your understanding of the biopsychosocial model in the context of geriatric care.
The biopsychosocial model is crucial in geriatric care. It acknowledges that an individual’s health and well-being are shaped by an intricate interplay of biological, psychological, and social factors. It moves beyond a purely medical model to encompass a more holistic view.
- Biological Factors: These encompass physical health conditions, genetic predispositions, physiological changes associated with aging (e.g., decreased muscle mass, reduced organ function), and the impact of chronic diseases.
- Psychological Factors: These include cognitive function, personality traits, emotional states (depression, anxiety), coping mechanisms, and mental health conditions.
- Social Factors: This includes social support networks, living arrangements, socioeconomic status, access to resources, cultural beliefs, and the impact of life events.
In practice, this means that when assessing an elderly client, I don’t just focus on their medical diagnosis. I also consider their mental health, coping abilities, social connections, and environmental influences. For example, an elderly person with arthritis (biological) might experience depression (psychological) due to social isolation (social), impacting their ability to manage their condition. Addressing all three factors is crucial for effective interventions.
Q 27. How do you advocate for the needs of your elderly patients within the healthcare system?
Advocating for my elderly patients requires a multi-pronged approach:
- Clear and Concise Communication: I clearly articulate their needs and concerns to healthcare providers, using precise and factual information. This ensures their voice is heard and understood.
- Collaboration with Healthcare Team: I work closely with doctors, nurses, and other healthcare professionals to ensure the best possible care for my clients. This includes participating in care plan meetings and advocating for specific interventions.
- Resource Navigation: I assist patients in accessing essential resources, such as home healthcare services, financial assistance, and community programs. This involves understanding the complex healthcare system and guiding clients through the process.
- Documentation: I meticulously document the client’s needs, care plans, and progress. This provides a clear record for healthcare professionals and facilitates continuity of care.
- Legal and Ethical Considerations: I am aware of legal and ethical guidelines concerning patient advocacy and ensure my actions uphold their rights and autonomy. This is especially important regarding informed consent and end-of-life care decisions.
- Patient Empowerment: My advocacy involves empowering the patient to participate actively in their care and decision-making process. This builds confidence and ensures their voice is heard.
Advocacy often involves navigating bureaucratic hurdles and championing the client’s needs within a system that can sometimes feel impersonal. My goal is to ensure that my clients receive the highest quality of care tailored to their individual circumstances.
Q 28. Describe your experience with crisis intervention in the context of gerontology counseling.
Crisis intervention in gerontology counseling often involves addressing urgent situations impacting the well-being of older adults. These situations might include:
- Suicidal Ideation: My immediate response involves assessing the level of risk, providing emotional support, and contacting emergency services or psychiatric professionals as needed. Ensuring safety is the primary concern.
- Abuse or Neglect: If I suspect abuse or neglect (physical, emotional, or financial), I follow mandated reporting procedures and cooperate with relevant authorities to ensure the client’s safety and protection.
- Acute Medical Crises: I assist clients in accessing appropriate medical care in emergencies, coordinating with their physicians or emergency services.
- Significant Life Changes: Significant life events, such as bereavement or sudden relocation, can trigger crises. I provide supportive counseling, help them adjust, and connect them with relevant resources.
- Behavioral Disturbances: In cases of sudden changes in behavior or acute confusion, I help determine the underlying cause and recommend appropriate interventions, such as medical evaluation or medication adjustment.
Crisis intervention requires rapid assessment, appropriate intervention, and coordination with other professionals to ensure the client’s immediate safety and well-being. It emphasizes quick action and resource mobilization.
Key Topics to Learn for Gerontology Counseling Interview
- Psychosocial Theories of Aging: Understanding Erikson’s stages, activity theory, and disengagement theory, and their application to counseling older adults.
- Cognitive and Physical Changes in Aging: Familiarize yourself with common age-related cognitive impairments (e.g., dementia, Alzheimer’s disease) and physical limitations, and how they impact counseling approaches.
- Loss and Grief Counseling: Mastering techniques for addressing grief, loss, and bereavement in older adults, including anticipatory grief and the unique challenges faced by this population.
- Ethical Considerations in Gerontology Counseling: Understanding issues like informed consent, confidentiality, capacity, and end-of-life decision-making within the context of geriatric care.
- Family Systems and Intergenerational Dynamics: Recognizing the influence of family relationships and intergenerational dynamics on the mental health and well-being of older adults.
- Practical Application: Case Study Analysis: Be prepared to discuss how you would approach specific case scenarios involving older adults facing various challenges (e.g., depression, social isolation, adjusting to retirement).
- Cultural Sensitivity and Diversity: Demonstrate awareness of the diverse needs and experiences of older adults from various cultural backgrounds and socioeconomic statuses.
- Assessment and Intervention Strategies: Understand various assessment tools and therapeutic interventions specifically designed for older adults, including evidence-based practices.
- Collaboration and Teamwork: Highlight your ability to collaborate effectively with other healthcare professionals, family members, and caregivers involved in the care of older adults.
- Advocacy and Resources: Demonstrate knowledge of available resources and support systems for older adults and their families, and your ability to advocate for their needs.
Next Steps
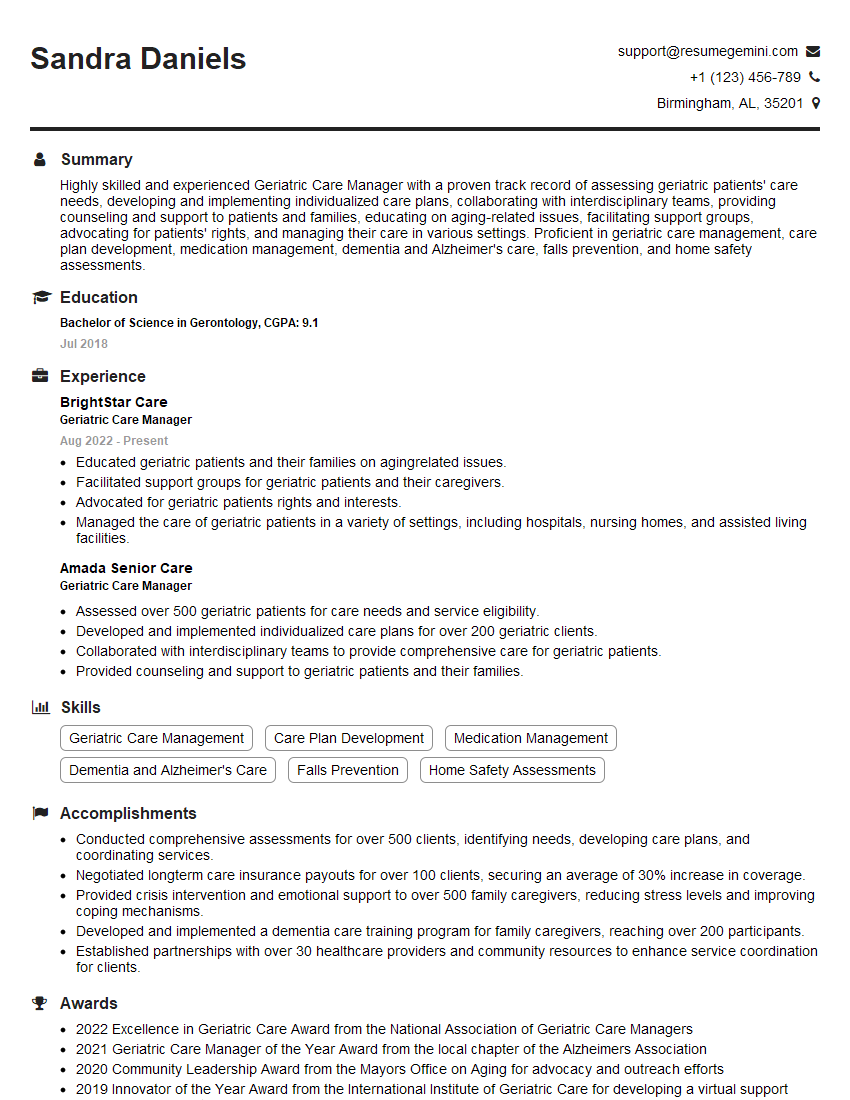
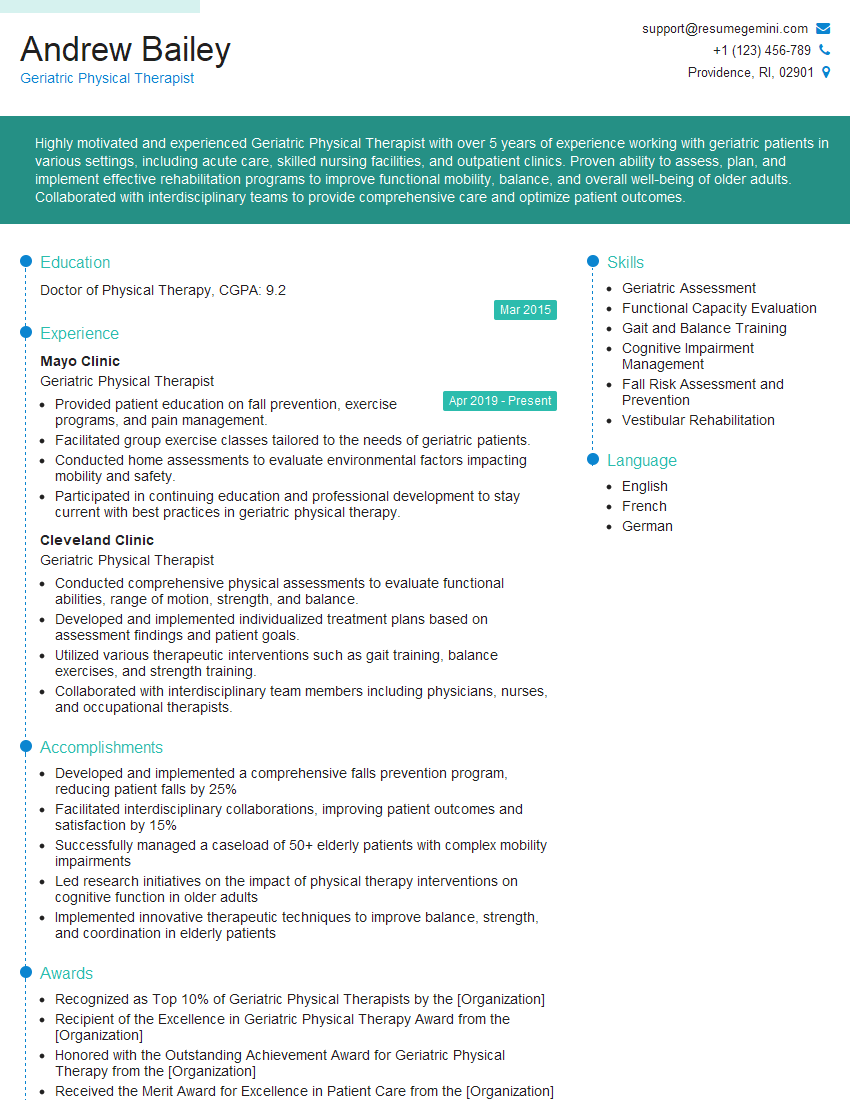
Mastering Gerontology Counseling opens doors to a rewarding career helping a vulnerable and deserving population. This specialized knowledge is highly sought after, leading to diverse opportunities and career advancement. To significantly improve your job prospects, focus on building an ATS-friendly resume that showcases your skills and experience effectively. ResumeGemini is a trusted resource to help you create a professional and impactful resume. They provide examples of resumes tailored to Gerontology Counseling to guide you, ensuring your qualifications shine.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.