Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Gout Management interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Gout Management Interview
Q 1. Explain the pathophysiology of gout.
Gout is a form of inflammatory arthritis caused by a buildup of uric acid crystals in the joints. This happens because the body produces too much uric acid, or the kidneys don’t excrete it efficiently enough. Uric acid is a byproduct of the breakdown of purines, substances found naturally in the body and in certain foods. When uric acid levels become too high (hyperuricemia), it crystallizes, forming needle-like structures that deposit in the joints, typically the big toe, but also in other joints like the knees, ankles, and hands. This crystal deposition triggers an intense inflammatory response, leading to the characteristic pain, swelling, and redness of a gout attack.
Think of it like this: imagine uric acid as tiny, sharp shards of glass. When these shards accumulate in a joint, they irritate the lining of the joint, causing inflammation and the painful symptoms of gout. The body’s immune system reacts to these crystals as if they are foreign invaders, further exacerbating the inflammation.
Q 2. Describe the diagnostic criteria for gout.
Diagnosing gout involves a combination of clinical findings and laboratory tests. The American College of Rheumatology (ACR) criteria are commonly used. These criteria don’t definitively diagnose gout, but they provide a strong indication. Key factors include:
- Acute onset of pain, typically in the first metatarsophalangeal joint (big toe), but other joints can also be affected. The sudden, intense pain is a hallmark of a gout attack.
- Presence of hyperuricemia: A blood test measuring serum uric acid levels will show elevated levels in most, but not all, patients with gout. Note that hyperuricemia alone doesn’t diagnose gout; many individuals with high uric acid levels never experience a gout attack.
- Presence of monosodium urate crystals in the synovial fluid: This is the gold standard diagnostic test. Synovial fluid (the fluid surrounding the joint) is aspirated and examined under a polarized light microscope to identify the characteristic needle-shaped crystals.
- Response to treatment with colchicine or NSAIDs: Rapid improvement in symptoms after treatment with these medications further supports the diagnosis.
It is crucial to rule out other conditions that can mimic gout, such as septic arthritis (joint infection).
Q 3. What are the common symptoms of an acute gout attack?
An acute gout attack typically starts suddenly, often at night. Symptoms include:
- Intense, burning pain: The pain is often described as excruciating and unbearable.
- Swelling and redness: The affected joint becomes visibly inflamed and swollen.
- Tenderness and warmth: The joint is extremely sensitive to touch and feels warmer than surrounding areas.
- Limited range of motion: Movement of the affected joint is severely restricted due to pain and inflammation.
- Fever and chills: In some cases, a gout attack can be accompanied by systemic symptoms like fever and chills.
Imagine waking up in the middle of the night with your big toe throbbing so intensely that even the weight of the bedsheet is unbearable. This is the kind of intense pain associated with an acute gout attack.
Q 4. Differentiate between acute and chronic gout.
Acute gout refers to the sudden, intense inflammatory attack described above. These episodes can last from days to weeks, resolving spontaneously or with treatment. Chronic gout, on the other hand, develops over time due to persistent hyperuricemia. It’s characterized by recurring acute attacks, the formation of tophi (deposits of urate crystals under the skin), and potentially chronic joint damage, leading to deformity and disability. Essentially, acute gout is the single episode of intense pain, while chronic gout is the persistent, long-term condition with recurring attacks and potential for permanent damage.
An analogy would be a leaky faucet (hyperuricemia): acute gout is like when the leak suddenly overflows, causing a mess (an attack), while chronic gout is like that leak continuously dripping, causing long-term damage (permanent joint issues).
Q 5. List the first-line treatment options for acute gout.
First-line treatment options for an acute gout attack focus on rapidly reducing pain and inflammation. Common choices include:
- NSAIDs (Nonsteroidal anti-inflammatory drugs): Such as ibuprofen or naproxen. These are effective at reducing pain and inflammation.
- Colchicine: This medication targets the inflammatory process specifically associated with gout. It’s particularly helpful in preventing further attacks.
- Corticosteroids: Oral or intra-articular (injected directly into the joint) corticosteroids can be used for severe attacks or when NSAIDs and colchicine are not tolerated or ineffective.
The choice of medication depends on the patient’s overall health, other medical conditions, and potential drug interactions. It is crucial to seek medical advice to determine the appropriate treatment strategy.
Q 6. What are the long-term management strategies for chronic gout?
Long-term management of chronic gout aims to prevent future attacks and reduce joint damage. This involves:
- Uricosuric therapy: Medications like probenecid or lesinurad increase the excretion of uric acid through the kidneys, lowering serum uric acid levels.
- Xanthine oxidase inhibitors: Allopurinol or febuxostat reduce the production of uric acid in the body. These are usually started after an acute attack has subsided.
- Lifestyle modifications: As described in the next answer, significant changes in diet and lifestyle are essential components of long-term gout management.
- Regular monitoring: Blood tests should be performed periodically to monitor uric acid levels and assess treatment effectiveness.
The goal is to lower and maintain uric acid levels below the saturation point to prevent further crystal formation and avoid future attacks. The specific treatment regimen is individualized based on the patient’s needs and response to therapy.
Q 7. Discuss the role of lifestyle modifications in gout management.
Lifestyle modifications are crucial for managing gout. They play a vital role in both preventing future attacks and slowing down the progression of chronic gout. Key strategies include:
- Dietary changes: Limiting purine-rich foods like organ meats (liver, kidney), red meat, seafood (especially shellfish), and sugary drinks is essential. A diet rich in fruits, vegetables, and whole grains is encouraged.
- Weight management: Obesity is a major risk factor for gout. Weight loss, even modest weight loss, can significantly reduce uric acid levels and improve gout symptoms.
- Hydration: Drinking plenty of water helps the kidneys excrete uric acid more efficiently, reducing its concentration in the blood.
- Alcohol moderation: Alcohol consumption, particularly beer, can increase uric acid levels and trigger gout attacks. Moderation or abstinence is advised.
- Regular exercise: Physical activity improves overall health and can contribute to weight management, but it’s important to listen to your body during an acute attack and avoid strenuous activity.
Implementing these lifestyle changes alongside medical treatment forms a comprehensive approach for effective gout management and improved patient outcomes. Imagine these changes as building a strong foundation for your health, reducing the burden of gout and improving your overall quality of life.
Q 8. Explain the importance of dietary changes in managing gout.
Dietary changes are absolutely crucial in managing gout. Gout is caused by a buildup of uric acid crystals in the joints, and a high-purine diet significantly contributes to this. Purines are naturally occurring substances found in many foods that the body breaks down into uric acid. By modifying the diet, we aim to reduce uric acid production and improve its excretion.
Key dietary recommendations include:
- Limiting purine-rich foods: This includes organ meats (liver, kidneys), red meat, seafood (especially shellfish), and certain alcoholic beverages, particularly beer.
- Increasing fluid intake: Drinking plenty of water helps flush out uric acid from the body. Aim for at least 8 glasses a day.
- Choosing low-purine foods: Fruits, vegetables, low-fat dairy products, and whole grains are good choices.
- Managing weight: Obesity is a risk factor for gout, so maintaining a healthy weight through diet and exercise is essential.
- Considering a DASH diet: The Dietary Approaches to Stop Hypertension (DASH) diet, rich in fruits, vegetables, and low-fat dairy, is often beneficial in managing gout.
Think of it like this: your body is a plumbing system. A high-purine diet is like constantly clogging the pipes with uric acid crystals. Dietary changes help clear those pipes and prevent further blockages.
Q 9. What are the common medications used to lower uric acid levels?
Several medications are used to lower uric acid levels, each working through different mechanisms. The most common include:
- Xanthine oxidase inhibitors: These, like allopurinol and febuxostat, reduce the production of uric acid.
- Uricosuric agents: These, such as probenecid and lesinurad, increase the excretion of uric acid through the kidneys.
- Pegloticase: This is a more recently introduced medication administered intravenously for patients who haven’t responded to other treatments. It works by directly breaking down uric acid in the blood.
The choice of medication depends on factors such as the patient’s medical history, kidney function, and response to previous treatments. For example, patients with kidney stones might benefit less from uricosuric agents which increase uric acid excretion through the kidneys.
Q 10. Describe the mechanism of action of allopurinol.
Allopurinol works by inhibiting xanthine oxidase, a crucial enzyme in the synthesis of uric acid. Normally, xanthine oxidase converts hypoxanthine to xanthine and then to uric acid. By blocking this enzyme, allopurinol significantly reduces the production of uric acid, leading to lower uric acid levels in the blood.
Imagine a factory producing uric acid. Allopurinol acts like a shutdown switch for a key part of the assembly line, dramatically reducing the final product.
Q 11. What are the potential side effects of colchicine?
Colchicine is an anti-inflammatory drug frequently used to treat acute gout attacks. While effective, it can have side effects, some of which can be serious. These can include:
- Gastrointestinal problems: Nausea, vomiting, diarrhea, and abdominal cramps are common and often dose-limiting.
- Myelosuppression: In rare cases, colchicine can suppress bone marrow function, leading to decreased blood cell production.
- Muscle weakness: Some patients experience muscle weakness or myopathy.
- Neurological side effects: In severe cases, neurological effects like peripheral neuropathy can occur.
It’s crucial to monitor patients closely for these side effects and adjust the dose accordingly. Proper patient education is essential to ensure they understand potential risks and report any issues promptly.
Q 12. How do you monitor the effectiveness of gout treatment?
Monitoring the effectiveness of gout treatment involves several strategies:
- Monitoring serum uric acid levels: Regular blood tests are performed to measure uric acid levels. The goal is to achieve and maintain levels below 6 mg/dL.
- Assessing symptom frequency and severity: Tracking the frequency and intensity of gout attacks provides insight into treatment success.
- Monitoring for tophi resolution: Tophi (deposits of uric acid crystals under the skin) may gradually decrease in size or number with effective treatment.
- Evaluating patient-reported outcomes: Assessing the patient’s quality of life, level of function, and satisfaction with the treatment is also important.
Think of this as a multi-pronged approach. We look at lab results, clinical symptoms, physical examination findings, and patient feedback to build a holistic picture of treatment effectiveness.
Q 13. Discuss the role of imaging in gout diagnosis.
Imaging plays a limited but valuable role in gout diagnosis. While not typically the primary diagnostic tool, imaging can be helpful in certain cases.
- X-rays: Can show erosions and joint deformities that are characteristic of long-standing gout, helping to confirm the diagnosis when clinical signs are unclear or when there is a suspicion of complications.
- Ultrasound: Ultrasound is more sensitive than X-rays in detecting acute gout. It can visualize the presence of monosodium urate crystals within the joint, providing a more definitive diagnosis, particularly in early stages when X-rays might be unremarkable.
However, imaging isn’t always necessary. A detailed history, physical examination, and sometimes joint fluid analysis are often sufficient for a diagnosis of gout.
Q 14. How do you manage tophi in patients with gout?
Managing tophi, the large deposits of uric acid crystals under the skin, requires a multi-faceted approach. The main goal is to lower uric acid levels through medication. This is often done using xanthine oxidase inhibitors like allopurinol, to prevent further tophi formation and possibly allow for some resolution over time.
For large, symptomatic tophi, surgical removal may be considered. This can be necessary for cosmetic reasons, to relieve pressure or pain, or if the tophi become infected. In some cases, injection of the tophi with corticosteroids can help reduce inflammation and size, although the crystals themselves remain. Ultimately, long-term management of uric acid levels is key to prevent the formation of new tophi and managing existing ones.
Q 15. What are the potential complications of untreated gout?
Untreated gout can lead to a range of significant complications, impacting both joint health and overall well-being. The most immediate concern is the recurring, debilitating pain and inflammation of acute gout attacks. These attacks can become more frequent and severe over time if left unmanaged.
- Joint Damage: Repeated episodes of inflammation cause damage to the cartilage and bone in the affected joints, often the big toe but also potentially the ankles, knees, wrists, and hands. This can lead to chronic pain, stiffness, limited range of motion, and even joint deformity (e.g., tophi).
- Kidney Stones: High uric acid levels, a hallmark of gout, can contribute to the formation of kidney stones, causing significant pain and potential long-term kidney damage. This risk is heightened by dehydration.
- Chronic Gouty Arthritis: Persistent hyperuricemia and frequent attacks can result in chronic gouty arthritis, characterized by persistent joint inflammation, swelling, pain, and reduced mobility. This stage is difficult to manage and significantly impairs quality of life.
- Tophi Formation: Urate crystals can deposit under the skin, forming hard nodules called tophi. These can be unsightly and painful, and in severe cases can erode underlying bone and soft tissue.
- Increased Cardiovascular Risk: Studies suggest a link between hyperuricemia and increased risk of cardiovascular events like heart attack and stroke. This isn’t fully understood but may be linked to inflammation and other metabolic factors.
Imagine a patient experiencing repeated gout attacks, each more painful than the last, leading to limited mobility and eventually permanent joint damage. This illustrates the importance of proactive gout management to prevent these devastating long-term consequences.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the patient education you provide regarding gout.
Patient education is crucial for successful gout management. My approach involves a multi-faceted strategy focusing on understanding the disease, lifestyle modifications, medication adherence, and recognizing warning signs.
- Disease Understanding: I explain the underlying cause of gout (uric acid crystal accumulation) and its relationship to diet, alcohol consumption, and other risk factors. I use simple analogies to explain complex concepts – for example, comparing uric acid crystals to sand in a joint.
- Dietary Guidelines: We collaborate to create a personalized dietary plan focusing on reducing purine-rich foods (red meat, organ meats, seafood) and increasing fluid intake to aid uric acid excretion. I emphasize the importance of portion control and mindful eating.
- Lifestyle Changes: We discuss weight management, if needed, as obesity is a significant risk factor. Alcohol consumption limits are established, and regular physical activity (low-impact exercises are recommended) is encouraged.
- Medication Adherence: I explain the purpose, dosage, and potential side effects of all prescribed medications, both acute (for gout attacks) and long-term (to lower uric acid levels). I address concerns and actively troubleshoot challenges to medication adherence.
- Recognizing Warning Signs: Patients are taught to identify early signs of a gout attack (sudden, intense joint pain, swelling, redness) and when to contact their doctor or seek immediate treatment. I empower them to take an active role in their health management.
For example, I might work with a patient to track their food intake using a journal or app, providing feedback and suggesting substitutions for high-purine foods. This patient-centered approach fosters understanding and facilitates adherence.
Q 17. How do you address patient adherence challenges in gout management?
Addressing adherence challenges requires a combination of strategies, acknowledging that each patient is unique. Building a strong patient-provider relationship is fundamental.
- Collaborative Goal Setting: I work with the patient to establish realistic, achievable goals. This collaborative approach fosters a sense of ownership and increases motivation.
- Addressing Barriers: We explore and address potential barriers to adherence, such as medication side effects, cost concerns, or lack of social support. I might suggest strategies to mitigate these obstacles, such as exploring medication assistance programs or involving family members in the treatment plan.
- Regular Follow-up: Frequent monitoring, including blood tests to measure uric acid levels and discussions about any challenges, helps track progress and make adjustments to treatment as needed.
- Education and Reinforcement: Providing ongoing education and reinforcement about the importance of adherence, both verbally and through written materials, is critical.
- Symptom Tracking: Encouraging patients to track their symptoms, such as pain levels and frequency of attacks, helps visualize progress and can motivate continued adherence.
For instance, if a patient experiences side effects from a medication, I might explore alternative medications or adjust the dosage, rather than simply telling the patient to persevere.
Q 18. What are the risk factors for developing gout?
Several factors increase the risk of developing gout. These factors often intertwine, making it crucial to address multiple risk factors for optimal management.
- Genetics: A family history of gout significantly increases the risk.
- High Purine Diet: Consuming excessive amounts of purine-rich foods (red meat, organ meats, shellfish, certain vegetables) leads to higher uric acid production.
- Obesity: Overweight and obese individuals are at increased risk because fat cells produce more uric acid.
- Alcohol Consumption: Alcohol, particularly beer, elevates uric acid levels and can trigger gout attacks.
- Metabolic Syndrome: Individuals with metabolic syndrome (a cluster of conditions including obesity, high blood pressure, and high blood sugar) are more prone to gout.
- Certain Medications: Some medications, such as diuretics (water pills) and low-dose aspirin, can increase uric acid levels.
- Kidney Disease: Impaired kidney function reduces the excretion of uric acid, leading to its accumulation.
- Age and Sex: Gout is more common in men and tends to develop later in women, often after menopause.
Understanding these risk factors allows us to develop a personalized prevention and management plan tailored to the individual’s specific circumstances.
Q 19. How do you differentiate gout from other inflammatory arthritides?
Differentiating gout from other inflammatory arthritides like rheumatoid arthritis (RA) and psoriatic arthritis requires a thorough clinical evaluation and sometimes additional tests.
- Clinical Presentation: Gout typically presents with a sudden onset of intense pain in one joint (monarticular arthritis), often the big toe. In contrast, RA often affects multiple joints symmetrically, while psoriatic arthritis may involve the spine and exhibit skin lesions.
- Joint Fluid Analysis: Analyzing the fluid from an affected joint is crucial. The presence of negatively birefringent monosodium urate crystals under polarized light microscopy confirms the diagnosis of gout.
- Imaging: X-rays can reveal joint damage characteristic of chronic gout, such as erosions and tophi. However, these changes might not be present in early-stage gout.
- Blood Tests: Elevated serum uric acid levels are often found in gout but aren’t specific to gout alone. Other tests may be helpful to rule out other inflammatory conditions.
- Clinical History: The patient’s medical history, including family history of gout, diet, alcohol consumption, and use of certain medications is also significant.
For example, a patient presenting with sudden, severe pain in their big toe, with a history of high alcohol consumption and a family history of gout, is highly suggestive of gout. Confirmation through joint fluid analysis would be essential. On the other hand, a patient with symmetrical joint swelling, morning stiffness, and elevated inflammatory markers would raise suspicion for rheumatoid arthritis.
Q 20. Explain the concept of hyperuricemia and its relationship to gout.
Hyperuricemia is a condition characterized by high levels of uric acid in the blood. Uric acid is a byproduct of purine metabolism, and normally it is filtered by the kidneys and excreted in urine. While hyperuricemia itself isn’t always symptomatic, it is a major risk factor for gout.
The relationship is as follows: when uric acid levels exceed the solubility limit in the body, urate crystals precipitate out of the solution, primarily in joints. These crystals trigger an inflammatory response, leading to the hallmark pain, swelling, redness, and warmth of a gout attack. Not everyone with hyperuricemia develops gout; other factors contribute to crystal formation and deposition.
Think of it like this: hyperuricemia is the buildup of ‘sand’ (uric acid), and gout is the painful ‘sandstorm’ (inflammation) that happens when the sand reaches critical levels and irritates the joint tissues.
Q 21. What are the contraindications for using certain gout medications?
Several gout medications have contraindications or should be used with caution in certain patients. This is why careful assessment before prescribing is essential.
- Allopurinol: Contraindicated in patients with a known hypersensitivity to allopurinol, a condition that can manifest as a severe allergic reaction (Stevens-Johnson syndrome). Kidney impairment requires careful dose adjustments.
- Febuxostat: Contraindicated in patients with severe hepatic impairment. It can also increase cardiovascular risk in some patients.
- Colchicine: Can be toxic at high doses, particularly in patients with impaired kidney or liver function. Careful monitoring is crucial.
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): Contraindicated in patients with known hypersensitivity, severe heart failure, active peptic ulcers, or bleeding disorders. Careful use is needed in individuals with kidney problems.
- Corticosteroids: Long-term use can have significant side effects, including weight gain, diabetes, and osteoporosis. They should be used judiciously, ideally for short durations.
Before prescribing any medication, I carefully review the patient’s medical history, including allergies, current medications, and organ function, to ensure safe and effective treatment.
Q 22. How do you manage gout in patients with comorbidities such as kidney disease?
Managing gout in patients with kidney disease requires a delicate balance. The primary challenge is that many medications used to treat gout, particularly some uric acid-lowering therapies, can be nephrotoxic (harmful to the kidneys). Therefore, careful monitoring of kidney function (eGFR, creatinine levels) is crucial before initiating and throughout treatment.
For example, we might avoid using high doses of NSAIDs or certain uricosuric agents like probenecid in patients with impaired kidney function. Instead, we might prioritize febuxostat or allopurinol at lower doses, carefully monitoring kidney function with blood tests. We might also consider xanthine oxidase inhibitors like allopurinol at lower doses, combined with lifestyle modifications and dietary changes. Patient education about hydration and avoidance of nephrotoxic substances like certain over-the-counter pain relievers is paramount. The goal is to control both gout and protect kidney health.
Each patient’s case is unique. A patient with mild kidney disease might tolerate low-dose allopurinol well, whereas a patient with severe chronic kidney disease might require a different approach altogether, perhaps focusing primarily on managing acute gout flares with colchicine or low-dose NSAIDs and avoiding uricosuric agents.
Q 23. Discuss the use of NSAIDs in acute gout management.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are often the first-line treatment for acute gout flares due to their rapid effectiveness in reducing pain and inflammation. They work by inhibiting the production of prostaglandins, which are mediators of inflammation. Common examples include ibuprofen and naproxen.
However, their use in gout needs careful consideration. NSAIDs can have significant gastrointestinal side effects, including ulcers and bleeding, particularly in patients with a history of such problems. They can also affect kidney function, especially in older adults or those with pre-existing kidney disease. Therefore, NSAID use should be short-term, ideally for only a few days to a week during an acute attack, at the lowest effective dose. Patients should be monitored closely for any adverse effects.
For instance, a patient presenting with severe gout pain might receive a short course of naproxen alongside colchicine. We would carefully assess their risk factors for gastrointestinal bleeding before prescribing and monitor for any signs of bleeding or kidney impairment during treatment.
Q 24. What are the limitations of serum uric acid levels in gout diagnosis?
Serum uric acid levels are helpful but have limitations in gout diagnosis. While elevated serum uric acid is a risk factor for gout, it’s not always diagnostic. Many individuals with elevated uric acid levels never develop gout, and conversely, some people with gout may have normal or only mildly elevated uric acid levels.
The major limitation is that hyperuricemia (high uric acid) is merely a marker of increased risk, not a direct cause or confirmation of gout. The actual diagnosis of gout relies on clinical presentation (acute onset of severe pain, swelling, redness, and tenderness in a single joint, typically the big toe) and supportive evidence from joint fluid analysis showing monosodium urate crystals.
Consider this: A patient might have persistently high uric acid levels but never experience a gout attack. Conversely, a patient might have a classic gout attack despite having only slightly elevated uric acid levels. Therefore, relying solely on serum uric acid to diagnose or manage gout is inadequate. The clinical picture and joint fluid analysis remain crucial for definitive diagnosis.
Q 25. Explain the role of genetic factors in gout development.
Genetic factors play a significant role in gout development. Several genes have been implicated in influencing uric acid metabolism and excretion. Variations in these genes can affect how efficiently the body produces, processes, and eliminates uric acid.
For example, genetic variations affecting enzymes involved in purine metabolism (the pathway that produces uric acid) can lead to increased uric acid production. Similarly, genetic factors influencing renal uric acid excretion can reduce the body’s ability to remove uric acid effectively. A family history of gout substantially increases an individual’s risk of developing the condition, highlighting the contribution of inherited genetic factors.
It’s important to remember that genetics isn’t the sole determinant. Environmental factors such as diet (high purine intake), alcohol consumption, and obesity also contribute significantly to the risk and severity of gout. Understanding the interplay between genetic predisposition and environmental triggers provides a comprehensive approach to gout management and prevention.
Q 26. How do you counsel patients on the long-term implications of gout?
Counseling patients on the long-term implications of gout is critical. It involves explaining the chronic nature of the condition and the importance of long-term management to prevent further attacks, joint damage, and associated comorbidities.
I emphasize the need for lifestyle modifications, including dietary changes (reducing purine-rich foods like red meat and organ meats), weight management (if overweight or obese), and moderate alcohol consumption. Adherence to prescribed medication is crucial, as is regular monitoring of serum uric acid levels and kidney function. I also stress the importance of recognizing and promptly treating acute flares to minimize joint damage. I explain the potential long-term complications, such as chronic joint inflammation, tophi (uric acid crystal deposits under the skin), and kidney stones. It’s a collaborative approach, where the patient understands their role in managing the disease and improving their quality of life.
For instance, I might show a patient images of tophi to illustrate the potential consequences of uncontrolled gout and empower them to participate actively in their management plan. I also provide resources and support groups to build a strong patient-provider relationship focused on long-term success.
Q 27. Discuss the current research and advancements in gout management.
Current research in gout management focuses on several areas. There’s ongoing investigation into newer, more effective uric acid-lowering therapies with fewer side effects. Researchers are exploring the role of various biologic agents that target inflammatory pathways to prevent and treat acute gout flares and potentially reduce long-term joint damage.
Another area of focus is personalized medicine, aiming to tailor gout treatment based on individual genetic profiles, comorbidities, and lifestyle factors. This could involve developing diagnostic tools to identify patients at higher risk for severe disease or those who are less likely to respond to standard treatments. Advances in imaging techniques help us better understand the pathophysiology of gout and assess the extent of joint damage. There’s increased emphasis on preventive strategies, focusing on early identification of individuals at high risk and implementing lifestyle interventions and early pharmacologic treatment to prevent disease onset.
For example, studies are evaluating the efficacy of new biologic therapies targeting IL-1β, a key inflammatory cytokine in gout. Furthermore, research is ongoing to explore the genetic basis of treatment response to help predict which patients will benefit most from specific medications.
Q 28. What are your strategies for managing resistant cases of gout?
Managing resistant cases of gout, where symptoms persist despite standard treatment, requires a multi-faceted approach. First, it’s crucial to re-evaluate the diagnosis, ensuring there aren’t any other underlying conditions mimicking gout. We need to ensure proper adherence to prescribed medication and review any potential drug interactions or contraindications.
Strategies include optimizing uric acid-lowering therapy. This might involve increasing the dose of allopurinol or febuxostat, switching to an alternative agent, or adding a uricosuric agent like lesinurad (with careful monitoring of kidney function). We also assess for and manage any comorbidities, such as hypertension or kidney disease, which can affect treatment choices. In some cases, we may consider combination therapies, using a combination of uric acid-lowering agents and anti-inflammatory medications for more effective control. If conservative approaches fail, we might explore options like intra-articular corticosteroid injections for localized disease or surgical removal of tophi in severe cases.
A patient with persistent gout despite taking allopurinol might benefit from a trial of febuxostat, or if kidney function allows, a combination with lesinurad. Close collaboration with the patient is essential to adjust treatment strategies and address any concerns or barriers to successful management.
Key Topics to Learn for Gout Management Interview
- Pathophysiology of Gout: Understand the underlying mechanisms of hyperuricemia, urate crystal deposition, and the inflammatory response in gout.
- Diagnosis of Gout: Familiarize yourself with diagnostic criteria, including serum uric acid levels, joint fluid analysis, and imaging techniques.
- Treatment Strategies: Master the principles of acute gout management (e.g., NSAIDs, colchicine, corticosteroids) and long-term management (e.g., urate-lowering therapy, lifestyle modifications).
- Pharmacotherapy in Gout Management: Develop a strong understanding of different medications used to treat gout, including their mechanisms of action, indications, contraindications, and potential adverse effects.
- Lifestyle Interventions: Know the role of diet (purine-rich foods, alcohol), weight management, and exercise in preventing and managing gout.
- Patient Education and Counseling: Understand the importance of educating patients about gout, its management, and potential complications.
- Monitoring and Assessment: Learn how to effectively monitor patients’ response to treatment, identify and manage potential complications, and adjust treatment plans accordingly.
- Differential Diagnosis of Gout: Be prepared to discuss conditions that mimic gout and how to differentiate them through clinical presentation and investigations.
- Special Populations: Understand the specific challenges in managing gout in patients with comorbidities (e.g., renal impairment, cardiovascular disease).
- Emerging Therapies in Gout Management: Stay updated on the latest advancements in gout management, including novel therapeutic agents and approaches.
Next Steps
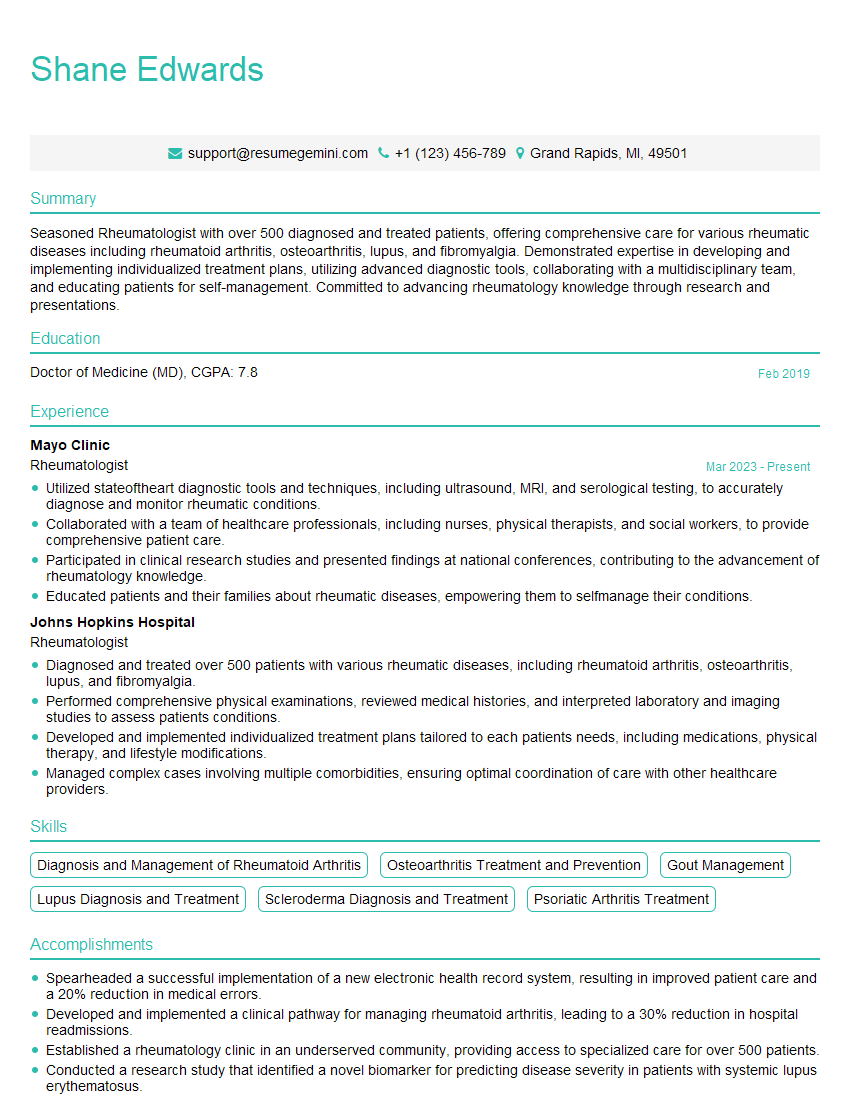
Mastering Gout Management demonstrates a strong foundation in rheumatology and patient care, significantly enhancing your career prospects in healthcare. A well-crafted resume is crucial for showcasing your skills and experience to potential employers. To maximize your chances, focus on building an ATS-friendly resume that highlights your relevant achievements and expertise. ResumeGemini is a trusted resource that can help you create a professional and impactful resume. Examples of resumes tailored to Gout Management are available to guide you in crafting the perfect application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.