The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Hearing Aid Fitting and Evaluation interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Hearing Aid Fitting and Evaluation Interview
Q 1. Describe the process of selecting appropriate hearing aids based on patient needs and audiogram results.
Selecting the right hearing aid involves a thorough understanding of the patient’s hearing loss, lifestyle, and preferences. It begins with a comprehensive audiological evaluation, resulting in an audiogram – a graph showing the patient’s hearing thresholds at different frequencies. This audiogram reveals the type, degree, and configuration of hearing loss (e.g., mild high-frequency loss, severe sensorineural hearing loss).
Next, we consider the patient’s lifestyle. Someone who is very active might benefit from a robust, durable hearing aid, while someone with dexterity issues might prefer a larger, easier-to-handle model. Their listening preferences – such as a preference for music or speech in noise – also play a role. Finally, we discuss budget and technological preferences. We present several options, explaining the pros and cons of each, ensuring the patient feels empowered in the decision-making process. For example, a patient with mild high-frequency loss might be a good candidate for an open-fit hearing aid, while someone with significant hearing loss across all frequencies might require a more powerful behind-the-ear (BTE) device. The goal is to find the best match between hearing loss, lifestyle, and available technology.
Q 2. Explain different types of hearing aid technology (e.g., BTE, ITE, RIC) and their suitability for various hearing losses.
Hearing aids come in various styles, each suited to different hearing losses and lifestyles.
- Behind-the-Ear (BTE): These are worn behind the ear and connected to a custom earmold that fits inside the ear canal. They are suitable for all degrees of hearing loss, especially significant losses, as they can house powerful amplification components. They are also generally more robust and durable.
- In-the-Ear (ITE): These are custom-made to fit completely inside the outer ear. They are suitable for mild to moderately severe hearing losses. They are less visible than BTEs but may be less durable.
- Receiver-in-Canal (RIC): These consist of a small case worn behind the ear, connected to a tiny receiver that sits inside the ear canal. They combine the benefits of both BTEs (power and durability) and ITEs (smaller size and better cosmetic appeal). They’re very popular for moderate to severe hearing losses.
- Completely-in-Canal (CIC) and Invisible-in-Canal (IIC): These are the smallest styles and are completely hidden within the ear canal. They are suitable for mild to moderate hearing losses and are ideal for patients who prioritize aesthetics. However, they can be more challenging to handle.
The choice depends on the individual’s hearing loss, ear anatomy, dexterity, and cosmetic preferences. We always carefully assess these factors before making a recommendation.
Q 3. How do you counsel patients about realistic expectations regarding hearing aid benefits and limitations?
Counseling patients about realistic expectations is crucial for successful hearing aid use. It involves managing their hopes and addressing potential limitations.
I emphasize that hearing aids amplify sounds, they don’t restore hearing to normal. They can significantly improve speech understanding, particularly in quiet environments. However, they might not fully eliminate background noise or perfectly restore hearing in challenging listening situations like crowded restaurants.
I use real-life examples to illustrate these points. For instance, I might explain that a hearing aid can make a conversation clearer, but it might not magically eliminate all the noise from a busy street.
I also discuss potential challenges like adjusting to the sound of their own voice (occlusion effect) and the need for ongoing adjustments and maintenance. Open communication is key. I encourage patients to share their experiences and concerns so that we can make necessary adjustments and ensure they’re happy with their hearing aids.
Q 4. What are the common challenges encountered during hearing aid fitting and how do you address them?
Common challenges include difficulty adapting to amplified sounds, feedback (a whistling sound), occlusion effect (a muffled feeling of one’s own voice), and difficulties with speech in noise.
- Adaptation: Many patients experience a period of adjustment as their brains learn to process amplified sounds. We use a gradual amplification strategy, starting with lower gains and gradually increasing them. We also provide regular follow-up appointments for support and encouragement.
- Feedback: This often occurs due to sound leaking from the ear canal. We address this by adjusting the earmold fit, using feedback reduction technology within the hearing aid, or changing the ear tip.
- Occlusion Effect: This is caused by the blocking of the ear canal. We address this through venting the earmolds or using specific hearing aid programs designed to reduce the occlusion effect.
- Speech in Noise: This is common. We use directional microphones, noise reduction algorithms, and other advanced features to help patients understand speech in noisy environments. We may also suggest strategies like facing the speaker directly.
Problem-solving involves careful listening, troubleshooting, and adjusting the hearing aids. We use a combination of technical solutions and patient education to address these challenges effectively.
Q 5. Describe your experience with real-ear measurement and its importance in hearing aid fitting.
Real-ear measurement (REM) is a crucial part of hearing aid fitting. It involves inserting a tiny microphone into the ear canal to measure the sound level delivered by the hearing aid directly at the eardrum.
This provides accurate data on how well the hearing aid is amplifying sounds at different frequencies, allowing us to fine-tune the amplification to achieve the best possible outcome. Without REM, we would be fitting hearing aids based on estimations, potentially resulting in suboptimal amplification and patient dissatisfaction.
For example, REM helps us identify and correct any discrepancies between the prescribed amplification and the actual sound delivered. It ensures that the hearing aid is providing the appropriate gain (amount of amplification) at each frequency, maximizing the patient’s hearing ability. It is essential for ensuring accurate fitting and optimal hearing aid performance.
Q 6. How do you verify hearing aid function and make necessary adjustments?
Verifying hearing aid function involves a combination of objective and subjective measures.
Objective measures include using real-ear measurements (REM) to ensure the hearing aid is delivering the prescribed amplification. We also use software to analyze the hearing aid’s output and functionality.
Subjective measures involve assessing the patient’s satisfaction and ability to understand speech in various listening situations. We use questionnaires, speech-in-noise tests, and informal conversations to gauge their experience.
Adjustments are made based on this combined data. If REM shows insufficient amplification at certain frequencies, we adjust the hearing aid’s settings accordingly. If the patient reports difficulty understanding speech in noise, we explore strategies to improve the signal-to-noise ratio. This iterative process of measurement, assessment, and adjustment is crucial for optimal hearing aid performance.
Q 7. Explain the process of troubleshooting common hearing aid problems (e.g., feedback, occlusion effect).
Troubleshooting common problems often requires a systematic approach.
- Feedback: We check the earmold fit, ensure the ear canal is free of wax, adjust the hearing aid’s settings, or modify the ear tip to eliminate sound leakage.
- Occlusion Effect: We might adjust the venting on the earmold, use different hearing aid programs, or even switch to an open-fit style hearing aid.
- Battery Issues: We check the battery compartment, ensure proper battery placement, and check battery type and freshness.
- Poor Sound Quality: We check the hearing aid’s settings, inspect for any blockages, and ensure the microphone is unobstructed.
- No Sound: We verify the hearing aid is turned on, that the battery is charged or replaced, and that the volume is adequately adjusted.
Patient education plays a significant role. We teach patients about basic troubleshooting steps, empowering them to handle minor issues independently. For persistent problems, they are always welcome to contact us for support.
Q 8. How do you assess a patient’s candidacy for different hearing aid styles?
Assessing a patient’s candidacy for different hearing aid styles involves a comprehensive evaluation considering several factors. It’s not just about hearing loss severity; it’s about the whole person. We begin with a detailed audiogram, which provides a precise map of hearing thresholds at different frequencies. This tells us the type and degree of hearing loss. Then, we consider the patient’s lifestyle, dexterity, and cognitive abilities.
Mild Hearing Loss: Patients with mild loss might be suitable for smaller, less visible styles like Completely-in-the-Canal (CIC) or Invisible-in-the-Canal (IIC) aids. However, these often have limited features and may be more difficult to manipulate.
Moderate to Severe Hearing Loss: Individuals with more significant hearing loss typically benefit from Behind-the-Ear (BTE) or In-the-Ear (ITE) hearing aids, which offer greater amplification and potentially more advanced features. BTEs are especially useful for those with dexterity issues.
Severe to Profound Hearing Loss: Powerful BTE aids, sometimes with additional features like telecoils for improved phone use, are usually necessary.
Dexterity and Cognitive Ability: Patients with limited dexterity might struggle with smaller, more intricate hearing aids. Similarly, those with cognitive impairment might require simpler devices with fewer adjustable settings. We always involve family members or caregivers in these situations.
For example, a young, tech-savvy individual with mild hearing loss might prefer a discreet CIC aid with Bluetooth connectivity. Conversely, an elderly patient with arthritis and moderate hearing loss might benefit from a larger, easier-to-handle BTE aid.
Q 9. How do you perform hearing aid orientation and provide patient education?
Hearing aid orientation and patient education are crucial for successful hearing aid use. This is not a one-time event; it’s an ongoing process. The initial session includes a thorough explanation of the hearing aid’s features, functionality, and how to perform basic maintenance (e.g., battery changes, cleaning). We demonstrate how to insert and remove the aids, adjust volume, and use any special features.
We then provide detailed instructions on troubleshooting common problems like feedback (whistling) and occlusion (a muffled sound). We also stress the importance of regular maintenance and follow-up appointments.
Patient Education Tailored to Needs: The education should be tailored to the individual’s learning style and comprehension level. Some might grasp the concepts quickly, while others might require more time and repeated explanations. We use visual aids, handouts, and real-world examples to enhance understanding. For example, I might use a diagram to explain how directional microphones work and how they enhance speech in noisy environments. We also encourage questions and provide contact information for any concerns that may arise after the initial session.
Furthermore, we might incorporate family members in the education process, especially if the patient has cognitive impairment or requires assistance with hearing aid maintenance.
Q 10. How do you address patient concerns and complaints regarding hearing aids?
Addressing patient concerns and complaints requires patience, empathy, and a systematic approach. We actively listen to the patient’s concerns, validate their feelings, and thoroughly investigate the issue. Common complaints include feedback, discomfort, poor sound quality, and difficulty adjusting to amplified sound.
Troubleshooting: We begin by systematically troubleshooting the problem. This might involve checking the hearing aid’s fit, battery level, earmold integrity, and verifying the hearing aid’s programming. We might also perform real-ear measurements to ensure the hearing aid is delivering the intended amplification. Sometimes, adjustments to the hearing aid’s settings are necessary.
Realistic Expectations: We often need to manage patient expectations. Hearing aids don’t restore hearing to normal; they improve it. It takes time to adjust to amplified sounds and new listening experiences. We provide encouragement, realistic expectations, and coping strategies.
Example: A patient complained of discomfort. We discovered the earmold had hardened, causing pressure on the ear canal. By replacing the earmold, the discomfort resolved, highlighting the importance of regular maintenance.
Q 11. Describe your experience with different types of hearing loss (conductive, sensorineural, mixed).
My experience encompasses all three types of hearing loss: conductive, sensorineural, and mixed.
Conductive Hearing Loss: This results from problems with the outer or middle ear, impeding sound transmission to the inner ear. Causes include earwax buildup, otitis media (middle ear infection), or ossicular chain abnormalities. Conductive losses are often treatable medically or surgically, sometimes eliminating the need for hearing aids.
Sensorineural Hearing Loss: This arises from damage to the inner ear (cochlea) or auditory nerve. Common causes include aging (presbycusis), noise exposure, certain medications, and genetic factors. Sensorineural hearing loss is usually permanent and often requires hearing aids for compensation.
Mixed Hearing Loss: This is a combination of conductive and sensorineural losses. For example, a patient might have both otosclerosis (a conductive problem) and age-related sensorineural hearing loss. Management often requires medical intervention for the conductive component and hearing aids to address the sensorineural component. The audiogram helps delineate the contributions of each component.
Understanding the type of hearing loss is crucial because it guides our treatment recommendations. A purely conductive loss might be managed medically, while a sensorineural loss requires amplification to compensate for the damaged sensory cells.
Q 12. Explain your understanding of different hearing aid features (e.g., noise reduction, directional microphones).
Modern hearing aids incorporate sophisticated features designed to enhance speech understanding and listening comfort in various environments.
Noise Reduction: This feature analyzes sounds and reduces background noise, making speech easier to hear in noisy settings. It works by identifying and attenuating unwanted sounds while preserving speech signals.
Directional Microphones: These focus on sounds coming from a specific direction, typically in front of the listener, reducing noise from other directions. Think of it as focusing a camera lens – it helps you isolate the sound source you want to hear, similar to focusing on the speaker in a noisy restaurant.
Feedback Cancellation: This system prevents the “whistling” sound (feedback) that can occur when sound escapes from the hearing aid and re-enters the microphone. This usually involves advanced algorithms to identify and suppress the feedback loop.
Frequency Compression: This feature compresses the high-frequency sounds that are often affected in hearing loss and maps them to lower frequencies, making them audible to the patient. It is useful for those with high-frequency hearing loss.
Bluetooth Connectivity: This allows wireless streaming of audio from smartphones, televisions, and other devices directly to the hearing aids.
The specific features included in a hearing aid depend on the patient’s needs and the hearing aid model. We always select features that address the patient’s unique listening challenges and preferences.
Q 13. How do you manage patients with multiple comorbidities affecting their hearing?
Managing patients with multiple comorbidities requires a holistic approach. We work collaboratively with other healthcare professionals, like physicians and neurologists, to ensure the best possible outcome for the patient. For example, a patient with diabetes and hearing loss might experience peripheral neuropathy affecting their dexterity, making it challenging to handle small hearing aids. In this case, we would select a hearing aid style and features that minimize these challenges. We might also discuss with the patient how to best incorporate hearing aid management into their daily routine with their diabetes.
Another scenario: A patient with Alzheimer’s disease might struggle with complex hearing aid adjustments. We simplify the device’s operation and provide clear instructions adapted to their cognitive capabilities. We might also involve family members in the management of the hearing aid.
Essentially, we consider all aspects of the patient’s health and tailor our approach to address the specific needs arising from multiple conditions. Good communication and collaboration are essential to providing effective care.
Q 14. How do you utilize audiometric data to inform hearing aid fitting decisions?
Audiometric data is the cornerstone of hearing aid fitting. The audiogram provides a detailed picture of the patient’s hearing sensitivity across different frequencies. This allows us to determine the type, degree, and configuration of hearing loss. This is paramount in selecting the appropriate hearing aid style, technology level, and fitting strategy.
Specific Examples:
Mild High-Frequency Loss: The audiogram reveals a mild-to-moderate high-frequency loss. This suggests that the hearing aid primarily needs to boost those specific frequencies, without significantly amplifying the lower frequencies, which might lead to discomfort or distortion.
Significant Low-Frequency Loss: A significant low-frequency loss suggests a greater need for amplification in the lower frequencies. The audiogram helps us adjust the hearing aid’s settings to provide the necessary amplification without causing distortion. We need to carefully manage the output to prevent discomfort for the patient.
Slope and Configuration: The shape of the audiogram (slope) significantly impacts the hearing aid programming. For example, a steeply sloping loss might require advanced features like frequency compression to make the high-frequency sounds audible.
Real-ear measurements are also crucial. These measurements verify that the hearing aid is delivering the intended amplification to the patient’s ear canal. We use these measurements to fine-tune the hearing aid’s settings and ensure optimal performance. The audiogram guides the initial settings, and real-ear measurements refine the fitting for optimal sound quality and comfort.
Q 15. What is your approach to managing difficult or demanding patients?
Managing challenging patients requires empathy, clear communication, and a structured approach. I begin by actively listening to their concerns, validating their feelings, and ensuring they understand the process. This often involves explaining complex audiological concepts in simple terms, using analogies to illustrate points. For instance, if a patient is frustrated with feedback, I might compare it to a microphone placed too close to a speaker, creating a screeching sound.
If a patient is particularly demanding, I establish clear expectations regarding appointment times, communication methods, and the scope of services. I document all interactions thoroughly, ensuring clear records of our conversations and any agreed-upon plans. In cases of persistent difficulties, I don’t hesitate to involve other healthcare professionals, such as their primary care physician or a therapist, if appropriate. The goal is to create a collaborative, respectful environment where their hearing needs are addressed effectively, while also setting professional boundaries.
For example, I once had a patient who was extremely anxious about hearing aids. By taking extra time to explain each step, answering her numerous questions patiently, and providing reassurance, I built trust and addressed her concerns, resulting in a positive fitting experience.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with assistive listening devices (ALDs).
Assistive listening devices (ALDs) are crucial for enhancing communication in various challenging listening environments. My experience encompasses a wide range of ALDs, from simple devices like amplified telephones to sophisticated systems like FM systems for classrooms or theaters. I’m proficient in evaluating a patient’s needs to determine the most suitable ALD, considering factors such as their hearing loss, lifestyle, and listening environments.
For example, a patient with significant hearing loss and difficulty following conversations in noisy restaurants might benefit from a table-top microphone system. In contrast, a student with hearing loss in a classroom would likely benefit from an FM system, which transmits the teacher’s voice directly to the student’s hearing aids. I guide patients on proper use and maintenance of the ALDs, ensuring they are effectively integrated into their daily routines. I also provide thorough training and troubleshooting support, assisting them in maximizing the benefits of their ALD.
Q 17. How do you handle situations where insurance coverage is limited?
Limited insurance coverage presents a common challenge. My approach involves a thorough understanding of the patient’s insurance plan and exploring all available coverage options. I explain the various hearing aid technologies and their associated costs transparently, helping the patient make informed decisions within their budget. This includes discussing various financing options, such as payment plans or manufacturer discounts.
If the patient cannot afford the technology needed to best address their hearing loss, I explore alternative solutions. This might involve recommending less expensive hearing aids with comparable features, prioritizing essential features based on their individual needs, or suggesting cost-effective strategies to manage their hearing loss in the interim. I always prioritize the patient’s needs and seek solutions that work within their budgetary constraints while providing the highest level of hearing care possible.
Q 18. How do you stay current with the latest advances in hearing aid technology?
Staying current with the rapidly advancing field of hearing aid technology is paramount. I actively participate in continuing education courses, conferences, and workshops offered by professional organizations like the American Academy of Audiology. I regularly read peer-reviewed journals and industry publications, staying informed about new technologies, research findings, and best practices.
I also maintain strong relationships with hearing aid manufacturers’ representatives, who provide updates on new product releases and technological advancements. This ensures that my knowledge base remains updated and allows me to offer patients the most current and effective solutions for their hearing healthcare needs.
Q 19. What is your approach to documenting hearing aid fitting and follow-up care?
Detailed documentation is crucial for providing high-quality hearing care. My documentation includes a comprehensive case history, audiometric findings, hearing aid selection rationale, fitting details (including specific settings and adjustments), and follow-up care plans. I utilize electronic health records (EHR) software that maintains a secure and easily accessible record of each patient’s journey.
Each patient’s file meticulously documents all appointments, including the date, time, specific interventions, patient feedback, and any necessary modifications to their hearing aids or ALDs. This comprehensive documentation ensures consistent and effective patient care across different time points and enables seamless transitions of care, if needed. Furthermore, it provides a valuable resource for ongoing analysis and improvement of my practice.
Q 20. Explain the importance of regular hearing aid maintenance and cleaning.
Regular maintenance and cleaning are crucial for ensuring optimal performance and longevity of hearing aids. Moisture, earwax, and debris can significantly impact hearing aid function, leading to reduced sound quality, feedback, and even device failure. I educate patients on the importance of daily cleaning using the appropriate tools, such as a soft brush and a drying kit.
I demonstrate proper cleaning techniques and stress the importance of regular professional servicing (typically every 3-6 months). During these service appointments, I perform thorough cleaning, inspect the hearing aids for damage, and make necessary adjustments to ensure optimal performance. I emphasize the impact of neglecting maintenance on both hearing aid lifespan and the patient’s overall hearing experience, making the analogy of regularly servicing a car to keep it running smoothly.
Q 21. How do you communicate effectively with other healthcare professionals involved in patient care?
Effective communication with other healthcare professionals is essential for providing holistic patient care. I utilize various communication methods, including secure electronic messaging systems, phone calls, and in-person meetings. When referring a patient to another specialist, I provide a concise and thorough summary of the patient’s audiological status, hearing aid fitting details, and any relevant medical history.
For example, if a patient presents with dizziness, I would communicate with their physician, sharing relevant information to ensure a coordinated approach to their care. Conversely, I welcome information from other specialists, such as neurologists or ENT physicians, to ensure I have a complete picture of the patient’s health, which helps me provide the most effective and appropriate hearing care.
Q 22. Describe your experience with different hearing aid brands and their features.
My experience spans a wide range of hearing aid brands, including Siemens (now Signia), Phonak, Widex, Starkey, and Oticon. Each brand offers unique technological features and approaches to sound processing. For example, Signia excels in its speech clarity algorithms and its use of advanced noise reduction technologies. Phonak is known for its Roger microphones, particularly beneficial for individuals in noisy environments or with significant hearing loss. Widex focuses on natural sound processing, aiming for a less processed, more realistic listening experience. Starkey emphasizes personalized fitting through its unique software and detailed patient assessments. Oticon’s brain-inspired technology is a major differentiator, seeking to optimize sound processing based on how the brain naturally processes auditory information. I find it crucial to understand the strengths and weaknesses of each brand to best match the technology to the individual patient’s needs and preferences, considering factors like hearing loss severity, lifestyle, and budget.
Beyond the core brands, I’m also familiar with various features common across many brands such as directional microphones (improving speech understanding in noise), feedback cancellation (eliminating whistling), Bluetooth connectivity (for streaming audio), and rechargeable batteries. The selection process involves careful consideration of these features in relation to a patient’s specific auditory profile and their daily listening demands.
Q 23. What are the ethical considerations involved in hearing aid fitting and dispensing?
Ethical considerations in hearing aid fitting and dispensing are paramount. These include:
- Informed Consent: Patients must fully understand their hearing loss, available treatment options (including non-hearing aid solutions), and the limitations of hearing aids. This requires clear, jargon-free communication and answering all patient questions thoroughly.
- Transparency and Disclosure: Full disclosure of all costs, including the hearing aid price, fitting fees, follow-up appointments, and potential maintenance expenses, is crucial. Avoiding hidden fees or misleading information is essential.
- Objectivity and Impartiality: Recommendations must be based solely on the patient’s audiological needs and preferences, not on financial incentives or personal biases toward specific brands or technologies. Presenting multiple options and helping patients weigh the pros and cons of each is vital.
- Confidentiality: Maintaining the patient’s privacy and protecting their personal health information is a fundamental ethical obligation.
- Continuing Education: Staying updated on the latest research, technology, and best practices ensures ethical and competent service delivery.
Ethical dilemmas can arise, particularly when managing patient expectations or balancing cost with desired technology. Open and honest communication is key to navigating these situations, ensuring the patient feels respected and well-informed.
Q 24. How do you ensure patient satisfaction and compliance with hearing aid use?
Ensuring patient satisfaction and compliance hinges on several strategies:
- Realistic Expectations: Setting realistic expectations about hearing aid benefits is crucial from the outset. Hearing aids don’t restore hearing to normal, but they can significantly improve hearing in most situations.
- Thorough Explanation: Providing clear explanations about how to use and care for the hearing aids, including battery changes, cleaning, and troubleshooting common issues is vital.
- Personalized Fitting: A hearing aid fitting tailored to the individual patient’s specific hearing loss, lifestyle, and preferences is paramount for success.
- Regular Follow-up: Scheduled follow-up appointments allow for adjustments, troubleshooting, and ongoing support, reinforcing patient confidence and addressing any concerns promptly. This demonstrates commitment to the patient’s long-term success.
- Patient Education: Providing educational materials, both written and verbal, empower patients to manage their hearing aids effectively and understand the importance of consistent use.
- Trial Period: Offering a trial period, allowing the patient to experience the hearing aids in their everyday life before making a final decision is a valuable strategy.
Active listening and building rapport with patients are essential throughout the process. Understanding their concerns and addressing them with empathy greatly improves satisfaction and compliance.
Q 25. Explain your experience with programming hearing aids using different software platforms.
I’m proficient in programming hearing aids using various software platforms, including those from Signia (fitting software), Phonak (Target), and Oticon (Genie 2). Each platform has its unique interface and features, but the core principles of programming remain consistent: This involves analyzing audiometric data (hearing test results), considering patient preferences, and fine-tuning the hearing aid settings to optimize speech understanding and comfort. For example, NOA (Narrowband Output Algorithm) and WDRC (Wide Dynamic Range Compression) are common algorithms used to manage amplification across different frequencies.
The process involves selecting appropriate amplification strategies, noise reduction settings, and frequency response shaping to address the specific nature of the individual’s hearing loss. Real-ear measurements (REM) are routinely integrated to verify the actual sound levels delivered to the patient’s ear, ensuring accurate and effective amplification.
Mastering these platforms requires ongoing training and hands-on experience. Regular updates and participation in advanced training programs keep my skills sharp and allow me to adapt to evolving technologies.
Q 26. How do you adapt your fitting strategy for patients with specific needs (e.g., cognitive impairment, dexterity limitations)?
Adapting my fitting strategy for patients with specific needs requires a flexible and patient-centered approach. For patients with cognitive impairment, I may utilize simpler explanations, visual aids, and involve caregivers in the process. I prioritize clear and concise instructions and incorporate frequent reinforcement of key concepts. For patients with dexterity limitations, I may explore hearing aids with larger controls, or recommend devices with remote control apps or automatic programs to simplify handling. In some cases, assistive technologies and training may be needed.
Other specific needs, such as tinnitus, hyperacusis (increased sensitivity to sound), or unilateral hearing loss, are carefully considered during the fitting process. The fitting strategy is always tailored to the individual’s unique profile, taking into account all relevant factors to maximize the potential benefits of hearing aid use and minimize discomfort.
Q 27. How do you counsel patients on the financial aspects of hearing aid acquisition and maintenance?
Counseling patients on the financial aspects of hearing aid acquisition and maintenance is a crucial part of my role. I clearly explain the costs involved, including the hearing aid price, fitting fees, follow-up appointments, and potential maintenance or repair costs. I provide detailed information about available financing options, insurance coverage, and manufacturer warranties. This transparency builds trust and ensures patients make informed decisions.
I also discuss the long-term cost savings associated with improved communication, reduced social isolation, and enhanced quality of life resulting from better hearing. We explore the best options, considering factors like the patient’s budget and the desired level of technology to find a solution that aligns with both financial considerations and auditory needs.
Q 28. Describe a challenging hearing aid fitting case and how you successfully resolved the issue.
One challenging case involved a patient with severe sensorineural hearing loss and significant tinnitus. Traditional amplification strategies were initially unsuccessful, causing increased discomfort and reduced tolerance for the hearing aids. The patient reported amplified tinnitus and significant difficulty adapting to the amplified sounds.
To address this, I utilized a combination of strategies. First, I adjusted the amplification settings to focus more on speech intelligibility in quiet environments rather than attempting aggressive noise reduction, which sometimes exacerbates tinnitus. Secondly, I incorporated tinnitus management features available in the hearing aids, such as notched filters or masking sounds. We also spent time exploring different sound processing strategies and fitting approaches. Regular follow-up appointments were key to continually monitoring the patient’s progress and making small, iterative adjustments. The successful resolution of this case demonstrates the importance of flexibility, patience, and ongoing collaboration with the patient throughout the fitting process.
Key Topics to Learn for Hearing Aid Fitting and Evaluation Interview
- Audiogram Interpretation: Understanding various audiometric configurations, identifying hearing loss types (conductive, sensorineural, mixed), and interpreting results to determine appropriate hearing aid styles and amplification strategies.
- Hearing Aid Technology: Familiarity with different hearing aid styles (BTE, ITE, RIC, etc.), amplification technologies (linear, non-linear), features (noise reduction, feedback management, directional microphones), and their suitability for various hearing loss profiles.
- Hearing Aid Fitting Procedures: Mastering the practical aspects of fitting hearing aids, including real-ear measurement (REM) techniques, verification, and validation procedures to ensure optimal amplification and patient comfort.
- Counseling and Communication: Developing effective communication skills to explain hearing loss, hearing aid technology, and management strategies to patients. Addressing patient concerns and expectations with empathy and professionalism.
- Troubleshooting and Problem-Solving: Developing the ability to identify and resolve common hearing aid problems, such as feedback, occlusion effect, and other performance issues. Understanding troubleshooting strategies and maintenance procedures.
- Real-World Case Studies: Preparing examples of successful hearing aid fittings and how you addressed specific patient needs and challenges. Highlighting your problem-solving skills and clinical judgment.
- Evidence-Based Practice: Understanding the importance of using current research and best practices to inform your fitting decisions and stay updated on the latest advancements in the field.
- Patient Management: Demonstrating understanding of the entire patient journey, from initial assessment to follow-up care, including managing patient expectations and providing ongoing support.
Next Steps
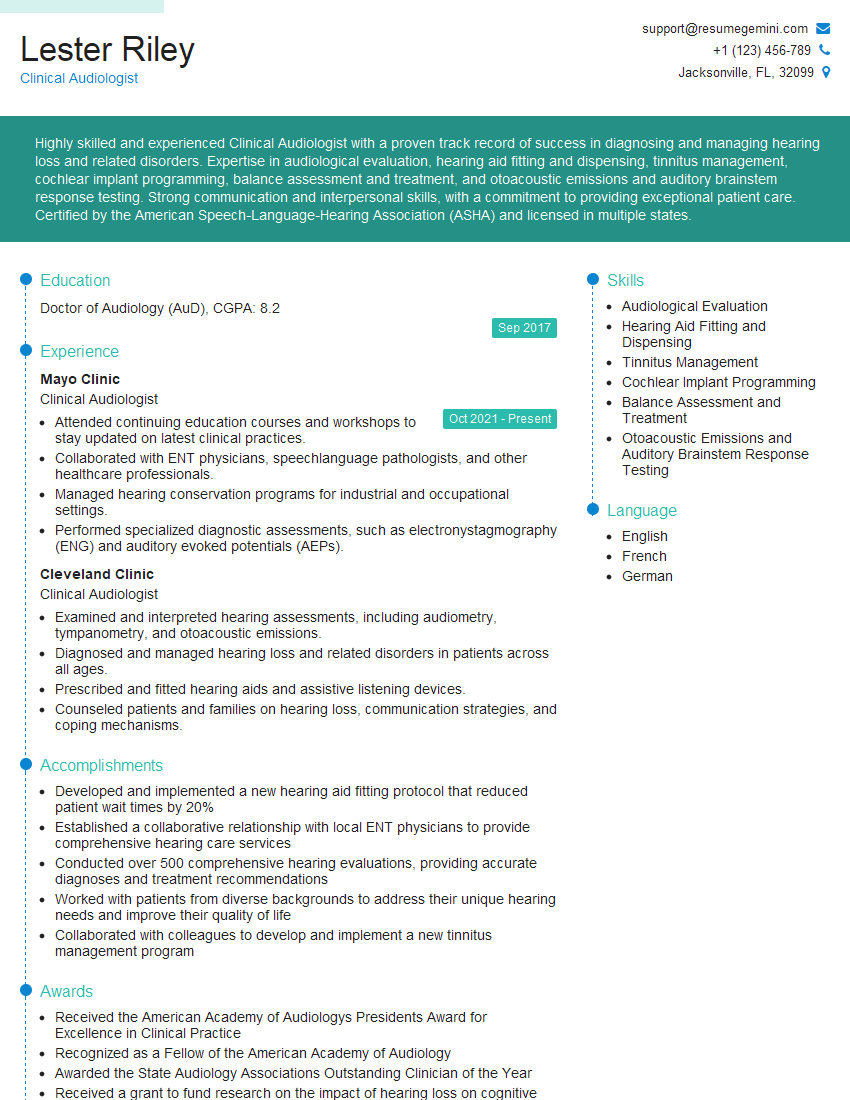
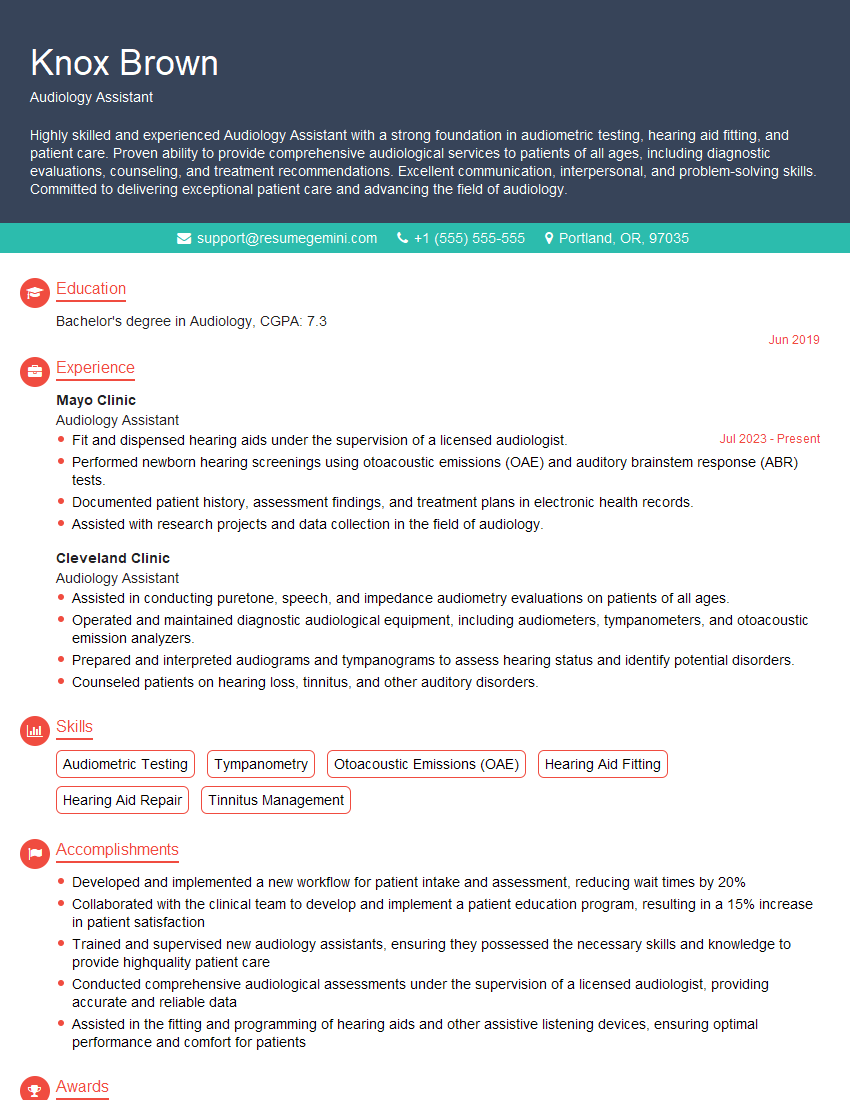
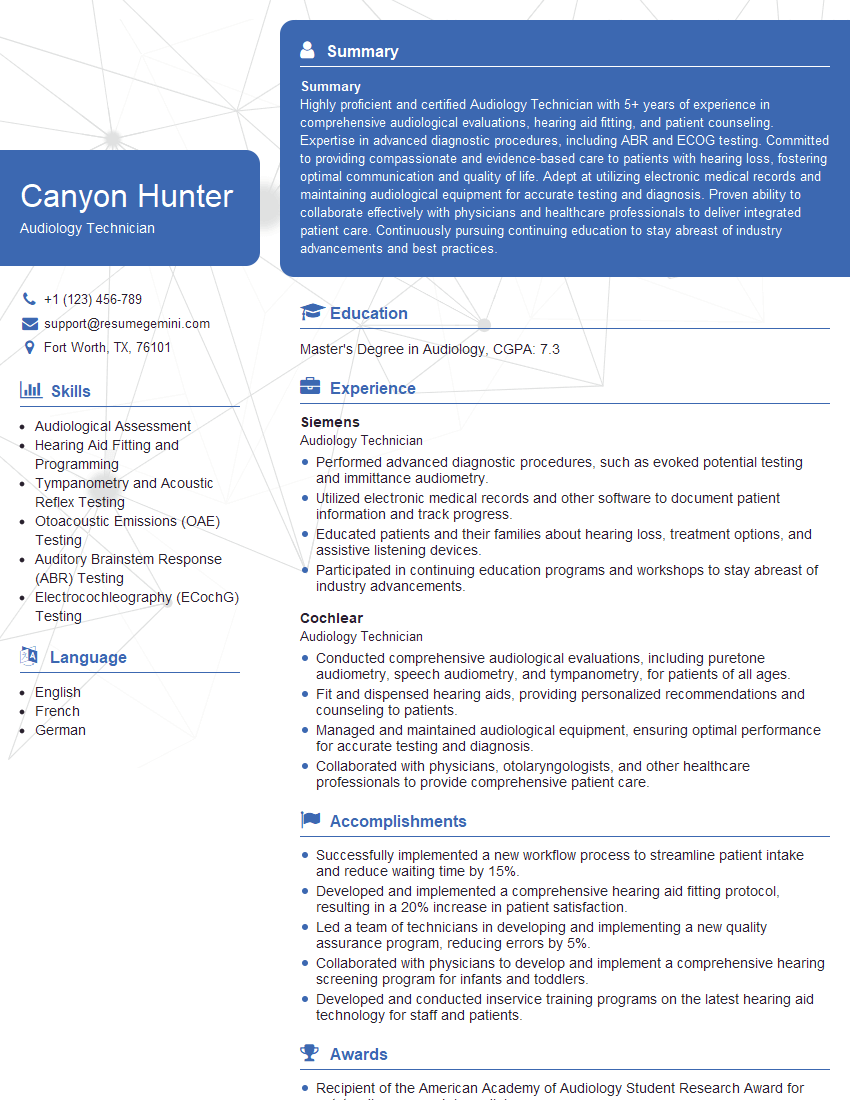
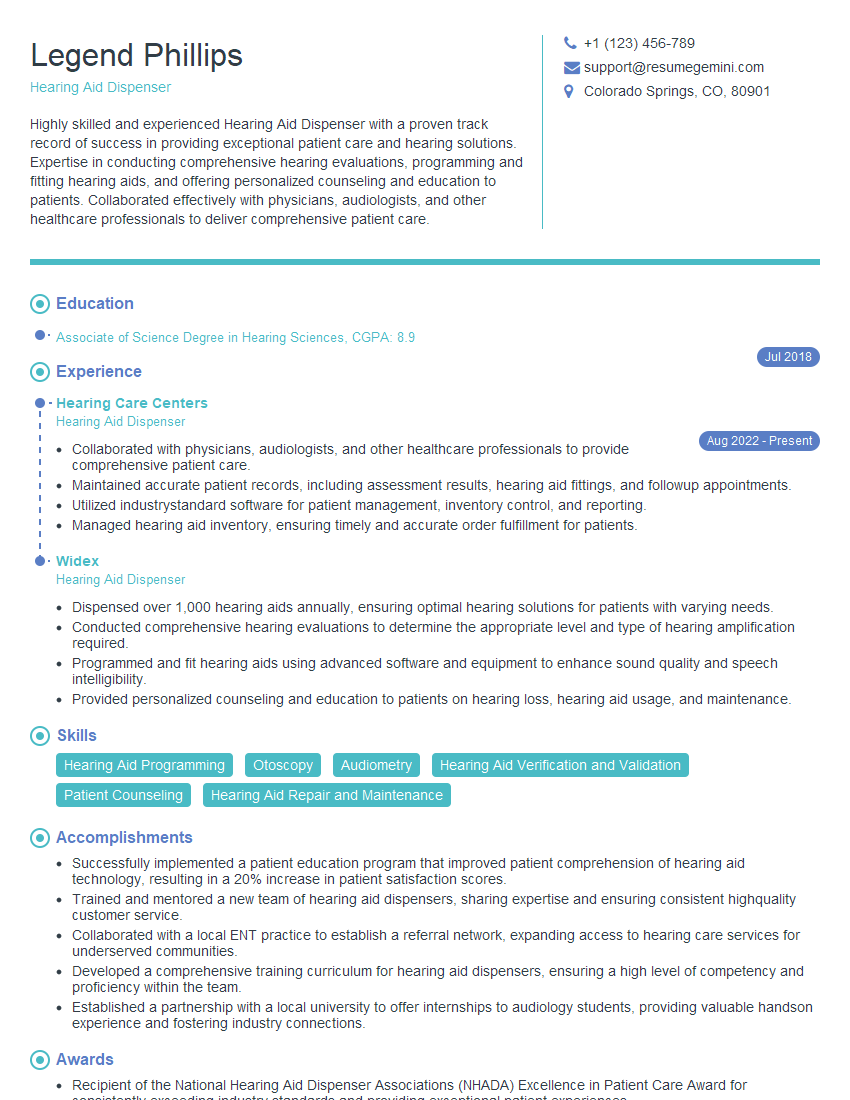
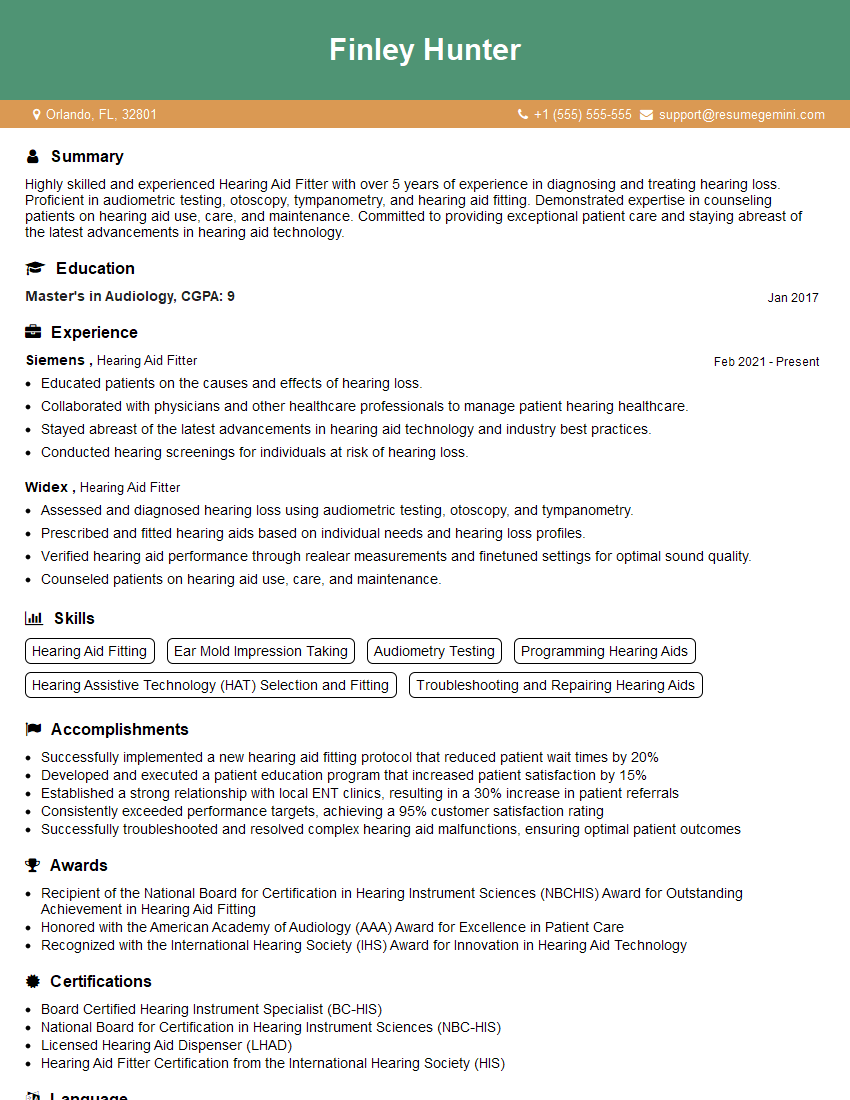
Mastering Hearing Aid Fitting and Evaluation is crucial for career advancement in audiology and related fields. A strong understanding of these concepts demonstrates your clinical skills and commitment to providing excellent patient care. To maximize your job prospects, create a resume that effectively showcases your skills and experience to Applicant Tracking Systems (ATS). ResumeGemini is a trusted resource to help you build a professional and ATS-friendly resume that highlights your qualifications. Examples of resumes tailored to Hearing Aid Fitting and Evaluation are available to guide you in crafting a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.