Cracking a skill-specific interview, like one for Heel Spur and Plantar Fasciitis Management, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Heel Spur and Plantar Fasciitis Management Interview
Q 1. Describe the anatomical structures involved in heel spur formation.
Heel spurs are bony outgrowths that develop on the underside of the heel bone, the calcaneus. This formation involves several anatomical structures. The plantar fascia, a thick band of tissue running along the bottom of the foot from the heel to the toes, plays a crucial role. Chronic tension or strain on the plantar fascia can cause microscopic tears near its insertion point on the calcaneus. The body, in an attempt to repair this damage, lays down new bone, leading to the development of a heel spur. The periosteum, the membrane covering the bone, is also involved in this bone formation process. Essentially, it’s a response to repetitive microtrauma and inflammation at the plantar fascia’s insertion point.
Imagine the plantar fascia as a strong rope constantly being pulled. Over time, repeated pulling can fray the rope near its attachment point. The body’s natural response is to reinforce the attachment, building up extra bone (the spur) to provide extra support and stability.
Q 2. Explain the pathophysiology of plantar fasciitis.
Plantar fasciitis is an inflammatory condition affecting the plantar fascia. The pathophysiology begins with repetitive micro-tears or overuse of the plantar fascia, often due to activities like prolonged standing, running, or wearing inadequate footwear. These micro-tears trigger an inflammatory response, characterized by swelling and pain. The inflammation can also involve the surrounding tissues, like the periosteum and surrounding soft tissues. Over time, chronic inflammation can lead to thickening and tightening of the plantar fascia, further contributing to pain. Biomechanical factors like foot pronation (flat feet) and tight calf muscles can exacerbate the condition by increasing strain on the plantar fascia.
Think of it like repeatedly bending a paperclip. Eventually, it will weaken and break. Similarly, consistent stress on the plantar fascia leads to microscopic tears, resulting in inflammation and pain.
Q 3. Differentiate between heel spurs and plantar fasciitis.
While often associated, heel spurs and plantar fasciitis are distinct entities. A heel spur is a bony outgrowth on the calcaneus, visible on X-ray. Plantar fasciitis is an inflammatory condition of the plantar fascia, primarily diagnosed clinically. Crucially, a heel spur may or may not be symptomatic. Many individuals have heel spurs without experiencing any pain. Conversely, plantar fasciitis can exist without a visible heel spur on imaging. The pain in plantar fasciitis is typically felt in the heel and arch, while heel spur pain is often localized to the heel itself. In essence, a heel spur can be a *result* of plantar fasciitis, or a completely separate, asymptomatic finding.
Imagine a tree root (plantar fascia) that’s inflamed (plantar fasciitis). A bony outgrowth (heel spur) might develop near where the root meets the ground, but the root’s inflammation is the main problem, even if the outgrowth is present.
Q 4. What are the common symptoms of heel spurs and plantar fasciitis?
Symptoms of heel spurs and plantar fasciitis often overlap. The most common symptom is heel pain, especially upon waking in the morning or after periods of rest. This is because the plantar fascia tightens overnight. The pain often diminishes with activity, but can return with prolonged standing or weight-bearing. Other symptoms can include stiffness in the heel, pain radiating along the arch of the foot, tenderness to palpation at the heel, and even limited range of motion in the ankle.
One of my patients described the pain as ‘like walking on marbles’ – a sharp, stabbing pain in the heel, followed by a dull ache.
Q 5. List three differential diagnoses for heel pain.
Differential diagnoses for heel pain are crucial to ensure accurate treatment. Three important ones to consider are:
- Stress fracture of the calcaneus: Pain is often more diffuse and may be worse with activity. Weight-bearing can be challenging.
- Achilles tendinitis: Pain is typically located more superiorly in the heel, near the insertion of the Achilles tendon. Palpation of the tendon often reveals tenderness.
- Tarsal tunnel syndrome: This involves compression of the tibial nerve at the ankle, causing pain that can radiate down the sole of the foot and toes, often accompanied by numbness or tingling.
A thorough history and physical examination are essential to distinguish between these conditions.
Q 6. Describe your approach to the physical examination of a patient with heel pain.
My physical examination of a patient with heel pain follows a structured approach. It begins with a comprehensive history, inquiring about the onset, duration, character, and aggravating/relieving factors of the pain. I then perform a visual inspection, noting any deformities, swelling, or erythema. Palpation of the heel and plantar fascia assesses for tenderness and the presence of a heel spur (although this is not always palpable). Range of motion of the ankle and toes is evaluated. I assess for tightness in the calf muscles via gastrocnemius and soleus stretching. Finally, I conduct specific orthopedic tests, such as the plantar fascia palpation test, to assess tenderness and tension in the plantar fascia.
For example, I’ll gently squeeze the plantar fascia to evaluate for tenderness, and I’ll passively dorsiflex the patient’s foot to assess for tightness in the plantar fascia. This allows me to systematically rule out other conditions and pinpoint the source of the pain.
Q 7. What imaging modalities are used to diagnose heel spurs and plantar fasciitis?
Imaging modalities play a vital role in diagnosing heel spurs and plantar fasciitis, although not always necessary. X-rays are the primary imaging technique for identifying heel spurs. They clearly show the bony outgrowth on the calcaneus. However, X-rays do not directly visualize the plantar fascia or show inflammation. Ultrasound can assess the thickness and echogenicity of the plantar fascia, providing information on inflammation. MRI can provide detailed images of soft tissues, including the plantar fascia and surrounding structures, offering valuable information in cases where the diagnosis is uncertain or when assessing the severity of plantar fasciitis.
In practice, I often start with X-rays to rule out fractures or other bony abnormalities and then use ultrasound if the clinical picture and X-ray findings don’t fully explain the patient’s symptoms. MRI is usually reserved for complex cases or when considering surgical intervention.
Q 8. Explain the indications and contraindications for using orthotics in the treatment of plantar fasciitis.
Orthotics, custom-made or over-the-counter shoe inserts, play a significant role in plantar fasciitis management. They provide support to the arch of the foot, reducing strain on the plantar fascia – the thick band of tissue on the bottom of your foot that connects your heel bone to your toes.
Indications for orthotic use include persistent heel pain, plantar fascia inflammation, and arch instability. They’re particularly helpful for individuals with flat feet or high arches, as these foot types are more prone to plantar fasciitis. Orthotics can help redistribute pressure, alleviate pain, and promote proper foot mechanics.
Contraindications are less common but can include cases where the patient has an underlying condition significantly affecting foot structure or function that orthotics can’t correct. For example, severe neurological issues impacting foot sensation or severe deformity might render orthotics less effective. A proper assessment by a podiatrist or physical therapist is crucial to rule out contraindications and determine suitability.
Consider this: imagine a sagging hammock (your plantar fascia). Orthotics act like supports, preventing it from stretching too thin and becoming painful.
Q 9. Describe different non-surgical treatment options for plantar fasciitis.
Non-surgical treatment for plantar fasciitis is the first line of defense and often highly effective. It focuses on reducing inflammation and improving foot mechanics. Options include:
- Rest and Ice: Avoiding activities that aggravate pain and applying ice packs to reduce inflammation are fundamental. Think of it as giving your plantar fascia a break to heal.
- Medication: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help manage pain and inflammation. Your doctor may also prescribe stronger medications in some cases.
- Stretching and Exercises: Targeted stretches, like calf stretches and plantar fascia stretches (e.g., towel stretches), improve flexibility and reduce tightness. Strengthening exercises for the lower leg muscles also support the plantar fascia.
- Physical Therapy: A physical therapist can guide you through a personalized exercise program, provide manual therapy (like massage) to address muscle tension, and teach you proper techniques for reducing strain.
- Night Splints: These devices hold the foot in a slightly dorsiflexed position (toes pointing upwards) during sleep, preventing the plantar fascia from shortening and tightening overnight.
- Shoe Modifications: Wearing supportive shoes with good arch support and cushioning can significantly reduce strain on the plantar fascia. Avoid high heels and flat, unsupportive footwear.
Many patients experience significant relief through a combination of these methods.
Q 10. What are the indications for surgical intervention in heel spur and plantar fasciitis cases?
Surgical intervention for heel spurs and plantar fasciitis is generally reserved for cases that haven’t responded to at least 6-12 months of conservative management.
Indications for surgery include:
- Severe, persistent pain: Pain that significantly impacts daily life and doesn’t improve with non-surgical treatments.
- Failed conservative treatment: When other treatments haven’t yielded any significant relief.
- Neuroma or other complications: Presence of a nerve tumor (neuroma) or other conditions associated with heel pain that require surgical intervention.
- Significant functional limitation: When the heel pain prevents you from performing your usual activities, like walking or exercising.
It’s crucial to understand that surgery isn’t a guaranteed solution and may have potential risks and complications. It’s a decision that should be made in close consultation with a surgeon after careful consideration of all treatment options.
Q 11. Explain the surgical techniques used to treat heel spurs.
Surgical techniques for heel spurs vary depending on the specific cause and severity of the problem. Common procedures include:
- Open surgical release of the plantar fascia: This involves a small incision to release the tight plantar fascia, relieving pressure on the heel spur.
- Endoscopic plantar fasciotomy: A minimally invasive procedure using small incisions and a camera to visualize and release the plantar fascia.
- Heel spur removal: In some cases, the heel spur itself may be removed, although this is less common as it’s often the result of plantar fasciitis, not the primary cause of pain. The focus is usually on addressing the underlying plantar fascia problem.
The choice of surgical technique depends on factors such as the severity of the condition, patient’s overall health, and surgeon’s preference.
Q 12. Describe post-operative care following surgery for heel spurs.
Post-operative care after heel spur surgery is essential for a successful recovery. It typically involves:
- Pain management: Medications to control pain and inflammation.
- Immobilization: The foot might be immobilized in a cast or boot for a period of time to protect the surgical site and promote healing.
- Physical therapy: A crucial component, physical therapy helps restore range of motion, strength, and function. This often includes specific stretches, exercises, and gait retraining.
- Weight-bearing restrictions: Initially, patients might be advised to avoid putting weight on the affected foot. This gradually progresses as healing occurs.
- Wound care: Keeping the surgical site clean and dry to prevent infection.
- Follow-up appointments: Regular check-ups with the surgeon to monitor healing progress.
Compliance with the post-operative care plan is crucial for minimizing complications and optimizing the outcome.
Q 13. What are the common complications associated with heel spur surgery?
While heel spur surgery is generally safe, potential complications include:
- Infection: As with any surgery, there’s a risk of infection at the surgical site.
- Nerve damage: Damage to nearby nerves can cause numbness, tingling, or pain.
- Scar tissue formation: Excessive scar tissue can lead to stiffness and restricted movement.
- Recurrence of plantar fasciitis: In some cases, the plantar fasciitis may recur despite surgery.
- Persistent pain: Some patients may experience persistent pain even after surgery.
- Delayed healing: Healing may take longer than expected in some cases.
These complications are not common, but patients should be aware of the possibility before undergoing surgery.
Q 14. How do you counsel patients on lifestyle modifications to manage heel pain?
Counseling patients on lifestyle modifications is a crucial part of managing heel pain, both before and after treatment. This involves a holistic approach addressing various aspects:
- Footwear: Encourage wearing supportive shoes with good arch support and cushioning, avoiding high heels and flat shoes. Recommend shoes with a wide toe box to prevent pressure points.
- Weight Management: Excess weight puts extra stress on the feet and can exacerbate heel pain. Encourage weight loss if appropriate.
- Activity Modification: Patients need to understand how to modify their activities to reduce stress on the plantar fascia. This might involve reducing high-impact activities or using assistive devices like canes if necessary.
- Stretching and Strengthening: Teach patients simple stretches and exercises they can perform daily to improve flexibility and strengthen the supporting muscles around the foot and ankle.
- Ergonomics: If the pain is work-related, advise patients on ergonomic improvements to their workspace to reduce strain on their feet.
- Regular Exercise: Promote overall physical fitness through moderate-impact exercises that don’t worsen the pain, like swimming or cycling.
- Hydration: Adequate hydration promotes tissue health and reduces inflammation.
Providing tailored advice and empowering patients to make these changes is key to long-term management and preventing recurrence. Think of it as building a strong foundation of support around the feet and whole body.
Q 15. Describe different types of stretching exercises for plantar fasciitis.
Stretching is crucial for managing plantar fasciitis, as it helps lengthen the tight plantar fascia and calf muscles. Here are some key stretches:
- Gastrocnemius and Soleus Stretch: This targets the calf muscles, which often contribute to plantar fascia tension. Find a wall or sturdy surface. Extend one leg slightly behind you, keeping your knee straight. Lean into the wall, feeling a stretch in your calf. Hold for 30 seconds and repeat on the other side. For the soleus stretch, slightly bend your back knee.
- Towel Stretch: Sit on the floor with one leg extended. Place a towel around the ball of your foot, holding the ends in your hands. Gently pull the towel, flexing your foot towards your shin. Hold for 30 seconds and repeat. This directly targets the plantar fascia.
- Foot-Rolling Exercise: Use a frozen water bottle, tennis ball, or a specialized massage roller. Roll your foot over the object, applying pressure to the arch and heel. This helps release tension and improve tissue mobility.
- Big Toe Extension: Sit comfortably and gently pull each big toe upwards towards the shin. Hold for several seconds. This focuses on releasing tension specifically around the plantar fascia insertion point.
Remember to perform these stretches regularly, ideally several times a day. It’s important to listen to your body and avoid pushing through pain.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the roles of NSAIDs and other medications in managing plantar fasciitis?
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), like ibuprofen or naproxen, play a significant role in managing the pain and inflammation associated with plantar fasciitis. They provide temporary relief but don’t address the underlying cause. They should be used as directed by a physician and with awareness of potential side effects. Other medications, such as corticosteroids (often injected directly into the plantar fascia), may be considered for severe cases. Corticosteroid injections provide stronger anti-inflammatory relief, but repeated injections carry risks. A physician will weigh the benefits against potential drawbacks like weakening of the plantar fascia.
It’s crucial to remember that medication is a supportive tool, not a sole treatment. It’s most effective when combined with other therapies such as stretching, orthotics, and physical therapy.
Q 17. How do you assess the effectiveness of treatment for plantar fasciitis?
Assessing treatment effectiveness for plantar fasciitis involves a multi-faceted approach. We monitor pain levels using visual analog scales or numerical rating scales. We look for improvements in functional activities: can the patient walk, run, or stand for longer periods without pain? Range of motion in the ankle and foot is also assessed. We compare initial evaluations with follow-up assessments to track progress. Imaging techniques such as X-rays might be used to evaluate the presence of a heel spur, although a spur alone doesn’t always correlate with symptom severity. The patient’s subjective feedback is also critical: their perception of pain relief and overall improvement in quality of life are valuable indicators of treatment success. A combination of these measures gives a comprehensive picture of treatment effectiveness.
Q 18. Explain the use of night splints in the treatment of plantar fasciitis.
Night splints are beneficial because they help maintain dorsiflexion (bending the foot upward) during sleep. This counteracts the plantar fascia’s tendency to shorten and tighten overnight. By keeping the plantar fascia in a stretched position, night splints help reduce morning stiffness and pain. They are particularly useful for those experiencing significant morning pain. The splint gently stretches the plantar fascia throughout the night, promoting tissue lengthening and reducing inflammation. It’s essential to choose a splint that provides comfortable support and doesn’t impede circulation. Compliance is key to success; patients must wear the splint consistently for optimal benefit.
Q 19. Describe your experience with different types of orthotics.
My experience with orthotics encompasses various types, each with specific advantages and disadvantages. Custom-made orthotics offer the best support and personalized correction, tailored to the individual’s foot structure and biomechanics. However, they come with a higher price tag and longer fabrication time. Over-the-counter (OTC) orthotics are readily available and more affordable but may not provide the same level of support as custom devices. They may not address specific foot problems as effectively. Semi-custom orthotics offer a middle ground, combining the benefits of customization with increased accessibility. These pre-fabricated devices are modified to better fit individual needs. The choice depends on the patient’s condition, budget, and individual requirements. For example, a patient with severe pes planus (flat feet) would benefit most from a custom orthotic, while someone with mild plantar fasciitis might find relief from a well-fitting OTC insole.
Q 20. How do you manage patients with chronic plantar fasciitis?
Managing chronic plantar fasciitis requires a comprehensive and often long-term approach. We continue to emphasize the core treatments: stretching, strengthening exercises, and orthotics. However, in chronic cases, we may explore more advanced techniques. Extracorporeal shock wave therapy (ESWT) is one option, though its effectiveness isn’t universally established. Surgical intervention is rarely considered, reserved only for patients who have failed all other conservative therapies after a lengthy trial. A multidisciplinary approach may involve physical therapists for targeted exercises and gait retraining, podiatrists for custom orthotics, and pain management specialists if necessary. In some instances, addressing underlying conditions like obesity or diabetes is crucial, as they can exacerbate plantar fasciitis.
Regular follow-up appointments are vital to monitor progress and adapt treatment strategies as needed. The focus is not just on reducing pain but also improving long-term functional capacity and preventing recurrence.
Q 21. What are the risk factors for developing heel spurs and plantar fasciitis?
Several factors increase the risk of developing heel spurs and plantar fasciitis. These include:
- Activities that put stress on the feet: Running, jumping, high-impact activities, and prolonged standing.
- Foot structure: High arches (pes cavus) or flat feet (pes planus) can alter foot mechanics and increase stress on the plantar fascia.
- Tight calf muscles: Limited flexibility in the calf muscles puts strain on the plantar fascia.
- Improper footwear: Shoes that lack adequate support or cushioning increase the risk.
- Obesity: Excess weight places added stress on the feet and plantar fascia.
- Age: The plantar fascia naturally loses elasticity with age, increasing susceptibility to injury.
- Certain medical conditions: Diabetes, rheumatoid arthritis, and other inflammatory conditions can increase risk.
Understanding these risk factors allows for proactive strategies, such as choosing supportive footwear, maintaining a healthy weight, and engaging in regular stretching to minimize the chances of developing heel spurs and plantar fasciitis.
Q 22. How do you differentiate between plantar fasciitis and other causes of heel pain, such as nerve entrapment?
Differentiating plantar fasciitis from other heel pain causes requires a thorough clinical examination and often imaging studies. Plantar fasciitis typically presents with pain in the heel, especially in the morning or after periods of rest, that improves with activity. The pain is often localized to the plantar fascia origin at the heel bone (calcaneus). This is unlike nerve entrapment, such as tarsal tunnel syndrome, which usually involves pain radiating down the foot, numbness, tingling, and may be worse at night.
For example, a patient with plantar fasciitis might describe a sharp, stabbing pain when they first step out of bed, which eases slightly as they walk around. A patient with tarsal tunnel syndrome might describe burning or tingling sensations along the inner ankle and sole of the foot, often worsening after prolonged standing or activity. A thorough history of the onset and character of pain, location of pain, and aggravating factors, combined with a physical examination assessing range of motion, palpation of the plantar fascia, and neurological testing, helps in the correct diagnosis. Imaging like X-rays can help rule out other causes like stress fractures or heel spurs (which often coexist with plantar fasciitis, but are not the direct cause of the pain).
Q 23. Describe your experience with extracorporeal shock wave therapy (ESWT) for plantar fasciitis.
Extracorporeal shock wave therapy (ESWT) is a treatment option I use for chronic plantar fasciitis that hasn’t responded to conservative management. It involves delivering sound waves to the affected area to stimulate tissue healing and reduce pain. My experience shows that ESWT can be effective, but it’s crucial to select appropriate candidates. Patients with acute plantar fasciitis or those with significant inflammatory conditions are generally not ideal candidates.
I typically reserve ESWT for patients who have failed at least 6-8 weeks of conservative treatment including physical therapy, stretching, orthotics, and NSAIDs. I explain the procedure, potential side effects (minor bruising or soreness at the treatment site), and the possibility of needing multiple sessions. Success rates vary, but I’ve seen good outcomes in a significant portion of patients, particularly those with chronic, recalcitrant plantar fasciitis. It’s not a standalone treatment and usually incorporated as part of a comprehensive management plan. For example, a patient who had completed physical therapy with minimal improvement might benefit greatly from three to five sessions of ESWT combined with continued stretching and orthotic use. Post-ESWT, we often revisit the conservative treatment plan, tailoring it to the individual’s ongoing needs.
Q 24. What is your approach to managing a patient who is not responding to conservative treatment for plantar fasciitis?
When a patient isn’t responding to conservative treatment for plantar fasciitis, a multi-faceted approach is needed. I would first re-evaluate the diagnosis, ensuring we haven’t missed a different condition. Imaging (X-ray) can help rule out other issues like stress fractures. If the diagnosis remains plantar fasciitis, we explore other therapeutic options.
- Platelet-rich plasma (PRP) injections: This involves injecting concentrated platelets from the patient’s own blood into the affected area to stimulate tissue repair.
- Surgical intervention: In very rare and severe cases, surgical release of the plantar fascia may be considered. This is usually a last resort for individuals experiencing debilitating pain that hasn’t improved with other treatments.
- Referral to a pain management specialist: They can offer additional pain-management strategies, such as nerve blocks or other advanced techniques.
- More intensive physical therapy: We may need to modify or intensify the physical therapy program to include more advanced techniques or modalities to optimize treatment outcomes.
It’s critical to maintain open communication and collaboration with the patient throughout this process. The goal is to collaboratively develop a comprehensive plan that considers their lifestyle, activity level, and pain tolerance.
Q 25. Explain the role of corticosteroid injections in the management of plantar fasciitis.
Corticosteroid injections provide temporary relief from plantar fasciitis pain by reducing inflammation in the plantar fascia. They are usually reserved for cases where pain is severe and impacting daily life. However, I often use them cautiously because of potential long-term risks.
The benefits are short-term pain relief, allowing the patient to engage more actively in physical therapy. However, the risks include potential weakening or rupture of the plantar fascia, skin atrophy, local infection, nerve damage, and the risk of plantar fascia rupture is increased, possibly leading to chronic pain and disability. Moreover, the analgesic effect is usually temporary, and the underlying problem isn’t addressed. Therefore, I typically only recommend injections in selected cases of acute severe inflammation and always in conjunction with a comprehensive physical therapy program designed to address the underlying biomechanical issues. I usually discuss the limitations, risks, and the temporary nature of the pain relief with the patient to manage expectations appropriately.
Q 26. How do you counsel patients on the potential risks and benefits of different treatment options?
Counseling patients about treatment options is a crucial part of my practice. I always start by explaining the condition, its likely cause (often overuse or biomechanical issues), and its natural progression. Then, I present the various treatment options, highlighting the potential benefits and risks of each. This includes conservative management options such as rest, ice, stretching, orthotics, physical therapy, over-the-counter analgesics, and prescription NSAIDs, as well as more interventional options like corticosteroid injections and ESWT. I emphasize that surgery is generally a last resort.
For example, I’ll explain that while corticosteroid injections offer quick pain relief, they have a higher risk of weakening the plantar fascia in the long run. Similarly, I discuss the potential for temporary discomfort or bruising with ESWT. I provide each patient with decision aids, such as written materials or online resources, to complement our in-person conversations. The ultimate treatment plan is always made in collaboration with the patient, ensuring they understand their options and feel comfortable with their choice. Their active participation in the decision-making process is paramount.
Q 27. Describe your experience working with patients of different ages and activity levels.
My experience encompasses working with a wide range of patients across different age groups and activity levels. Older patients may present with chronic plantar fasciitis often related to age-related changes in foot biomechanics and reduced tissue elasticity. Younger, more active patients may have acute plantar fasciitis as a result of intense physical activity or inappropriate footwear.
Treatment strategies are tailored to individual needs. For example, a sedentary elderly patient might benefit most from orthotics, gentle stretching, and pain management strategies, whereas a young athlete might require a more aggressive approach involving physical therapy focused on strength and flexibility training, and possibly ESWT or even surgery if conservative treatment is unsuccessful. I’ve found it’s vital to understand each patient’s specific demands and expectations to provide personalized, effective care. I also adjust communication style to suit individual patients, being mindful that younger patients are often keen on understanding the evidence behind the recommendations, whereas older patients may prioritize simplicity and comfort.
Q 28. How do you stay up-to-date on the latest research and advancements in the treatment of heel spurs and plantar fasciitis?
Staying current in this rapidly evolving field requires ongoing commitment to continuing medical education. I regularly review peer-reviewed medical journals, such as the Journal of the American Podiatric Medical Association and Foot & Ankle International, for the latest research on plantar fasciitis and heel spur management.
I also participate in professional conferences and workshops, attend seminars and webinars, and actively engage with online communities of podiatrists and other healthcare professionals. Membership in professional organizations provides access to continuing education materials and keeps me abreast of best practices and current guidelines. By integrating these diverse resources, I’m able to refine my knowledge and improve my approach to patient care.
Key Topics to Learn for Heel Spur and Plantar Fasciitis Management Interview
- Anatomy and Biomechanics: Understanding the structures involved (plantar fascia, heel bone, surrounding muscles) and how they contribute to the condition.
- Etiology and Risk Factors: Identifying the causes of heel spurs and plantar fasciitis, including factors like overuse, obesity, and foot mechanics.
- Clinical Presentation and Diagnosis: Differentiating between heel spurs and plantar fasciitis, recognizing key symptoms, and understanding diagnostic methods (physical examination, imaging).
- Conservative Management: Mastering non-surgical treatment options, including rest, ice, stretching, orthotics, physical therapy, and medication.
- Surgical Management: Understanding the indications, techniques, and post-operative care for surgical interventions (e.g., plantar fasciotomy).
- Rehabilitation and Recovery: Developing comprehensive rehabilitation plans, including exercises, modalities, and patient education, to ensure optimal patient outcomes.
- Differential Diagnosis: Distinguishing heel spurs and plantar fasciitis from other conditions with similar symptoms (e.g., nerve entrapment, stress fractures).
- Patient Education and Communication: Effectively communicating with patients regarding diagnosis, treatment options, and expectations for recovery.
- Evidence-Based Practice: Applying the latest research and clinical guidelines to inform treatment decisions.
- Case Studies and Problem-Solving: Analyzing different case scenarios to develop appropriate diagnosis and management plans.
Next Steps
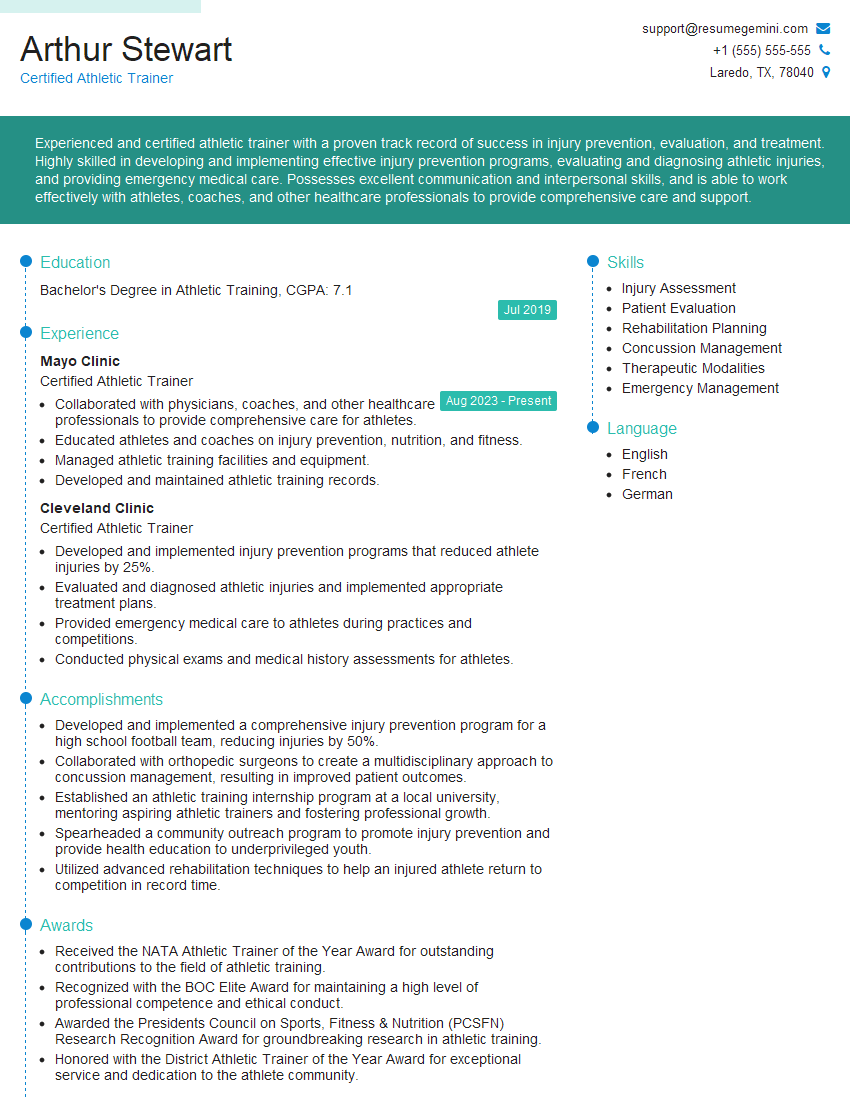
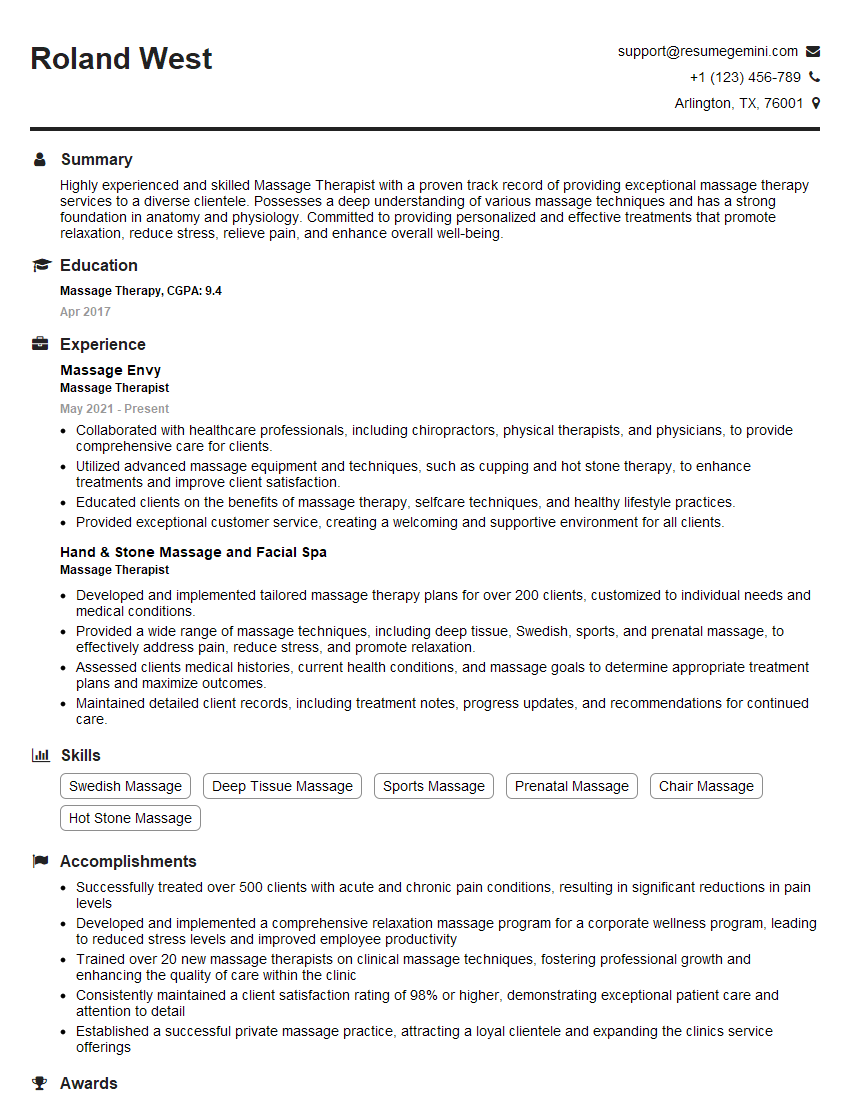
Mastering Heel Spur and Plantar Fasciitis Management is crucial for career advancement in podiatry, physical therapy, and related fields. A strong understanding of these conditions demonstrates clinical expertise and patient care capabilities, highly valued by employers. To significantly improve your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to your skills and experience. Examples of resumes specifically designed for candidates in Heel Spur and Plantar Fasciitis Management are available to help you showcase your expertise effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.