Are you ready to stand out in your next interview? Understanding and preparing for Hospital Care interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Hospital Care Interview
Q 1. Describe your experience with Electronic Health Records (EHR) systems.
My experience with Electronic Health Records (EHR) systems spans over eight years, encompassing various systems like Epic, Cerner, and Meditech. I’m proficient in using EHRs for patient registration, charting, medication ordering, and accessing lab results. I understand the importance of data integrity and adhering to HIPAA regulations regarding patient privacy. For example, in a previous role, I utilized Epic to streamline the admission process for trauma patients, significantly reducing wait times and improving the efficiency of our emergency department. I’m also adept at using EHR reporting tools to analyze trends and improve care delivery. Further, I am familiar with various EHR functionalities including clinical documentation, order entry, and result management, understanding the impact of appropriate and accurate data entry on patient safety and clinical decision-making.
Q 2. Explain the process of administering medication safely.
Safe medication administration is a multi-step process crucial for patient safety. It begins with verifying the physician’s order against the patient’s allergies and medical history. Next, I perform the ‘five rights’ check: right patient, right medication, right dose, right route, and right time. Before administering the medication, I visually inspect the medication for any discrepancies, double-checking the label against the order. Following administration, I document the time, route, dose, and patient’s response in the EHR. If there are any unusual reactions or challenges during the process, I immediately report them to the supervising physician. For instance, I once noticed a discrepancy in the dosage of a medication prescribed for a patient with renal impairment. By identifying this error before administration, I prevented a potentially serious adverse event. This exemplifies the importance of meticulous attention to detail and adherence to established protocols.
Q 3. How do you prioritize patient care in a high-pressure environment?
Prioritizing patient care in a high-pressure environment requires a structured approach. I utilize a system based on urgency and acuity, focusing first on patients with life-threatening conditions. This involves identifying those who need immediate attention (e.g., cardiac arrest, respiratory distress) and delegating tasks effectively to the team. For instance, during a busy shift, I might triage patients based on the ABCDE system (Airway, Breathing, Circulation, Disability, Exposure) directing the attention of the team towards those with critical airway issues first. Then, I use clinical judgment, prioritizing tasks based on the potential for harm or impact on the patient’s overall well-being. Using a combination of time management techniques and team collaboration keeps the care efficient and patient-focused.
Q 4. What is your approach to handling a medical emergency?
My approach to handling medical emergencies is rooted in a calm and systematic response. The first step is rapid assessment of the situation using a standardized approach to evaluate the patient’s condition. This is followed by initiating immediate life support measures, such as CPR or administering oxygen, based on the patient’s needs. Simultaneously, I will alert the appropriate medical team (e.g., Rapid Response Team, Code Blue team), clearly communicating the patient’s condition and necessary interventions. After the immediate crisis is stabilized, I ensure thorough documentation of all actions taken and the patient’s response, and follow up with subsequent monitoring and treatment as required. For example, in a scenario involving a patient experiencing anaphylactic shock, immediate administration of epinephrine was critical in stabilizing the patient before the arrival of the emergency medical services. This illustrates the need for quick, decisive action and clear communication during emergencies.
Q 5. Describe your experience with patient assessment and charting.
Patient assessment and charting are integral to providing high-quality care. I begin by collecting comprehensive data through a combination of observation, physical examination, and patient interview, thoroughly documenting findings in the EHR using standardized terminology and medical codes. This includes recording vital signs, symptoms, allergies, medical history, and any relevant social determinants of health. For example, when assessing a patient with chest pain, I document the characteristics of the pain, its location, radiation, and any associated symptoms. Accurate charting is crucial not only for providing continuity of care, but also for legal protection and for supporting effective communication between healthcare providers involved in the patient’s care. My approach includes using objective data and ensuring comprehensive charting of any interventions and patient response.
Q 6. How do you communicate effectively with patients and their families?
Effective communication is paramount in building trust with patients and their families. I practice active listening, ensuring that patients feel heard and understood. I use clear, concise language, avoiding medical jargon whenever possible. I explain medical information in a way that’s easy to comprehend, tailored to their individual level of understanding. I also involve family members as appropriate, empowering them to participate in decision-making and ensuring they are well-informed. For instance, when explaining a complex diagnosis to a patient and their family, I used visual aids and simple analogies to enhance comprehension. This approach fosters a collaborative relationship and builds trust, leading to a better overall patient experience and compliance with treatment plans.
Q 7. Explain your understanding of infection control protocols.
My understanding of infection control protocols is comprehensive, encompassing standard precautions, contact, droplet, and airborne isolation techniques. I am adept at using personal protective equipment (PPE) appropriately, including gloves, gowns, masks, and eye protection, based on the specific infection risk. I adhere to strict hand hygiene practices, using alcohol-based hand rubs and performing thorough handwashing according to established guidelines. I also maintain a clean and disinfected work environment and follow proper procedures for handling contaminated materials and waste disposal. My commitment to infection control extends to education, educating patients and their families about ways to reduce infection risk. In summary, infection prevention is a continuous process that requires rigorous adherence to guidelines and continuous improvement in practice.
Q 8. Describe your experience with wound care.
My wound care experience spans over eight years, encompassing a wide range of wound types and treatment modalities. I’ve worked extensively with acute and chronic wounds, including pressure ulcers, diabetic foot ulcers, surgical wounds, and traumatic injuries. My approach is always holistic, considering the patient’s overall health, comorbidities, and lifestyle factors.
I’m proficient in various wound assessment techniques, from visual inspection and palpation to the use of specialized tools like measuring wound dimensions and assessing tissue viability. This allows me to accurately stage the wound and determine the best course of treatment. For example, I’ve successfully managed a complex case of a diabetic foot ulcer that required meticulous debridement, negative pressure wound therapy (NPWT), and advanced dressings. This patient required close monitoring for infection and careful management of blood sugar levels, highlighting the interconnectedness of wound care and overall patient health.
I’m also experienced in educating patients and their families on proper wound care at home, ensuring a smooth transition from hospital to home environment. This includes demonstrating proper dressing changes, hygiene practices, and recognizing signs of infection. My goal is always to empower patients to actively participate in their healing process.
Q 9. How do you manage conflict with colleagues or patients?
Conflict resolution is a crucial skill in healthcare. My approach is always based on open communication, empathy, and a focus on finding mutually beneficial solutions. When conflict arises with colleagues, I initiate a calm and respectful conversation, actively listening to their perspective before explaining my own. I aim to identify the root cause of the disagreement and collaboratively explore possible resolutions. For example, a recent disagreement regarding patient care protocols was resolved through a team meeting where we discussed the evidence-based rationale for different approaches and reached a consensus based on best practices.
With patients, I prioritize empathy and understanding. I actively listen to their concerns, validate their feelings, and explain my actions clearly and patiently. If a patient expresses dissatisfaction, I try to understand the source of their frustration and collaboratively work towards a solution that respects their wishes and aligns with medical best practices. I always ensure they feel heard and respected, even if we cannot accommodate every request.
Q 10. How do you stay updated on the latest medical advancements?
Staying current with medical advancements is essential in healthcare. I utilize several strategies to stay updated, including:
- Professional memberships: I’m an active member of professional organizations like [Mention Relevant Professional Organizations e.g., The American Nurses Association, etc.], which provide access to journals, conferences, and continuing education opportunities.
- Medical journals and publications: I regularly review reputable medical journals such as The New England Journal of Medicine and The Lancet to stay informed about the latest research and clinical trials.
- Conferences and workshops: Attending medical conferences and workshops allows me to engage directly with experts and learn about cutting-edge technologies and treatment modalities.
- Online resources and continuing education courses: I utilize online platforms offering CME (Continuing Medical Education) credits and updated guidelines on various medical practices.
This multifaceted approach ensures that I maintain a high level of competency and provide my patients with the most up-to-date and evidence-based care.
Q 11. Describe your experience with different types of medical equipment.
Throughout my career, I’ve gained extensive experience with a variety of medical equipment, including:
- Monitoring devices: I’m proficient in using and interpreting data from vital signs monitors, ECG machines, and pulse oximeters.
- Infusion pumps and ventilators: I’m skilled in operating and troubleshooting infusion pumps and ventilators, ensuring safe and effective medication delivery and respiratory support.
- Wound care equipment: My experience includes using advanced wound care devices like NPWT (Negative Pressure Wound Therapy) systems and various types of dressings and topical agents.
- Imaging equipment: I’m familiar with interpreting basic imaging results such as X-rays and understanding their implications for patient care.
My familiarity with these devices extends beyond basic operation; I understand their limitations and potential risks and always prioritize patient safety when using them. I’m also adept at troubleshooting minor malfunctions and escalating issues as needed.
Q 12. What is your experience with patient education?
Patient education is an integral part of my practice. I believe that informed patients are empowered patients. My approach to patient education is tailored to each individual’s learning style, health literacy, and cultural background. I use a combination of verbal explanations, visual aids, and written materials to ensure that information is clearly understood.
For example, when educating a patient about diabetes management, I would explain the disease process in simple terms, demonstrate proper insulin administration techniques, and provide written instructions with diagrams. I always allow time for questions and encourage active participation to ensure understanding. Following discharge, I provide patients with clear and concise instructions to ensure successful transition to home care. My goal is to equip patients with the knowledge and skills they need to manage their health effectively.
Q 13. How do you handle difficult or emotionally charged situations?
Handling difficult or emotionally charged situations requires a combination of empathy, professionalism, and effective communication skills. My approach involves:
- Active listening: I listen carefully to the patient or family member’s concerns, validating their feelings without judgment.
- Empathy and compassion: I strive to understand their perspective and respond with empathy and compassion.
- Clear and concise communication: I explain medical information and treatment plans clearly and concisely, using language that is easy to understand.
- Collaboration: I work collaboratively with the patient and family to develop a plan that addresses their concerns while respecting medical best practices.
- Seeking support: If the situation is beyond my scope of practice, I seek guidance and support from senior colleagues or other members of the healthcare team.
For instance, I’ve had to deal with grieving family members after the loss of a loved one. In these situations, my focus is on offering comfort, support, and honest communication, while respecting the family’s wishes and ensuring they have the resources they need.
Q 14. Describe your experience with discharge planning.
Discharge planning is a critical aspect of hospital care that ensures a safe and smooth transition for the patient from the hospital to their home or other care setting. My experience encompasses comprehensive discharge planning, encompassing:
- Assessment of patient needs: I conduct a thorough assessment of the patient’s physical, cognitive, and emotional needs to identify any potential challenges upon discharge.
- Collaboration with interdisciplinary team: I collaborate closely with physicians, nurses, social workers, therapists, and other healthcare professionals to develop an individualized discharge plan.
- Coordination of services: I coordinate necessary home healthcare services, such as medication delivery, wound care, physical therapy, and home health aides.
- Patient and family education: I provide comprehensive education to the patient and their family regarding medication management, wound care, follow-up appointments, and potential complications.
- Follow-up arrangements: I arrange for appropriate follow-up appointments with specialists or primary care physicians.
A successful discharge plan minimizes the risk of readmission and ensures a positive patient experience after leaving the hospital. For instance, a recent discharge plan for a patient recovering from a stroke included arranging for home health physical therapy, occupational therapy, and speech therapy, along with setting up regular follow-up appointments with neurology and cardiology.
Q 15. What is your understanding of HIPAA regulations?
HIPAA, the Health Insurance Portability and Accountability Act, is a US federal law designed to protect sensitive patient health information. It sets national standards for the privacy, security, and transmission of electronic protected health information (ePHI). My understanding encompasses its three core components: the Privacy Rule, the Security Rule, and the Breach Notification Rule. The Privacy Rule dictates how protected health information can be used, disclosed, and protected. The Security Rule outlines administrative, physical, and technical safeguards to ensure ePHI security. The Breach Notification Rule mandates timely notification in the event of a data breach. In essence, HIPAA ensures patient confidentiality and accountability within the healthcare system.
Understanding HIPAA is crucial for ethical and legal practice. For instance, I know that before discussing a patient’s case with anyone outside the direct care team, I must obtain proper authorization, unless exceptions like mandated reporting apply. Failure to comply with HIPAA can lead to serious legal and professional consequences.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure patient confidentiality?
Ensuring patient confidentiality is paramount in healthcare. My approach is multi-faceted. First, I strictly adhere to HIPAA regulations, ensuring that I only access and share patient information necessary for direct care and with appropriate authorization. Second, I utilize secure communication channels for exchanging patient data. This includes using encrypted email, secure messaging systems, and adhering to organizational policies concerning electronic health records (EHRs). Third, I maintain a physically secure work environment, ensuring that patient records are stored properly and access is limited to authorized personnel. Finally, I am meticulous in disposing of any physical patient information, using secure shredding methods. For example, if I inadvertently print a patient’s chart, I immediately shred the document and report the incident. Maintaining confidentiality goes beyond technical measures; it also involves fostering a culture of trust and respect within the healthcare team.
Q 17. How do you contribute to a positive team environment?
I contribute to a positive team environment by actively participating in teamwork, effective communication, and mutual respect. I believe in open and honest communication, readily sharing information and expertise with colleagues while being receptive to their input. I actively listen during team meetings and offer constructive suggestions. I also proactively offer support to colleagues facing heavy workloads or challenging situations. I recall one instance where a junior nurse was struggling with a complex procedure. I patiently guided her through the steps, providing encouragement and feedback, which not only helped her complete the procedure successfully but also fostered a sense of trust and collaboration. Creating a positive team dynamic involves a commitment to collaboration, support, and mutual respect, leading to a safer and more efficient healthcare environment.
Q 18. Describe a time you had to make a difficult decision regarding patient care.
I once had to make a difficult decision regarding a patient’s treatment plan. The patient, an elderly woman with advanced dementia, experienced a fall resulting in a hip fracture. The surgical risk was high due to her age and overall health. Her family was divided on whether to proceed with surgery or opt for palliative care. I facilitated a family meeting involving the physician, social worker, and family members to carefully discuss the risks, benefits, and alternatives of both surgical and non-surgical options. We considered her quality of life and her expressed wishes (as best we could determine them). The process involved empathetic listening and providing them with factual medical information in a way that was understandable and respectful. Ultimately, the family decided on palliative care, a decision that, while difficult, prioritized the patient’s comfort and well-being. This experience reinforced the importance of patient-centered care and shared decision-making in complex medical situations.
Q 19. How do you handle stressful situations in the workplace?
Stressful situations are inevitable in healthcare. My approach involves a combination of proactive strategies and coping mechanisms. Proactively, I prioritize time management, delegating tasks effectively, and maintaining clear communication with my team. When stress arises, I utilize techniques such as deep breathing exercises and mindfulness to manage my emotional response. I also rely on my support network, which includes colleagues and supervisors. Openly discussing challenges and seeking support helps to alleviate pressure and find constructive solutions. If the stress persists, I utilize resources offered by my employer such as employee assistance programs (EAPs). This approach ensures that I can effectively manage stress without compromising patient care or my own well-being.
Q 20. Describe your experience with pain management.
My experience with pain management encompasses both acute and chronic pain scenarios. I have worked with various pain management modalities, including pharmacological interventions (analgesics, opioids, adjuvants), non-pharmacological methods (physical therapy, heat/cold therapy, relaxation techniques), and interdisciplinary approaches involving pain specialists and other healthcare professionals. I understand the importance of individualizing pain management plans, taking into account the patient’s specific condition, medical history, and personal preferences. This involves assessing the nature and intensity of the pain using validated pain scales and thoroughly documenting the patient’s response to different treatment options. A crucial aspect is ongoing communication with the patient and their family to evaluate the effectiveness of the pain management plan and adjust accordingly. For example, I’ve helped patients navigate the challenges of opioid use, emphasizing the importance of adherence to prescribed regimens and strategies to manage potential side effects.
Q 21. How do you identify and respond to patient deterioration?
Identifying and responding to patient deterioration requires a proactive and systematic approach. I utilize early warning scoring systems (e.g., MEWS, NEWS2) to continuously monitor patients’ vital signs and other indicators of physiological instability. Regular assessment of the patient’s condition, paying attention to subtle changes in their mental status, respiratory effort, oxygen saturation, and urine output is crucial. If I notice any signs of deterioration, I immediately notify the physician and follow established protocols for escalation of care. This may involve administering emergency medications, initiating respiratory support, or transferring the patient to a higher level of care. Effective communication with the physician and other members of the care team is crucial to ensure timely and coordinated intervention. For example, if a patient exhibits signs of sepsis, I would immediately report this to the physician, initiating intravenous fluids, antibiotics, and other supportive measures as directed. Proactive monitoring and timely response to subtle changes are critical in preventing adverse outcomes.
Q 22. What is your experience with end-of-life care?
End-of-life care is a multifaceted aspect of hospital care focusing on providing comfort, dignity, and support to patients in their final stages of life, as well as their families. My experience encompasses working with patients and families facing terminal illnesses, offering emotional support, managing pain and symptoms, and facilitating open communication about end-of-life wishes. This includes collaborating with interdisciplinary teams, including palliative care specialists, chaplains, and social workers, to create holistic care plans. For example, I once worked with a patient with advanced cancer who was deeply concerned about leaving unfinished business with their family. We facilitated several family meetings, allowing for open communication and reconciliation, which brought significant peace to the patient in their final days. Another example involved managing the symptoms of a patient with severe respiratory distress, ensuring their comfort through medication and breathing support. I believe providing compassionate and attentive care during this difficult time is crucial for both the patient and their loved ones.
Q 23. How do you manage a patient with challenging behavior?
Managing patients with challenging behavior requires a patient-centered, multi-pronged approach. Understanding the root cause of the behavior is paramount. This often involves assessing for pain, medication side effects, cognitive impairment, or underlying psychological distress. For example, a patient experiencing delirium post-surgery may exhibit agitation and confusion. Addressing pain, ensuring adequate hydration and rest, and creating a calm, familiar environment can significantly improve behavior. In other cases, underlying psychiatric conditions need to be addressed in collaboration with a psychiatrist. Clear, consistent communication is essential; using simple language, providing choices when possible, and ensuring patient safety are crucial. De-escalation techniques, like active listening and empathy, are valuable tools. If behavior escalates, involving security personnel while maintaining patient dignity and safety is necessary. Ultimately, effective management requires a tailored approach based on the individual patient’s needs and circumstances. Proper documentation of the behavior, interventions, and responses is vital for continuity of care.
Q 24. Describe your experience with different types of medical emergencies.
My experience encompasses a wide range of medical emergencies, including cardiac arrests, strokes, severe allergic reactions, respiratory distress, trauma cases, and septic shock. Each emergency demands rapid assessment, prioritization of interventions, and effective teamwork. For instance, during a cardiac arrest, my role involved initiating CPR, assisting with defibrillation, and maintaining airway patency until the arrival of the emergency response team. In a stroke case, my actions focused on rapidly identifying stroke symptoms, contacting the stroke team for neuroimaging, and managing vital signs. In managing severe allergic reactions, prompt administration of epinephrine was crucial, followed by close monitoring for anaphylaxis. Effective communication with the medical team, nurses, and other supporting staff is vital in these situations. My experience has solidified my ability to work under pressure, prioritize effectively, and remain calm in highly stressful circumstances.
Q 25. How do you handle a disagreement with a physician?
Disagreements with physicians are inevitable in a collaborative healthcare environment. However, addressing these disagreements professionally and constructively is crucial. I believe in open and respectful communication. I typically start by seeking clarification on the point of disagreement, ensuring a complete understanding of the physician’s perspective. I clearly and concisely express my concerns, supporting my statements with evidence-based practices or relevant patient data. If the disagreement persists, I seek mediation from a senior physician or manager to facilitate a productive conversation and arrive at a mutually agreeable solution that prioritizes patient safety and well-being. Transparency and maintaining a collaborative spirit are key to resolving conflicts effectively.
Q 26. How do you ensure accuracy in medication administration?
Ensuring medication accuracy is a cornerstone of safe patient care. My approach involves rigorous adherence to the five rights of medication administration: right patient, right medication, right dose, right route, and right time. I meticulously check the medication order against the patient’s identification band and chart before administration. I double-check the medication label three times, and I clarify any ambiguities with the physician or pharmacist. I am adept at using barcode scanning technology to verify medication and patient data. Prior to administration, I explain the medication’s purpose and side effects to the patient, addressing any concerns they may have. After administration, I meticulously document the medication, time, dose, route, and patient’s response. Careful attention to detail and adherence to established protocols are essential in preventing medication errors.
Q 27. How do you manage your time effectively in a busy hospital setting?
Effective time management in a busy hospital setting is essential. My approach involves prioritizing tasks based on urgency and importance, focusing on immediate patient needs first. I use organizational tools such as to-do lists and task-management apps to schedule my day efficiently and track progress. I frequently re-evaluate my schedule throughout the day, adapting to unexpected changes. I prioritize teamwork and delegation when appropriate, collaborating with colleagues to efficiently manage tasks and patient care. Continuous self-reflection and refinement of my time management strategies allow me to adapt and work effectively in the dynamic hospital environment. Being proactive, anticipating needs, and preventing bottlenecks are crucial for maximizing productivity.
Q 28. Describe your experience with quality improvement initiatives.
I have been actively involved in several quality improvement initiatives. For example, I participated in a project aimed at reducing hospital-acquired infections by implementing stricter hand hygiene protocols and promoting the use of evidence-based infection control measures. This involved data collection, analysis, and the development of targeted interventions. Another initiative focused on improving patient satisfaction scores by enhancing communication and providing more patient-centered care. My contributions to these projects involved actively participating in brainstorming sessions, implementing changes, and evaluating outcomes through data analysis. I am passionate about applying evidence-based practices to improve the quality and safety of patient care. My commitment to continuous improvement drives me to seek out opportunities to enhance processes and outcomes within the hospital setting.
Key Topics to Learn for Hospital Care Interview
- Patient Care Fundamentals: Understanding patient assessment, monitoring, and basic nursing procedures. Practical application includes describing your experience with vital sign monitoring and recognizing deteriorating patient conditions.
- Hospital Workflow & Teamwork: Knowledge of hospital processes, including admission, discharge, and transfer procedures; emphasize effective communication and collaboration within a multidisciplinary team. Consider exploring case studies demonstrating successful teamwork in challenging situations.
- Medical Terminology & Abbreviations: Demonstrate familiarity with common medical terms and abbreviations used in hospital settings. Practical application includes accurately interpreting and documenting patient information.
- Infection Control & Safety Protocols: Understanding and applying infection control principles, including hand hygiene, personal protective equipment (PPE) usage, and adherence to safety regulations. Problem-solving examples might include describing how you’ve handled a potential infection control breach.
- Ethical Considerations & Legal Aspects: Familiarity with relevant ethical guidelines and legal implications in hospital care, such as patient confidentiality and informed consent. Explore case studies that highlight ethical dilemmas and their resolutions.
- Technology & Medical Equipment: Demonstrate basic understanding of commonly used medical equipment and electronic health record (EHR) systems. Practical application includes describing your experience with EHR software or specific medical devices.
- Emergency Response & Crisis Management: Understanding protocols for responding to medical emergencies and handling crisis situations. Consider scenarios and your approach to problem-solving in high-pressure environments.
Next Steps
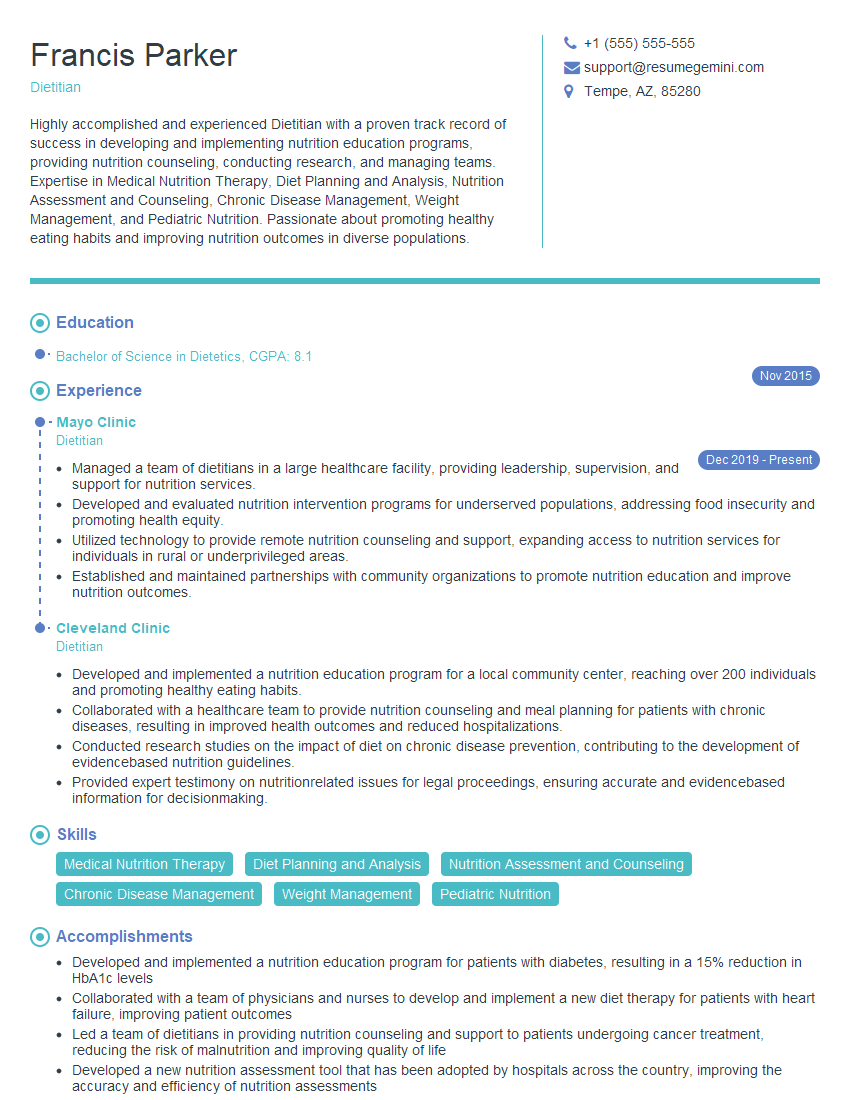
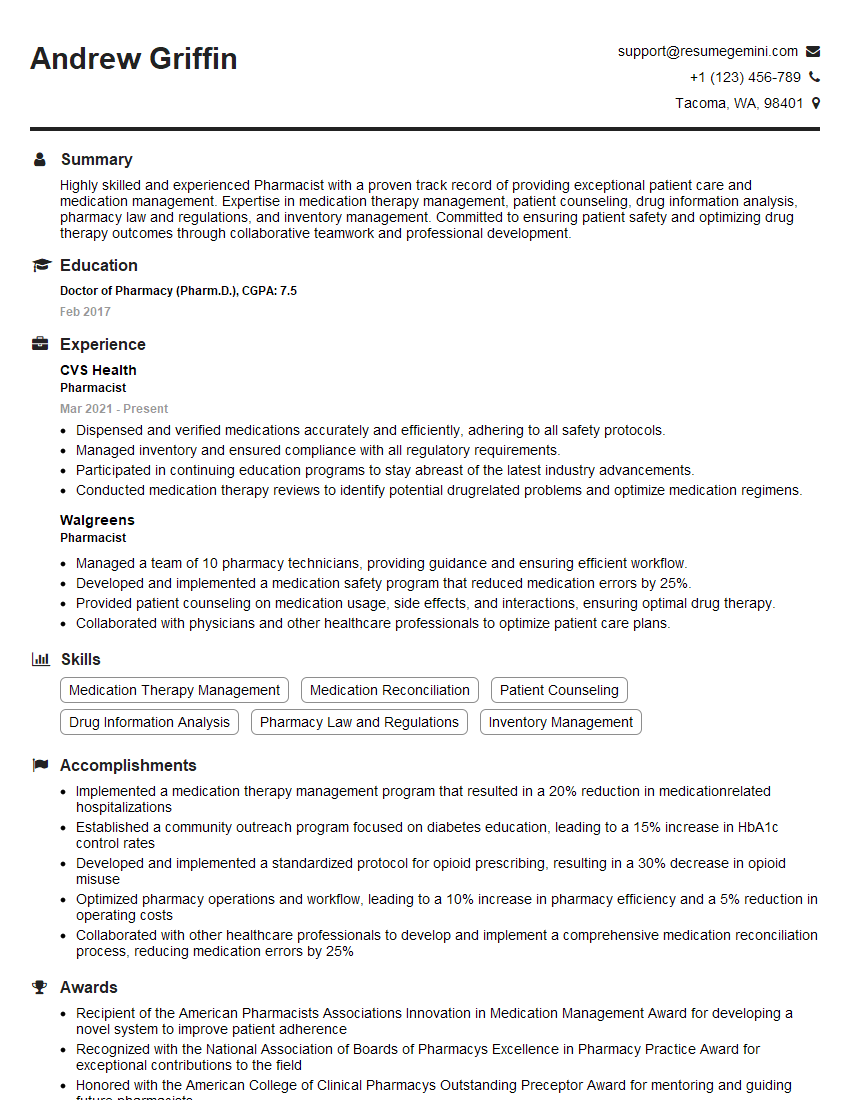
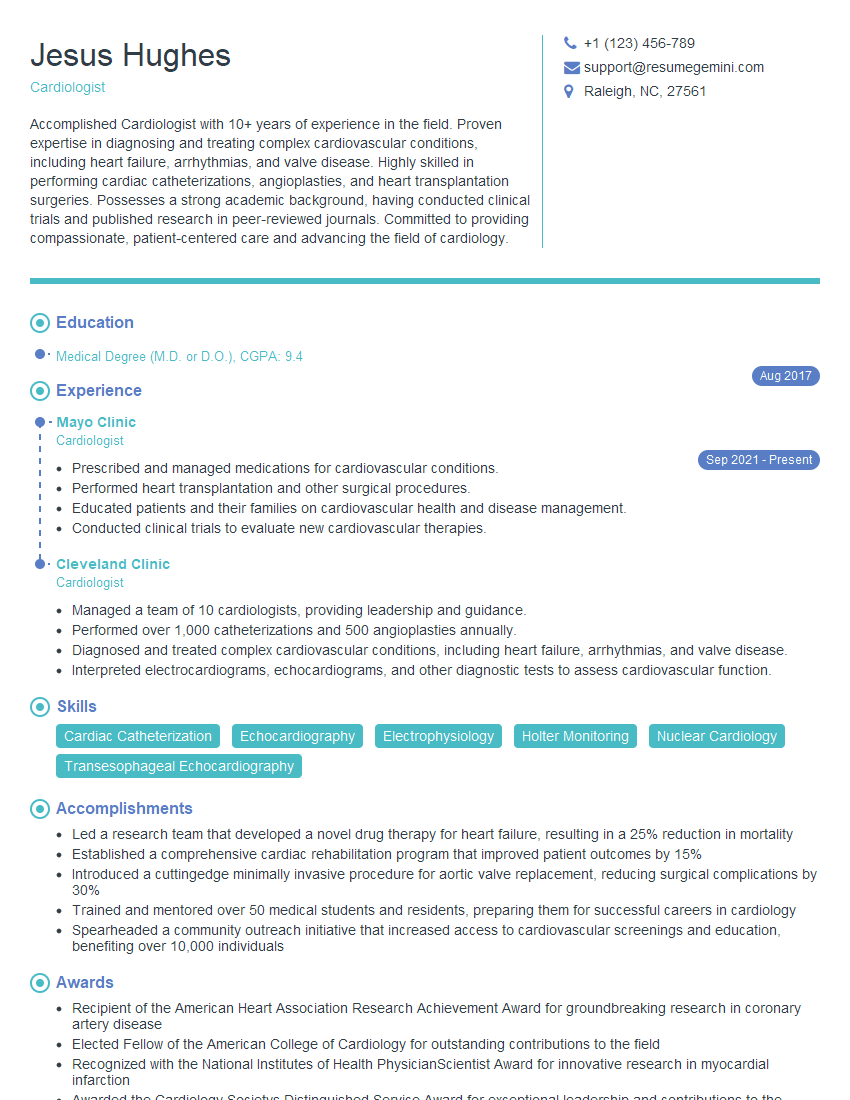
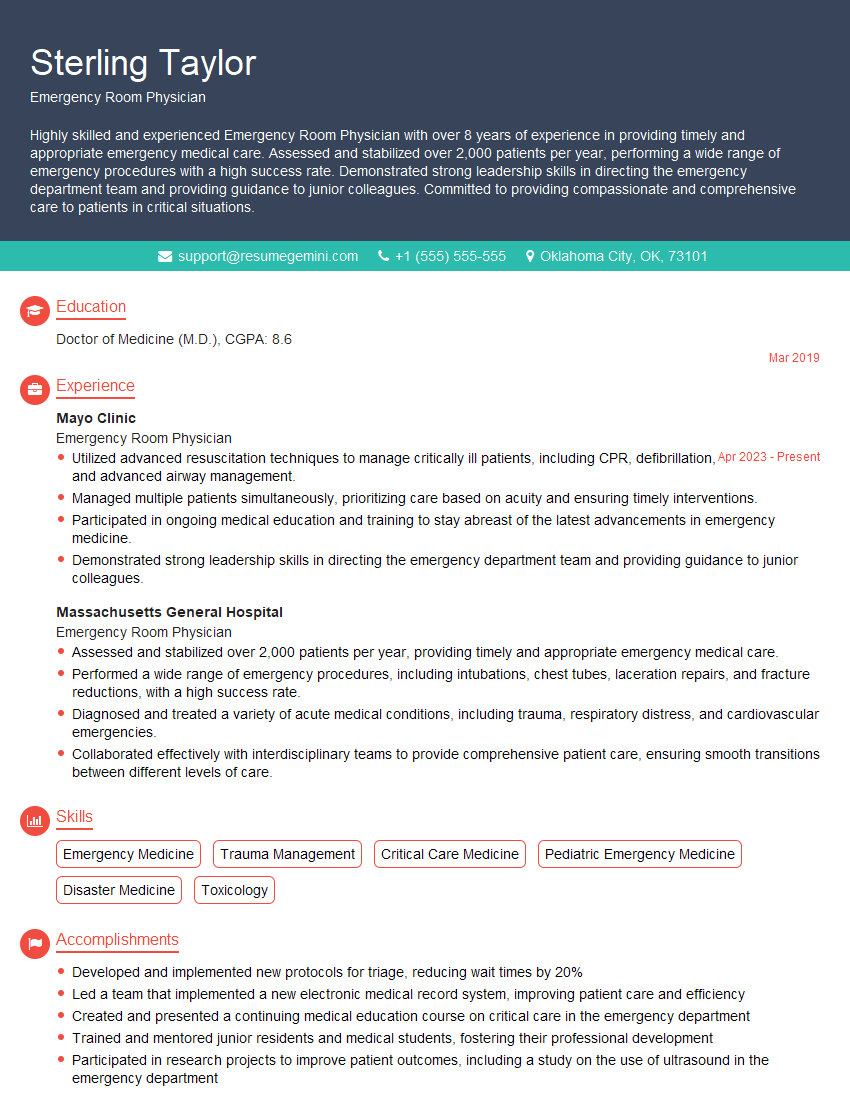
Mastering the intricacies of Hospital Care opens doors to rewarding and impactful careers in healthcare. To maximize your job prospects, crafting a compelling and ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional resume that showcases your skills and experience effectively. We provide examples of resumes tailored to Hospital Care to help you create a document that truly stands out. Invest time in refining your resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.