Unlock your full potential by mastering the most common Knowledge of ethical considerations in epilepsy management interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Knowledge of ethical considerations in epilepsy management Interview
Q 1. Describe the ethical considerations surrounding informed consent in epilepsy surgery.
Informed consent in epilepsy surgery is a cornerstone of ethical practice. It means the patient understands the risks, benefits, and alternatives to surgery, and freely chooses to proceed. This requires a multi-faceted approach.
- Capacity Assessment: We must first ensure the patient has the mental capacity to understand the information presented. This might involve assessing their cognitive function, considering the impact of their epilepsy on their decision-making, and potentially involving a neuropsychologist.
- Information Provision: We need to explain the surgical procedure in clear, non-technical language, tailored to the patient’s understanding. This includes discussing potential benefits (e.g., seizure reduction, improved quality of life), risks (e.g., bleeding, infection, neurological deficits), and the possibility of no improvement. We also explain alternative treatments, like medication or vagus nerve stimulation.
- Documentation: Meticulous documentation is crucial. This includes recording the discussions, ensuring the patient has had adequate time to ask questions, and confirming their understanding before obtaining their signature on the consent form. A witness should also be present.
- Ongoing Dialogue: Consent isn’t a one-time event. We should maintain open communication with the patient throughout the process, addressing any new concerns or questions they may have. This ensures the patient’s continued willingness to proceed.
For instance, if a patient with complex partial seizures is considering surgery, we need to fully explain the intricacies of the procedure, the potential for cognitive side effects, and the chance of surgery failing to achieve seizure freedom. We’d also discuss the ongoing need for medication post-surgery.
Q 2. Explain the ethical implications of disclosing a patient’s epilepsy diagnosis to third parties.
Disclosing a patient’s epilepsy diagnosis to third parties is ethically complex and governed by strict confidentiality rules. Generally, disclosure is only justified in limited circumstances, prioritizing patient autonomy and safety.
- Patient Consent: Unless the patient explicitly consents to disclosure, we should not share their diagnosis with anyone, even family members. There might be exceptions, such as when the patient lacks capacity and a family member is their legal guardian.
- Mandatory Reporting: In some situations, legal requirements might mandate disclosure. For example, if a patient’s seizures pose an imminent risk to themselves or others (e.g., driving), we may be obligated to inform relevant authorities.
- Protection from Harm: If a patient’s condition poses a serious risk to themselves or others, we may need to disclose information to protect them, even without explicit consent. This usually involves careful consideration and consultation with legal and ethical review boards.
For example, if a patient with uncontrolled seizures insists on driving, and we believe this poses a significant risk to public safety, we may be legally and ethically obligated to inform the relevant licensing authorities. However, we’d always try to engage the patient in a conversation to mitigate the risk before taking such a step.
Q 3. How would you address a conflict between a patient’s wishes and their family’s concerns regarding epilepsy treatment?
Conflicts between a patient’s wishes and their family’s concerns are challenging. The patient’s autonomy should always be respected as the primary ethical consideration, but we need to facilitate open communication and find a resolution that respects everyone’s values.
- Mediation: We act as a neutral facilitator, encouraging open communication between the patient and their family. We help them understand each other’s perspectives and concerns.
- Shared Decision-Making: We encourage a shared decision-making model. This involves presenting all treatment options, their risks and benefits, and exploring how each option aligns with the patient’s goals and the family’s concerns.
- Ethical Consultation: In complex cases, we may seek guidance from an ethics committee or other expert professionals. They can provide an objective perspective and help navigate ethical dilemmas.
- Legal Considerations: If the conflict is irresolvable, legal intervention may be necessary. This is rare, but could be necessary if the family’s concerns significantly impact the patient’s treatment or well-being.
For example, if a patient with well-controlled epilepsy refuses surgery despite their family’s strong belief that it’s necessary, we would thoroughly explore the patient’s reasons for refusal. We would also work with the family to understand their concerns, ensuring everyone understands the risks and benefits of surgery. Our goal would be to reach a consensus, while respecting the patient’s right to self-determination.
Q 4. What are the ethical considerations related to the use of cannabis for epilepsy treatment?
The use of cannabis for epilepsy treatment raises several ethical considerations. While some evidence suggests potential benefits, its use is complex and requires careful ethical navigation.
- Lack of Rigorous Evidence: The scientific evidence supporting the efficacy and safety of cannabis for epilepsy is still evolving. This means treatment decisions should be made cautiously, with a focus on patient safety and well-being.
- Legal and Regulatory Issues: The legal status of cannabis varies widely, creating challenges in access, quality control, and potential legal ramifications for both patients and physicians.
- Potential Side Effects: Cannabis use carries potential side effects, including cognitive impairment, psychosis, and addiction. These risks need to be carefully weighed against the potential benefits, particularly in vulnerable populations.
- Informed Consent: Patients must be fully informed about both the potential benefits and risks of cannabis use, including the lack of comprehensive clinical trial data. Consent must be voluntary and informed.
For example, if a patient requests cannabis as a treatment, we must engage in a detailed discussion about the limited evidence, the potential risks, and the availability of alternative treatments. We would also highlight the lack of FDA approval and the varying legal landscape. The patient’s decision must be fully informed and respected.
Q 5. Discuss the ethical challenges of managing medication side effects in epilepsy patients.
Managing medication side effects in epilepsy patients presents significant ethical challenges. The goal is to balance seizure control with minimizing adverse effects, recognizing the impact on the patient’s quality of life.
- Prioritizing Patient Well-being: The patient’s overall well-being, including their physical and psychological health, should be paramount. We must consider the impact of side effects on daily living, relationships, and emotional state.
- Shared Decision-Making: We should actively involve the patient in decisions regarding medication adjustments, balancing seizure control with tolerability of side effects. This requires open communication and empathy.
- Monitoring and Assessment: Regular monitoring for side effects is crucial, using validated assessment tools to track their severity and impact on the patient’s life. This allows for timely adjustments to the treatment plan.
- Ethical Considerations of Medication Changes: Decisions regarding medication changes must consider the balance between potential benefits and risks. Sometimes, reducing medication dosage might increase seizure frequency, requiring careful consideration and communication with the patient.
For example, if a patient experiences significant cognitive side effects from a particular anti-epileptic drug, we might need to explore alternative medications, even if it means slightly compromising seizure control. We’d involve the patient in the decision-making process, weighing their priorities against the potential risks and benefits of each option.
Q 6. How do you ensure patient confidentiality when discussing epilepsy management?
Ensuring patient confidentiality when discussing epilepsy management is critical. We adhere to strict professional guidelines and regulations to protect sensitive information.
- HIPAA Compliance (or equivalent): In the US, HIPAA regulations strictly govern the handling of protected health information (PHI). We follow all relevant regulations to ensure confidentiality.
- Data Security: We use secure electronic health records (EHRs) and implement measures to prevent unauthorized access to patient data. Paper records are stored securely, following institutional guidelines.
- Limited Disclosure: We only share information with individuals directly involved in the patient’s care, such as other healthcare professionals involved in their treatment, and only with the patient’s consent or when legally mandated.
- Privacy in Conversations: We always conduct conversations about epilepsy management in private settings, ensuring no unauthorized individuals can overhear sensitive information.
For example, we would never discuss a patient’s diagnosis or treatment plan in a public area, or with anyone not directly involved in their care. All communication would be through secure channels and with appropriate authorization.
Q 7. Explain the ethical considerations related to the use of Vagus Nerve Stimulation (VNS) for epilepsy.
Vagus nerve stimulation (VNS) for epilepsy presents several ethical considerations, primarily surrounding informed consent and balancing benefits against potential risks.
- Informed Consent: Patients must fully understand the procedure’s complexities, including the surgical risks, the potential for side effects (e.g., voice changes, cough, pain), and the possibility of limited efficacy. They also need to understand that VNS is not a cure, but an adjunctive therapy.
- Benefit-Risk Assessment: A careful assessment of the potential benefits of VNS versus the risks and side effects is essential. This assessment should involve shared decision-making with the patient, considering their values and preferences.
- Resource Allocation: VNS is a relatively expensive therapy. Ethical considerations arise regarding resource allocation and ensuring equitable access for all patients who could benefit.
- Long-Term Follow-up: Ethical considerations extend to long-term follow-up and ongoing assessment of the device’s effectiveness and the management of any side effects. This is important to ensure the treatment remains beneficial and safe over time.
For instance, we must carefully explain to a patient considering VNS that while it might reduce seizure frequency, it won’t eliminate seizures entirely. We must also discuss potential side effects like hoarseness and throat discomfort, and obtain their informed consent for the procedure after thoroughly answering all their questions.
Q 8. Describe the ethical implications of using invasive monitoring techniques in epilepsy diagnosis.
Invasive monitoring techniques, such as intracranial EEG (iEEG), are crucial for localizing seizure foci in epilepsy patients who haven’t responded to other diagnostic methods. However, these procedures carry significant ethical implications. The most prominent is the risk-benefit ratio. While iEEG can provide invaluable information leading to potentially curative surgery, it involves inserting electrodes into the brain, which carries risks of bleeding, infection, and even neurological damage. Informed consent becomes paramount. Patients must fully understand the procedure, including its benefits, risks, and alternatives, before giving their consent. This necessitates clear, transparent communication from the medical team, using language easily understood by the patient and their family. Furthermore, the procedure’s invasiveness raises ethical concerns related to patient autonomy and their right to refuse potentially risky treatments. Even if iEEG offers the best chance for seizure control, the patient ultimately has the right to decline.
For example, imagine a patient with medically refractory epilepsy who is presented with the option of iEEG. The medical team must meticulously explain the risks, which could range from minor discomfort and headaches to serious complications. They must also emphasize that less invasive options have been exhausted and that iEEG offers the best chance of identifying the seizure focus and enabling life-altering surgery. This careful dialogue aims to empower the patient to make an informed decision, free from coercion.
Q 9. How do you balance the benefits and risks of different epilepsy treatments when making ethical decisions?
Balancing the benefits and risks of epilepsy treatments is a constant ethical challenge. It’s not just about choosing the most effective drug or procedure; it’s about finding the best fit for each individual, acknowledging their unique values, preferences, and circumstances. A framework for ethical decision-making might involve weighing the potential benefits (e.g., seizure reduction, improved quality of life) against the potential harms (e.g., side effects, cost, invasiveness). This requires careful consideration of the severity of the patient’s epilepsy, their response to previous treatments, and their overall health status. Shared decision-making, a collaborative approach involving the patient, their family, and the healthcare team, is critical. For instance, a patient with mild epilepsy may prioritize minimal side effects over achieving complete seizure freedom, while a patient with severe, debilitating epilepsy might accept more significant risks for potentially greater benefits.
Let’s consider the choice between medication and surgery. Anti-epileptic drugs (AEDs) often have significant side effects, ranging from mild drowsiness to severe liver damage. Surgery, while potentially curative, carries its own risks of infection, bleeding, and neurological deficits. The ethical decision hinges on a thorough assessment of the patient’s individual situation and a shared discussion about their preferences and values. It’s vital to respect patient autonomy and ensure they understand the implications of each treatment option before making a decision.
Q 10. Discuss the ethical considerations surrounding the use of experimental treatments for epilepsy.
The use of experimental treatments for epilepsy, such as novel AEDs or gene therapies, raises unique ethical considerations. The primary concern is the balance between potential benefits and unknown risks. Phase I, II, and III clinical trials are designed to carefully evaluate safety and efficacy, but unpredictable side effects can still occur. Informed consent becomes even more crucial in this context, requiring detailed explanations of both the potential benefits and the potential harms, including the possibility of unknown long-term effects. Patients must understand that they are participating in research and may not experience a benefit. The ethical oversight of clinical trials is also crucial. Independent review boards (IRBs) play a vital role in ensuring the ethical conduct of these trials, protecting the rights and safety of participants.
For instance, a new gene therapy promising to cure a specific type of epilepsy might be offered to patients in a clinical trial. The ethical challenge lies in ensuring that patients understand the uncertainty involved. They need to be fully aware that the therapy might not work, could have unforeseen side effects, and that they’re essentially participating in a scientific experiment. They must also be made aware of alternative treatments available and be given the opportunity to choose between participating in the trial and pursuing other options.
Q 11. How would you handle a situation where a patient refuses necessary epilepsy medication?
A patient’s refusal of necessary epilepsy medication presents a complex ethical dilemma. The core principle is respecting patient autonomy—the right to make decisions about their own body and health, even if those decisions seem medically unwise. However, this must be balanced with the physician’s responsibility to act in the patient’s best interests. The first step involves open and empathetic communication. Understanding the reasons behind the refusal is vital. Are there concerns about side effects, cost, or loss of independence? Addressing these concerns and exploring alternatives, such as different medications or medication management strategies, is essential. If the refusal puts the patient at significant risk of harm (e.g., frequent seizures leading to injury or death), the physician might need to consider involuntary treatment, but this should be pursued only as a last resort and through appropriate legal channels.
A scenario might involve a patient who experiences unpleasant side effects from their AEDs, leading them to discontinue the medication despite experiencing frequent seizures. The physician must carefully listen to the patient’s concerns and explore whether adjusting the dosage, changing medications, or implementing alternative strategies (e.g., lifestyle changes) could address the issues without compromising seizure control. If the patient’s refusal continues to pose a considerable risk to their well-being, legal counsel might be necessary to determine if involuntary treatment is justified.
Q 12. Explain the ethical implications of driving restrictions for patients with epilepsy.
Driving restrictions for patients with epilepsy raise several ethical considerations. The primary concern is balancing public safety with the patient’s autonomy and right to mobility. Driving restrictions are implemented to prevent seizures from occurring while driving, which could endanger the driver and others. However, these restrictions can significantly impact a patient’s independence, employment, and overall quality of life. The ethical challenge is ensuring that driving restrictions are fair, consistent, and based on objective assessments of seizure risk. Regular neurological evaluations, including seizure frequency, type, and response to treatment, are crucial for determining the appropriate level of driving restriction. It’s also important to consider individual circumstances and the availability of alternative transportation.
For example, a patient with well-controlled epilepsy who hasn’t had a seizure in years might face unnecessary restrictions, while a patient with frequent seizures may be correctly advised against driving. A just and ethical approach involves regular assessments, transparency about the rationale behind restrictions, and sensitivity to the patient’s concerns. The patient should be fully informed of the reasons for any driving restrictions and the process for appealing those restrictions if they feel they are unjustly imposed.
Q 13. What are the ethical considerations related to genetic testing for epilepsy?
Genetic testing for epilepsy raises several ethical considerations related to privacy, autonomy, and potential psychological impact. Genetic tests can identify gene variants associated with an increased risk of epilepsy, but they don’t always provide a definitive diagnosis. The results can have significant implications for the patient and their family members, including reproductive decisions and potential insurance discrimination. Informed consent is paramount. Patients must fully understand the potential benefits and limitations of the test, as well as the potential psychological impact of receiving results that indicate a higher risk of epilepsy. Genetic information is highly sensitive and should be protected from unauthorized access or disclosure. Furthermore, genetic testing can raise complex ethical issues for family members who might be indirectly affected by the results.
For example, if a genetic test reveals a family member carries a gene associated with a high risk of a severe form of epilepsy, this individual will need support in dealing with the emotional impact of the news. Their decision on whether or not to have children or undergo further genetic testing must be respected. Genetic counselors and other healthcare professionals can offer guidance in navigating the complex emotional and ethical challenges associated with genetic testing for epilepsy. Careful consideration of the psychological well-being of patients and their families should be at the forefront of decision-making.
Q 14. How do you address concerns about stigma and discrimination related to epilepsy?
Addressing concerns about stigma and discrimination related to epilepsy requires a multi-faceted approach involving education, advocacy, and policy changes. Epilepsy is often misunderstood, leading to prejudice and social exclusion. Educational initiatives can help dispel myths and misconceptions surrounding the condition, promoting greater understanding and empathy. Advocacy groups play a vital role in raising awareness, challenging discriminatory practices, and promoting the rights of individuals with epilepsy. Policies promoting inclusivity in employment, education, and other areas of life are essential to combat discrimination. Open conversations about epilepsy can help reduce stigma and encourage individuals to seek help without shame or fear.
For instance, a public awareness campaign could highlight the successes of individuals living with epilepsy, showcasing their contributions to society and dispelling the misconception that epilepsy is a barrier to leading a full and productive life. In the workplace, initiatives promoting understanding and reasonable accommodations for individuals with epilepsy can make a significant difference in fostering inclusivity. Ultimately, creating a supportive and inclusive environment for people with epilepsy requires a collective effort from healthcare professionals, educators, employers, policymakers, and the wider community.
Q 15. Describe the ethical considerations surrounding the use of deep brain stimulation (DBS) for epilepsy.
Deep brain stimulation (DBS) offers a potential treatment for refractory epilepsy, but its use raises several ethical considerations. The most prominent is the balance between potential benefits and risks. DBS surgery carries inherent risks, including bleeding, infection, and device malfunction. Weighing these risks against the potential for seizure reduction requires a thorough discussion between the neurologist, neurosurgeon, and patient (or their surrogate), ensuring informed consent is truly informed.
Another ethical challenge is resource allocation. DBS is an expensive procedure, and its availability may not be equal across all populations. This raises concerns about fairness and justice in healthcare access. Prioritizing patients for DBS based on severity of illness, prognosis, and access to post-operative care is essential to ensure ethical allocation.
Finally, the long-term effects of DBS are still being investigated. Potential psychological impacts, such as changes in personality or mood, must be carefully considered and discussed with patients. Open communication, ongoing monitoring, and a commitment to patient well-being are crucial aspects of ethical DBS practice.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the ethical implications of long-term care decisions for patients with refractory epilepsy.
Long-term care decisions for patients with refractory epilepsy involve navigating complex ethical dilemmas. Autonomy is paramount – respecting the patient’s right to make decisions about their own care, even if those decisions may seem risky to others. This requires careful assessment of the patient’s capacity to make decisions, and if capacity is limited, involving family members or legal guardians in the decision-making process, while still centering the patient’s best interests.
Beneficence and non-maleficence – acting in the patient’s best interest while minimizing harm – are also critical. This involves weighing the potential benefits and harms of different treatment options, including the risks associated with medication side effects or invasive procedures. A balance must be struck between maximizing quality of life and minimizing suffering.
Justice demands that all patients, regardless of their socioeconomic status or other factors, have access to the level of care they need. This means addressing potential disparities in access to long-term care services and advocating for policies that promote equitable care.
Q 17. How do you ensure equitable access to epilepsy care for all patients?
Ensuring equitable access to epilepsy care requires a multi-pronged approach. Reducing financial barriers is crucial. This can be done through government subsidies, affordable insurance coverage, and charitable organizations offering financial assistance.
Addressing geographical barriers is also important. Many individuals live in areas with limited access to neurologists or epilepsy centers. Telemedicine, mobile clinics, and initiatives to train healthcare providers in underserved areas can help overcome this.
Cultural competency is key. Providers need to understand and respect the cultural beliefs and practices of their patients, ensuring that care is tailored to their individual needs. Language barriers must also be addressed through interpretation services.
Finally, advocacy is essential. Healthcare professionals should advocate for policies and programs that support equitable access to epilepsy care for all.
Q 18. Discuss the ethical responsibilities of healthcare professionals in managing epilepsy during pregnancy.
Managing epilepsy during pregnancy presents a unique set of ethical challenges. The primary concern is balancing the health of the mother and the fetus. Anti-epileptic drugs (AEDs) are often necessary to control seizures, but some AEDs carry risks of birth defects.
Shared decision-making is paramount. The obstetrician and neurologist should work collaboratively with the pregnant woman to carefully weigh the risks and benefits of different AEDs and other treatment options. This includes exploring the option of seizure monitoring and adjusting medication dosages as needed, potentially even considering a switch to a lower-risk drug in consultation with a teratology specialist.
Informed consent is crucial, ensuring the woman fully understands the risks and benefits of all available options and is empowered to make informed choices about her treatment. Transparency is vital, and the woman’s preferences and values should be respected.
Q 19. Describe the ethical considerations surrounding the use of ketogenic diets for epilepsy.
The ketogenic diet is a specialized dietary therapy for epilepsy, but it raises several ethical considerations. The diet is highly restrictive and can be difficult to maintain, leading to potential nutritional deficiencies and social isolation. Parental autonomy versus the child’s best interests is often a central focus, particularly when treating children. Parents must be fully informed of the diet’s potential benefits and risks before agreeing to it for their child.
Monitoring and follow-up are crucial. Regular blood tests and nutritional assessments are necessary to detect and address any deficiencies, ensuring the child’s overall health is protected. This continuous monitoring requires commitment from both families and healthcare professionals.
Accessibility and affordability also pose challenges. Specialized dietary assistance and regular follow-up visits can be expensive and may not be equally accessible to all families. This highlights an important element of health equity and the need for supportive resources.
Q 20. Explain the ethical implications of reporting suspected child abuse in a patient with epilepsy.
Reporting suspected child abuse in a patient with epilepsy involves a delicate balance between protecting the child and respecting patient confidentiality. Healthcare professionals have a legal and ethical obligation to report suspected abuse, but this must be done responsibly and appropriately.
The key is to gather sufficient evidence to support the suspicion before making a report. This may include physical examination findings, patient history, and witness statements. The report should be made to the appropriate child protective services agency, following the legal guidelines of the jurisdiction.
It’s crucial to document thoroughly all observations and actions taken. This ensures a clear record of the events, protecting both the healthcare professional and the child. Transparency and open communication with the patient (where appropriate and safe) can help build trust and foster collaborative care.
In instances where the suspicion is not clear-cut, seeking advice from colleagues or legal counsel is advisable.
Q 21. How would you address a situation where there is a conflict of interest in managing a patient with epilepsy?
Conflicts of interest in managing epilepsy can arise in various forms, such as financial incentives for prescribing specific medications or engaging in research with potential biases. The most important step is transparency and disclosure. Healthcare professionals have an ethical obligation to disclose any potential conflicts of interest to their patients. This allows patients to make informed decisions about their care and ensures trust in the physician-patient relationship.
If a conflict of interest cannot be avoided or resolved through disclosure, the healthcare professional should recuse themselves from the patient’s care. This ensures the patient receives unbiased and objective care. Referral to another healthcare provider who does not have a conflict of interest is essential in such cases.
Institutional policies and ethical guidelines play a vital role in preventing and managing conflicts of interest. Adherence to these guidelines is crucial in maintaining ethical conduct and upholding the integrity of the medical profession. Maintaining objectivity and patient well-being must always remain the primary focus.
Q 22. What are the ethical considerations related to the use of artificial intelligence (AI) in epilepsy diagnosis and treatment?
The integration of Artificial Intelligence (AI) in epilepsy diagnosis and treatment presents exciting possibilities but also significant ethical challenges. One key concern is algorithmic bias. AI algorithms are trained on data, and if that data reflects existing biases (e.g., underrepresentation of certain demographics), the AI may misdiagnose or mistreat patients from those underrepresented groups. This could lead to disparities in healthcare access and outcomes.
Another concern is data privacy and security. AI systems require vast amounts of patient data for training and operation. Ensuring the confidentiality, integrity, and availability of this sensitive information is crucial. Breaches could have devastating consequences for patients.
Transparency and explainability are also vital. Many AI algorithms, especially deep learning models, are ‘black boxes,’ meaning their decision-making processes are opaque. This lack of transparency makes it difficult to understand why an AI made a specific diagnosis or treatment recommendation, hindering trust and accountability. Clinicians need to understand how the AI arrived at its conclusions to make informed decisions and maintain control over patient care.
Finally, there’s the issue of responsibility and liability. If an AI system makes an incorrect diagnosis or recommendation, who is held accountable – the developer, the hospital, or the clinician using the AI? Establishing clear lines of responsibility is crucial to ensure patient safety and prevent legal disputes.
Q 23. Describe the role of ethics committees in addressing ethical dilemmas related to epilepsy management.
Ethics committees play a vital role in navigating the complex ethical dilemmas encountered in epilepsy management. They provide a forum for discussion and deliberation, ensuring that patient autonomy, beneficence, non-maleficence, and justice are upheld. In the context of epilepsy, ethics committees might be involved in:
- Reviewing research protocols involving human subjects with epilepsy, ensuring informed consent and minimizing risks.
- Addressing conflicts of interest, such as financial incentives that could compromise patient care.
- Evaluating the ethical implications of new technologies, such as AI or deep brain stimulation, before their implementation.
- Resolving disputes between patients, families, and healthcare providers regarding treatment decisions.
- Developing guidelines and policies for ethical epilepsy management within a healthcare system.
Essentially, ethics committees act as a safeguard, ensuring that decisions are made in the best interests of the patient while upholding ethical principles.
Q 24. Explain the ethical considerations surrounding end-of-life care for patients with severe epilepsy.
End-of-life care for patients with severe, refractory epilepsy presents particularly challenging ethical considerations. The focus shifts from cure to comfort and quality of life. Decisions surrounding life-sustaining treatments, such as artificial ventilation or feeding tubes, become crucial. These decisions must be made in accordance with the patient’s wishes, as expressed through advance directives or surrogates if the patient lacks capacity.
Ethical dilemmas can arise when there is conflict between the patient’s wishes (or those of their family) and the medical team’s assessment of the patient’s best interests. For example, a family may want to continue aggressive life-sustaining treatments even when the patient’s prognosis is extremely poor and their suffering is significant. Open communication, careful consideration of the patient’s values, and involvement of palliative care specialists are essential to navigate these difficult situations.
The concept of ‘futility‘ – the point at which further medical interventions are deemed unlikely to provide benefit and may even cause harm – is often a significant consideration. Determining futility, however, requires careful clinical judgment and sensitive communication with patients and families.
Q 25. How do you ensure cultural sensitivity in epilepsy care?
Cultural sensitivity in epilepsy care is paramount because epilepsy is experienced and understood differently across cultures. Some cultures may attribute epilepsy to supernatural causes, leading to stigma and discrimination. Others may have specific beliefs and practices regarding treatment. Ignoring these cultural differences can undermine trust, hinder treatment adherence, and worsen patient outcomes.
Ensuring cultural sensitivity involves:
- Understanding cultural beliefs and practices related to epilepsy within the patient’s community.
- Using culturally appropriate communication styles and avoiding jargon.
- Involving family members in decision-making, as appropriate, respecting their cultural roles.
- Providing culturally competent education and resources.
- Adapting treatment plans to accommodate cultural preferences and beliefs, where possible, while ensuring safety and efficacy.
For example, a healthcare provider might need to work with a family who believes in traditional healing methods to integrate these practices alongside Western medicine, creating a holistic approach that respects the patient’s cultural background.
Q 26. Discuss the ethical implications of using wearable technology to monitor epilepsy.
Wearable technology offers promising opportunities for epilepsy monitoring, allowing for continuous data collection and early detection of seizures. However, it also raises several ethical considerations. One major concern is data privacy. Wearables collect intimate data about an individual’s health and activity, raising the possibility of unauthorized access or misuse. The data’s storage, transmission, and security protocols need careful attention.
Another concern is autonomy and control. Patients need to be fully informed about what data is collected, how it is used, and who has access to it. They should have the right to opt out of data collection or to control how their data is shared. Clear and accessible consent processes are crucial.
Data security is also important. Robust measures must be implemented to prevent data breaches and hacking, protecting patients’ sensitive information. Finally, there is the potential for over-reliance on the data generated by wearable technology. While these devices are valuable tools, they should complement, not replace, clinical judgment and professional expertise.
Q 27. What are the ethical considerations related to data privacy in epilepsy management?
Data privacy in epilepsy management is critical given the sensitive nature of the information involved. Patient records, including seizure logs, EEG data, and medication details, are protected by regulations like HIPAA (in the US) and GDPR (in Europe). However, these regulations alone are not sufficient to address all the ethical challenges.
Key considerations include:
- Data anonymization and de-identification: Techniques should be used to remove or obscure identifying information from data sets used for research or analysis.
- Data security and encryption: Robust security measures are essential to prevent unauthorized access and data breaches.
- Data minimization: Only necessary data should be collected and retained.
- Transparency and consent: Patients must be fully informed about how their data will be used and must provide explicit consent for its collection, storage, and use.
- Data governance and accountability: Clear policies and procedures should be in place to govern the handling of patient data, with clear lines of responsibility for data security and privacy.
Breaches of data privacy can have devastating consequences for patients, leading to discrimination, identity theft, and emotional distress. Robust data protection measures are therefore not just a legal requirement but an ethical imperative.
Q 28. Explain the ethical responsibilities of researchers conducting clinical trials for new epilepsy treatments.
Researchers conducting clinical trials for new epilepsy treatments have significant ethical responsibilities. These responsibilities stem from the need to protect the well-being and rights of participants while ensuring the integrity and validity of the research.
Key ethical considerations include:
- Informed consent: Participants must be fully informed about the purpose, procedures, risks, and benefits of the trial before they agree to participate. This includes providing information in a language they understand and addressing any questions or concerns they may have.
- Minimizing risks and maximizing benefits: Researchers have a duty to design and conduct the trial in a way that minimizes potential harms to participants while maximizing the potential benefits of the new treatment. This includes careful selection of participants, rigorous monitoring for adverse events, and appropriate safety measures.
- Data integrity and transparency: Researchers must collect, analyze, and report data accurately and honestly. Transparency in the research process, including the publication of results, is crucial to ensure public trust and accountability.
- Equity and fairness: Trial design should ensure equitable access to participation and that all participants are treated fairly, regardless of their background or characteristics.
- Confidentiality and privacy: Researchers must protect the privacy and confidentiality of participants’ data throughout the trial.
Failure to uphold these ethical responsibilities can lead to serious consequences, including harm to participants, flawed research results, and damage to public trust in medical research.
Key Topics to Learn for Knowledge of Ethical Considerations in Epilepsy Management Interview
- Informed Consent and Patient Autonomy: Understanding the complexities of obtaining informed consent from patients with epilepsy, particularly those with cognitive impairments or fluctuating mental states. Explore practical applications such as navigating decision-making capacity assessments and involving surrogate decision-makers.
- Balancing Risks and Benefits of Treatment: Analyzing the ethical dilemmas surrounding treatment choices, weighing the potential benefits of medication, surgery, or other interventions against their potential risks and side effects. Consider case studies involving difficult treatment decisions.
- Confidentiality and Disclosure: Mastering the ethical considerations surrounding patient confidentiality, including the legal and professional obligations related to disclosure of sensitive information, especially concerning driving safety or employment limitations.
- Equity and Access to Care: Addressing potential disparities in access to quality epilepsy care, including considerations of socioeconomic status, geographic location, and healthcare insurance coverage. Discuss strategies for promoting equitable access to treatment and resources.
- End-of-Life Care and Advance Care Planning: Understanding the ethical issues surrounding end-of-life care for individuals with epilepsy, including the importance of advance care planning, respecting patient wishes, and providing compassionate palliative care.
- Research Ethics in Epilepsy: Familiarize yourself with the ethical principles governing research involving individuals with epilepsy, such as informed consent, data privacy, and the responsible conduct of clinical trials.
- Management of Conflicts of Interest: Explore potential conflicts of interest that may arise in the management of epilepsy and strategies for mitigating these conflicts to ensure patient well-being and ethical practice.
Next Steps
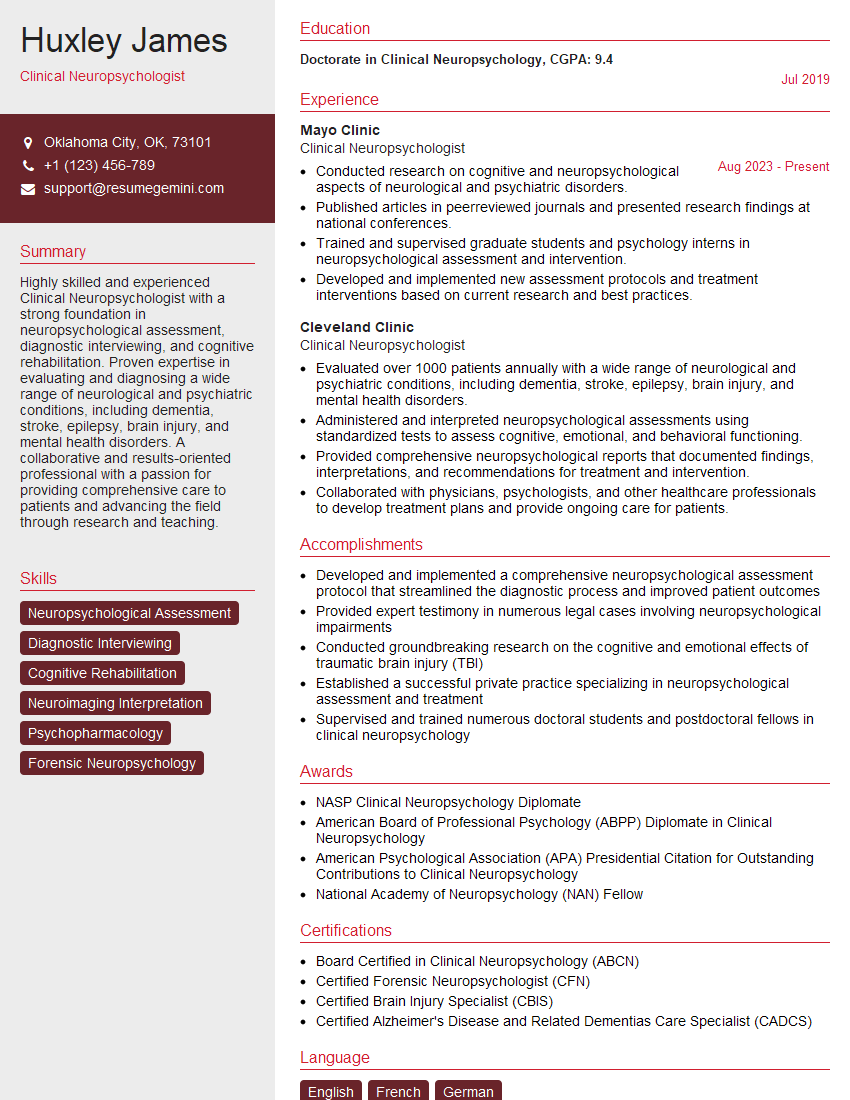
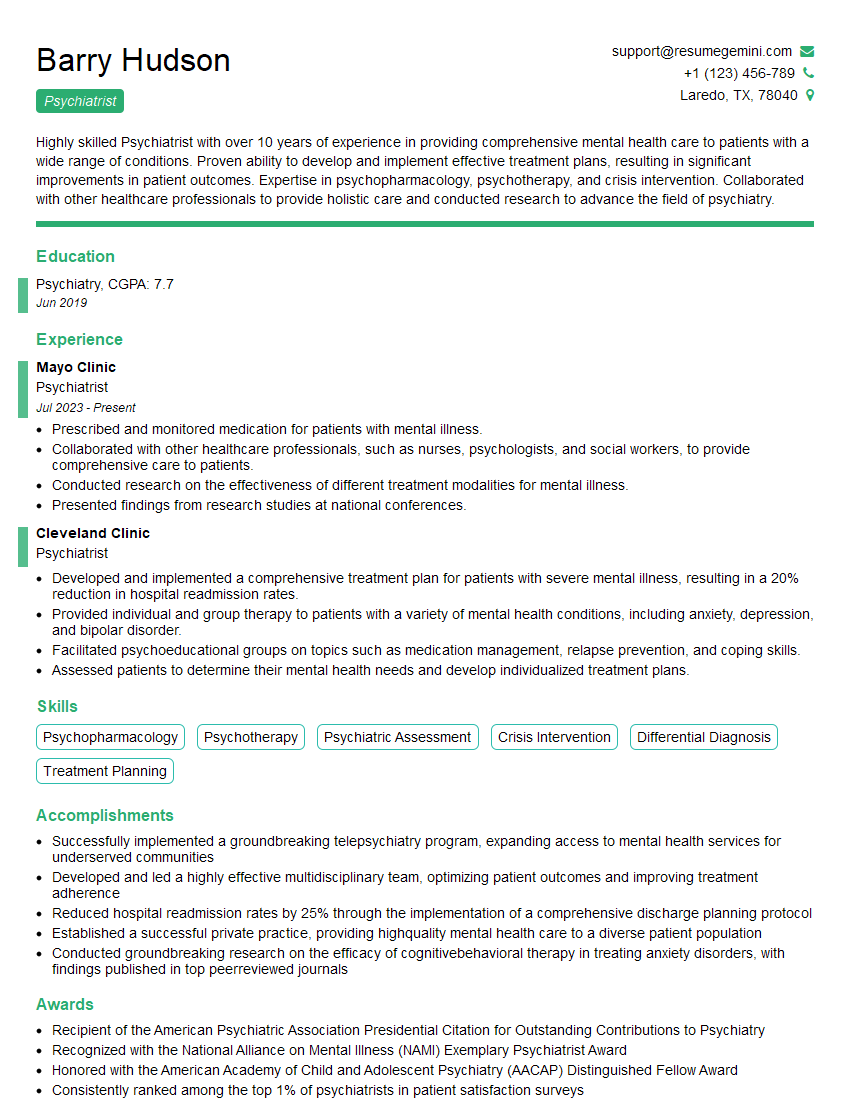
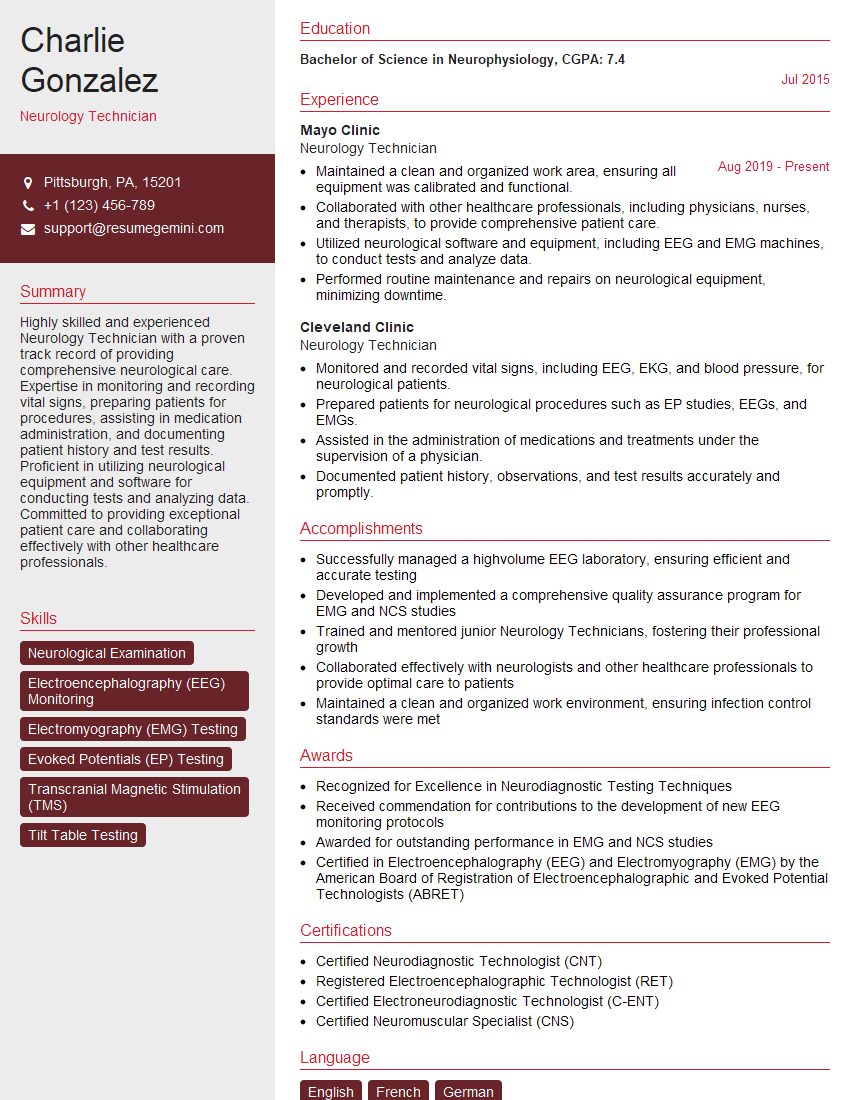
Mastering ethical considerations in epilepsy management is crucial for demonstrating your commitment to patient-centered care and advancing your career in this specialized field. A strong understanding of these principles significantly enhances your credibility and marketability to potential employers. To maximize your job prospects, creating an ATS-friendly resume is vital. ResumeGemini is a trusted resource that can help you build a professional and effective resume tailored to highlight your expertise. Examples of resumes specifically tailored to showcase knowledge of ethical considerations in epilepsy management are available through ResumeGemini to guide your resume creation process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.