Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Laser and Radiofrequency Vein Ablation interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Laser and Radiofrequency Vein Ablation Interview
Q 1. Describe the mechanism of action for laser ablation.
Laser ablation for vein treatment uses a laser fiber to deliver energy directly to the vein wall. This energy, typically in the form of near-infrared light, heats the vein wall, causing collagen and elastin fibers to contract and the vessel to collapse. The heat also triggers a thermal injury, causing the vein lining to seal and ultimately close the vein off from the circulation. Think of it like shrinking and sealing a leaky pipe from the inside. The blood flow then redirects to healthier veins.
Different laser wavelengths are used with varying levels of energy penetration. For example, endovenous laser ablation (EVLA) often utilizes 1470nm wavelength which has good absorption properties by water within the vein wall resulting in efficient heating and sealing of the vein.
Q 2. Explain the mechanism of action for radiofrequency ablation.
Radiofrequency ablation (RFA) operates on a similar principle to laser ablation, but uses radiofrequency energy instead of laser light to heat and close the vein. A radiofrequency catheter is inserted into the vein, and energy is delivered to the vein wall, causing tissue heating and coagulation. This leads to collagen shrinkage and eventual closure of the vein, much like the effect of a soldering iron creating a tight seal.
The mechanism involves the conversion of radiofrequency energy into thermal energy which raises the vein wall temperature to a therapeutic range. This triggers a controlled injury process resulting in the closure of the vein while minimizing damage to surrounding tissue. The specific temperature and energy delivery parameters are carefully adjusted based on the vein diameter and location.
Q 3. What are the advantages and disadvantages of laser ablation compared to radiofrequency ablation?
Both laser and radiofrequency ablation are effective for treating varicose veins, but they have some differences.
- Advantages of Laser Ablation: Often considered faster, potentially requiring shorter procedure times. Some studies suggest potentially lower rates of complications such as hematomas (blood clots under the skin). The smaller laser fibers can offer greater access to smaller veins.
- Advantages of Radiofrequency Ablation: May offer slightly more even heating of the vein wall, potentially leading to improved results in some patients, Generally, the equipment can be less expensive than some laser systems.
- Disadvantages of Laser Ablation: The initial equipment cost can be higher compared to RFA. The laser fiber is more delicate and can be prone to damage.
- Disadvantages of Radiofrequency Ablation: The procedure might be slightly longer and less comfortable for some patients.
Ultimately, the best technique depends on factors specific to each patient, including vein size, location, and patient preference. A physician specializing in phlebology would assess these factors before choosing between the two procedures.
Q 4. What are the indications for laser and radiofrequency ablation?
Both laser and radiofrequency ablation are primarily indicated for the treatment of superficial venous insufficiency. This includes:
- Great saphenous vein (GSV) reflux: Where blood flows backward in the GSV vein.
- Small saphenous vein (SSV) reflux: Similar to GSV reflux, but in the SSV vein.
- Reticular veins: Larger, visible veins that are closer to the surface of the skin.
- Varicose veins: The visibly enlarged, twisted veins.
The specific indications are determined on a case-by-case basis during a thorough clinical evaluation that often includes a venous ultrasound to assess the extent of venous reflux and identify the appropriate vein for treatment.
Q 5. What are the contraindications for laser and radiofrequency ablation?
Contraindications for both laser and radiofrequency ablation are similar and include:
- Severe peripheral artery disease (PAD): Compromised blood flow to the legs could negatively impact healing.
- Active infection at the treatment site: This would increase the risk of complications.
- Severe obesity: Obesity can affect the ultrasound visibility of veins, making the procedure more difficult.
- Pregnancy: The safety of these procedures during pregnancy hasn’t been fully established.
- Uncontrolled bleeding disorders: Increased risk of hematoma.
- Severe heart or lung disease: This increases risk associated with general anesthesia.
A thorough medical history and physical examination are crucial in determining suitability for either procedure.
Q 6. How do you select patients for laser or radiofrequency ablation?
Patient selection for laser or radiofrequency ablation begins with a comprehensive assessment. This includes a detailed medical history, physical examination, and a venous ultrasound. The ultrasound helps visualize the veins, identify areas of reflux (backward blood flow), and measure the size and location of the affected veins. Factors considered include the patient’s age, overall health, the severity of symptoms, and the extent of the venous disease. Physician preference, available technology and patient preference may also play a role in the final decision. The goal is to choose the safest and most effective treatment option for each individual patient.
Q 7. Describe the procedure for laser ablation, step-by-step.
The laser ablation procedure, typically EVLA, is performed under ultrasound guidance and typically involves these steps:
- Pre-procedure preparation: The patient is given local anesthesia and an intravenous line is placed.
- Venous access: A small incision is made, and a thin catheter is inserted into the vein (usually under ultrasound guidance).
- Catheter advancement: The catheter is advanced to the desired location within the vein, usually guided by ultrasound.
- Laser fiber placement: A laser fiber is passed through the catheter.
- Laser energy delivery: The laser energy is delivered to the vein wall, causing the vein to close.
- Catheter removal: Once the entire vein is treated, the catheter is removed and the incision is closed.
- Post-procedure care: The patient usually wears compression stockings and is advised to follow instructions for post-operative care.
The specific steps might vary slightly depending on the type of laser system used and the physician’s technique. It’s important to note that the procedure is minimally invasive but still requires skilled professionals and a proper sterile environment.
Q 8. Describe the procedure for radiofrequency ablation, step-by-step.
Radiofrequency ablation (RFA) is a minimally invasive procedure used to close varicose veins. It involves using heat generated by radiofrequency energy to seal off the affected vein. Think of it like carefully cauterizing a small section of a leaky pipe to stop the leak. Here’s a step-by-step breakdown:
- Ultrasound Guidance: The procedure begins with an ultrasound scan to visualize the vein and its tributaries. This allows the physician to precisely target the problematic vein.
- Access Point: A small puncture is made in the skin, usually near the groin or ankle, depending on the location of the vein.
- Catheter Insertion: A thin, flexible catheter (a small tube) is carefully inserted into the vein under ultrasound guidance.
- Catheter Advancement: The catheter is advanced to the targeted section of the vein.
- Radiofrequency Energy Delivery: Once positioned correctly, radiofrequency energy is delivered through the catheter. This generates heat that causes the vein wall to collapse and seal shut.
- Withdrawal and Closure: After the vein is treated, the catheter is carefully withdrawn, and the puncture site is closed with a small bandage.
The patient usually experiences minimal discomfort thanks to local anesthesia or sedation used during the procedure.
Q 9. What are the potential complications of laser ablation?
Laser ablation, while highly effective, carries some potential risks, though they are relatively uncommon. These can include:
- Nerve Damage: In rare cases, damage to nearby nerves can cause pain, numbness, or tingling. This is usually temporary but can be persistent in some cases.
- Hematoma: A collection of blood under the skin at the puncture site. Usually resolves on its own.
- Thrombophlebitis: Inflammation of the vein, which can cause pain and swelling. Proper compression and medication help to manage this.
- Pigmentation changes: Some patients might experience temporary or permanent discoloration of the skin around the treatment area.
- Deep vein thrombosis (DVT): Although rare, there is a slight risk of a blood clot forming in a deeper vein. This is a serious complication, but proactive measures like compression stockings can help to mitigate this risk.
- Allergic reaction: Although infrequent, there can be a reaction to local anesthetic or other materials used.
It’s vital to emphasize that the benefits of laser ablation usually outweigh these risks, especially when compared to the alternative of leaving the problem untreated.
Q 10. What are the potential complications of radiofrequency ablation?
Similar to laser ablation, radiofrequency ablation also has potential complications, although they are usually mild and temporary. These include:
- Pain and discomfort: Some patients experience pain or discomfort at the puncture site or along the treated vein. Pain medication can effectively manage this.
- Bruising: Bruising is common and typically resolves within a few weeks.
- Swelling: Some swelling around the treated area is expected and usually subsides within a short time.
- Infection: Infection at the puncture site is rare but possible. Antibiotics are used if necessary.
- Nerve damage: Although rare, nerve damage can occur near the treatment site, resulting in numbness or tingling. This is usually temporary.
- Deep vein thrombosis (DVT): This is a serious but rare complication.
The physician will carefully monitor the patient for any signs of these complications and take appropriate steps to address them immediately.
Q 11. How do you manage complications during and after laser ablation?
Managing complications during and after laser ablation requires a proactive and multi-faceted approach. The key is early detection and prompt intervention.
- During the procedure: Continuous ultrasound monitoring allows immediate detection of issues like bleeding or perforation. Immediate pressure can often resolve bleeding. If a nerve is inadvertently affected, careful repositioning of the catheter might be necessary.
- Post-procedure: Regular follow-up appointments are crucial. Pain medication is prescribed as needed. Compression stockings help to reduce swelling and the risk of DVT. Antibiotics are given if there is evidence of infection. Close observation for signs of nerve damage is vital, and further investigations might be needed in certain cases.
Patient education is key – patients should be aware of what to expect and report any concerning symptoms immediately.
Q 12. How do you manage complications during and after radiofrequency ablation?
Managing complications following RFA is similar to laser ablation management. Prompt identification and treatment are paramount.
- During the procedure: Continuous ultrasound monitoring is crucial to identify any immediate complications such as bleeding or catheter malposition.
- Post-procedure: Post-operative care focuses on pain management (analgesics), minimizing swelling (compression stockings), and preventing infection (antibiotics if needed). Regular follow-up appointments allow for early detection of any delayed complications such as DVT, hematoma, or nerve damage. Patients are educated to report any unusual pain, swelling, or changes in skin color. Immediate attention to these symptoms ensures prompt intervention and reduces the risk of long-term effects.
Open communication between the patient and the physician is critical for successful post-operative management.
Q 13. What are the post-operative instructions for patients after laser ablation?
Post-operative instructions after laser ablation aim to ensure patient comfort and recovery and minimize complications. These generally include:
- Compression Stockings: Wearing compression stockings for a specified period is essential to reduce swelling and support blood flow.
- Activity Level: Gradual resumption of normal activities is recommended. Avoid strenuous activity initially.
- Pain Management: Over-the-counter pain relievers or prescription medications as needed.
- Wound Care: Keeping the puncture site clean and dry.
- Follow-up Appointments: Attending scheduled follow-up appointments for monitoring progress and addressing any issues.
- Hydration and Diet: Maintain a healthy diet and hydration to support healing.
Detailed written instructions are typically given to each patient. It’s crucial for patients to understand the importance of adhering to these instructions.
Q 14. What are the post-operative instructions for patients after radiofrequency ablation?
Post-operative care after RFA mirrors that of laser ablation, emphasizing patient comfort and minimizing complications. The instructions typically cover:
- Compression: Wearing compression stockings helps manage swelling and improve circulation. The duration will be specified by your physician.
- Activity: Gradual increase in activity levels is advised, avoiding strenuous exercise in the initial days.
- Pain Relief: Over-the-counter or prescribed pain relievers can help manage any discomfort.
- Wound Care: The puncture site needs to be kept clean and dry to prevent infection.
- Follow-up: Attending all scheduled follow-up appointments is vital for monitoring your progress and addressing any concerns.
- Hydration and Diet: Maintain adequate hydration and a balanced diet to support healing.
Open communication with your physician is crucial. Report any unusual symptoms immediately to ensure prompt management.
Q 15. How do you monitor patients after laser or radiofrequency ablation?
Post-procedure monitoring after laser or radiofrequency ablation is crucial for ensuring patient safety and optimal outcomes. It involves a multifaceted approach focusing on early detection and management of potential complications.
- Immediate Post-Procedure Monitoring: This includes vital signs monitoring (heart rate, blood pressure, oxygen saturation) to detect any signs of bleeding, hypotension, or other adverse events. Patients are observed for pain, swelling, or signs of nerve injury.
- Ambulatory Monitoring: Patients are typically discharged the same day or after a short observation period. However, they’re given detailed instructions on wound care and activity restrictions. They are advised to report any concerning symptoms like excessive pain, swelling, or changes in skin color immediately.
- Follow-up Appointments: Scheduled follow-up appointments (usually within a few weeks and then at intervals thereafter) are essential for assessing healing progress, evaluating the effectiveness of the treatment, and addressing any lingering issues. Ultrasound scans may be performed to confirm vein closure.
- Patient Education: Thorough education on potential complications, such as hematoma formation, nerve injury, or deep vein thrombosis (DVT), and how to recognize them is paramount. Patients are taught self-care measures to minimize the risk of complications.
For instance, a patient experiencing significant pain or swelling at the treatment site would require immediate medical attention, potentially including pain management and ultrasound evaluation to rule out a hematoma.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common imaging techniques used in the diagnosis and treatment of venous disease?
Imaging plays a pivotal role in both diagnosing and guiding the treatment of venous disease. Several techniques are commonly employed:
- Duplex Ultrasound: This is the cornerstone of venous disease diagnosis. It combines B-mode imaging (grayscale images showing vein structure) with Doppler imaging (assessing blood flow). This allows visualization of vein structure, identification of reflux (backward blood flow), and assessment of blood flow velocity. It’s invaluable for identifying incompetent valves, varicose veins, and deep vein thrombosis (DVT).
- Venography: This is an invasive technique where contrast dye is injected into the veins, allowing visualization of the venous system via X-ray. While less frequently used now due to the advances in ultrasound, venography remains a valuable tool in complex cases or when ultrasound results are inconclusive.
- CT Venography/MR Venography: These advanced imaging techniques provide detailed three-dimensional images of the venous system. They’re often used to assess the extent of venous disease and plan complex surgical interventions. However, they are more expensive and carry potential risks associated with contrast agents.
For example, a patient with suspected DVT would undergo a duplex ultrasound to assess blood flow in the deep veins. If the results are unclear, a CT venography or MR venography might be considered.
Q 17. Explain your understanding of the different types of venous insufficiency.
Venous insufficiency refers to the impaired ability of the veins to effectively return blood from the lower extremities to the heart. This can manifest in several ways:
- Chronic Venous Insufficiency (CVI): This is a long-term condition characterized by venous hypertension, leading to damage to the valves and walls of the veins. Symptoms include edema (swelling), pain, skin changes (hyperpigmentation, lipodermatosclerosis), and venous ulcers.
- Varicose Veins: These are abnormally dilated and tortuous superficial veins, often visible just under the skin’s surface. They are a common manifestation of CVI.
- Telangiectasias (Spider Veins): These are small, dilated capillaries or venules near the skin’s surface, often appearing as fine red or purple lines or webs.
- Deep Vein Thrombosis (DVT): This is a serious condition involving the formation of blood clots in the deep veins of the legs. It can cause pain, swelling, and potentially life-threatening complications like pulmonary embolism.
The distinction is crucial because treatment strategies vary significantly. For example, varicose veins may be treated with minimally invasive procedures like laser or radiofrequency ablation, while DVT necessitates anticoagulation therapy.
Q 18. How do you interpret ultrasound imaging for venous disease?
Interpreting ultrasound imaging for venous disease requires a thorough understanding of both anatomy and hemodynamics. The sonographer assesses various parameters:
- Vein Compression: The compressibility of veins is assessed by applying gentle pressure with the ultrasound probe. Compressible veins suggest patency (openness), while incompressible veins may indicate thrombosis (blood clot formation).
- Blood Flow Direction: Doppler ultrasound assesses the direction of blood flow. Retrograde (reversed) flow during maneuvers like the Valsalva maneuver signifies valvular incompetence.
- Flow Velocity: Measurement of blood flow velocity provides insights into the severity of venous obstruction.
- Vein Diameter and Wall Thickness: These measurements can help differentiate between normal and abnormal veins. Dilated veins may suggest venous hypertension.
- Identification of Collateral Veins: The presence of collateral veins indicates that the body is trying to compensate for venous obstruction or insufficiency.
For example, a patient with suspected superficial venous reflux might demonstrate retrograde flow in the great saphenous vein during the Valsalva maneuver. In contrast, a patient with DVT would show incompressible deep veins and potentially absent or sluggish blood flow.
Q 19. What are the different types of lasers used in laser ablation?
Several types of lasers are used in endovenous laser ablation (EVLA), each with its specific characteristics and applications:
- Nd:YAG (Neodymium-doped Yttrium Aluminum Garnet): This laser emits light in the near-infrared spectrum (1064 nm). It’s frequently used due to its good tissue penetration and relatively low risk of skin burns.
- 1470 nm Diode Laser: This laser offers improved tissue penetration and absorption characteristics compared to Nd:YAG, potentially leading to more effective vein closure and less thermal damage to surrounding tissue.
The choice of laser depends on factors such as vein size, location, and the physician’s preference. The laser energy heats the vein wall, causing it to collapse and seal, effectively eliminating reflux.
Q 20. What are the different types of radiofrequency catheters used in ablation?
Various radiofrequency (RF) catheters are used in radiofrequency ablation (RFA), differing primarily in their design and energy delivery mechanisms:
- Straight Tip Catheters: These are simpler in design and are suitable for treating relatively straight segments of veins.
- Curved Tip Catheters: Designed to navigate more tortuous venous pathways, enhancing access to challenging anatomical locations.
- Multipolar Catheters: These possess multiple electrodes, allowing for more uniform heating and coagulation of the vein wall. They’re often preferred for larger veins.
- Circular Catheters: The circular shape aids in uniform heating of the vein.
The catheter is introduced into the vein under ultrasound guidance. The RF energy generated by the catheter heats the vein wall, causing collagen denaturation, vein shrinkage, and ultimately occlusion.
Q 21. How do you ensure patient safety during these procedures?
Patient safety is the paramount concern during laser and radiofrequency ablation procedures. Several measures are implemented:
- Pre-Procedure Assessment: A thorough medical history, physical examination, and appropriate laboratory tests are conducted to identify and mitigate potential risks.
- Informed Consent: Patients must receive comprehensive information about the procedure, including potential benefits, risks, and alternatives, before providing informed consent.
- Ultrasound Guidance: Real-time ultrasound guidance is crucial for accurate catheter placement, minimizing the risk of nerve or vessel injury.
- Hemodynamic Monitoring: Close monitoring of vital signs, including heart rate and blood pressure, during the procedure helps to identify and address any adverse events.
- Temperature Monitoring: Monitoring the temperature of the vein wall during ablation helps prevent thermal injury to surrounding tissues.
- Post-Procedure Monitoring: As previously discussed, meticulous post-procedure monitoring is essential for early detection and management of complications.
- Appropriate Anesthesia: Using appropriate anesthesia, typically tumescent anesthesia (local anesthetic injected into surrounding tissue) or conscious sedation, manages pain and allows for patient comfort.
For instance, if a patient’s heart rate or blood pressure deviates significantly from baseline during the procedure, the intervention may be temporarily suspended until it’s stabilized. Proper ultrasound guidance minimizes the risk of collateral nerve damage.
Q 22. What are the latest advancements in laser and radiofrequency ablation technology?
Advancements in laser and radiofrequency ablation technology are constantly improving patient outcomes and minimizing invasiveness. Recent innovations include:
- Improved catheter designs: Newer catheters offer better maneuverability, improved energy delivery, and reduced trauma to the vessel wall. For example, some catheters incorporate multiple emitters for more uniform heating.
- Energy delivery systems: We’re seeing advancements in the type of energy delivered. For instance, some radiofrequency systems now use non-thermal energy modalities along with the thermal energy, allowing for improved efficacy and a potentially reduced risk of complications.
- Imaging guidance: Real-time ultrasound guidance and even intravascular ultrasound (IVUS) are becoming more prevalent, allowing for precise targeting of the diseased vein and verification of treatment efficacy.
- Closed-system technologies: This reduces the risk of infection and enhances safety compared to some of the older techniques. These systems offer a more streamlined and efficient procedure workflow.
- Data analysis and AI: Sophisticated software is being integrated into the systems. This allows for better treatment planning based on patient-specific data and provides potential for improved outcomes via AI-powered analysis of the procedure.
These advancements translate to shorter procedure times, reduced pain, quicker recovery, and improved cosmetic results for patients.
Q 23. Discuss the role of tumescent anesthesia in these procedures.
Tumescent anesthesia plays a crucial role in laser and radiofrequency ablation procedures. It’s a technique where a large volume of dilute local anesthetic solution is injected into the subcutaneous tissue surrounding the target vein. Think of it as creating a ‘waterbed’ around the vein.
The benefits are substantial:
- Improved comfort: The tumescence provides excellent pain control during the procedure, making it much more tolerable for the patient.
- Reduced bleeding: The solution helps compress the vein and reduces bleeding, improving visualization and making the procedure safer.
- Enhanced thermal distribution: The tumescent fluid acts as a heat sink, improving the distribution of energy from the catheter and enhancing the effectiveness of the ablation.
- Improved tissue plane dissection: The fluid makes it easier to identify and access the target veins, minimizing the risk of injury to surrounding structures.
Proper tumescent technique is essential for optimal results and patient safety. We carefully calculate the volume and concentration of the solution, ensuring proper injection techniques and monitoring for any adverse reactions.
Q 24. Describe your experience with different types of energy delivery systems.
My experience encompasses various energy delivery systems for both laser and radiofrequency ablation. This includes different wavelengths of laser energy (e.g., Nd:YAG, diode lasers) and various radiofrequency generators with varying frequencies and power settings.
I’ve found that each system has its strengths and weaknesses depending on the patient’s specific anatomy, the size and location of the vein, and the presence of any comorbidities. For example, I might prefer a diode laser for smaller superficial veins due to its precise energy delivery, while a radiofrequency system might be better suited for larger, deeper veins. The choice is guided by a comprehensive assessment of the patient and the individual characteristics of the affected veins.
My experience also includes using various catheter types with these systems, and understanding the nuances of each system is key to successful outcomes. I’ve noticed trends in the adoption of newer technologies that combine different energy modalities or incorporate advanced imaging capabilities for improved precision. This is an ever-evolving field.
Q 25. How do you manage patients with co-morbidities undergoing these procedures?
Managing patients with comorbidities requires a careful, individualized approach. Conditions like diabetes, peripheral artery disease (PAD), and bleeding disorders can significantly impact the risks and outcomes of these procedures.
Before the procedure, a thorough assessment is crucial. This includes a detailed review of their medical history, medication list, and relevant lab results. We carefully evaluate the potential risks and benefits, often consulting with other specialists if necessary. For instance, a patient with diabetes may require stricter glucose control pre- and post-operatively. Those with PAD may require additional imaging to assess vascular status and possibly modify the procedural technique. Patients on anticoagulants often need a modified protocol to minimize the risk of bleeding.
Close monitoring during and after the procedure is essential, and appropriate adjustments to the treatment plan are made as needed. This proactive and individualized approach is key to ensuring patient safety and optimizing outcomes.
Q 26. What are the long-term outcomes and success rates associated with these treatments?
Long-term outcomes and success rates for laser and radiofrequency ablation are generally excellent. Studies show high success rates in eliminating or significantly reducing varicose veins and associated symptoms. The success rate often exceeds 90% at a five-year follow-up period for appropriately selected patients. However, several factors influence the long-term results.
Factors influencing long-term success include:
- The patient’s overall health: Comorbidities can affect outcomes.
- The skill and experience of the physician: Proper technique is crucial.
- The type of energy system used: Different systems have varying efficacies.
- Patient compliance with post-procedure instructions: This often involves compression therapy and lifestyle modifications.
While most patients experience lasting relief from symptoms, recurrence is possible, though typically at a low rate. Regular follow-up appointments allow for early detection and management of any recurrence.
Q 27. How do you assess the efficacy of laser/radiofrequency ablation?
Assessing the efficacy of laser/radiofrequency ablation involves a multi-faceted approach, combining clinical evaluation with imaging studies.
Methods of assessment include:
- Clinical examination: This includes evaluating the reduction or elimination of varicose veins, improvement in leg pain, swelling, and other symptoms.
- Ultrasound imaging: Post-procedural ultrasound helps to confirm the closure or obliteration of the treated veins. This is a crucial component of assessment.
- Patient-reported outcome measures: We utilize validated questionnaires to quantify symptom improvement from the patient’s perspective. This provides subjective but valuable information.
Combining these methods allows for a thorough and comprehensive assessment of treatment efficacy, enabling us to measure both objective and subjective improvements in patient condition.
Q 28. Describe a challenging case you encountered and how you managed it.
One challenging case involved a patient with extensive venous disease, including significant varicose veins and a history of deep vein thrombosis (DVT). This presented multiple challenges: The presence of DVT increased the risk of pulmonary embolism, and the extensive disease required a more extensive procedure.
My approach was multi-pronged:
- Thorough pre-operative assessment: This included extensive imaging studies (duplex ultrasound, venography) to map out the venous system thoroughly and assess the risks.
- Multi-modal treatment plan: Given the extent of the disease, I opted for a combined approach that included endovenous ablation of the major superficial veins, combined with phlebectomy (surgical removal of smaller varicose veins). This approach optimized treatment effectiveness and minimized the potential risks.
- Close monitoring during and after the procedure: The patient was carefully monitored for any signs of complications such as bleeding or pulmonary embolism. This involved frequent vital signs checks and close observation. Post-operative anticoagulation was managed conservatively.
- Patient education and support: The patient was fully educated about the risks and benefits of the procedure. Post-operative instructions were clearly communicated, including compression therapy and activity modification. This was crucial for a successful recovery.
While challenging, a careful, multi-faceted approach resulted in a successful outcome with no complications. This case highlighted the importance of thorough pre-operative planning, careful execution of the procedure, and close post-operative monitoring, particularly in patients with complex venous disease.
Key Topics to Learn for Laser and Radiofrequency Vein Ablation Interview
- Laser Ablation Mechanisms: Understand the principles of laser energy interaction with vein tissue, including selective photothermolysis and the impact of wavelength and power settings.
- Radiofrequency Ablation Mechanisms: Grasp the fundamentals of radiofrequency energy delivery, heat generation in vein walls, and the resulting tissue coagulation and contraction.
- Patient Selection Criteria: Learn to identify suitable candidates for laser and radiofrequency ablation based on vein size, location, and patient-specific factors like comorbidities.
- Procedure Techniques: Familiarize yourself with different catheter types, cannulation techniques, and energy delivery methods for both laser and radiofrequency ablation.
- Pre- and Post-operative Care: Understand the necessary preparations before the procedure and the post-operative management, including compression therapy and patient education.
- Complications and Management: Be prepared to discuss potential complications like hematoma, nerve injury, and deep vein thrombosis, and their management strategies.
- Imaging and Monitoring: Understand the role of ultrasound guidance during the procedure and the interpretation of pre- and post-procedural imaging (e.g., duplex ultrasound).
- Comparison of Laser and Radiofrequency Ablation: Be able to compare and contrast the advantages and disadvantages of each technique in various clinical scenarios.
- Emerging Technologies: Stay updated on advancements in laser and radiofrequency ablation technologies and their clinical implications.
- Troubleshooting and Problem-Solving: Develop your ability to anticipate and address potential challenges during the procedure, such as catheter malpositioning or inadequate tissue heating.
Next Steps
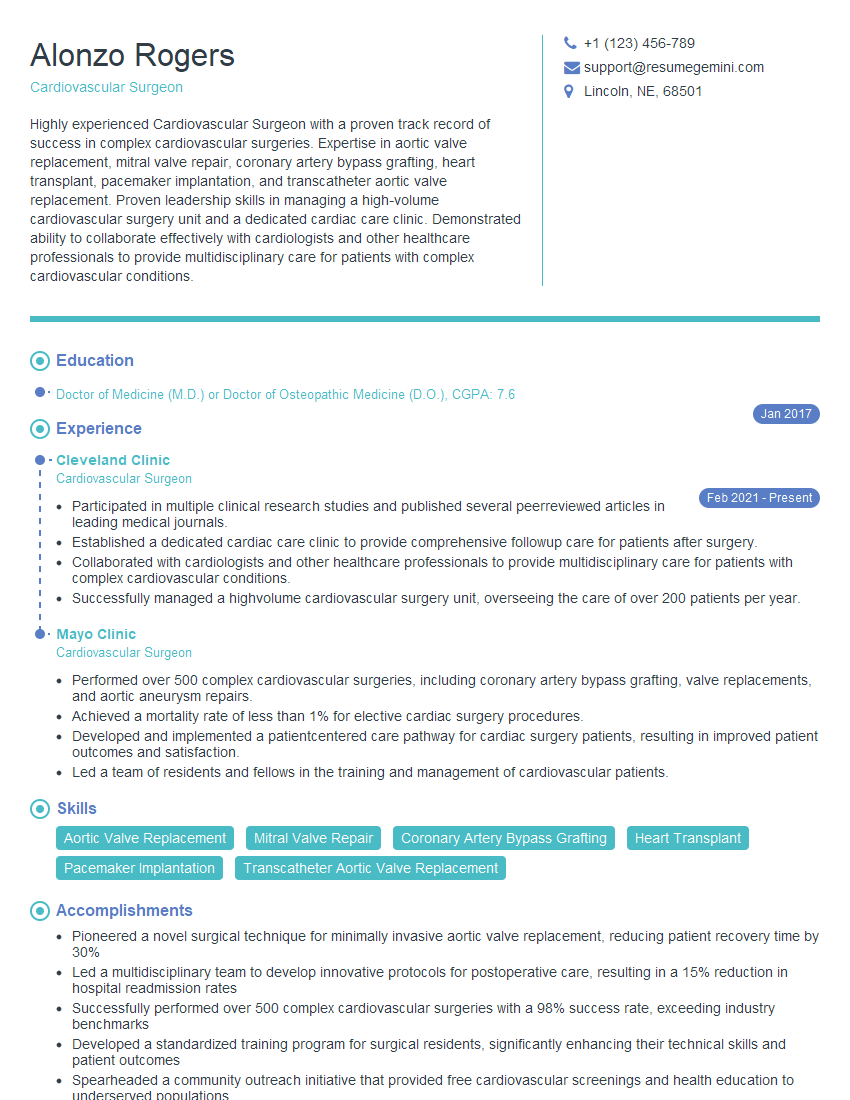
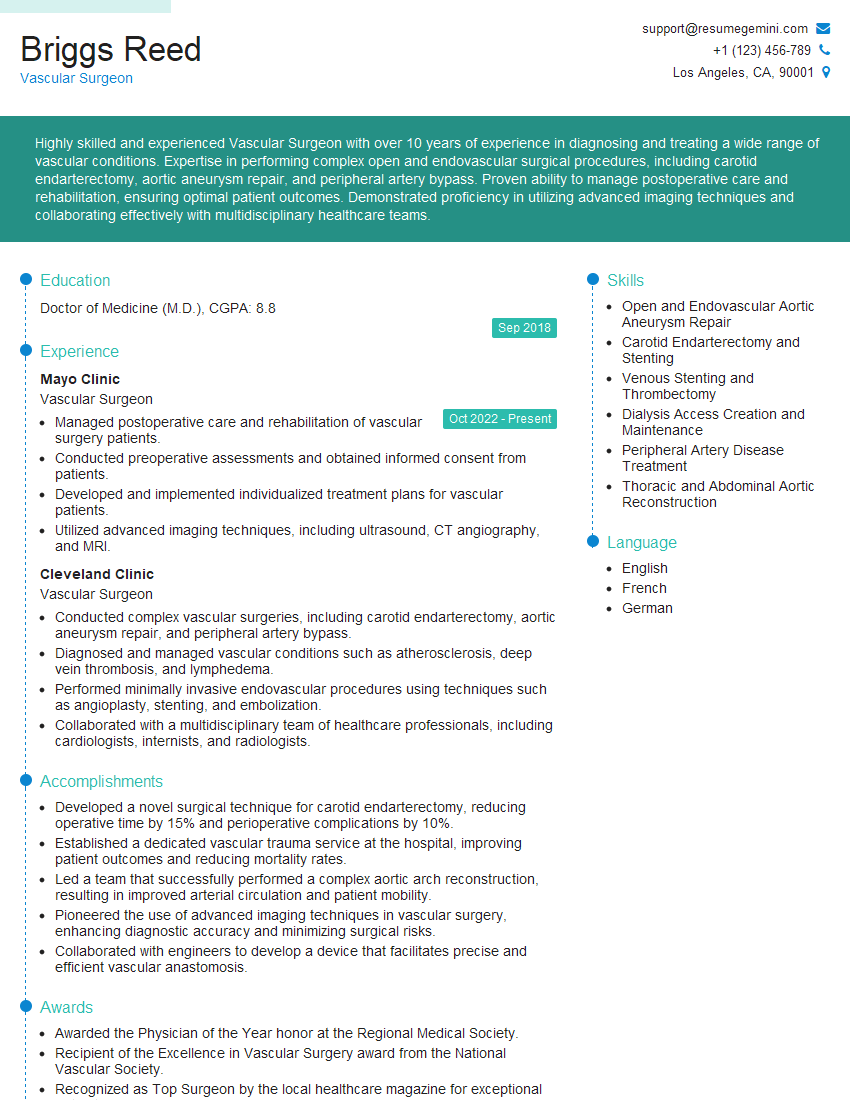
Mastering Laser and Radiofrequency Vein Ablation techniques is crucial for career advancement in vascular medicine. A strong understanding of these procedures significantly enhances your marketability and opens doors to specialized roles and higher earning potential. To secure your dream position, a well-crafted resume is essential. Creating an ATS-friendly resume is key to getting past applicant tracking systems and into the hands of hiring managers. We highly recommend using ResumeGemini to build a powerful, ATS-optimized resume that showcases your skills and experience effectively. ResumeGemini provides examples of resumes tailored specifically to Laser and Radiofrequency Vein Ablation professionals, ensuring your application stands out from the competition. Invest in your future – build a winning resume today.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.