Unlock your full potential by mastering the most common Medical Device and Technology Evaluation interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Medical Device and Technology Evaluation Interview
Q 1. Explain the differences between 510(k) clearance and PMA approval.
The FDA’s 510(k) clearance and Premarket Approval (PMA) pathways are both used for marketing medical devices in the United States, but they differ significantly in their requirements and the level of scrutiny involved. Think of it like this: a 510(k) is like getting a driver’s permit, while a PMA is like getting a full driver’s license.
510(k) Clearance: This pathway is used for devices that are substantially equivalent to a legally marketed predicate device. This means your new device is similar enough to an existing device that it’s deemed to have a similar safety and effectiveness profile. The FDA reviews your submission to assess this substantial equivalence. It’s a shorter, less rigorous process, making it suitable for devices with lower risk.
PMA Approval: This is the more stringent route, required for Class III devices (high risk) or for devices that don’t have a legally marketed predicate. Here, the manufacturer must submit extensive data, including clinical trial results, demonstrating the safety and effectiveness of their device. The FDA thoroughly reviews this data before granting approval. This is a longer, more complex process, reflecting the higher stakes involved with higher-risk devices.
In short: 510(k) is for devices that are similar to existing ones; PMA is for novel or high-risk devices requiring extensive pre-market testing and data.
Q 2. Describe your experience with ISO 13485.
ISO 13485:2016 is the internationally recognized standard for quality management systems (QMS) in the medical device industry. My experience with ISO 13485 is extensive, encompassing implementation, auditing, and continuous improvement within a range of medical device companies. I’ve personally led teams in developing and maintaining compliant QMSs, ensuring adherence to all clauses of the standard. This includes establishing procedures for design control, risk management, document control, internal audits, corrective and preventative actions (CAPA), and management review. I have hands-on experience with implementing effective change control systems, reducing errors and improving product quality. My involvement also extends to external audits conducted by Notified Bodies. I’ve directly addressed audit findings, ensuring timely resolution and driving improvements to our QMS. Furthermore, I have a thorough understanding of the transition from previous versions of ISO 13485.
Q 3. How do you conduct a risk analysis for a medical device?
Risk analysis for a medical device is a systematic process to identify, analyze, and control potential hazards. We typically use a structured approach like Failure Mode and Effects Analysis (FMEA) or Fault Tree Analysis (FTA).
FMEA: This involves identifying potential failure modes, assessing their severity, occurrence, and detectability, and calculating a risk priority number (RPN). A high RPN indicates a need for mitigation. For example, in a pacemaker, a failure mode could be battery depletion. We’d assess the severity (potential for patient harm), occurrence (likelihood of battery failure), and detectability (how easily the failure can be detected). Based on these, we’d implement controls like improved battery technology or low-battery alerts.
FTA: This is a top-down approach that starts with an undesired event (e.g., device malfunction) and works backward to identify the potential causes. It uses Boolean logic to show how different events can lead to the undesired event. This is especially useful for complex systems.
Ultimately, the goal is to create a risk management plan documenting identified hazards, their associated risks, and planned mitigation strategies. This process is iterative and continues throughout the device’s lifecycle.
Q 4. What are the key elements of a design control process?
Design control is the cornerstone of a robust medical device development process. It ensures that the final product meets its intended use and user needs while minimizing risks. Key elements include:
- Planning: Defining the design and development plan, including timelines, resources, and responsibilities.
- Input: Gathering requirements from various sources, including user needs, regulatory requirements, and technical specifications.
- Output: Defining specific design outputs and verifying their alignment with requirements.
- Design Review: Conducting formal reviews to assess the design’s adequacy and identify potential issues.
- Verification & Validation: Verifying that the design meets its specifications and validating that it meets user needs and intended use. This is often done through testing and simulations.
- Design Transfer: Transitioning the design to manufacturing and ensuring that the manufacturing process is capable of producing the device consistently.
- Design Changes: Establishing a controlled process for managing changes to the design after initial approval.
A well-defined design control process ensures traceability throughout the entire development lifecycle, allowing for easier troubleshooting, risk management, and regulatory compliance.
Q 5. Explain the concept of usability testing for medical devices.
Usability testing is crucial for medical devices to ensure that healthcare professionals and patients can effectively and safely use the device. It assesses the ease of use, efficiency, and satisfaction associated with the device. This involves observing users interacting with the device under realistic conditions. It’s not just about functionality; it’s about the overall user experience.
Methods include:
- Cognitive walkthroughs: Experts simulate user tasks to identify potential usability issues.
- Heuristic evaluation: Experts evaluate the design against established usability principles.
- User testing: Observing actual users performing tasks with the device, gathering feedback on their experience, and collecting performance metrics.
Usability testing helps identify design flaws early in the development process, reducing the likelihood of costly redesigns and improving the overall safety and effectiveness of the medical device. Imagine a complex infusion pump – usability testing ensures the healthcare professional can easily set the correct dosage and parameters, minimizing the risk of medication errors.
Q 6. Describe your experience with different types of medical device testing (e.g., biocompatibility, electrical safety).
My experience with medical device testing encompasses a broad spectrum of modalities, ensuring compliance with regulatory requirements and product safety. This includes:
- Biocompatibility Testing: Evaluating the device’s interaction with biological systems. This often involves in vitro and in vivo testing to assess cytotoxicity, sensitization, irritation, and genotoxicity. For instance, a heart valve would require extensive biocompatibility testing to ensure it doesn’t cause inflammation or blood clotting.
- Electrical Safety Testing: Verifying that the device meets relevant safety standards (e.g., IEC 60601-1). This includes tests for insulation resistance, leakage current, and protection against electric shock. A defibrillator, for example, would require rigorous electrical safety testing to ensure operator and patient safety.
- Mechanical Testing: Assessing the device’s mechanical properties, such as strength, durability, and fatigue resistance. For instance, a surgical instrument would be tested for its ability to withstand repeated use under stress.
- Performance Testing: Evaluating the device’s ability to perform its intended function. This could include testing accuracy, precision, and reliability. For a blood glucose monitor, this would include testing its accuracy against a reference method.
Each testing modality requires specific expertise, detailed protocols, and meticulous documentation to ensure the validity and reliability of the results.
Q 7. How do you ensure compliance with relevant FDA regulations?
Ensuring compliance with FDA regulations is paramount in the medical device industry. This is a continuous process, not a one-time event. My approach involves a multi-faceted strategy:
- Proactive Regulatory Strategy: Early engagement with the FDA to understand their expectations and to obtain pre-submission feedback on the device’s design and development plan. This helps to avoid costly delays later in the process.
- Comprehensive Quality System: Implementation and maintenance of a robust quality management system compliant with ISO 13485 and FDA’s Quality System Regulation (QSR) 21 CFR Part 820.
- Thorough Documentation: Meticulous record-keeping throughout the entire device lifecycle, including design inputs, design outputs, test results, and CAPA documentation. This provides traceability and transparency to the regulatory authorities.
- Regular Audits and Inspections: Conducting internal audits to identify and address potential compliance issues, preparing for and actively cooperating with FDA inspections.
- Post-Market Surveillance: Continuously monitoring the device’s performance in the field to identify and address any post-market issues.
Compliance is not merely about adhering to regulations; it’s about ensuring patient safety and building trust with the FDA. A proactive and well-documented approach minimizes risks and facilitates successful regulatory interactions.
Q 8. What is your experience with post-market surveillance?
Post-market surveillance (PMS) is the ongoing process of monitoring a medical device’s safety and performance after it’s been released to the market. It’s crucial for identifying potential problems that might not have been detected during pre-market evaluation. My experience encompasses various aspects of PMS, including designing and implementing surveillance plans, analyzing collected data (e.g., adverse event reports, field complaints, and performance data), and collaborating with regulatory bodies to address identified issues. For example, I worked on a PMS plan for a new implantable cardiac device. We established a robust system for collecting and analyzing data from patients, incorporating feedback from clinicians, and using statistical methods to detect trends indicating potential safety or performance problems. This led to the identification of a rare but serious complication, prompting a field safety correction and a subsequent software update to mitigate the risk.
The process typically involves defining key performance indicators (KPIs), establishing methods for data collection (e.g., through electronic health records, device registries, or direct contact with healthcare providers), and using statistical analysis techniques to identify trends and anomalies. A key element is proactive communication with regulatory agencies such as the FDA, keeping them informed of any significant findings and implementing corrective actions as needed.
Q 9. Explain the concept of design verification and validation.
Design verification and validation are distinct but complementary processes in medical device development, ensuring the device meets its intended use and performs safely and effectively. Design verification confirms that the device meets its pre-defined design specifications. Think of it as checking that you built the device correctly – according to the blueprints. Design validation, on the other hand, demonstrates that the device meets its intended use – that the resulting product actually does what it’s supposed to do in real-world conditions. It’s about checking if you built the right device.
- Verification often involves testing against predefined specifications (e.g., testing the strength of a material, the accuracy of a sensor, or the efficacy of a sterilization process). Methods could include simulations, bench testing, and component testing.
- Validation typically involves clinical trials or other in-vivo studies to demonstrate that the device performs effectively and safely in its intended clinical setting. It frequently involves rigorous statistical analysis of the data generated.
For instance, in developing a new drug delivery system, verification might focus on ensuring the precise release rate of the drug as defined in the design specifications. Validation would involve clinical trials to demonstrate that the system delivers the therapeutic dose effectively and safely to patients.
Q 10. Describe your experience with CAPA (Corrective and Preventive Actions).
Corrective and Preventive Actions (CAPA) is a systematic process for addressing identified non-conformances and preventing their recurrence. My experience includes developing and implementing CAPA plans, leading investigations into root causes of issues, and verifying the effectiveness of corrective actions. I’ve worked on CAPAs ranging from minor documentation errors to significant design flaws impacting product safety. A key aspect is thorough root cause analysis to prevent similar issues from recurring. We utilize various tools and methodologies, including the 5 Whys technique, fault tree analysis, and fishbone diagrams.
For example, during the production of a disposable diagnostic device, we identified a defect resulting in inaccurate test results. Our CAPA process involved meticulously investigating the root cause, identifying several contributing factors (e.g., a flaw in the manufacturing process, inadequate operator training, and insufficient quality checks), and implementing a comprehensive solution that addressed all identified factors. This solution included process improvements, staff retraining, upgraded quality control equipment, and improved documentation procedures. The effectiveness of these corrective actions was then rigorously monitored and documented.
Q 11. How do you handle conflicting requirements during the evaluation process?
Conflicting requirements are a common challenge during the medical device evaluation process. Handling them effectively requires a structured approach. The first step is clear documentation and communication of all requirements, identifying and prioritizing the conflicts. Next, a prioritization matrix can be used, weighting the relative importance of each conflicting requirement based on factors such as safety, regulatory compliance, and clinical efficacy. It’s crucial to involve stakeholders (e.g., engineers, clinicians, and regulatory affairs specialists) in the decision-making process to ensure a balanced and informed resolution.
Sometimes, compromise is necessary. Trade-off analysis allows for a systematic comparison of different solutions, weighing the benefits and risks of each option. In some cases, creative problem-solving might be required to identify new solutions that satisfy all or most of the conflicting requirements. Clear documentation of the decision-making process, including justifications for any compromises made, is essential for regulatory compliance and traceability.
Q 12. What is your experience with different types of medical device software validation?
My experience includes validating various types of medical device software, including software used in diagnostic equipment, therapeutic devices, and patient monitoring systems. This encompasses different validation approaches depending on the software’s criticality and intended function. For example, software with a direct impact on patient safety, such as the control software for a pacemaker, requires a higher level of rigor compared to a software component that provides only user interface functionality. I’ve worked extensively with risk-based approaches using the IEC 62304 standard, which emphasizes a systematic and proportionate approach to software validation. This involves:
- Hazard analysis: Identifying potential hazards associated with software failures.
- Risk assessment: Evaluating the likelihood and severity of those hazards.
- Software verification and validation: Implementing testing and analysis techniques (e.g., unit testing, integration testing, system testing, and usability testing) proportional to the level of risk.
Specific methods applied include unit testing, integration testing, system testing, and performance testing. We also conduct usability testing to ensure the software is intuitive and easy for healthcare professionals to use. Thorough documentation is crucial, ensuring traceability throughout the entire process.
Q 13. How do you evaluate the clinical effectiveness of a medical device?
Evaluating the clinical effectiveness of a medical device is a complex process that typically involves analyzing clinical data obtained from clinical trials, post-market surveillance, and real-world evidence. The approach differs depending on the device’s intended use and the available data. For high-risk devices, well-designed and rigorously conducted clinical trials are crucial, demonstrating clinical benefit and safety. These trials need to meet regulatory requirements and be conducted according to good clinical practice guidelines. The evaluation process includes statistical analysis of the data, comparing the device’s performance to existing treatment options or placebos. Key parameters include efficacy, safety, and tolerability. We also consider factors like the device’s cost-effectiveness and the impact on the patient’s quality of life.
For lower-risk devices, less extensive clinical evaluation might be sufficient, potentially using smaller studies, retrospective data analysis, or observational studies. Post-market surveillance data also plays a vital role in assessing long-term safety and effectiveness. Meta-analyses and systematic reviews of existing literature can also provide additional evidence of clinical effectiveness.
Q 14. Explain the importance of traceability in medical device development.
Traceability in medical device development is essential for ensuring the quality, safety, and regulatory compliance of the final product. It provides a complete and auditable record of all activities, decisions, and changes made throughout the entire product lifecycle. This includes a clear chain of documentation linking design requirements, design inputs, design outputs, verification and validation activities, manufacturing processes, and post-market surveillance. Good traceability helps to ensure that every aspect of the device’s development and production can be tracked and justified, simplifying investigations into issues, supporting regulatory audits, and facilitating continuous improvement.
For instance, traceability allows us to track the origin of a particular component, its performance during testing, its incorporation into the final device, and any subsequent changes made. This is essential for addressing non-conformances and performing root cause analysis. Traceability is typically achieved using a combination of documentation systems (e.g., design history files, change control records), unique identifiers for components and processes, and software tools to manage and track changes.
Q 15. Describe your experience with statistical analysis in medical device evaluation.
Statistical analysis is crucial in medical device evaluation to demonstrate safety and effectiveness. My experience encompasses a wide range of techniques, from descriptive statistics (like calculating means and standard deviations) to inferential statistics (like t-tests, ANOVA, and regression analysis). I’m proficient in using statistical software packages such as R and SPSS to analyze data from clinical trials, bench testing, and pre-clinical studies.
For instance, in evaluating a new blood pressure cuff, I’d use paired t-tests to compare the readings obtained from the new device against a gold standard device on the same patients. If evaluating multiple devices, ANOVA would be more appropriate. Furthermore, I’m adept at handling missing data and identifying outliers, ensuring the integrity of the analysis. Understanding the limitations of different statistical tests and selecting the appropriate method for the specific research question is paramount. I’ve also worked extensively with survival analysis techniques, relevant for assessing the lifespan or failure rate of implantable devices.
Beyond basic statistical tests, I have experience in developing and applying more advanced methods like generalized linear models, which are particularly useful for analyzing data with non-normal distributions or binary outcomes (e.g., success/failure of a procedure). My reports always include a clear interpretation of statistical results within the context of the device’s intended use and clinical significance.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your understanding of human factors engineering principles related to medical devices?
Human factors engineering (HFE) focuses on designing medical devices that are safe, effective, and user-friendly. My understanding of HFE principles centers around usability, ergonomics, and error prevention. This includes considering factors such as the physical dimensions and weight of the device, the clarity and intuitiveness of its controls and displays, and the potential for user error.
For example, I’ve been involved in evaluations where we assessed the usability of a new infusion pump through user testing, focusing on factors like the ease of programming, the clarity of the display, and the risk of accidental errors. We used techniques like task analysis and heuristic evaluation to identify areas for improvement in the design. We also employ various user-centered design methods, including iterative prototyping and usability testing, to refine the device’s design and user interface based on direct user feedback.
In addition to usability, HFE also encompasses considerations of environmental factors (e.g., lighting, noise levels), the cognitive load on the user, and potential fatigue. A well-designed device should minimize the cognitive burden on healthcare professionals, especially during critical procedures. A thorough HFE assessment considers the entire use environment and anticipates potential human errors to mitigate risks.
Q 17. How do you manage technical challenges during a medical device evaluation?
Managing technical challenges during medical device evaluation requires a systematic and proactive approach. My strategy involves a multi-step process:
- Problem Identification & Documentation: Thorough documentation of the challenge, including its nature, impact, and potential root causes. This might involve analyzing device logs, reviewing test data, and consulting with engineering staff.
- Root Cause Analysis: Employing techniques like fault tree analysis or Fishbone diagrams to determine the underlying reasons for the technical issue.
- Risk Assessment: Evaluating the potential risks associated with the challenge and their impact on the overall evaluation. This includes assessing the safety implications for patients and users.
- Mitigation Strategy: Developing a comprehensive plan to address the challenge, which could involve modifications to the testing protocol, device modifications, or alternative testing methods. This often requires collaboration with the device manufacturer.
- Documentation & Reporting: Clearly documenting all aspects of the technical challenge, the mitigation strategies employed, and the impact on the overall evaluation findings. This transparency is vital for regulatory submissions.
For example, if a device malfunctioned during a test, I would systematically investigate, potentially involving a failure analysis report from the manufacturer, to understand why it failed and if this failure is a genuine risk or an isolated incident. The evaluation would then be adjusted to reflect the findings, and the risk would be communicated transparently in the final report.
Q 18. What is your experience with different medical device technologies (e.g., implantable, diagnostic, therapeutic)?
My experience encompasses a broad range of medical device technologies, including implantable, diagnostic, and therapeutic devices. I’ve worked on evaluations of:
- Implantable Devices: Cardiac pacemakers, implantable defibrillators, and neurostimulators. This often involves evaluating biocompatibility, long-term performance, and the reliability of the device’s power source.
- Diagnostic Devices: Imaging systems (MRI, CT, ultrasound), in-vitro diagnostic tests (blood analyzers, genetic testing), and point-of-care diagnostic tools. This requires a strong understanding of diagnostic accuracy, sensitivity, and specificity.
- Therapeutic Devices: Surgical instruments, drug delivery systems, and minimally invasive surgical devices. This involves evaluating factors like device safety, effectiveness, and ease of use in a clinical setting.
Each device type presents unique challenges and requires specialized knowledge. My expertise lies in applying the appropriate evaluation methodologies and regulatory standards to each context, ensuring a comprehensive and rigorous assessment.
Q 19. Explain your process for writing a technical report on medical device evaluation.
My process for writing a technical report on medical device evaluation follows a structured format to ensure clarity and completeness:
- Introduction: Provides background information about the device, its intended use, and the objectives of the evaluation.
- Methods: Details the evaluation methodology, including the test methods, statistical analysis techniques, and the participants involved (if applicable).
- Results: Presents the findings of the evaluation, including both quantitative and qualitative data. This section uses tables, figures, and charts to effectively present the results.
- Discussion: Interprets the results in the context of the device’s intended use and compares them with relevant standards or benchmarks. This section also discusses any limitations of the evaluation.
- Conclusion: Summarizes the key findings and provides an overall assessment of the device’s safety and effectiveness.
- Appendices (if necessary): Includes supplementary materials such as raw data, statistical analysis outputs, and any other relevant documentation.
The report is written in a clear and concise manner, avoiding jargon wherever possible. It is tailored to the intended audience (e.g., regulatory agencies, manufacturers, or healthcare providers), and it always adheres to relevant regulatory guidelines and standards (e.g., ISO 14971, IEC 62304).
Q 20. How do you ensure data integrity in medical device testing?
Ensuring data integrity in medical device testing is paramount. My approach emphasizes a multi-layered strategy:
- SOPs and Protocols: Strict adherence to Standard Operating Procedures (SOPs) and detailed testing protocols that define data collection, handling, and analysis procedures.
- Calibration and Validation: Regular calibration and validation of all testing equipment to ensure accuracy and reliability.
- Chain of Custody: Maintaining a meticulous chain of custody for all samples and data, documenting every step of the process from collection to analysis.
- Data Logging and Tracking: Using electronic data capture systems and appropriate software to minimize manual data entry and ensure data traceability.
- Auditing and Verification: Regular internal audits and independent verification of data to detect and correct any errors or inconsistencies.
- Data Security: Implementing robust security measures to protect the data from unauthorized access, modification, or deletion.
For example, using electronic signatures and audit trails for all data modifications ensures transparency and accountability. Any deviations from SOPs are meticulously documented and justified. This rigorous approach minimizes bias and ensures the reliability and validity of the test results.
Q 21. Describe your experience with regulatory submissions.
My experience with regulatory submissions includes supporting the preparation of documentation for submissions to regulatory bodies such as the FDA (in the US) and the EMA (in Europe). This involves:
- Understanding Regulatory Requirements: A thorough grasp of the applicable regulations and standards for the specific device type and intended use.
- Documentation Preparation: Compiling and preparing all the necessary documentation for the submission, including technical files, clinical data, and risk management reports. This process requires meticulous attention to detail and accuracy.
- Submission Preparation and Management: Formatting and submitting the regulatory documentation according to the specific requirements of the regulatory body. This often involves using specialized submission software and navigating complex electronic systems.
- Responding to Regulatory Feedback: Effectively addressing any questions or concerns raised by regulatory reviewers, providing clear and concise responses supported by evidence.
I have been involved in both pre-market and post-market submissions, navigating the complexities of each regulatory pathway. This experience includes managing interactions with regulatory bodies, addressing their queries, and obtaining necessary approvals. It is crucial to have a strong understanding of both regulatory requirements and the technical aspects of the device to successfully navigate this process.
Q 22. How familiar are you with IEC 60601-1 (medical electrical equipment)?
IEC 60601-1 is the cornerstone of safety standards for medical electrical equipment. It’s a comprehensive collection of standards that define the basic safety and essential performance requirements for these devices. Think of it as the rulebook ensuring that medical devices won’t harm patients or clinicians during their use. I’m extremely familiar with it, having used it extensively throughout my career in risk management and device evaluation. My experience includes reviewing design documentation, testing reports, and participating in audits to ensure compliance. I’m knowledgeable about all parts of the standard, including:
- Basic Safety: This covers aspects like electrical safety, mechanical safety, and protection against various hazards like fire and overheating.
- Essential Performance: This ensures the device functions as intended and provides the necessary clinical performance, without compromising safety.
- EMC (Electromagnetic Compatibility): This addresses the device’s ability to operate without causing interference or being affected by interference from other devices or environmental sources.
For example, I once worked on a project where a new infusion pump needed to meet IEC 60601-1. We conducted rigorous testing to verify the pump’s protection against electrical shocks, and ensured it met EMC requirements to avoid interference with other medical equipment in a hospital setting.
Q 23. What is your approach to identifying and mitigating potential risks associated with medical devices?
My approach to risk management follows a structured, systematic process. It starts with a thorough hazard analysis, identifying all potential hazards associated with the device throughout its entire lifecycle—from design and manufacturing to use and disposal. This involves brainstorming sessions with the design team, reviewing relevant literature, and conducting user-needs analysis. Tools like Failure Mode and Effects Analysis (FMEA), which I will elaborate on later, are crucial here.
Once hazards are identified, I evaluate their severity, probability of occurrence, and the ability to detect them. This helps prioritize risks. Mitigating risks involves implementing control measures, which can range from design modifications to warnings and instructions for use. We then verify the effectiveness of these controls through testing and ongoing monitoring. A key element is documenting all these steps meticulously. For instance, if a hazard is identified as a potential for electrical shock, mitigation could involve adding insulation, implementing ground fault protection, and including prominent warning labels.
Q 24. How do you stay current with the latest regulations and standards in the medical device industry?
Staying current in the rapidly evolving medical device regulatory landscape is paramount. I achieve this through a multi-pronged approach:
- Subscription to Regulatory Newsletters and Databases: I actively subscribe to newsletters and databases from organizations like the FDA, the IEC, and other relevant regulatory bodies. These provide timely updates on new regulations and guidance documents.
- Attendance at Industry Conferences and Webinars: Attending conferences and webinars allows for direct engagement with leading experts, offering valuable insights into the latest regulatory developments and best practices.
- Networking with Colleagues and Industry Professionals: Regular interaction with colleagues and experts provides valuable information sharing and facilitates a proactive approach to regulatory compliance.
- Continuous Professional Development: I actively pursue continuing education opportunities relevant to medical device regulations and standards to stay abreast of changes.
This constant vigilance ensures my work remains compliant and aligned with current best practices.
Q 25. Explain your understanding of Design Failure Mode and Effects Analysis (DFMEA).
Design Failure Mode and Effects Analysis (DFMEA) is a proactive risk assessment technique used to identify potential failures in a design and assess their potential impact. It’s a systematic process aimed at preventing failures *before* they occur. It’s like a preemptive strike against potential problems. The process involves:
- Defining the Function: Clearly outlining the intended function of the device or its components.
- Identifying Potential Failure Modes: Brainstorming all ways the device or component could fail.
- Assessing Severity: Evaluating the potential harm caused by each failure mode. This is often rated on a scale (e.g., 1-10).
- Assessing Occurrence: Estimating the likelihood of each failure mode happening.
- Assessing Detection: Determining the likelihood of detecting the failure before it reaches the user.
- Calculating the Risk Priority Number (RPN): Multiplying the Severity, Occurrence, and Detection ratings to obtain the RPN. Higher RPN indicates higher risk.
- Developing and Implementing Control Plans: Creating and putting into action solutions to mitigate the risks associated with the highest-RPN failure modes. These might involve design changes, testing procedures, or warning labels.
- Review and Update: Regularly reviewing the DFMEA and updating it as needed based on testing results, feedback, or design changes.
For example, in the design of a surgical robot, a DFMEA might identify a potential failure mode as a motor malfunction. The severity could be high (potential for patient harm), the occurrence might be moderate (depending on motor quality), and detection might be low (unless specific tests are implemented). A high RPN would then trigger the implementation of robust testing and potentially using a redundant motor system to mitigate risk.
Q 26. How do you collaborate with cross-functional teams during medical device evaluation?
Collaboration is essential in medical device evaluation. I believe in a highly collaborative approach, working closely with diverse teams including:
- Engineering: Understanding design choices and technical specifications is crucial for evaluating safety and performance.
- Clinical Affairs: Clinical data and user feedback are vital for assessing the device’s effectiveness and potential risks in real-world scenarios.
- Regulatory Affairs: Ensuring compliance with regulations is a top priority, requiring close coordination.
- Quality Assurance: Verifying that processes are in place to ensure product quality and safety.
- Manufacturing: Understanding manufacturing processes is vital for assessing potential sources of failure.
I facilitate communication using regular meetings, shared documentation, and clear communication channels. I prioritize open discussion, encouraging each team member to contribute their expertise. This collaborative spirit fosters a shared understanding of the device and its associated risks, leading to more effective evaluation and mitigation strategies.
Q 27. Describe your experience with quality management systems (QMS).
I have extensive experience with Quality Management Systems (QMS), primarily based on ISO 13485. This standard provides the framework for establishing and maintaining a robust quality management system within the medical device industry. My experience encompasses:
- Internal Audits: Conducting internal audits to ensure the QMS is effectively implemented and maintained.
- Supplier Management: Evaluating suppliers to ensure they meet the quality requirements needed for medical device manufacturing.
- CAPA (Corrective and Preventive Action): Participating in the process of identifying, investigating, and addressing deviations and nonconformances.
- Documentation Review: Reviewing design documentation, manufacturing records, and other relevant documents to ensure compliance.
- Management Review: Participating in management review meetings to assess the effectiveness of the QMS and identify areas for improvement.
I understand the importance of a well-documented and rigorously implemented QMS for ensuring the safety and quality of medical devices. In a previous role, I helped a company successfully transition to ISO 13485, leading to improved product quality and regulatory compliance.
Q 28. What is your experience with medical device cybersecurity?
Medical device cybersecurity is a critical and increasingly important aspect of medical device evaluation. My experience includes understanding the vulnerabilities and threats associated with connected medical devices, such as implantable devices, infusion pumps, and diagnostic imaging equipment. This includes:
- Risk Assessment for Cybersecurity Threats: Identifying potential vulnerabilities in the device’s software and hardware and assessing the potential impact of cyberattacks.
- Review of Security Controls: Evaluating the effectiveness of security controls implemented by the manufacturer, such as authentication mechanisms, encryption, and access control.
- Compliance with Cybersecurity Regulations: Staying up to date with evolving cybersecurity regulations and guidance documents and ensuring that the device meets those standards.
- Vulnerability Testing: Participating in penetration testing or vulnerability assessments to identify and mitigate potential security weaknesses.
- Incident Response Planning: Understanding incident response processes to address and minimize the impact of a cyberattack.
For example, I recently reviewed the cybersecurity aspects of a remotely controlled insulin pump. This required reviewing its software architecture, evaluating its authentication protocols, and assessing the potential impact of a successful cyberattack. We identified several areas of potential vulnerability and recommended design modifications to strengthen the system’s cybersecurity posture.
Key Topics to Learn for Medical Device and Technology Evaluation Interview
- Regulatory Landscape: Understand FDA regulations (510(k), PMA, de novo), EU MDR, and other international standards. Consider the impact of these regulations on the evaluation process.
- Risk Management: Learn about risk analysis methodologies (e.g., FMEA, FTA) and their application in evaluating device safety and efficacy. Be prepared to discuss practical examples of risk mitigation strategies.
- Clinical Evaluation: Familiarize yourself with the design and execution of clinical trials, including data analysis and interpretation. Understand the different types of clinical evidence and their relative strengths.
- Performance Evaluation: Master the methodologies for evaluating device performance characteristics, including accuracy, precision, sensitivity, and specificity. Be prepared to discuss different testing methods and their limitations.
- Biocompatibility: Understand the principles of biocompatibility testing and the regulatory requirements for demonstrating biocompatibility. Be able to discuss different biocompatibility test methods.
- Usability Engineering: Familiarize yourself with usability testing methodologies and their application to medical devices. Be prepared to discuss how usability impacts safety and effectiveness.
- Data Integrity and Analysis: Understand the principles of good data management and analysis in the context of medical device evaluation. Be prepared to discuss statistical methods and data visualization techniques.
- Quality Systems: Understand the role of quality systems (e.g., ISO 13485) in ensuring the quality and safety of medical devices throughout their lifecycle.
- Post-Market Surveillance: Understand the importance of post-market surveillance and the methods used to monitor device performance and identify potential safety issues.
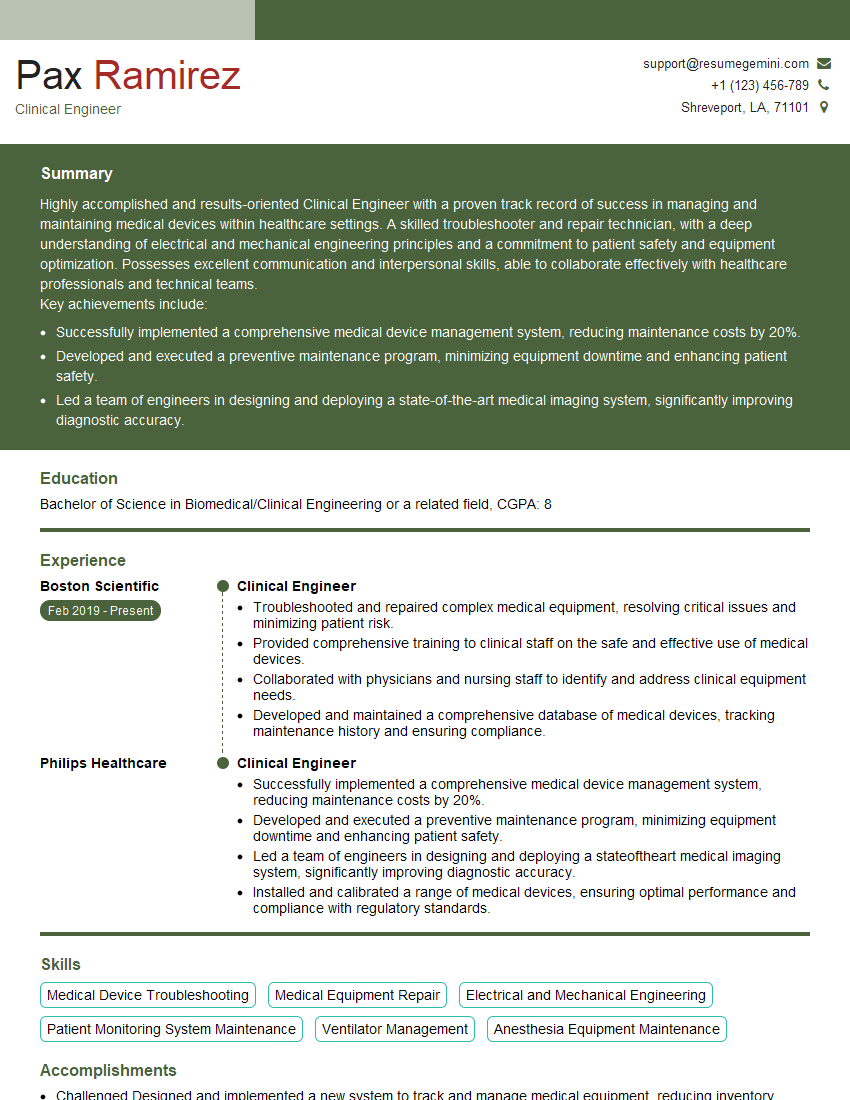
Next Steps
Mastering Medical Device and Technology Evaluation opens doors to exciting and impactful careers in a rapidly growing field. Demonstrating a strong understanding of these concepts is crucial for securing your dream role. To significantly enhance your job prospects, focus on creating a compelling and ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource that can help you build a professional and effective resume tailored to the specific requirements of this field. Examples of resumes tailored to Medical Device and Technology Evaluation are available to help guide you. Take the next step towards your career success today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.