Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Medical Ethics and Legal Compliance interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Medical Ethics and Legal Compliance Interview
Q 1. Explain the concept of informed consent in a medical setting.
Informed consent is a cornerstone of medical ethics and legal practice. It ensures patients have the autonomy to make decisions about their own healthcare. This means they must be fully informed about their condition, proposed treatment options (including potential benefits and risks), alternative treatments, and the option of refusing treatment altogether. The process involves a conversation between the healthcare provider and patient, ensuring understanding and agreement before any procedure or treatment commences.
- Understanding: The patient must comprehend the information provided, which may require the healthcare provider to use plain language, visual aids, or interpreters as needed.
- Voluntariness: The patient must give consent freely, without coercion or undue influence from family, friends, or healthcare providers.
- Capacity: The patient must possess the mental capacity to understand the information and make a reasoned decision. This may involve assessing their cognitive abilities and considering the impact of any medical conditions.
Example: Imagine a patient scheduled for knee replacement surgery. Informed consent requires the surgeon to explain the procedure, potential complications (infection, blood clots, etc.), success rates, and alternative treatments (e.g., physical therapy). The patient should then be given ample time to ask questions and reflect before signing the consent form. If the patient does not understand something, it is the physician’s responsibility to clarify the information.
Q 2. Describe the key provisions of HIPAA.
The Health Insurance Portability and Accountability Act (HIPAA) is a US federal law designed to protect the privacy and security of patients’ health information. Its key provisions revolve around:
- Privacy Rule: This dictates how protected health information (PHI) can be used and disclosed. It establishes specific requirements for obtaining patient consent, allowing patients access to their own medical records, and implementing safeguards to prevent unauthorized access or breaches.
- Security Rule: This outlines administrative, physical, and technical safeguards healthcare providers must implement to ensure the confidentiality, integrity, and availability of electronic PHI (ePHI).
- Breach Notification Rule: This mandates the notification of individuals and authorities in the event of a data breach affecting their PHI.
- Enforcement Rule: This outlines the processes for investigating complaints, imposing sanctions, and ensuring compliance.
HIPAA’s impact extends to all covered entities, such as healthcare providers, health plans, and healthcare clearinghouses, and their business associates. It’s crucial to note that HIPAA is not just a set of rules; it’s a comprehensive framework for building trust and maintaining the ethical handling of sensitive patient information.
Q 3. What are the ethical considerations surrounding end-of-life care?
Ethical considerations surrounding end-of-life care are complex and deeply personal. They often involve navigating conflicting values and beliefs. Key ethical considerations include:
- Patient autonomy: Respecting the patient’s right to make decisions about their own care, including the right to refuse treatment and choose a course of action aligned with their values and wishes (e.g., through advance directives like living wills and durable power of attorney for healthcare).
- Beneficence: Acting in the best interest of the patient, which may include providing comfort and palliative care, even if it doesn’t cure the underlying condition.
- Non-maleficence: Avoiding causing harm, including unnecessary pain and suffering. This involves careful consideration of treatments and ensuring a peaceful and dignified end of life.
- Justice: Ensuring equitable access to quality end-of-life care, regardless of a patient’s social status, economic background, or insurance coverage.
Discussions involving family members, spiritual advisors, and palliative care teams play a critical role in providing holistic support. The goal is to provide compassionate care that respects the patient’s dignity and autonomy while alleviating suffering.
Q 4. How would you handle a conflict between patient autonomy and physician paternalism?
Conflicts between patient autonomy and physician paternalism are common in healthcare. Physician paternalism is the belief that a doctor knows what’s best for the patient and should make decisions on their behalf. However, modern medical ethics emphasizes patient autonomy. Resolving this conflict requires a delicate balance.
Step-by-step approach:
- Open communication: Engage in a thorough discussion with the patient, actively listening to their concerns, values, and preferences.
- Shared decision-making: Present all relevant information about the patient’s condition, treatment options, potential benefits and risks, and the implications of each choice. This allows the patient to participate actively in the decision-making process.
- Respectful disagreement: If the physician believes a patient’s choice is not in their best interest, the physician should explain their rationale clearly and respectfully, but ultimately, the patient’s decision must be honored, provided they have the capacity to make one.
- Ethical consultation: In complex or challenging cases, seeking guidance from an ethics committee or experienced colleagues can provide valuable insights and support.
Example: A patient with a terminal illness refuses life-sustaining treatment. While the physician may want to prolong the patient’s life, respecting the patient’s autonomy means accepting their decision and focusing on providing comfort and palliative care.
Q 5. Explain the process of conducting a compliance audit in a healthcare facility.
A compliance audit in a healthcare facility is a systematic review of policies, procedures, and practices to ensure adherence to relevant laws and regulations, including HIPAA, state regulations, and internal policies. The process typically involves:
- Planning: Defining the scope of the audit, identifying key areas of focus (e.g., data security, informed consent practices, billing procedures), and establishing a timeline.
- Data collection: Gathering relevant documentation such as policies, procedures, training records, incident reports, and patient records (with appropriate authorization). This may involve reviewing electronic health records, conducting interviews, and observing workplace practices.
- Analysis: Evaluating the collected data against relevant regulatory requirements and internal policies to identify gaps, inconsistencies, or areas of non-compliance.
- Reporting: Summarizing the findings, identifying areas of strength and weakness, and recommending corrective actions to address identified compliance issues.
- Corrective action plan: Implementing the recommended changes and regularly monitoring effectiveness to prevent recurrence of issues.
Example: An audit might focus on ensuring proper authorization for accessing patient records. The auditor might review access logs, interview staff, and examine policies to determine whether sufficient safeguards are in place to prevent unauthorized access.
Q 6. What are the potential legal consequences of violating HIPAA regulations?
Violating HIPAA regulations can lead to serious legal and financial consequences. Penalties vary depending on the nature and severity of the violation, whether it was intentional or negligent, and the entity’s history of compliance. Potential consequences include:
- Civil monetary penalties (CMPs): Significant fines ranging from a few thousand to hundreds of thousands of dollars per violation.
- Criminal penalties: In cases of willful neglect or intentional breaches, criminal charges can be filed, resulting in imprisonment and substantial fines.
- Reputational damage: Breaches can severely damage a healthcare facility’s reputation and erode public trust.
- Loss of business: Hospitals and other healthcare providers might experience a reduction in patient volume and contracts due to a tarnished reputation.
- Lawsuits: Individuals whose PHI was compromised might file civil lawsuits seeking compensation for damages.
It’s crucial for healthcare entities to invest in robust compliance programs, staff training, and effective data security measures to mitigate the risk of violating HIPAA and facing these repercussions.
Q 7. How do you ensure patient confidentiality in electronic health records?
Ensuring patient confidentiality in electronic health records (EHRs) requires a multi-layered approach incorporating technical, administrative, and physical safeguards:
- Access control: Implementing robust authentication mechanisms (e.g., strong passwords, multi-factor authentication) and authorization controls to limit access to EHRs based on roles and responsibilities. Only authorized personnel should have access to specific patient data.
- Data encryption: Encrypting data both in transit and at rest to protect it from unauthorized access even if a breach occurs.
- Audit trails: Maintaining detailed audit trails of all EHR access and modifications to track who accessed what information and when, facilitating investigations of potential breaches.
- Regular security updates and vulnerability assessments: Keeping EHR systems up-to-date with security patches and regularly conducting vulnerability assessments to identify and address potential security weaknesses.
- Employee training and education: Providing comprehensive training to staff on HIPAA regulations, data security practices, and the importance of protecting patient confidentiality.
- Data backup and disaster recovery: Implementing robust backup and recovery procedures to ensure data availability and prevent data loss in case of system failures or natural disasters.
Beyond these technical aspects, fostering a strong culture of confidentiality within the healthcare organization is crucial. This involves emphasizing the ethical obligations of staff and promoting a commitment to protecting patient privacy.
Q 8. Describe your understanding of medical malpractice and negligence.
Medical malpractice and negligence are both forms of professional misconduct in healthcare, but they differ slightly in their legal definitions. Negligence is a broader term encompassing a failure to exercise the care that a reasonably prudent person would exercise in similar circumstances. In medicine, this translates to a doctor, nurse, or other healthcare professional not providing the standard of care expected of someone with their training and experience. Medical malpractice, on the other hand, is a specific type of negligence that involves a breach of the duty of care owed to a patient by a healthcare provider, resulting in injury or harm to the patient. To prove malpractice, a plaintiff must demonstrate that a breach of the standard of care occurred, that the breach directly caused injury, and that damages resulted.
For example, a nurse failing to properly administer medication (negligence) could lead to a patient experiencing adverse effects, constituting medical malpractice if the harm was directly caused by the improper administration and the nurse’s actions fell below the accepted standard of care. Think of it like this: Negligence is a general failure to act responsibly, while malpractice is negligence specifically in a medical context leading to demonstrable harm.
Q 9. What is the role of an ethics committee in a hospital?
A hospital ethics committee plays a crucial role in navigating complex ethical dilemmas arising in patient care, research, and hospital operations. These committees are typically multidisciplinary, including physicians, nurses, ethicists, clergy, legal professionals, and patient representatives. Their primary function is to provide guidance and recommendations on ethically challenging cases, ensuring patient autonomy, beneficence, non-maleficence, and justice are upheld.
- Case Review: They review cases involving difficult clinical decisions, such as end-of-life care, withholding or withdrawing treatment, or the use of experimental therapies.
- Policy Development: They contribute to the development of hospital policies related to ethics, patient rights, and research integrity.
- Education: They educate healthcare professionals about ethical principles and standards of conduct.
- Conflict Resolution: They help resolve conflicts among patients, families, and healthcare professionals regarding ethical issues.
For instance, an ethics committee might be consulted when a patient lacks decision-making capacity and the family disagrees about the course of treatment. The committee would guide the decision-making process by considering the patient’s best interests and wishes, whenever possible, while respecting the family’s values and concerns.
Q 10. How would you address a situation where a colleague is engaging in unethical behavior?
Addressing unethical behavior by a colleague requires a sensitive and structured approach. The first step is to gather evidence documenting the unethical conduct. Then, I would directly address the colleague privately, expressing my concerns in a non-accusatory manner and focusing on the impact of their actions. It’s important to maintain a professional tone and prioritize open communication. If this informal approach is unsuccessful, I would escalate the matter to my supervisor or the hospital’s ethics committee, following established internal procedures for reporting unethical conduct. Depending on the severity and nature of the misconduct, further action might involve reporting to the relevant licensing board or regulatory agency.
For example, if a colleague consistently falsifies patient records, I would first speak to them privately, explaining the severity of this breach of ethics and potential legal repercussions. If the behavior continues, I would then report it to my supervisor and the appropriate authorities. This ensures patient safety and upholds the integrity of the healthcare profession.
Q 11. Explain the difference between clinical negligence and medical malpractice.
While closely related, clinical negligence and medical malpractice are not interchangeable. Clinical negligence refers to any instance where a healthcare professional fails to provide the standard of care expected of a reasonably competent professional in their field, regardless of whether it results in harm. Medical malpractice, however, requires proof of negligence and resulting harm. In essence, medical malpractice is a subset of clinical negligence.
Imagine a doctor misdiagnoses a patient’s condition (clinical negligence). If the misdiagnosis doesn’t cause any harm, it remains clinical negligence. However, if the misdiagnosis leads to a worsening of the patient’s condition, requiring extensive further treatment and causing significant distress, it then becomes medical malpractice due to the demonstrable harm caused by the negligent act.
Q 12. What are the ethical implications of using artificial intelligence in healthcare?
The use of artificial intelligence (AI) in healthcare presents significant ethical implications. Bias is a major concern; algorithms trained on biased data can perpetuate and amplify existing health disparities, leading to unequal access to care and inaccurate diagnoses for certain populations. Data privacy and security are paramount, as AI systems often require access to sensitive patient information, raising concerns about breaches and misuse of data. Transparency and explainability are crucial – it’s ethically important to understand how AI systems arrive at their conclusions, especially in high-stakes decisions like diagnosis and treatment planning. Finally, accountability needs careful consideration – who is responsible when an AI system makes an error with potentially harmful consequences?
For example, an AI algorithm used for risk prediction might show bias against certain racial groups if the training data disproportionately reflects those groups’ historical experiences. Ensuring fairness and equity in the design, development, and deployment of AI systems is crucial to mitigate these risks and promote ethical and responsible innovation in healthcare.
Q 13. Discuss the ethical considerations of genetic testing and screening.
Genetic testing and screening raise complex ethical considerations. Autonomy: Individuals have the right to decide whether or not to undergo testing and to know or not know the results. Privacy and confidentiality: Genetic information is highly sensitive and its protection is crucial. Informed consent: Individuals must fully understand the implications of testing before consenting, including potential psychological and social consequences. Discrimination: Concerns exist about genetic discrimination in employment, insurance, and other areas. Reproductive rights: Genetic testing can raise questions about reproductive choices, such as prenatal diagnosis and selective abortion. Family implications: Genetic information about one individual can reveal information about their family members, raising issues of familial responsibility and disclosure.
For example, a couple considering genetic testing before pregnancy might face difficult decisions if the test reveals a high risk of a serious genetic condition in their child. Ensuring they have access to adequate genetic counseling and support to navigate these choices ethically is crucial.
Q 14. How do you navigate conflicts of interest in medical research?
Navigating conflicts of interest in medical research requires a proactive and transparent approach. Disclosure is critical – researchers must disclose any potential conflicts of interest, such as financial ties to pharmaceutical companies or other entities that could influence their research findings. Independent review by ethics committees and institutional review boards (IRBs) is essential to assess the potential impact of conflicts of interest on research integrity. Implementing strict guidelines on financial relationships, gifts, and consulting arrangements can help mitigate the risk of bias. Finally, prioritizing transparency in research methods, data collection, and publication processes fosters trust and accountability.
For example, a researcher receiving funding from a pharmaceutical company to study a new drug must fully disclose this funding source in their research publications and grant applications. This ensures transparency and allows others to assess the potential influence of the funding on the research results.
Q 15. What are the key elements of a strong compliance program?
A strong compliance program is the backbone of any healthcare organization, ensuring ethical conduct and adherence to all applicable laws and regulations. It’s not just a set of rules; it’s a culture. Key elements include:
Written Policies and Procedures: Clear, concise, and readily accessible documentation outlining ethical and legal expectations for all staff, encompassing areas like patient privacy (HIPAA), billing practices, and conflict of interest.
Designated Compliance Officer: A responsible individual with the authority and resources to oversee the program, conduct regular audits, and investigate potential violations.
Effective Training and Education: Regular, comprehensive training for all employees covering relevant regulations, ethical dilemmas, and reporting procedures. This shouldn’t be a one-time event, but an ongoing process.
Hotlines and Reporting Mechanisms: Confidential channels for reporting suspected violations, ensuring staff feel comfortable speaking up without fear of retaliation. These should be well-publicized and easy to access.
Monitoring and Auditing: Regular audits of billing practices, medical records, and other relevant areas to identify potential compliance gaps and areas needing improvement. This proactive approach helps prevent problems before they arise.
Corrective Action Plans: A clear process for addressing identified violations, including investigation, remediation, and prevention of future occurrences. This includes disciplinary action where appropriate.
Regular Review and Updates: Healthcare regulations are constantly evolving. The compliance program must be regularly reviewed and updated to reflect changes in laws, guidelines, and best practices.
For example, a hospital might conduct regular audits of its coding practices to ensure accurate billing and avoid potential violations of the False Claims Act. A strong compliance program will also include a robust system for handling patient complaints related to potential ethical violations.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you respond to a patient complaint related to a potential ethical violation?
Responding to a patient complaint about a potential ethical violation requires a calm, professional, and thorough approach. My first step would be to listen empathetically to the patient’s concerns, ensuring they feel heard and understood. I would then document the complaint meticulously, including details about the alleged violation, the date, the individuals involved, and any supporting evidence.
Next, I would initiate a confidential investigation, following established protocols. This might involve interviewing witnesses, reviewing medical records, and consulting with legal counsel and the compliance officer. The goal is to gather all relevant information to determine if an ethical violation occurred.
Depending on the findings, appropriate actions would be taken, which could include: providing a sincere apology to the patient, implementing corrective actions, initiating disciplinary measures for staff involved, and reporting the incident to relevant regulatory bodies if necessary. Transparency and open communication with the patient throughout the process are crucial, even if the investigation doesn’t reveal a violation. Maintaining patient confidentiality is paramount throughout the process.
For instance, if a patient alleges a physician disclosed their medical information without consent, a thorough investigation would be conducted, potentially involving interviews with the physician and review of the patient’s medical records to determine if HIPAA regulations were violated.
Q 17. Describe your understanding of the Stark Law and Anti-Kickback Statute.
The Stark Law and the Anti-Kickback Statute are federal laws designed to prevent fraud and abuse in healthcare. They aim to curb conflicts of interest that could compromise the quality of patient care.
Stark Law (Physician Self-Referral Law): This law prohibits physicians from referring Medicare and Medicaid patients for certain designated health services (DHS) to entities with which the physician or an immediate family member has a financial relationship, unless an exception applies. The aim is to prevent physicians from profiting from referrals. For example, a cardiologist owning a cardiac imaging center cannot refer patients to that center without meeting specific exceptions outlined in the law.
Anti-Kickback Statute (AKS): This law makes it a criminal offense to knowingly and willfully offer, pay, solicit, or receive anything of value to induce or reward referrals of items or services reimbursable by a federal healthcare program. This broadly aims to prevent improper inducements to steer patients towards particular providers. For instance, offering a physician a free vacation in exchange for patient referrals would be a clear violation.
Both laws are complex and have numerous exceptions. Understanding these nuances is crucial for maintaining compliance. Failure to comply can result in significant penalties, including hefty fines, exclusion from federal healthcare programs, and even criminal prosecution.
Q 18. Explain the process for reporting a potential violation of healthcare regulations.
Reporting a potential violation of healthcare regulations varies depending on the nature of the violation and the organization involved. However, a general process usually includes:
Internal Reporting: First, report the potential violation to the organization’s designated compliance officer or through an established internal reporting mechanism (e.g., a hotline or ethics committee).
Documentation: Maintain detailed documentation of the incident, including dates, times, individuals involved, and any evidence supporting the potential violation.
Investigation: The compliance officer will typically conduct a thorough investigation to determine whether a violation occurred.
External Reporting (if necessary): If the internal investigation confirms a violation or if the organization fails to adequately address the issue, external reporting may be necessary. This might involve contacting relevant federal or state agencies, such as the Office of Inspector General (OIG), the Centers for Medicare & Medicaid Services (CMS), or the state attorney general’s office.
Whistleblower Protection: Laws exist to protect whistleblowers from retaliation for reporting suspected violations. This protection encourages individuals to come forward with concerns without fear of losing their jobs or facing other adverse consequences.
It is vital to follow the established reporting procedures within your organization while being mindful of legal and ethical responsibilities to protect patient safety and maintain compliance.
Q 19. How do you ensure compliance with state and federal regulations in your work?
Ensuring compliance with state and federal regulations requires a multi-faceted approach. I actively stay informed about changes in regulations through several methods:
Subscription to Regulatory Updates: I subscribe to newsletters, journals, and online resources that provide updates on changes in healthcare law and regulations, including those from CMS, the OIG, and other relevant agencies.
Professional Development: I regularly attend conferences, webinars, and workshops focusing on medical ethics and legal compliance to stay abreast of current best practices and recent legal developments.
Collaboration with Legal Counsel: I maintain close communication with legal counsel to discuss emerging issues and ensure our practices align with the latest regulations.
Internal Audits and Monitoring: I participate in and contribute to regular internal audits and compliance reviews to proactively identify potential compliance gaps.
Review of Policy and Procedure Manuals: I ensure all policy and procedure manuals are updated to reflect the most current regulations. This includes the review and update of our organization’s internal policies and procedures.
By utilizing these strategies, I ensure our work consistently meets the highest standards of ethical conduct and legal compliance.
Q 20. Describe your experience in developing and implementing compliance training programs.
I have extensive experience in designing and delivering compliance training programs, tailoring them to the specific needs of various healthcare settings and staff roles. My approach focuses on making training engaging, practical, and relevant.
I start by conducting a needs assessment to identify knowledge gaps and areas needing reinforcement. This involves reviewing existing documentation, conducting interviews with staff, and analyzing previous audit findings. Based on the assessment, I develop training materials, including presentations, case studies, interactive exercises, and quizzes, that are tailored to the specific regulatory requirements and the unique context of the organization.
For instance, when developing a training program on HIPAA compliance, I would incorporate interactive scenarios that simulate real-world situations, allowing participants to practice applying HIPAA principles in different contexts. The training would also include examples of real-world HIPAA violations and the consequences of non-compliance. Finally, I always ensure that the training program is regularly reviewed and updated to account for changes in legislation and best practices. Post-training assessments are also key to evaluating effectiveness and identifying areas requiring further attention.
Q 21. How do you stay updated on changes in healthcare regulations and ethical guidelines?
Staying current in the ever-changing landscape of healthcare regulations and ethical guidelines is crucial. I employ several strategies:
Professional Organizations: I am an active member of professional organizations such as the American Health Lawyers Association (AHLA) and similar groups. These organizations provide valuable resources, publications, and networking opportunities to stay informed about current issues and trends.
Government Websites and Publications: I regularly consult the websites of government agencies like CMS, OIG, and the Federal Register for official updates and announcements regarding regulatory changes.
Legal and Compliance Journals: I subscribe to and actively read leading journals in healthcare law and compliance to gain insights into recent court decisions, legal interpretations, and best practices.
Continuing Education: I actively participate in ongoing continuing education courses and professional development opportunities to ensure my knowledge remains up-to-date and relevant. This ensures that I stay informed about any changes to legislation or ethical guidelines.
Networking and Collaboration: I engage in regular networking with other compliance professionals to share information, best practices, and discuss emerging challenges in the field.
This multi-pronged approach ensures that I remain knowledgeable about the latest developments and can proactively address any potential compliance risks.
Q 22. Describe a time you had to make a difficult ethical decision in a healthcare setting.
One of the most challenging ethical dilemmas I faced involved a patient with advanced cancer who refused further treatment, despite a high likelihood of suffering significant pain and discomfort without it. His family strongly urged him to reconsider, believing that he was ‘giving up’ too easily. This created a conflict between respecting the patient’s autonomy (his right to make decisions about his own body and treatment) and the principle of beneficence (doing what is in his best interest, which, in their eyes, included continued treatment).
My approach involved several steps. First, I held separate discussions with the patient and his family, ensuring each felt heard and understood. I carefully explained the risks and benefits of continuing treatment, emphasizing that the decision ultimately rested with the patient. Second, I explored the patient’s reasons for refusing treatment, finding he had a strong sense of peace with his decision and prioritized quality of life over extending it at the cost of increased suffering. Finally, I facilitated open communication between the patient and his family, helping them to understand and, eventually, respect his wishes. The outcome involved a compromise where palliative care was prioritized to manage his pain and discomfort, ensuring a comfortable end-of-life experience.
Q 23. What are some common ethical dilemmas faced by healthcare professionals?
Healthcare professionals frequently encounter ethical dilemmas. These often revolve around competing principles and values. Some common examples include:
- End-of-life care: Balancing patient autonomy with beneficence in cases involving terminal illness and the use of life-sustaining treatments.
- Resource allocation: Making difficult decisions about the distribution of scarce medical resources, such as organ transplantation or ICU beds.
- Informed consent: Ensuring patients have the capacity and understanding to make informed decisions about their treatment, especially in complex medical situations.
- Confidentiality: Protecting patient privacy while fulfilling legal obligations to report suspected abuse or neglect.
- Truth-telling: Determining the appropriate level of disclosure to patients about their diagnosis and prognosis.
- Conflicts of interest: Managing situations where personal interests may compromise professional judgment or patient well-being.
Addressing these dilemmas requires careful consideration of ethical frameworks, relevant laws and regulations, and a commitment to patient-centered care.
Q 24. How do you assess risk in a healthcare compliance context?
Assessing risk in healthcare compliance is a systematic process aimed at identifying, analyzing, and mitigating potential violations of laws, regulations, and ethical standards. This involves a multi-step approach:
- Identify potential risks: This involves reviewing relevant laws and regulations (HIPAA, Stark Law, Anti-Kickback Statute, etc.), internal policies, and conducting risk assessments based on the organization’s specific activities and vulnerabilities.
- Analyze the likelihood and impact of risks: For each identified risk, determine the probability of it occurring and the potential consequences (financial penalties, reputational damage, patient harm). A risk matrix can be a valuable tool here.
- Develop mitigation strategies: Based on the risk analysis, implement strategies to reduce or eliminate the likelihood and impact of identified risks. This could involve training programs, improved documentation processes, strengthened internal controls, and enhanced auditing procedures.
- Monitor and evaluate: Regularly monitor the effectiveness of mitigation strategies and adapt them as needed. This requires ongoing assessment of the healthcare environment and relevant changes in laws and regulations.
For example, a risk assessment might reveal a high probability of a HIPAA violation due to inadequate staff training on data security. The mitigation strategy would be to implement mandatory HIPAA training for all staff and regular audits to ensure compliance.
Q 25. Explain the concept of beneficence and non-maleficence in medical ethics.
Beneficence and non-maleficence are two core principles in medical ethics. They are often presented together, although they represent distinct but complementary concepts.
Beneficence refers to the healthcare professional’s obligation to act in the best interests of the patient. This involves actively promoting the patient’s well-being, providing appropriate treatment, and taking positive steps to prevent harm. It’s about doing good.
Non-maleficence, on the other hand, emphasizes the duty to ‘do no harm’. This involves avoiding actions that could cause harm or injury, whether intentional or unintentional. It’s about preventing harm and minimizing risks.
In practice, these principles are often intertwined. For instance, a surgeon must weigh the potential benefits of an operation against the risks of complications (beneficence vs. non-maleficence). Finding the optimal balance between these principles often forms the crux of ethical decision-making in medicine.
Q 26. What are the ethical considerations surrounding organ donation and transplantation?
Organ donation and transplantation raise a number of significant ethical considerations:
- Consent: Ensuring that organ donation is truly voluntary and informed. The process must be transparent and free from coercion.
- Allocation: Developing equitable and fair systems for allocating scarce organs, given the high demand and limited supply. Criteria often involve medical urgency, waiting time, and tissue compatibility.
- Justice and equity: Addressing potential disparities in access to transplantation based on factors such as socioeconomic status, race, or geographic location.
- Commercialization: Preventing the exploitation of vulnerable individuals through the illegal buying and selling of organs.
- Confidentiality: Protecting the privacy of donors and recipients, respecting their wishes about disclosure of information.
Organ donation and transplantation are complex ethical issues that require careful consideration of competing values and interests. The aim is to balance the needs of potential recipients with the rights and wishes of donors and their families while maintaining ethical standards.
Q 27. Describe your understanding of patient rights and responsibilities.
Patient rights are fundamental entitlements that protect individuals during their healthcare journey. These include the right to:
- Informed consent: Receiving complete and understandable information about their diagnosis, treatment options, and potential risks and benefits before making decisions about their care.
- Privacy and confidentiality: Having their personal and medical information protected.
- Access to care: Receiving timely and appropriate medical care.
- Refusal of treatment: Making decisions about their own care, even if it means refusing treatment.
- Second opinion: Seeking advice from another healthcare provider.
Patient responsibilities, conversely, refer to the actions individuals should take to contribute to their own well-being and the effective functioning of the healthcare system. These include:
- Providing accurate information: Sharing relevant details about their medical history and current condition.
- Following treatment plans: Adhering to instructions and advice from healthcare professionals.
- Asking questions: Clarifying any doubts or uncertainties about their treatment.
- Respecting healthcare providers: Treating healthcare professionals with courtesy and consideration.
A balanced understanding of both rights and responsibilities is crucial for fostering positive patient-provider relationships and ensuring high-quality care.
Q 28. How do you balance patient confidentiality with the need to report suspected abuse or neglect?
Balancing patient confidentiality with the duty to report suspected abuse or neglect is a critical ethical and legal challenge. Patient confidentiality, protected by HIPAA and other regulations, is paramount. However, there are exceptions to this principle, particularly when there is a legal obligation to report suspected harm to others. This often involves a careful weighing of competing interests.
The steps involved generally include:
- Assessing the situation: Carefully evaluating the evidence to determine if there is reasonable suspicion of abuse or neglect. This requires a clear understanding of the signs and symptoms of various forms of abuse and neglect.
- Consulting with colleagues and supervisors: Discussing the situation with other healthcare professionals to get their input and perspective.
- Documenting thoroughly: Keeping detailed records of all observations, interactions, and decisions made.
- Reporting appropriately: Following established procedures for reporting suspected abuse or neglect to the appropriate authorities (e.g., child protective services, adult protective services, law enforcement). This often involves adhering to specific reporting laws and regulations.
The overriding principle is to act in the best interest of the vulnerable individual, even if it means breaching confidentiality. This is often a difficult decision, but the potential consequences of inaction (failure to report) can be far more severe.
Key Topics to Learn for Medical Ethics and Legal Compliance Interview
- Patient Autonomy & Informed Consent: Understanding the principles of patient autonomy, the elements of informed consent, and navigating situations where capacity is compromised.
- Confidentiality & Privacy: Applying HIPAA regulations and ethical considerations regarding patient confidentiality, including disclosure exceptions and data security.
- Beneficence & Non-Maleficence: Balancing the principles of doing good and avoiding harm in clinical decision-making, considering potential conflicts and ethical dilemmas.
- Justice & Fairness: Analyzing resource allocation, equitable access to care, and addressing disparities in healthcare delivery.
- Professional Boundaries & Relationships: Maintaining appropriate professional conduct, recognizing and addressing potential conflicts of interest, and navigating challenging interpersonal dynamics.
- End-of-Life Care & Advance Directives: Understanding legal and ethical frameworks surrounding end-of-life decisions, including advance directives, palliative care, and physician-assisted death (where applicable).
- Research Ethics: Applying ethical principles to research involving human subjects, including informed consent, risk assessment, and data privacy.
- Legal Frameworks: Familiarity with relevant laws and regulations impacting healthcare, such as HIPAA, state-specific regulations, and malpractice considerations.
- Case Studies & Ethical Decision-Making Frameworks: Applying ethical frameworks (e.g., principlism, casuistry) to analyze complex case studies and develop reasoned solutions.
- Reporting Mechanisms & Whistleblower Protection: Understanding procedures for reporting ethical violations and legal non-compliance, and the importance of whistleblower protection.
Next Steps
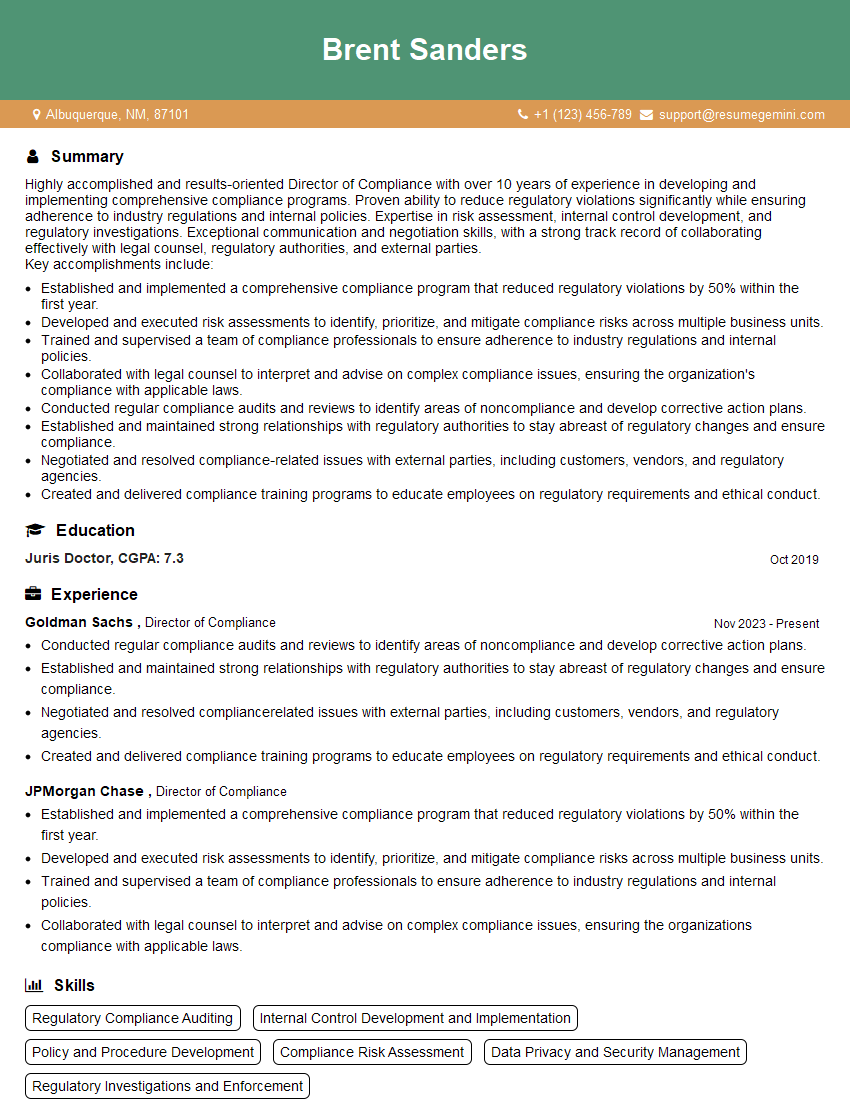
Mastering Medical Ethics and Legal Compliance is crucial for career advancement in healthcare. A strong understanding of these principles demonstrates professionalism, competence, and a commitment to patient well-being – qualities highly valued by employers. To significantly boost your job prospects, invest time in creating an ATS-friendly resume that effectively showcases your skills and experience. ResumeGemini is a trusted resource that can help you build a compelling and professional resume. We offer examples of resumes tailored to Medical Ethics and Legal Compliance to help you get started. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.