Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Medication Prescribing interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Medication Prescribing Interview
Q 1. Explain the process of choosing the most appropriate medication for a specific patient.
Choosing the right medication is a multifaceted process that prioritizes patient safety and efficacy. It’s not simply about the disease; it’s about the individual patient.
- Assessment: Thorough patient history, including current medications, allergies, comorbidities (other health conditions), and lifestyle factors (smoking, alcohol use, diet) is crucial. A physical exam helps identify any relevant clinical findings.
- Diagnosis: Accurate diagnosis of the condition is paramount. Misdiagnosis leads to ineffective or harmful treatment.
- Treatment Goals: Clearly defined goals, like blood pressure control or symptom relief, guide medication selection. These goals must align with the patient’s preferences and values.
- Medication Selection: Considering factors like efficacy, safety profile (side effects, drug interactions), cost, and ease of administration (oral, injection, topical) is crucial. Evidence-based guidelines and clinical practice guidelines often inform this step. For example, if treating hypertension, we might consider ACE inhibitors, ARBs, or diuretics, each with its own benefits and drawbacks depending on the patient’s overall health profile.
- Monitoring & Adjustment: Regular monitoring is necessary to assess the medication’s effectiveness and identify any adverse effects. Dose adjustments might be needed based on patient response and lab results. For instance, we may need to adjust the dosage of a blood thinner based on regular blood tests.
Example: A patient with hypertension and kidney disease requires careful medication selection. An ACE inhibitor might be avoided due to its potential to worsen kidney function, leading to the selection of an ARB or another suitable alternative.
Q 2. Describe your experience with medication reconciliation.
Medication reconciliation is the process of comparing a patient’s medication list with what they’re currently taking. It’s essential to prevent medication discrepancies, which are a major source of medication errors. My experience involves actively participating in this process at various transition points in care, such as hospital admission, discharge, and transfer between care settings.
- Hospital Admissions: I meticulously compare the patient’s home medication list with their current medications to identify any omissions or discrepancies. This often involves verifying information with the patient, family, or their pharmacy.
- Discharge Planning: I ensure the discharge medications align with the patient’s needs and address any changes in their condition. Clear instructions are provided to the patient and their caregivers about dosages, timing, and potential side effects.
- Transitions of Care: When a patient moves between care settings, reconciliation is crucial to ensure continuity of care and avoid interruptions in treatment. I’ve successfully used standardized tools and checklists to streamline this process.
Medication reconciliation helps prevent adverse drug events, reduces hospital readmissions, and improves patient safety. It requires excellent communication and teamwork with other healthcare professionals.
Q 3. How do you handle medication errors?
Handling medication errors requires a systematic approach prioritizing patient safety and learning from mistakes. It’s never about blaming; it’s about improving the system.
- Immediate Action: Assess the patient’s condition immediately. If necessary, provide appropriate supportive care.
- Documentation: Thoroughly document the error, including the type of error, the patient’s response, and any interventions taken. This documentation is crucial for analysis and prevention.
- Reporting: Report the error to the appropriate authorities (e.g., hospital incident reporting system). This allows for a formal review and potential system improvements.
- Root Cause Analysis: A thorough investigation is conducted to determine the underlying causes of the error. This may involve interviewing staff, reviewing procedures, and examining medication administration processes. This is essential to prevent recurrence.
- Corrective Actions: Based on the root cause analysis, implement corrective actions to address the identified weaknesses. This might include changes in procedures, training for staff, or improvements to the medication administration system.
Example: If a wrong dose is administered, immediate assessment is crucial. Following reporting and root cause analysis, corrective action might involve implementing double-checking mechanisms for medication dispensing and administering, reinforcing training and education for nurses on medication calculation.
Q 4. What are the key considerations when prescribing medications to elderly patients?
Prescribing for elderly patients requires extra caution due to age-related physiological changes that affect drug absorption, metabolism, and excretion (pharmacokinetics). Polypharmacy (taking multiple medications) is also common, increasing the risk of drug interactions.
- Pharmacokinetics: Reduced renal and hepatic function often leads to slower drug clearance, increasing the risk of drug accumulation and toxicity. Lower doses or less frequent dosing might be necessary.
- Pharmacodynamics: Increased sensitivity to certain drugs can lead to amplified effects even with standard doses. For example, elderly patients may be more susceptible to the sedative effects of certain medications.
- Polypharmacy: Carefully review all medications to identify potential interactions and avoid unnecessary prescriptions. Consider deprescribing (stopping medications that are no longer needed or beneficial).
- Comorbidities: The presence of multiple chronic conditions often complicates medication management. Prescribing decisions need to consider the impact on other existing conditions.
- Cognitive Function: Consider the patient’s cognitive abilities when providing medication instructions. Simplify instructions and provide written and visual aids, if necessary.
- Patient Preferences: Always engage the patient and their family in shared decision-making to ensure adherence and acceptance of the prescribed regimen.
Example: An elderly patient with both hypertension and heart failure requires careful consideration of drug choices to avoid worsening kidney function. A lower dose of medication or a different class of drug might be necessary.
Q 5. How do you assess a patient’s adherence to their medication regimen?
Assessing medication adherence involves a multifaceted approach combining various methods to gain a comprehensive understanding of a patient’s medication-taking behavior.
- Patient Self-Report: Asking the patient directly about their medication-taking habits is a starting point. However, self-reports can be unreliable.
- Pill Counts: Counting the remaining pills in the prescription bottle can provide a quantitative measure of adherence, but it doesn’t fully capture the complexities of medication-taking behavior.
- Medication Adherence Questionnaires: Standardized questionnaires help assess self-reported adherence patterns. These tools have limitations, as patients may not always be accurate in their self-reporting.
- Electronic Monitoring: Smart pill dispensers and wearable sensors can objectively track medication intake. These technologies offer a more accurate assessment of adherence but can be costly and may raise privacy concerns.
- Biochemical Markers: For certain medications, blood or urine tests can confirm drug levels in the body, providing evidence of adherence, though the cost and invasiveness need to be considered.
- Clinical Outcomes: Assessing the clinical response to the medication (e.g., blood pressure control) provides an indirect measure of adherence. Good clinical outcomes suggest good adherence, while poor outcomes may suggest poor adherence. But this is not foolproof, as several other factors can affect clinical response.
A combination of these methods provides a more holistic view. It’s crucial to discuss barriers to adherence and address them through patient education, simplifying medication regimens, or using medication assistance programs.
Q 6. Explain your understanding of pharmacokinetics and pharmacodynamics.
Pharmacokinetics describes what the body does to a drug. It encompasses the processes of absorption (how the drug enters the bloodstream), distribution (how the drug reaches its target site), metabolism (how the drug is broken down), and excretion (how the drug is eliminated from the body). Think of it as the drug’s journey through the body.
Pharmacodynamics describes what the drug does to the body. It focuses on the drug’s mechanism of action, its effects on the body (both intended and unintended), and the relationship between drug concentration and its effect. Think of it as the drug’s impact.
Understanding both is crucial for safe and effective prescribing. For example, a drug with poor absorption might require a higher dose to achieve the desired effect. Conversely, a drug with strong pharmacodynamic effects might require a lower dose to avoid adverse events.
Q 7. Describe your knowledge of common drug interactions.
Knowledge of common drug interactions is essential to prevent adverse events. Interactions can occur between two or more drugs, or between drugs and other substances (e.g., food, alcohol).
- Additive effects: Two drugs with similar effects taken together increase the overall effect. For example, taking two sedatives together might result in excessive drowsiness.
- Synergistic effects: The combined effect of two drugs is greater than the sum of their individual effects. This can be beneficial (e.g., using combination therapy for HIV) or harmful (e.g., combining two drugs that both cause QT prolongation).
- Antagonistic effects: One drug reduces or blocks the effect of another. This can be intentional (e.g., using naloxone to reverse opioid overdose) or unintentional (e.g., one drug interfering with the absorption of another).
- Metabolic interactions: One drug alters the metabolism of another, leading to increased or decreased levels of the second drug. This can be a significant concern, particularly with drugs metabolized by the liver (CYP450 enzymes).
Example: Grapefruit juice inhibits certain enzymes in the liver, leading to increased blood levels of certain medications, potentially causing toxicity. Similarly, combining a non-steroidal anti-inflammatory drug (NSAID) with a blood thinner can increase the risk of bleeding.
Resources like drug interaction databases (e.g., Micromedex, Lexicomp) are invaluable tools for checking potential drug interactions.
Q 8. How do you counsel patients about their medications?
Patient medication counseling is a crucial part of safe and effective medication use. It’s not just about handing over a prescription; it’s about empowering the patient to be an active participant in their healthcare. My approach involves a structured conversation covering several key aspects.
- Medication Name and Purpose: Clearly explaining the medication’s name, its intended use, and how it will help manage their condition. For example, if prescribing Metformin for Type 2 diabetes, I’ll explain that it helps the body use insulin more effectively.
- Dosage and Administration: Providing precise instructions on the dose, frequency, and route of administration. I’ll use visuals like pill organizers or written instructions to reinforce this, especially for patients with multiple medications.
- Expected Benefits and Potential Side Effects: Discussing what patients can expect to experience (e.g., improved blood sugar control with Metformin) and potential side effects (e.g., gastrointestinal upset). I always emphasize that side effects aren’t necessarily inevitable and that many are mild and transient.
- Medication Interactions: Inquiring about other medications, supplements, or herbal remedies they are taking to identify potential interactions. This includes over-the-counter drugs and even common foods that could impact efficacy or safety.
- Missed Dose Instructions: Providing clear guidance on what to do if a dose is missed, emphasizing that it’s crucial to follow the prescribed schedule. This helps to avoid complications caused by inconsistent medication intake.
- Storage and Disposal: Explaining proper medication storage (e.g., away from heat and moisture) and safe disposal methods to prevent accidental ingestion or environmental contamination.
- Follow-up and Monitoring: Scheduling follow-up appointments to monitor effectiveness and address any concerns or side effects. I encourage patients to contact my office at any time with questions.
I tailor my communication style to each patient, adjusting my language and using visual aids when necessary to ensure understanding. For instance, I use simpler language for patients with lower health literacy and provide written materials in their preferred language.
Q 9. What are the legal and ethical considerations surrounding medication prescribing?
Legal and ethical considerations in medication prescribing are paramount. They form the bedrock of responsible medical practice. These considerations encompass several key areas:
- Licensure and Scope of Practice: Prescribing medications is restricted to licensed healthcare professionals within their legally defined scope of practice. This means I must only prescribe medications within my area of expertise and according to relevant regulations.
- Informed Consent: Patients have the right to be fully informed about their treatment options, including the benefits, risks, and alternatives to medication. This includes discussing potential side effects and the patient’s understanding of their condition.
- Confidentiality: All patient information, including their medication history and prescriptions, must be kept strictly confidential in accordance with HIPAA regulations (and equivalent privacy laws where applicable).
- Controlled Substances: Prescribing controlled substances requires adherence to stringent regulations, including proper documentation, patient monitoring, and reporting to regulatory agencies. This often involves regular checks for medication misuse or abuse.
- Appropriate Indications: Prescribing medications must be evidence-based and only for approved indications. This prevents inappropriate use and minimizes potential harm. I always thoroughly review a patient’s medical history and relevant studies before prescribing.
- Avoiding Conflicts of Interest: Maintaining objectivity and transparency in prescribing decisions is crucial. This means avoiding conflicts of interest such as accepting gifts or incentives from pharmaceutical companies.
- Documentation: Meticulous documentation of all prescribing decisions, including the rationale, is essential for legal protection and quality of care. The electronic health record plays a vital role in this process.
A violation of these legal and ethical guidelines can have serious consequences, including disciplinary actions, loss of license, and legal liabilities.
Q 10. How do you stay updated on the latest guidelines and research in medication prescribing?
Staying abreast of the latest guidelines and research is a continuous process. I employ several strategies to ensure my prescribing practices remain up-to-date and evidence-based:
- Subscription to Professional Journals: I regularly subscribe to and read reputable medical journals like the New England Journal of Medicine, JAMA, and others relevant to my specialty.
- Participation in Continuing Medical Education (CME): Attending conferences, workshops, and online courses to earn CME credits is essential to maintain my knowledge and expertise. Many organizations offer specific CME in medication prescribing best practices.
- Membership in Professional Organizations: Being part of professional organizations keeps me informed about relevant updates and offers networking opportunities with colleagues.
- Monitoring Regulatory Updates: I regularly check for updates from regulatory agencies such as the FDA on drug approvals, warnings, and guidelines.
- Utilizing Clinical Practice Guidelines: I actively utilize evidence-based clinical practice guidelines published by organizations like the American College of Cardiology or the American Diabetes Association to inform my prescribing decisions.
- Engaging in Peer Review: Discussing cases and treatment strategies with colleagues through peer review helps to broaden perspectives and stay informed about new research.
Staying informed isn’t just a requirement; it’s a commitment to providing the best possible patient care. The rapidly evolving field of medicine demands continuous learning to ensure optimal treatment.
Q 11. Describe your experience with controlled substances prescribing.
Prescribing controlled substances requires a high level of vigilance and adherence to strict legal and ethical guidelines. My experience involves a multifaceted approach:
- Careful Patient Assessment: Before prescribing, I conduct a thorough assessment to determine the legitimacy of the need for controlled substances, ruling out potential misuse or addiction.
- Documentation: Meticulous documentation of all prescribing actions, including the patient’s history, rationale for prescription, and ongoing monitoring plans, is critical. This documentation should be readily accessible for audit.
- Regular Monitoring: I schedule frequent follow-up appointments to monitor the patient’s response to the medication and check for signs of misuse or abuse. This might include regular urine drug screenings or pain assessments.
- Prescription Drug Monitoring Programs (PDMP): I utilize PDMP databases to track the patient’s prescription history for controlled substances across multiple providers, helping to identify any potential red flags.
- Patient Education: Comprehensive patient education on the risks associated with misuse and addiction is paramount, emphasizing the importance of adherence to the prescribed dosage and schedule.
- Collaboration with Specialists: When appropriate, I collaborate with pain management specialists or addiction specialists to ensure appropriate management and reduce the risk of misuse.
- Adherence to State and Federal Regulations: I strictly comply with all state and federal regulations governing the prescribing of controlled substances. This includes understanding and adhering to DEA requirements.
My goal is to provide pain relief or address other legitimate medical needs while minimizing the risks associated with controlled substances, always prioritizing patient safety and well-being.
Q 12. How do you address patient concerns about medication side effects?
Addressing patient concerns about medication side effects is a critical aspect of patient care. My approach involves active listening, empathy, and a collaborative problem-solving strategy:
- Active Listening: I carefully listen to the patient’s concerns, validating their feelings and acknowledging the impact of side effects on their daily lives. This creates a safe space for open communication.
- Assessment and Investigation: I thoroughly assess the reported side effects, determining their severity, frequency, and potential relationship to the medication. This may involve reviewing the patient’s medication list for potential interactions.
- Education and Reassurance: I provide education on the expected side effects of the medication, explaining that many side effects are mild and temporary. If the side effects are expected and manageable, I offer strategies for coping with them (e.g., dietary changes for nausea).
- Dose Adjustment or Medication Change: If the side effects are severe or intolerable, I consider adjusting the dosage or exploring alternative medications. The decision depends on a careful balancing of the benefits and risks.
- Referral to Specialists: In cases of complex or severe side effects, I may refer the patient to a specialist (e.g., gastroenterologist for severe nausea) for further evaluation and management.
- Monitoring and Follow-up: I closely monitor the patient’s response to the medication adjustments or alternative therapies, scheduling frequent follow-up appointments to address any ongoing concerns.
Open communication and proactive problem-solving are essential for ensuring the patient’s comfort and adherence to the prescribed medication regimen.
Q 13. What is your approach to prescribing medications for patients with multiple comorbidities?
Prescribing for patients with multiple comorbidities requires a careful and systematic approach to minimize potential drug interactions and adverse effects. My approach involves:
- Comprehensive Medication Review: I conduct a thorough review of all medications, including over-the-counter drugs and supplements, to identify potential interactions. I utilize resources like drug interaction databases to assess compatibility.
- Prioritization of Treatment Goals: I prioritize treatment goals based on the severity and urgency of each condition. For example, managing blood pressure might be prioritized over managing mild arthritis pain in some situations.
- Stepwise Approach to Medication Selection: I start with the least potent medication with the fewest potential side effects whenever possible, gradually increasing the intensity or adding other medications as needed.
- Monitoring for Drug Interactions: I closely monitor the patient for signs of drug interactions or adverse events. This includes regular blood tests, ECGs, or other diagnostic tests depending on the specific medications and conditions.
- Patient Education and Shared Decision-Making: I educate the patient about each medication, explaining potential side effects and risks, to empower them to actively participate in their treatment decisions.
- Collaboration with Specialists: I collaborate with other specialists when necessary to ensure coordinated care and reduce the risk of medication-related problems. For example, a cardiologist’s input may be crucial if several medications impact cardiac function.
- Regular Follow-up: Frequent follow-up appointments are crucial to monitor the patient’s response to medications, assess for any new symptoms or side effects, and make adjustments as needed.
Managing patients with multiple comorbidities requires a comprehensive and individualized approach, placing a high value on collaboration and patient engagement.
Q 14. How do you utilize electronic health records (EHRs) in medication prescribing?
Electronic Health Records (EHRs) are indispensable tools in medication prescribing, significantly enhancing safety, efficiency, and coordination of care. My utilization of EHRs includes:
- Medication Reconciliation: EHRs facilitate medication reconciliation, comparing the patient’s current medication list with their past medication history and identifying potential discrepancies or omissions. This prevents errors and ensures accurate prescribing.
- Drug Interaction Checking: EHRs have built-in drug interaction checkers that alert me to potential interactions between different medications, reducing the risk of adverse events.
- Allergy and Contraindication Checks: EHRs provide quick access to the patient’s allergy and contraindication history, preventing prescription of harmful medications.
- Decision Support Systems: Many EHRs incorporate decision support systems that offer guidelines and recommendations for medication selection based on evidence-based medicine.
- Electronic Prescribing (e-Prescribing): E-prescribing minimizes the risk of errors associated with handwritten prescriptions and improves the communication of prescriptions to pharmacies, often in real-time.
- Patient Medication Lists: EHRs provide readily accessible medication lists for patients, improving their understanding of their medication regimen and enhancing adherence.
- Reporting and Monitoring: EHRs assist in tracking medication effectiveness and adverse events, allowing for better monitoring and adjustments to treatment plans.
The use of EHRs in medication prescribing streamlines workflows, reduces errors, and ultimately improves patient safety and treatment outcomes.
Q 15. Explain your understanding of different medication administration routes.
Medication administration routes refer to the different ways a drug can be delivered into a patient’s body. The choice of route depends on various factors, including the drug’s properties, the patient’s condition, and the desired speed of action.
- Oral (PO): This is the most common route, involving swallowing medication in pill, capsule, liquid, or tablet form. It’s convenient but has the slowest onset of action due to absorption in the gastrointestinal tract. For example, taking a paracetamol tablet for headache relief.
- Sublingual (SL): Medication is placed under the tongue where it dissolves and is rapidly absorbed into the bloodstream. This route is useful for medications that are broken down by stomach acid, like nitroglycerin for angina.
- Buccal: Similar to sublingual, but the medication is placed between the cheek and gum.
- Intravenous (IV): The drug is directly injected into a vein, providing the fastest and most reliable absorption. It’s ideal for emergencies or when rapid drug action is crucial, such as administering antibiotics for sepsis.
- Intramuscular (IM): Injection into a muscle, allowing for slower, sustained release of the medication. Flu vaccines are commonly administered intramuscularly.
- Subcutaneous (SC): Injection into the fatty layer beneath the skin. Insulin injections are a typical example of this route.
- Topical: Applying medication directly to the skin or mucous membranes. Creams, ointments, and lotions are examples. This route is used for localized treatment.
- Transdermal: Medication is absorbed through the skin using patches. Nicotine patches for smoking cessation are a common example of transdermal administration.
- Inhalation: Drugs are inhaled into the lungs via an inhaler or nebulizer. Asthma medications are often administered this way.
- Rectal: Medication is administered as a suppository or enema. This route is useful when oral administration is not feasible, such as in cases of nausea or vomiting.
Choosing the right route is critical to ensure both efficacy and safety of the medication. Each route has its advantages and disadvantages regarding absorption rate, convenience, and potential side effects.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage polypharmacy in your patients?
Polypharmacy, the concurrent use of multiple medications, is a significant concern, particularly among elderly patients. Managing it requires a systematic approach:
- Comprehensive Medication Review (CMR): I conduct a thorough review of all medications a patient is taking, including over-the-counter drugs and supplements. This helps identify potential drug interactions, duplications, and inappropriate prescriptions.
- Deprescribing: Where appropriate, I work with the patient to gradually discontinue medications that are no longer necessary or beneficial, reducing the overall medication burden. This often involves close monitoring for withdrawal symptoms and alternative management strategies.
- Prioritization and Optimization: I prioritize essential medications and adjust dosages or schedules as needed to minimize adverse effects and improve adherence. This might involve using simpler medication regimens to improve patient compliance.
- Patient Education: Thorough patient education is crucial. I explain the purpose, dosage, potential side effects, and interactions of each medication clearly and concisely. I provide written materials and encourage questions.
- Regular Follow-up: I schedule regular follow-up appointments to monitor for any adverse events, assess the effectiveness of the medications, and make necessary adjustments. This allows for proactive management and detection of any issues.
For example, I recently worked with a 78-year-old patient taking 12 different medications. Through a CMR, I identified that three were redundant and two were contributing to adverse effects. After careful deprescribing and dosage adjustments, we reduced the number to seven medications with significantly improved patient outcomes and reduced risk of adverse drug events.
Q 17. Describe your approach to prescribing medications for pregnant or breastfeeding women.
Prescribing for pregnant or breastfeeding women requires extra caution due to the potential impact on the fetus or infant. My approach involves:
- Minimizing Medication Use: I prioritize non-pharmacological interventions whenever possible. Lifestyle changes, physical therapy, or other conservative measures might be sufficient.
- Selecting Safe Medications: If medication is necessary, I select drugs with a well-established safety profile during pregnancy and lactation. I consult resources like the LactMed database and relevant guidelines to ensure the safest possible option.
- Lowest Effective Dose: I prescribe the lowest effective dose for the shortest duration necessary to achieve the desired therapeutic effect. This minimizes exposure to both mother and child.
- Close Monitoring: I closely monitor both the mother and the baby (if breastfeeding) for any adverse effects, adjusting the medication or management strategy as needed. Regular checkups are crucial.
- Patient Education: I provide thorough education on the risks and benefits of the medication, addressing any concerns or questions the mother may have. I also counsel on breastfeeding if applicable, considering the medication’s potential impact on milk production and infant health.
For instance, when treating a pregnant woman with hypertension, I would opt for medications categorized as pregnancy category A or B, and carefully monitor blood pressure and fetal development throughout the pregnancy.
Q 18. How do you identify and manage potential drug allergies?
Identifying and managing potential drug allergies is paramount for patient safety. My approach involves:
- Thorough History Taking: I meticulously document the patient’s medication history, including previous allergic reactions. I use open-ended questions to elicit detailed descriptions of the reaction (rash, swelling, difficulty breathing, etc.).
- Allergy Verification: I verify reported allergies with the patient’s medical records. Sometimes, what a patient perceives as an allergy may be a side effect or an adverse drug reaction.
- Accurate Documentation: I clearly document all confirmed allergies in the patient’s electronic medical record (EMR) using standardized terminology, ensuring easy retrieval and preventing future errors. This often includes the medication causing the reaction and the type of reaction experienced.
- Alternative Medications: When a patient has a known allergy to a medication, I select an alternative medication from a different class to avoid any cross-reactivity or similar adverse reactions.
- Allergy Testing (When Necessary): In ambiguous cases, I might consider allergy testing to confirm or refute a suspected allergy before prescribing alternative medications.
For example, if a patient reports a penicillin allergy, I thoroughly investigate the nature of the reaction. If it was a mild rash, we may consider prescribing a different beta-lactam antibiotic after careful assessment. However, if it involved anaphylaxis, we would strictly avoid all penicillin-type antibiotics and opt for a completely different class of antibiotic.
Q 19. Explain your experience with using clinical decision support systems (CDSS) for medication prescribing.
Clinical Decision Support Systems (CDSS) have become invaluable tools in medication prescribing. My experience with CDSS has been overwhelmingly positive. These systems provide:
- Drug Interaction Checks: CDSS flags potential drug interactions, alerting me to possible adverse effects before prescribing a medication. This helps prevent potentially harmful combinations.
- Dosage Alerts: CDSS checks for appropriate dosing based on patient characteristics (age, weight, renal function) and flags potential dosing errors or contradictions.
- Allergy Checks: The system verifies patient allergies against the medication being prescribed, preventing the prescription of potentially dangerous medications.
- Contraindication Checks: CDSS identifies potential contraindications based on patient medical history, reducing the risk of prescribing inappropriate medications.
- Treatment Guidelines: Many CDSS incorporate evidence-based guidelines and treatment protocols, supporting informed decision-making.
For example, when prescribing a new medication, the CDSS may alert me to a potential interaction with another medication the patient is currently taking, prompting me to review the patient’s profile and make necessary adjustments to the treatment plan to ensure the patient’s safety.
Q 20. How do you incorporate patient preferences into medication selection?
Incorporating patient preferences is essential for medication adherence and overall treatment success. I actively engage patients in shared decision-making:
- Open Communication: I initiate open dialogue about treatment options, discussing potential benefits, risks, and side effects of each. This includes discussing factors like dosage forms (pills, liquids, etc.) and administration frequency.
- Understanding Patient Needs: I actively listen to the patient’s concerns, preferences, and lifestyle factors to tailor the treatment plan accordingly. For example, a patient with a busy schedule might prefer a once-daily medication.
- Shared Decision-Making: I empower patients to participate in the decision-making process, providing information to support their informed choices. This can include comparing different medications side-by-side.
- Addressing Concerns: I address patient concerns and misconceptions about medications transparently and constructively. This helps build trust and facilitates medication adherence.
- Follow-up and Adjustment: I follow up with patients to assess their experience with the selected medication and make necessary adjustments based on their feedback and observed outcomes.
For instance, a patient may prefer a medication in liquid form because of swallowing difficulties. Understanding this preference allows me to prescribe an appropriate formulation rather than solely relying on the standard tablet form.
Q 21. Describe your understanding of the principles of rational polypharmacy.
Rational polypharmacy focuses on using multiple medications effectively and safely, avoiding unnecessary or harmful combinations. The principles include:
- Clinical Justification: Each medication should have a clear indication and clinical justification for its use. There should be a demonstrable benefit from each individual medication.
- Minimizing Interactions: Careful assessment is crucial to minimize potential drug interactions. Monitoring for both direct and indirect interactions is necessary.
- Dose Optimization: Medications should be prescribed at the lowest effective dose for the shortest duration needed to achieve therapeutic goals.
- Regular Review: The medication regimen must be regularly reviewed to identify and address any issues that may arise and ensure continued efficacy.
- Patient-Centered Approach: The patient’s preferences and values should be considered when designing a medication plan. Shared decision making is a key component of this principle.
- Medication Reconciliation: Every interaction with the patient involves a review of all medications currently taken to identify duplicates, potential interactions, and identify opportunities for deprescribing.
In essence, rational polypharmacy aims to provide the best possible therapeutic outcomes while minimizing the risks associated with taking multiple medications. It requires a proactive, patient-centered approach, and ongoing monitoring.
Q 22. How do you monitor the effectiveness and safety of prescribed medications?
Monitoring medication effectiveness and safety is crucial for optimal patient outcomes. It involves a multi-faceted approach combining objective clinical data with subjective patient reporting.
- Objective Measures: Regular follow-up appointments are essential. We monitor lab results (e.g., blood tests to check for therapeutic drug levels or organ function), vital signs (blood pressure, heart rate), and physical examinations to assess the medication’s impact. For example, if prescribing blood pressure medication, we’d track blood pressure readings at each visit. Imaging studies (like X-rays or ultrasounds) may also be necessary depending on the medication and the condition being treated.
- Subjective Reporting: Open communication with patients is paramount. We actively encourage them to report any side effects, no matter how minor they seem. A simple question like, “How are you feeling since starting this medication?” can uncover important information. We use standardized questionnaires to assess symptom severity, quality of life, and patient satisfaction.
- Adverse Drug Reaction (ADR) Surveillance: We maintain awareness of known ADRs associated with the prescribed medication. Resources like the FDA’s MedWatch program provide valuable updates on reported side effects. If a suspected ADR occurs, we carefully evaluate its severity and take appropriate action, potentially discontinuing the medication or adjusting the dosage.
Imagine a patient taking a new blood thinner. We’d monitor their INR (International Normalized Ratio) regularly to ensure it’s within the therapeutic range. If the INR is too high, we risk bleeding; if too low, the medication isn’t effective. Close monitoring allows us to adjust the dosage to achieve the best balance between efficacy and safety.
Q 23. Explain your knowledge of medication reconciliation processes within healthcare transitions.
Medication reconciliation is the process of comparing a patient’s medication list with what they are currently taking to identify discrepancies. This is vitally important during healthcare transitions, such as hospital admission, discharge, or transfer between facilities. Inconsistencies can lead to medication errors, adverse drug events, and poor patient outcomes.
My approach involves a systematic review of all medications—prescription, over-the-counter, and herbal supplements—obtained from the patient, their family, or their previous healthcare providers. We utilize various tools, including electronic health records (EHRs) and medication reconciliation software, to facilitate this process. The goal is to create an accurate, up-to-date medication list that reflects the patient’s current needs and minimizes the risk of errors.
For example, during hospital discharge, we carefully compare the patient’s home medication list with the medications administered during their hospital stay. This helps avoid duplications, omissions, or dosage changes that could harm the patient upon returning home. We provide clear instructions and follow up to ensure the patient understands their medication regimen and potential side effects. We also involve the patient’s family or caregiver as appropriate to ensure smooth medication management.
Q 24. How do you handle situations where a patient refuses a prescribed medication?
When a patient refuses a prescribed medication, my approach centers on understanding the reasons behind their refusal. It’s rarely a simple ‘no.’ Often, it stems from concerns about side effects, cost, or a lack of understanding about the medication’s benefits.
- Active Listening and Empathy: I start by actively listening to the patient’s concerns without judgment. Creating a safe space for open communication is key. Empathy and understanding are crucial here.
- Education and Clarification: I then clarify the medication’s purpose, its potential benefits and risks, and address any misconceptions. I use clear, simple language, avoiding medical jargon whenever possible. I also answer all their questions honestly and thoroughly.
- Exploring Alternatives: Depending on the situation, we might explore alternative treatment options, including non-pharmacological approaches if appropriate. It’s important to involve the patient in shared decision-making.
- Documentation: I meticulously document the patient’s refusal, the reasons behind it, and the steps taken to address their concerns. This is vital for legal and medical record-keeping.
For example, if a patient refuses a statin due to concerns about muscle pain, I carefully explain the risks and benefits, discuss potential strategies to mitigate muscle pain (e.g., starting with a low dose), and explore alternative approaches if necessary. But, ultimately, respecting patient autonomy is paramount. If after full discussion and education, the patient maintains their refusal, we respect their decision, while noting potential risks involved.
Q 25. Describe your experience with managing adverse drug reactions.
Managing adverse drug reactions (ADRs) requires prompt recognition, appropriate intervention, and careful documentation. The first step involves careful assessment to determine if the observed symptoms are indeed caused by the medication. This may involve reviewing the patient’s history, examining the medication’s known side effects, and considering other potential causes.
- Severity Assessment: ADRs range from mild (e.g., rash, nausea) to severe (e.g., anaphylaxis, organ damage). Severity dictates the urgency of intervention. Mild ADRs might require monitoring and adjustments to medication. Severe ADRs require immediate action, often involving medication discontinuation, supportive care, and potential hospitalization.
- Intervention: This might include discontinuing the medication, adjusting the dosage, or administering supportive treatments to alleviate symptoms. In some cases, we may need to refer the patient to a specialist, such as an allergist or nephrologist.
- Reporting: Suspected ADRs must be reported to relevant authorities, such as the FDA’s MedWatch program. This is crucial for monitoring the safety of medications and protecting other patients.
- Documentation: Detailed documentation, including the symptoms, the timeline, the intervention taken, and the patient’s response, is essential for future reference and for tracking the ADR’s impact.
For example, if a patient develops a severe allergic reaction (anaphylaxis) after taking a new antibiotic, we would immediately administer epinephrine, provide respiratory support, and transport the patient to the emergency room. The medication would be discontinued, and the event would be thoroughly documented and reported to the FDA.
Q 26. How do you address non-adherence to medication regimens?
Non-adherence to medication regimens is a significant challenge. It’s crucial to understand the reasons behind non-adherence, which can range from forgetfulness or lack of understanding to cost concerns or side effects.
- Patient Education: I emphasize the importance of adhering to the prescribed regimen and provide clear, concise instructions in a language the patient understands. Using medication organizers, pill boxes, or mobile apps can also be helpful.
- Addressing Barriers: If cost is a concern, I explore options like patient assistance programs or generic alternatives. If side effects are problematic, I may suggest strategies to mitigate them or consider adjusting the dosage or changing medications.
- Building a Therapeutic Relationship: Establishing a strong patient-provider relationship fosters trust and enhances adherence. Regular follow-up appointments provide opportunities for monitoring medication effectiveness, addressing concerns, and reinforcing the importance of adherence.
- Behavioral Interventions: In some cases, behavioral interventions, such as goal-setting or motivational interviewing, can be effective in improving adherence.
For example, if a patient forgets to take their medication regularly, I might suggest using a daily pill organizer or setting reminders on their phone. If side effects are interfering with adherence, I may adjust the dosage or explore alternative medication options.
Q 27. What is your approach to choosing between brand-name and generic medications?
The choice between brand-name and generic medications is often a matter of cost and efficacy. Generic medications contain the same active ingredient as brand-name drugs, but they are typically cheaper because they don’t incur the costs associated with marketing and brand development.
In most cases, generic medications are just as effective and safe as brand-name drugs. The FDA requires generic medications to meet the same rigorous standards as brand-name drugs, ensuring that they are bioequivalent, meaning they have the same active ingredient, strength, and dosage form, and they are absorbed and used by the body in the same way.
However, there are some exceptions. In rare instances, a patient might experience better results with one formulation over another due to individual differences in metabolism or tolerance. If a patient has had a positive experience with a specific brand-name drug, and cost is not a major issue, we may consider sticking with it. But, generally, generic equivalents provide the same therapeutic benefit at a significantly reduced price, making them the preferred choice unless there’s a specific medical reason to opt for the brand-name medication.
Key Topics to Learn for Medication Prescribing Interview
- Pharmacokinetics & Pharmacodynamics: Understanding how drugs are absorbed, distributed, metabolized, and excreted, and their effects on the body. Consider practical application examples like calculating dosages based on patient factors.
- Medication Interactions: Analyzing potential drug-drug, drug-food, and drug-disease interactions. Practice identifying and mitigating potential adverse effects.
- Legal & Ethical Considerations: Reviewing relevant legislation and professional guidelines governing medication prescribing, including informed consent and patient safety. Explore case studies involving ethical dilemmas.
- Patient Assessment & Monitoring: Mastering techniques for comprehensive patient history taking, physical examination relevant to medication management, and ongoing monitoring for treatment efficacy and adverse reactions. Focus on practical application through scenarios.
- Common Medications & Therapeutic Classes: Gaining a solid understanding of the mechanisms of action, indications, contraindications, and side effects of commonly prescribed medications across various therapeutic classes. Consider comparing and contrasting similar drugs.
- Electronic Health Records (EHR) Systems: Familiarizing yourself with the use of EHR systems for medication ordering, documentation, and monitoring. Practice navigating a sample EHR interface (if possible).
- Dosage Calculations & Conversions: Mastering accurate dosage calculations and conversions to ensure safe and effective medication administration. Practice different calculation methods and scenarios.
Next Steps
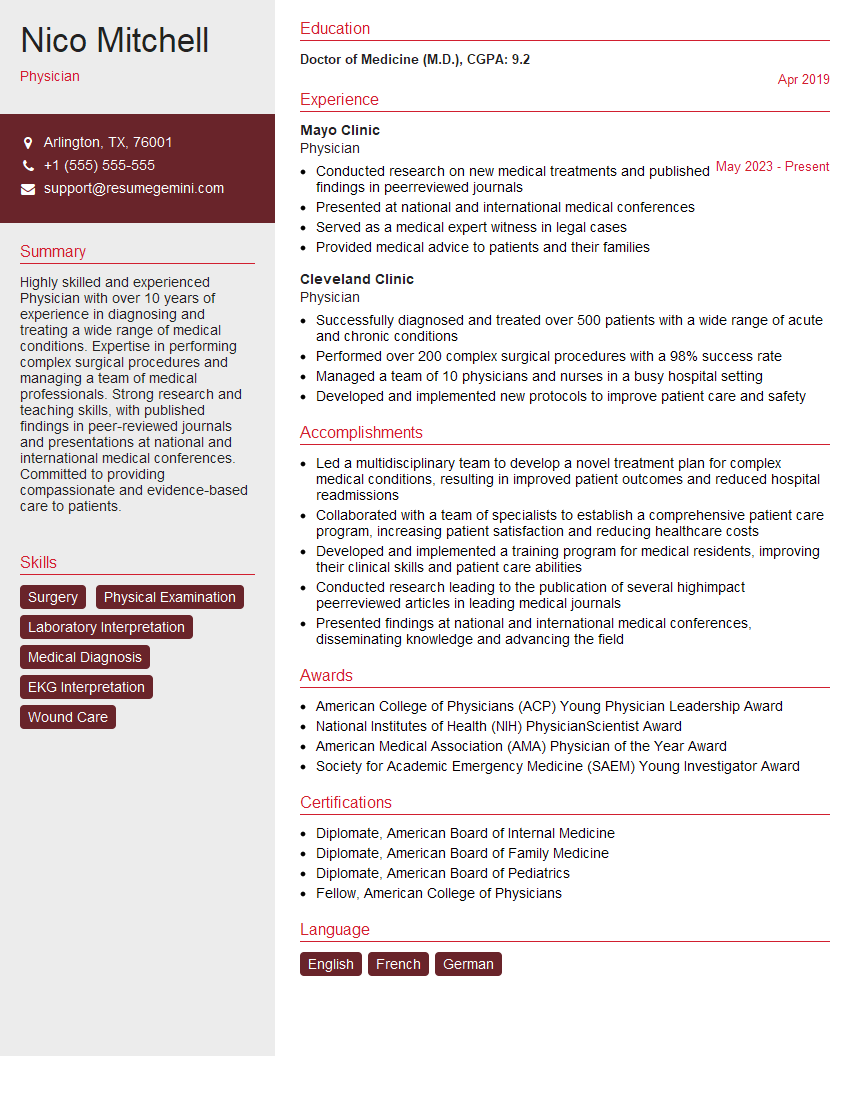
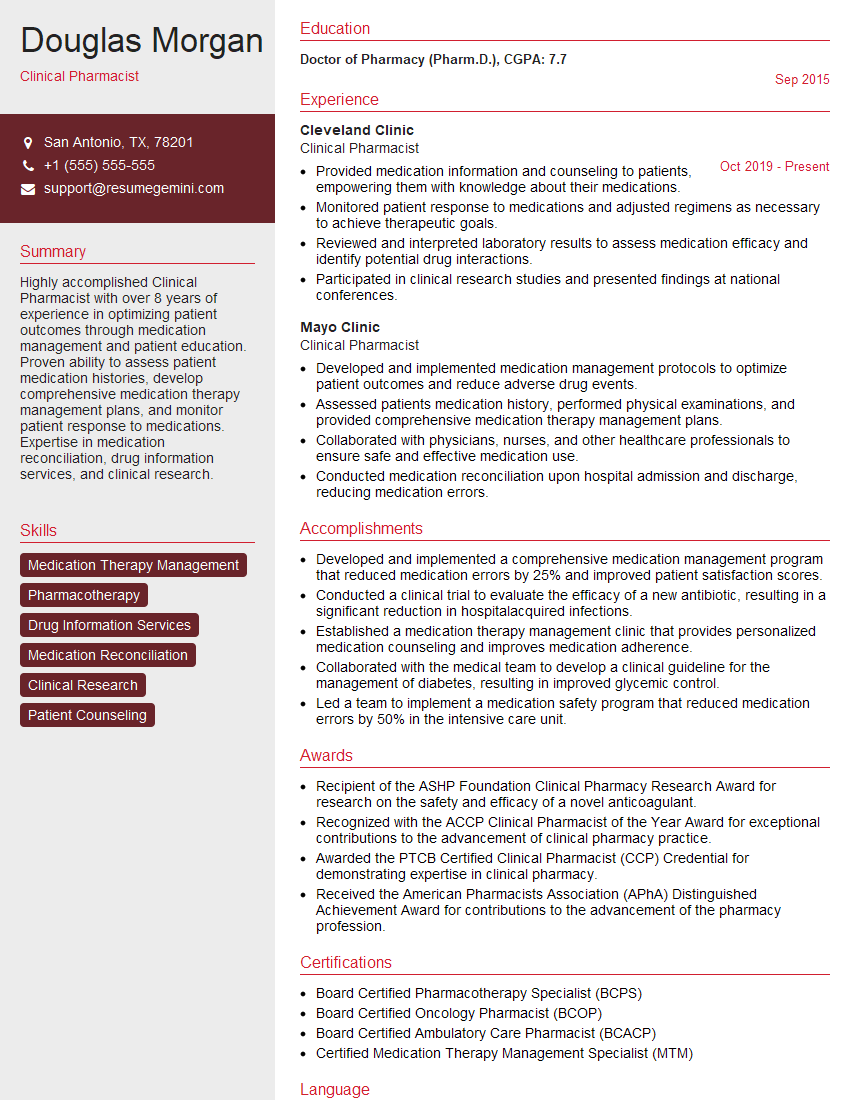
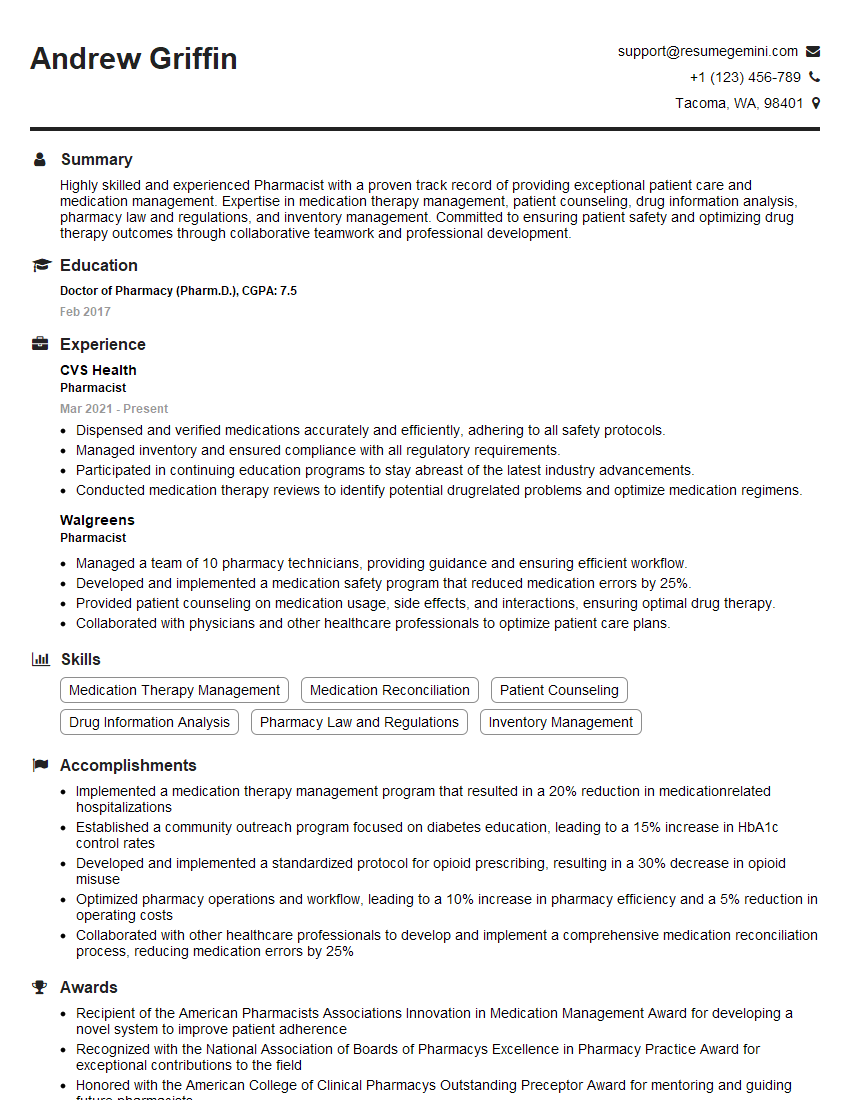
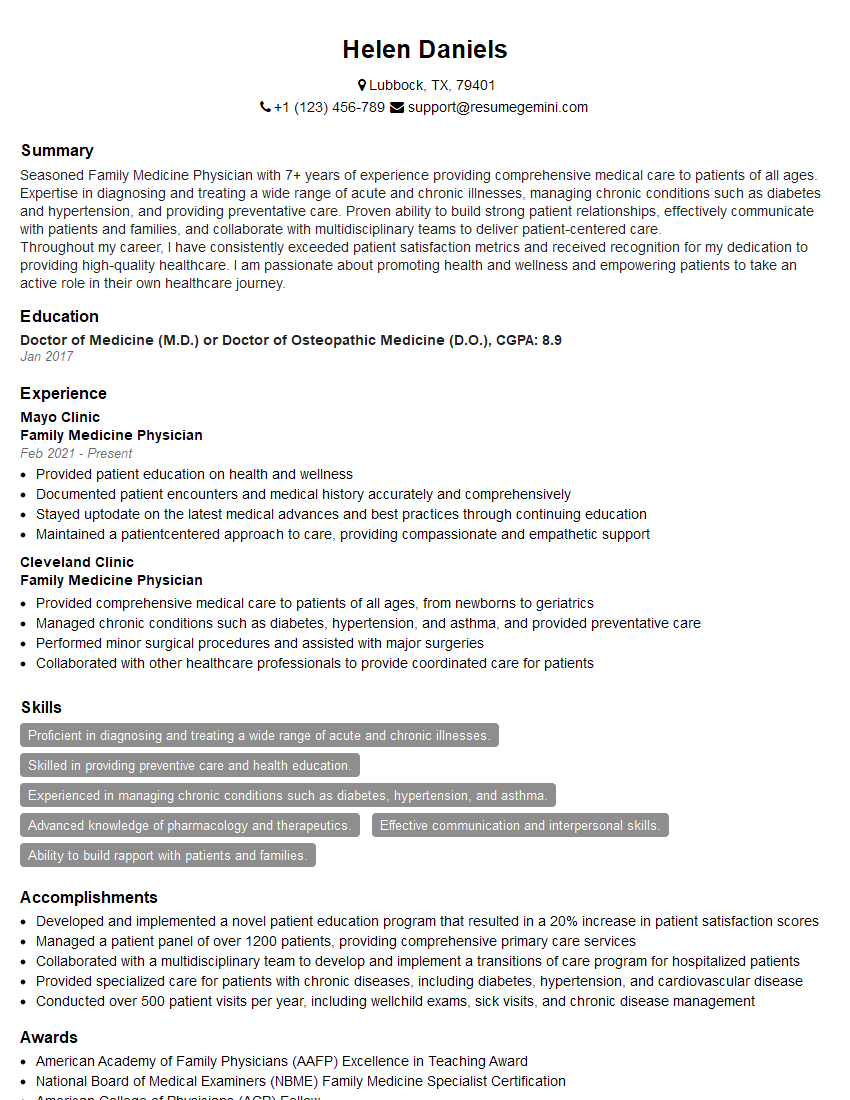
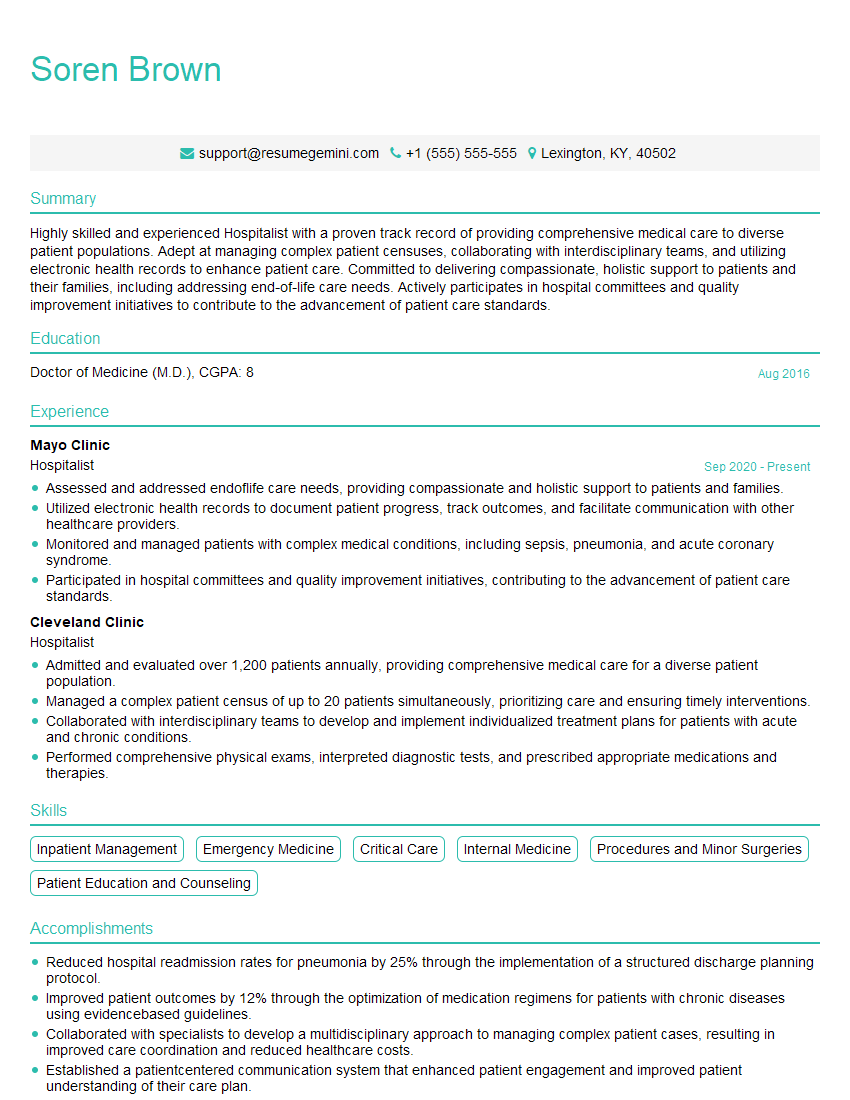
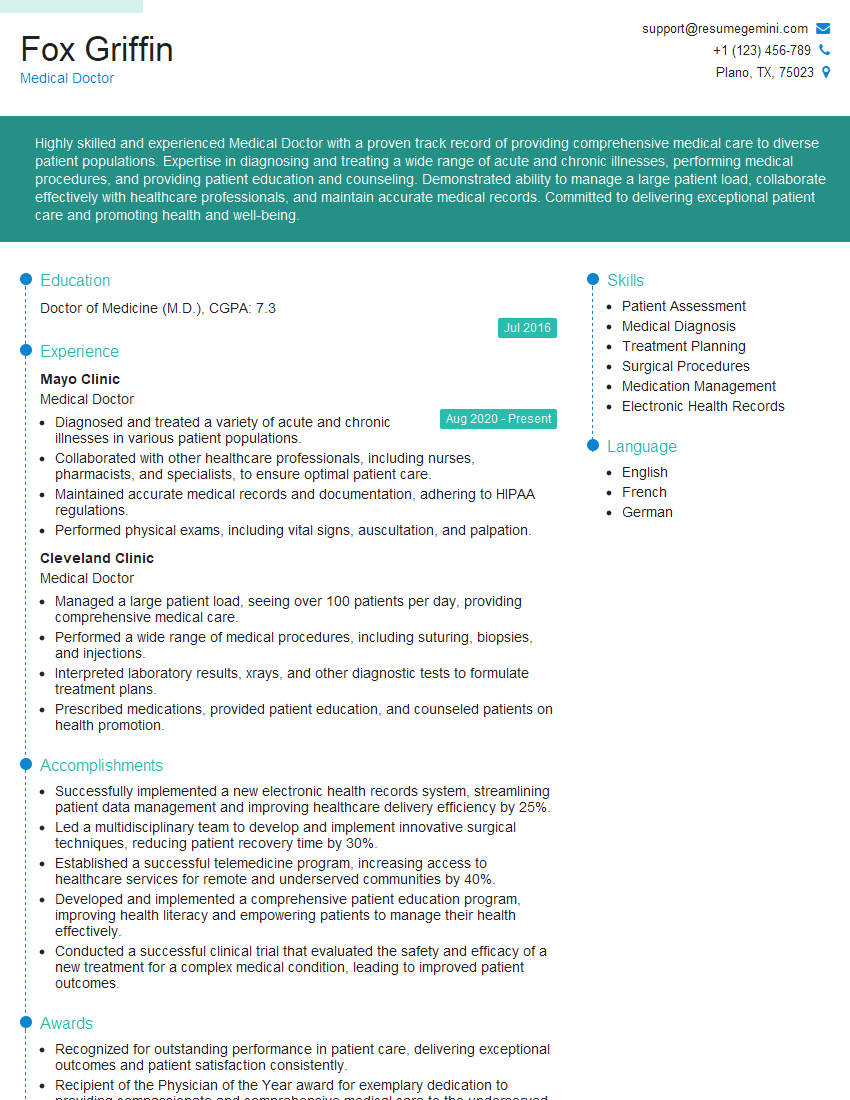
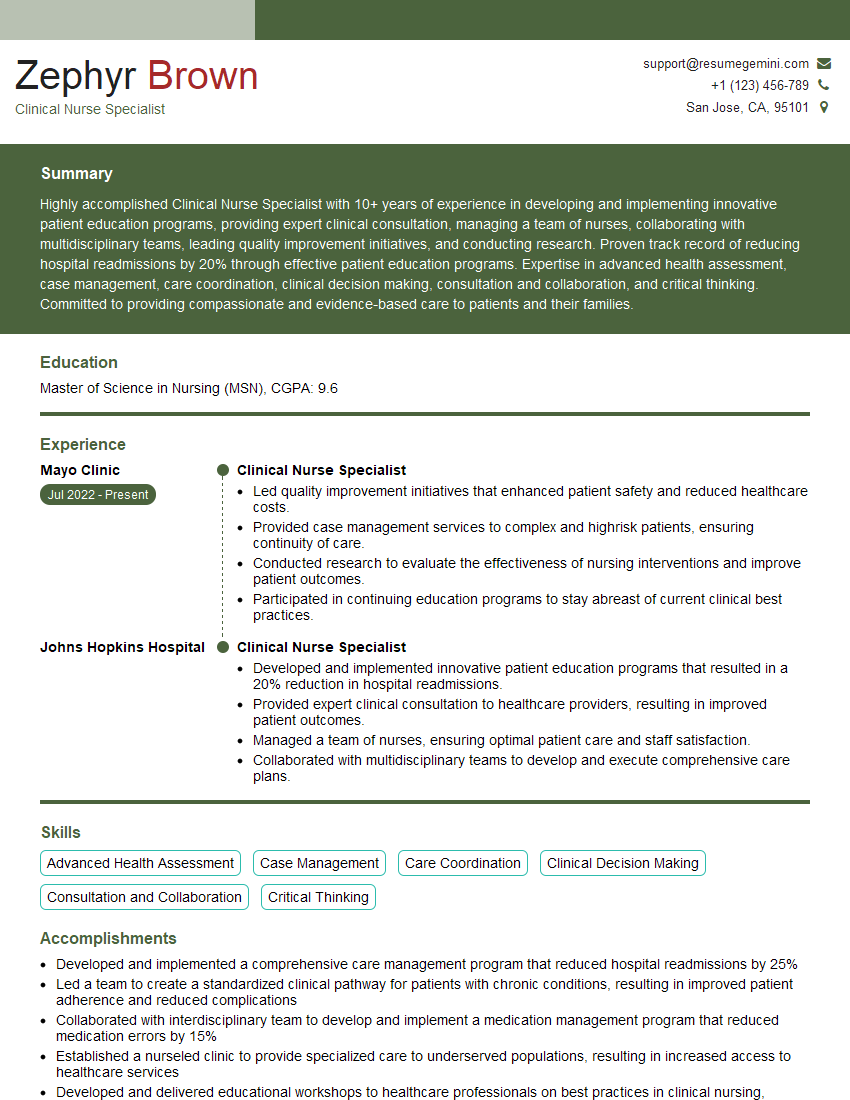
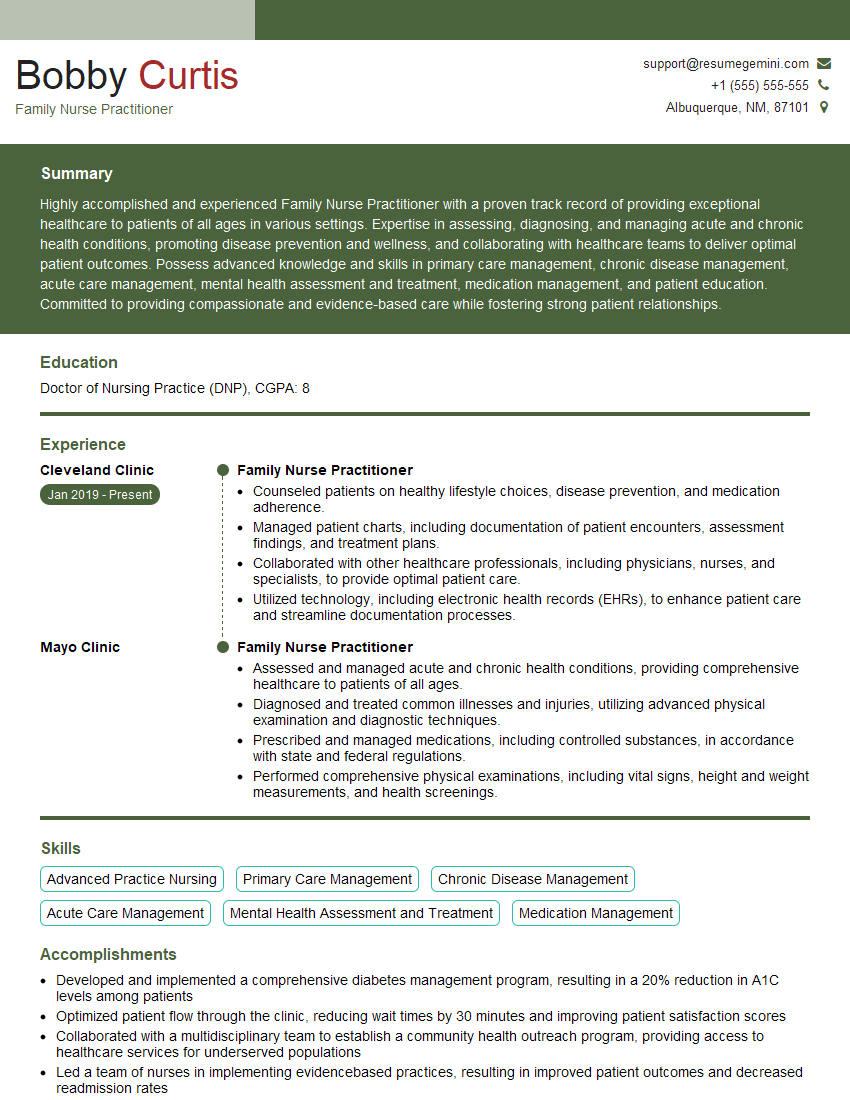
Mastering medication prescribing is crucial for career advancement in healthcare, opening doors to specialized roles and increased responsibility. A strong resume is your key to unlocking these opportunities. Crafting an ATS-friendly resume ensures your application gets noticed by recruiters. We highly recommend using ResumeGemini to build a professional and impactful resume. ResumeGemini provides tools and resources to create a compelling narrative, showcasing your skills and experience effectively. Examples of resumes tailored to Medication Prescribing professionals are available to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.