Cracking a skill-specific interview, like one for Microlaryngoscopy, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Microlaryngoscopy Interview
Q 1. Describe the procedure for performing a flexible microlaryngoscopy.
Flexible microlaryngoscopy is a minimally invasive procedure used to visualize the larynx (voice box) and surrounding structures. It’s performed using a thin, flexible endoscope, typically passed through the nose.
- Preparation: The patient is typically given topical anesthesia (a numbing spray) to the nose and throat. Sometimes mild sedation may be used for comfort.
- Insertion: The flexible endoscope, which contains a light source and camera, is gently passed through one nostril and advanced into the pharynx (throat) and larynx. The patient may experience some mild discomfort.
- Visualization: The images are projected onto a monitor, allowing the physician to thoroughly examine the vocal cords, epiglottis, and other structures within the larynx. Different positions of the endoscope can provide views of different angles.
- Examination: The physician assesses the vocal cords for lesions, swelling, polyps, paralysis, or any other abnormality. Movement of the cords during phonation (speech) can also be evaluated.
- Removal: Once the examination is complete, the endoscope is carefully withdrawn.
Imagine it like looking at the inside of your throat with a tiny, flexible camera. This procedure allows for a thorough and comfortable view, ideal for patients who may be anxious about more invasive procedures.
Q 2. What are the indications for performing a rigid microlaryngoscopy?
Rigid microlaryngoscopy involves using a rigid, larger diameter endoscope inserted through the mouth. While less comfortable, it offers superior image quality and allows for the use of instruments for biopsy or other interventions. Indications include:
- Suspected laryngeal cancer: The higher image quality helps in precise diagnosis and biopsy sampling.
- Need for surgical intervention: Rigid endoscopes can accommodate instruments for removing lesions, performing laser surgery, or other procedures.
- Evaluation of airway obstruction: The rigid scope provides a clearer view to assess the severity and cause of airway compromise.
- Foreign body removal: Instruments can be used to remove foreign objects lodged in the larynx or trachea.
- Difficult intubation: It can help visualize and assess the airway before attempting intubation in challenging cases.
Think of it as a more powerful, but less comfortable, version of the flexible scope—necessary when a clear view and potential intervention are needed.
Q 3. Explain the differences between flexible and rigid microlaryngoscopy.
The main difference lies in the rigidity of the endoscope and the resulting impact on the examination and potential for interventions.
- Rigidity: Flexible endoscopes are smaller and more flexible, allowing for easier nasal insertion and patient comfort. Rigid endoscopes provide superior image quality and allow for surgical procedures.
- Image Quality: Rigid scopes generally provide clearer, higher-resolution images due to their larger diameter and optics. Flexible scopes can be more prone to some image distortion.
- Procedure Capabilities: Rigid microlaryngoscopy allows for biopsies and surgical interventions, which are not typically possible with flexible scopes.
It’s like comparing a simple magnifying glass to a high-powered microscope. The magnifying glass (flexible) is easy to use and suitable for general observation, while the microscope (rigid) is necessary for detailed analysis and precise work.
Q 4. What are the potential complications associated with microlaryngoscopy?
Although generally safe, microlaryngoscopy, like any medical procedure, carries potential complications:
- Bleeding: Minor bleeding is possible, especially during biopsies.
- Infection: Infection at the insertion site or within the larynx is a rare but possible complication.
- Laryngeal spasm or edema: These may cause temporary difficulty breathing and usually resolve with supportive treatment.
- Airway obstruction: Although rare, particularly if a foreign body is involved, complications can lead to airway compromise, requiring immediate intervention.
- Adverse reactions to anesthesia: This includes allergic reactions or reactions to sedation.
- Tooth damage: Possible with rigid endoscopy.
These complications are rare with proper patient selection, preparation, and skilled performance of the procedure.
Q 5. How do you manage airway complications during microlaryngoscopy?
Airway complications during microlaryngoscopy are a serious concern and require immediate action. Management depends on the severity.
- Mild airway compromise: This may manifest as slight stridor (noisy breathing) or mild respiratory distress. Treatment may involve removing the endoscope, administering oxygen, and monitoring the patient.
- Severe airway compromise: This is a life-threatening emergency requiring immediate intervention. This may include securing the airway with an endotracheal tube, providing ventilation, and possibly performing a tracheotomy.
- Laryngospasm: This often responds to positive pressure ventilation with oxygen and sometimes muscle relaxants.
The key is early recognition and prompt intervention. This involves maintaining a high level of vigilance during the procedure and having a plan for emergency airway management readily available.
Q 6. Describe your experience with microlaryngoscopy in diagnosing laryngeal pathologies.
Throughout my career, I’ve performed numerous microlaryngoscopies, utilizing both flexible and rigid techniques. My experience includes diagnosing a wide range of laryngeal pathologies, from benign lesions such as vocal cord polyps and cysts to more serious conditions like laryngeal cancer. For example, I recently diagnosed a patient with early-stage squamous cell carcinoma of the larynx using rigid microlaryngoscopy, which allowed us to obtain a precise biopsy and initiate prompt treatment.
I also regularly use flexible microlaryngoscopy to evaluate patients with voice disorders, allowing us to assess vocal cord function and identify potential sources of hoarseness, such as vocal cord nodules or paralysis.
In addition to diagnosis, the procedure enables treatment such as laser ablation of lesions in a controlled manner. I am experienced in navigating the challenges associated with complex cases.
Q 7. How do you interpret the findings of a microlaryngoscopy?
Interpreting microlaryngoscopy findings requires careful assessment of the larynx’s anatomy and function. The physician evaluates several key factors:
- Vocal cord appearance: This includes assessing the color, surface characteristics (smoothness, lesions), size, and symmetry of the vocal cords.
- Vocal cord mobility: The physician evaluates how well the vocal cords move during phonation (speaking).
- Presence of lesions: Any growths, ulcers, or other abnormalities are noted, including their location, size, and appearance.
- Presence of inflammation or edema: The presence of swelling or redness within the larynx can indicate infection or other conditions.
- Airway patency: The physician assesses the width and overall condition of the airway, including the trachea and pharynx.
Correlation with the patient’s symptoms and other diagnostic tests is critical. For instance, finding a suspicious lesion necessitates biopsy, and then histopathology, to confirm the diagnosis.
Q 8. What are the limitations of microlaryngoscopy?
Microlaryngoscopy, while a powerful diagnostic and surgical tool, has certain limitations. Its magnification, while excellent for visualizing the larynx, is still limited compared to techniques like high-resolution endoscopy. This can make identifying very small lesions or subtle changes in tissue difficult. Another limitation is the indirect nature of the view; the scope itself can obstruct the view or cause inadvertent trauma. Additionally, patient factors, such as significant inflammation, obesity, or anatomical variations, can hinder visualization and maneuverability. Finally, the procedure is inherently invasive, carrying a risk of complications like bleeding, infection, or vocal cord injury. For example, in a patient with severe laryngeal stenosis, navigating the scope and performing surgery can be very challenging.
Q 9. How do you prepare a patient for microlaryngoscopy?
Patient preparation for microlaryngoscopy begins with a thorough history and physical examination to assess their overall health and identify any potential contraindications. This includes evaluating their airway, cardiovascular, and respiratory systems. Preoperative instructions are vital: patients are advised to fast for a specified period before the procedure to minimize the risk of aspiration. They should be informed about the procedure, its purpose, and potential risks and complications. An informed consent form must be signed. For example, I always discuss the possibility of voice changes post-procedure and the importance of following postoperative vocal rest instructions. Finally, depending on the anesthetic technique, additional preparations such as premedication might be necessary.
Q 10. What are the different types of anesthetic techniques used in microlaryngoscopy?
Several anesthetic techniques are used in microlaryngoscopy, chosen based on the patient’s health, the complexity of the procedure, and surgeon preference. Local anesthesia with topical or injection techniques allows for patient cooperation and reduces the risks associated with general anesthesia, but it may not be suitable for complex procedures or anxious patients. General anesthesia provides a higher level of control and patient comfort, allowing for more extensive procedures. It involves intravenous sedation and endotracheal intubation for airway management. Monitored anesthesia care (MAC) represents a middle ground, offering sedation and analgesia while maintaining the patient’s airway reflexes. The choice involves careful consideration of risks and benefits in each individual case. In one case, I opted for MAC for a patient undergoing a relatively simple biopsy, prioritizing minimizing the risks associated with general anesthesia.
Q 11. Describe your experience with microlaryngoscopy-guided laser surgery.
My experience with microlaryngoscopy-guided laser surgery is extensive. I’ve performed numerous procedures, including laser resection of vocal cord lesions (like polyps or nodules), treatment of laryngeal papillomas, and resection of early-stage laryngeal cancers. Precise laser application under direct microlaryngoscopic visualization allows for minimally invasive surgery, often leading to faster recovery and improved functional outcomes. For example, a case of recurrent respiratory papillomatosis in a child requires meticulous technique to avoid damaging the surrounding healthy tissue. The precision offered by the combination of microlaryngoscopy and the laser allows for effective lesion removal while preserving vocal function. Careful planning, precise laser settings, and a meticulous surgical technique are paramount to minimize risks and maximize results.
Q 12. How do you manage bleeding during microlaryngoscopy?
Managing bleeding during microlaryngoscopy is critical. The use of appropriate surgical instruments, meticulous technique, and careful hemostasis are crucial steps. Topical vasoconstrictors like epinephrine or cocaine can be applied to reduce bleeding. Specific surgical techniques like bipolar electrocautery can be employed to control bleeding in small vessels. In situations where bleeding is more significant or uncontrolled, surgical packing or the application of hemostatic agents like thrombin may be necessary. In rare instances, a more extensive procedure to address the bleeding source may be required. I recall a case where a small vessel bled unexpectedly during a vocal cord polyp resection; prompt use of bipolar cautery effectively controlled the bleeding without further complications. Every effort is made to minimize blood loss to reduce the risk of complications and ensure a smooth recovery for the patient.
Q 13. Describe your experience with using imaging techniques in conjunction with microlaryngoscopy.
Integrating imaging techniques with microlaryngoscopy enhances the accuracy and efficacy of diagnosis and surgery. High-resolution endoscopy, often coupled with narrow-band imaging (NBI), provides detailed visualization of the laryngeal structures. Fluoroscopy can be used for guidance during transoral laser microsurgery of certain lesions. CT scans and MRIs provide pre-operative anatomical information useful for treatment planning. For instance, using NBI during microlaryngoscopy allows for better differentiation between benign and malignant lesions. This improved visualization guides treatment decisions and enhances the surgical precision. The combination of imaging and microlaryngoscopy provides a holistic and robust approach to managing laryngeal disorders.
Q 14. What is your approach to managing a patient with a difficult airway during microlaryngoscopy?
Managing a difficult airway during microlaryngoscopy requires experience, planning, and rapid decision-making. A thorough pre-operative airway assessment is crucial. If anticipated, the use of a fiberoptic bronchoscope for airway management might be necessary. Alternatively, techniques such as awake fiberoptic intubation may be considered. In certain emergency scenarios, a tracheostomy may need to be performed. A multidisciplinary approach, often involving anesthesiologists and critical care specialists, is frequently necessary. Collaboration with the patient’s primary care team is paramount for an appropriate management strategy. A difficult airway presents unique challenges and a careful, step-wise approach is necessary to ensure patient safety.
Q 15. How do you counsel patients about the risks and benefits of microlaryngoscopy?
Counseling patients about microlaryngoscopy involves a thorough discussion of both the potential benefits and risks. It’s crucial to tailor the conversation to the individual’s understanding and anxiety levels. I begin by explaining the procedure in simple terms – essentially, it’s a minimally invasive examination of the larynx using a thin, flexible scope. I then outline the potential benefits, which depend on the reason for the procedure. For example, if it’s for diagnosing a voice problem, I explain how microlaryngoscopy allows for precise visualization of the vocal cords, helping to identify things like vocal cord nodules, polyps, or paralysis. If it’s for suspected cancer, I would explain how early detection through microlaryngoscopy is crucial for successful treatment.
Regarding risks, I explain that while complications are rare, they can include bleeding, infection, or discomfort during and after the procedure. I carefully address the patient’s concerns and answer their questions honestly and openly, reassuring them that I’ll be monitoring them closely. I might use analogies, such as comparing the scope to a tiny camera exploring a small space. I also explain the preparation needed, such as fasting before the procedure. Providing a written summary of the discussion reinforces the information and allows the patient time to process it before making an informed decision.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the latest advancements in microlaryngoscopy technology?
Microlaryngoscopy technology has seen significant advancements recently. One major development is the increasing use of high-definition (HD) cameras and digital imaging. HD technology provides much clearer and more detailed images of the larynx, allowing for more accurate diagnosis and better surgical planning. Another advancement is the incorporation of narrow-band imaging (NBI). NBI enhances the visualization of blood vessels, which helps to differentiate between normal and abnormal tissue, particularly in identifying cancerous lesions early. Flexible endoscopes have also become smaller and more maneuverable, leading to greater patient comfort and reduced risk of trauma. The integration of digital image processing and storage allows for easy sharing of images with colleagues and for storing patients’ records effectively. Lastly, the development of specialized scopes with integrated lasers facilitates treatment during the procedure. This minimizes the need for a separate surgical intervention.
Q 17. Describe your experience with using different types of microlaryngoscopy equipment.
My experience encompasses various microlaryngoscopy equipment, including both rigid and flexible endoscopes. Rigid endoscopes offer a stable view, ideal for detailed examinations and procedures that require precision. I’ve extensively used them for procedures requiring biopsy or surgical intervention. However, flexible endoscopes provide greater patient comfort and allow for easier navigation of the airway. They’re particularly useful for examining the entire larynx and pharynx during a routine evaluation. I am proficient in using various illumination systems, and I am always mindful of maintaining optimal image quality. I’ve found that different manufacturers offer slightly different ergonomic designs, impacting maneuverability. For example, I find the XYZ brand’s flexible endoscope particularly suited for pediatric cases due to its smaller diameter. Similarly, the ABC brand’s rigid scope excels in providing superior image clarity during complex procedures. Regular calibration and maintenance of each piece of equipment are essential to ensure accuracy and image clarity.
Q 18. How do you maintain the sterility of the equipment and environment during microlaryngoscopy?
Maintaining sterility is paramount during microlaryngoscopy. We adhere to strict protocols to minimize infection risk. This begins with proper hand hygiene and the use of sterile gloves, gowns, and masks by all personnel involved. The endoscopes are meticulously sterilized using a validated sterilization process, typically involving high-level disinfection and/or autoclaving. The operating environment itself is prepared using sterile drapes and solutions. All instruments and equipment that come into contact with the patient’s airway are sterile. During the procedure, aseptic technique is rigorously followed to avoid contamination. Regular monitoring and auditing of these processes are vital in ensuring ongoing adherence to standards and preventing any potential outbreaks.
Q 19. What are the key steps in post-microlaryngoscopy patient care?
Post-microlaryngoscopy care focuses on patient comfort and monitoring for potential complications. Patients are closely monitored for bleeding, airway obstruction, and signs of infection. I typically advise rest and hydration, providing specific instructions about throat lozenges or analgesics to manage any discomfort. If a biopsy was performed, instructions about follow-up appointments for pathology reports are provided. Patients are advised to avoid strenuous activities for a day or two to allow for proper healing. I also provide clear instructions regarding when to contact me or the clinic if they experience any concerning symptoms, such as excessive bleeding or difficulty breathing. This personalized approach ensures the patient has clear post-operative care information and a means of contacting me should complications arise.
Q 20. How do you document your findings from a microlaryngoscopy procedure?
Documentation of microlaryngoscopy findings is crucial for continuity of care and medico-legal reasons. My documentation includes a detailed description of the procedure, including the type of endoscope used and the techniques employed. The findings are meticulously recorded, including detailed descriptions of any lesions observed, their location, size, and appearance, and the results of any biopsies taken. High-quality images and videos are a vital part of the record and are stored digitally according to regulatory requirements. Any interventions performed during the procedure, such as laser treatment or biopsies, are carefully documented, along with the patient’s response. I use a standardized reporting format to ensure clarity and completeness. Precise and detailed documentation ensures appropriate follow-up care is provided and allows for future comparisons and analysis of the patient’s condition.
Q 21. How do you differentiate between benign and malignant lesions during microlaryngoscopy?
Differentiating between benign and malignant lesions during microlaryngoscopy requires a combination of visual assessment, and potentially biopsy and further testing. Benign lesions often appear smooth or slightly irregular in shape, with a normal surrounding tissue color. They usually do not grow rapidly and often have a well-defined border. Examples include vocal cord nodules or polyps. Malignant lesions, on the other hand, tend to present as irregular, ulcerated, or nodular growths. They might bleed easily. The tissue surrounding these lesions might exhibit abnormal color changes, often appearing pale or red. The borders are often poorly defined, and rapid growth is a significant indicator. However, visual assessment alone isn’t always conclusive. Suspicious lesions usually necessitate a biopsy, with the tissue sent for pathological examination. Additional imaging studies, such as CT or MRI scans, may be needed to assess the extent of the lesion and its infiltration into surrounding structures. The pathology report provides a definitive diagnosis, guiding further management plans.
Q 22. What is your approach to biopsy suspicious lesions during microlaryngoscopy?
My approach to biopsying suspicious lesions during microlaryngoscopy prioritizes precision and minimizing trauma. It begins with a thorough assessment of the lesion’s location, size, and vascularity using magnification and optimal illumination provided by the microlaryngoscope. I then select the appropriate biopsy instrument, which could range from micro-scissors for superficial lesions to a KTP laser for deeper or vascular lesions, depending on the suspected pathology.
The procedure itself involves careful dissection to expose the lesion and obtain a representative sample while avoiding damage to surrounding healthy tissue. Hemostasis is crucial, so I utilize bipolar cautery or topical thrombin as needed. Multiple biopsies may be necessary, especially for larger lesions or to sample different areas. Post-biopsy, I carefully inspect the surgical field for any bleeding or unexpected findings. The samples are then sent for histopathological examination to establish a definitive diagnosis.
For example, a suspicious leukoplakia on the vocal cord might require a punch biopsy using a small-gauge needle, while a more deeply situated mass might necessitate a cold steel cup biopsy or even laser excisional biopsy with subsequent histopathological analysis.
Q 23. Describe your experience with microlaryngoscopy in pediatric patients.
Microlaryngoscopy in pediatric patients requires a different approach due to their smaller anatomy and potential for increased anxiety. It’s crucial to employ a gentle and patient-centered approach, often involving parental presence and a comprehensive explanation of the procedure tailored to the child’s age and understanding. Smaller instruments and specialized scopes are essential. We use topical anesthesia and sometimes sedation, always weighing the risks and benefits carefully.
For example, a child presenting with stridor might require microlaryngoscopy to evaluate for subglottic stenosis. The procedure would involve a smaller scope and gentle handling to avoid any airway trauma. Post-operative care focuses on comfort and minimizing any airway irritation. Successful pediatric microlaryngoscopy relies heavily on a calm and reassuring approach, minimizing discomfort and anxiety throughout the process.
Q 24. How do you manage a patient with vocal cord paralysis detected during microlaryngoscopy?
Managing a patient with vocal cord paralysis detected during microlaryngoscopy involves a multi-faceted approach focusing on diagnosis, etiology determination, and tailored treatment. Initially, I’d perform a thorough history and physical examination, including neurological assessment to identify any potential causes such as trauma, viral infections, or neurological disorders. Imaging studies like MRI and CT scans may be needed to rule out lesions impinging on the recurrent laryngeal nerve.
Treatment options are individualized and depend on the cause and severity of the paralysis. This might involve watchful waiting for spontaneous recovery if the cause is idiopathic, or surgical intervention such as arytenoid adduction, medialization thyroplasty, or injection augmentation using materials like collagen or fat.
Speech therapy is often a crucial component of management, aiming to improve vocal quality and function. In cases of severe paralysis leading to significant airway compromise, tracheostomy may be necessary. The goal is to optimize the patient’s voice and breathing, restoring as much function as possible. For instance, a patient with unilateral vocal cord paralysis might benefit from voice therapy and medialization thyroplasty if spontaneous recovery does not occur.
Q 25. Describe your experience in using microlaryngoscopy for foreign body removal.
My experience with microlaryngoscopy for foreign body removal is extensive, emphasizing careful visualization and precise instrumentation. The key is to carefully assess the location and nature of the foreign body using the microlaryngoscope. I avoid any forceful maneuvers that might push the object deeper into the airway or cause damage to the surrounding tissues. The choice of instrument depends on the characteristics of the foreign body. Forceps, small hooks, or even specialized retrieval devices might be employed, with meticulous attention to protecting the delicate laryngeal mucosa.
For example, a small coin lodged in the pyriform sinus might be easily removed with forceps under direct visualization. A more complex case involving an irregular shaped object close to the vocal cords would require more skillful maneuvering and perhaps the use of specialized instruments to avoid trauma. Post-procedure, careful monitoring for any complications such as bleeding or edema is crucial. A detailed explanation to the patient and their family regarding the nature of the foreign body and the procedure is vital for overall patient care.
Q 26. What are the ethical considerations associated with microlaryngoscopy?
Ethical considerations in microlaryngoscopy center around informed consent, patient autonomy, and minimizing risks. Patients must fully understand the procedure, its benefits, risks (including potential complications like bleeding, infection, or vocal cord damage), and alternatives before providing informed consent. The physician’s role involves ensuring patients comprehend the information, answering questions thoroughly, and addressing any concerns.
Maintaining patient confidentiality and respecting their privacy are paramount. Appropriate documentation and adherence to professional standards of practice are essential. Furthermore, in cases where decisions regarding minors are involved, parental or guardian consent is necessary, ensuring the best interest of the child is prioritized. Using the appropriate level of sedation or anesthesia, ensuring qualified personnel are present to manage any complications, and ensuring appropriate post-operative care are all crucial ethical considerations.
Q 27. How do you stay current with the latest developments in microlaryngoscopy?
Staying current with the latest developments in microlaryngoscopy involves active participation in continuing medical education (CME) activities, attending relevant conferences and workshops, and engaging with professional organizations such as the American Academy of Otolaryngology. I regularly review peer-reviewed journals and relevant literature to stay abreast of advancements in surgical techniques, instrumentation, and treatment modalities.
Furthermore, I actively participate in professional societies and collaborate with colleagues to discuss challenging cases and share best practices. This continuous learning ensures that I’m employing the most up-to-date and effective techniques while providing my patients with the highest quality care. The field of microlaryngoscopy is constantly evolving, and this commitment to ongoing education is essential for maintaining expertise.
Q 28. Describe a challenging case involving microlaryngoscopy and how you resolved it.
One challenging case involved a patient with a large, friable vascular lesion obstructing nearly 75% of the airway. The lesion was highly vascularized, making traditional biopsy methods extremely risky. Initial attempts at cold biopsy resulted in significant bleeding, necessitating immediate intervention to secure the airway. After careful assessment, I opted for a staged approach using KTP laser vaporization to gradually remove the lesion in multiple sessions.
This minimized bleeding significantly while allowing for precise removal of the tissue. The patient required close monitoring post-procedure to manage inflammation and monitor the airway. This approach proved successful, gradually restoring the airway and allowing for subsequent histopathological analysis that revealed a benign lesion. This case highlighted the importance of adaptability, strategic planning, and the need to prioritize airway management in complex microlaryngoscopic procedures.
Key Topics to Learn for Microlaryngoscopy Interview
- Instrumentation and Technique: Mastering the intricacies of microlaryngoscopy equipment, including various scopes and illumination systems, and understanding the nuances of different surgical techniques.
- Anatomy and Physiology of the Larynx: Demonstrate a thorough understanding of the larynx’s complex anatomy and the physiological processes affected during microlaryngoscopic procedures. Be prepared to discuss variations and potential complications related to anatomy.
- Surgical Applications: Discuss various microlaryngoscopic procedures, including diagnostic and therapeutic applications, such as biopsy, polypectomy, and laser surgery. Highlight your understanding of indications, contraindications, and potential risks for each.
- Image Interpretation and Diagnosis: Explain your ability to interpret images obtained during microlaryngoscopy, including identifying normal and abnormal findings, and correlating them with clinical presentation and pathology reports.
- Pre- and Post-operative Care: Detail your understanding of patient preparation, intraoperative management, and post-operative care protocols specific to microlaryngoscopy.
- Complications and Management: Discuss potential complications associated with microlaryngoscopy, such as bleeding, infection, and vocal cord injury, and articulate your approach to their prevention and management.
- Ethical and Legal Considerations: Demonstrate awareness of ethical and legal implications relevant to microlaryngoscopy, including informed consent and documentation.
- Technological Advancements: Stay updated on recent technological advancements in microlaryngoscopy, including robotic-assisted surgery and image-guided techniques.
Next Steps
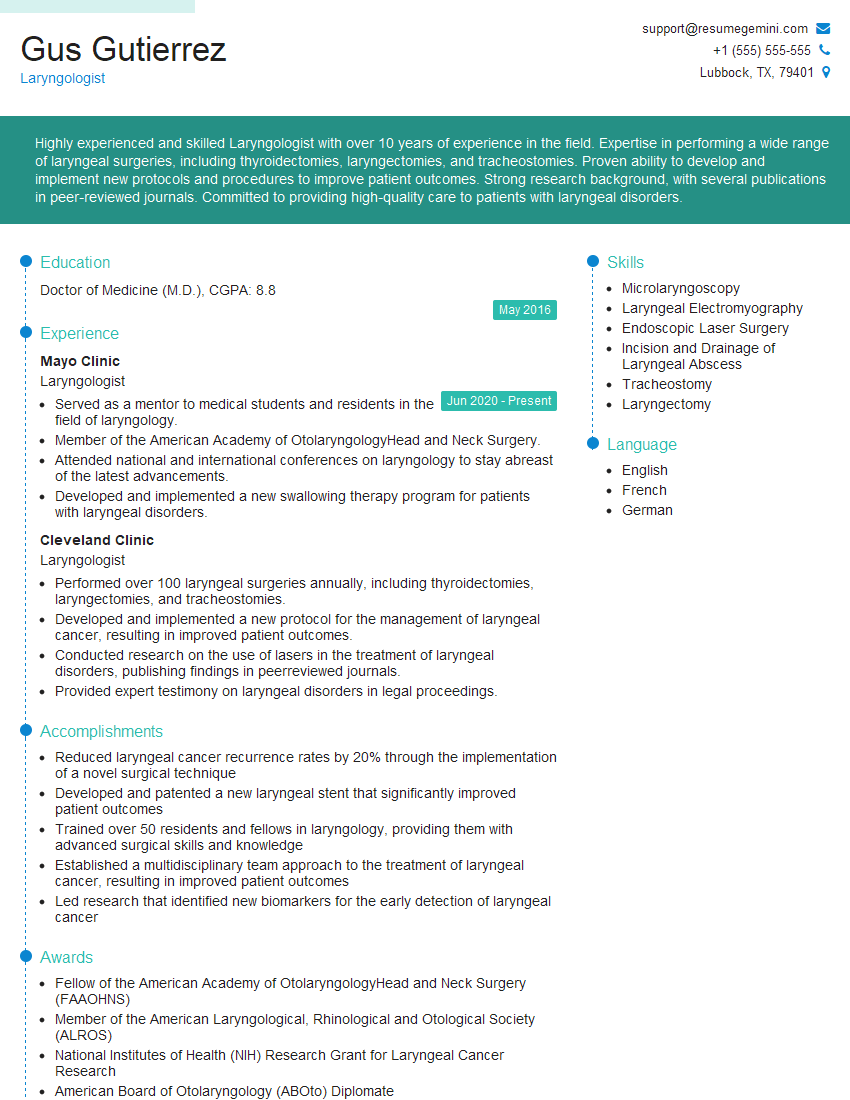
Mastering microlaryngoscopy opens doors to exciting career advancements within otolaryngology and related fields. A strong understanding of its theoretical and practical aspects is crucial for securing your desired position. To maximize your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. ResumeGemini provides examples of resumes tailored to microlaryngoscopy, ensuring your qualifications are presented effectively to potential employers. Take the next step in your career journey – build a compelling resume with ResumeGemini.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.