Cracking a skill-specific interview, like one for Narcolepsy, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Narcolepsy Interview
Q 1. Describe the diagnostic criteria for narcolepsy according to the ICSD-3.
According to the International Classification of Sleep Disorders, 3rd edition (ICSD-3), a diagnosis of narcolepsy requires the presence of excessive daytime sleepiness (EDS) plus at least one of the following: cataplexy, hypocretin deficiency, or short sleep latency on a multiple sleep latency test (MSLT).
- Excessive Daytime Sleepiness (EDS): This is a core symptom, characterized by overwhelming daytime sleepiness despite adequate nighttime sleep. It’s not simply feeling tired; it’s an irresistible urge to sleep at inappropriate times, often leading to sudden sleep episodes.
- Cataplexy: This is a sudden, brief loss of muscle tone, triggered by strong emotions like laughter, surprise, or anger. It can range from mild weakness in the knees to complete collapse. It’s a hallmark feature of narcolepsy type 1.
- Hypocretin Deficiency: Hypocretin (or orexin) is a neurotransmitter crucial for wakefulness. Cerebrospinal fluid (CSF) testing for hypocretin-1 levels is the gold standard for confirming narcolepsy type 1. Low levels strongly support the diagnosis.
- Short Sleep Latency on MSLT: The MSLT measures how quickly a person falls asleep during the day. A short sleep latency (typically less than 8 minutes) and the presence of sleep-onset REM periods (rapid eye movement sleep occurring very quickly after sleep onset) during the test are highly suggestive of narcolepsy.
A diagnosis requires a thorough clinical evaluation, including a detailed sleep history, neurological examination, and polysomnography (PSG).
Q 2. Differentiate between narcolepsy type 1 and narcolepsy type 2.
Narcolepsy is classified into two types based primarily on the presence or absence of cataplexy and hypocretin deficiency:
- Narcolepsy Type 1 (NT1): This is characterized by EDS, cataplexy, and hypocretin deficiency. Cataplexy is a defining feature, and low CSF hypocretin-1 levels confirm the diagnosis. Individuals with NT1 often experience vivid hypnagogic (sleep-onset) and hypnopompic (sleep-offset) hallucinations.
- Narcolepsy Type 2 (NT2): This type is defined by EDS but lacks cataplexy and shows normal hypocretin levels. Other narcolepsy symptoms like sleep paralysis and hypnagogic hallucinations might be present, but the absence of cataplexy and normal hypocretin levels distinguish it from NT1.
The key difference lies in the underlying neurobiological mechanism: NT1 involves a significant loss of hypocretin-producing neurons, while NT2 lacks this specific neurological finding. This difference in underlying pathophysiology may also explain differences in response to some treatments.
Q 3. Explain the role of hypocretin (orexin) deficiency in narcolepsy.
Hypocretin (also known as orexin) is a neuropeptide produced in the hypothalamus, a region of the brain crucial for regulating sleep-wake cycles. It plays a critical role in promoting wakefulness and maintaining arousal. In narcolepsy type 1, there’s a significant loss of hypocretin-producing neurons, leading to a deficiency of this crucial neurotransmitter. This deficiency disrupts the normal sleep-wake cycle, resulting in the characteristic excessive daytime sleepiness and other symptoms of narcolepsy.
Imagine hypocretin as the ‘wakefulness switch’ in the brain. In narcolepsy type 1, this switch is largely broken, leading to frequent and inappropriate transitions into sleep.
Q 4. What are the common symptoms of narcolepsy, and how do they present?
Narcolepsy presents with a constellation of symptoms, the most prominent being excessive daytime sleepiness (EDS). Other common symptoms include:
- Cataplexy: Sudden, brief loss of muscle tone, often triggered by strong emotions.
- Sleep Paralysis: Inability to move or speak while falling asleep or waking up.
- Hypnagogic and Hypnopompic Hallucinations: Vivid, dream-like experiences occurring while falling asleep (hypnagogic) or waking up (hypnopompic).
- Automatic Behaviors: Performing actions unconsciously during periods of microsleeps.
The presentation of these symptoms varies widely among individuals. Some may experience only mild EDS, while others experience severe cataplexy and frequent sleep attacks. The severity and combination of symptoms can significantly impact daily life.
For example, a person might experience a sudden inability to speak during a meeting (sleep paralysis), or collapse during a moment of laughter (cataplexy).
Q 5. Discuss the various polysomnographic findings indicative of narcolepsy.
Polysomnography (PSG) is a crucial diagnostic tool in narcolepsy. Key findings indicative of narcolepsy on PSG include:
- Short Sleep Latency on MSLT: As previously mentioned, this is a key finding, showing rapid sleep onset during daytime naps.
- Sleep-Onset REM (SOREM) Periods: The appearance of REM sleep very early in sleep episodes, often within 15 minutes of sleep onset. This is a hallmark characteristic of narcolepsy.
- Excessive Sleepiness During Overnight PSG: In some cases, individuals with narcolepsy might exhibit sleepiness even during the overnight sleep study, with frequent awakenings.
- Nocturnal Sleep Fragmentation: While sleep architecture is generally normal, people with narcolepsy might experience more fragmented sleep throughout the night.
While PSG alone doesn’t definitively diagnose narcolepsy, the combination of these findings with clinical symptoms and potentially hypocretin testing provides strong diagnostic support.
Q 6. Outline the recommended treatment strategies for narcolepsy, including pharmacotherapy and lifestyle modifications.
Treatment for narcolepsy aims to improve wakefulness and manage symptoms. Strategies typically include:
- Pharmacotherapy:
- Stimulants (e.g., methylphenidate, modafinil, armodafinil): These medications promote wakefulness and reduce daytime sleepiness. They are often the first-line treatment for EDS.
- Sodium oxybate (Xyrem): This medication is used to treat both cataplexy and excessive daytime sleepiness. It’s particularly effective for nighttime sleep disturbances and cataplexy.
- Other medications: Depending on the specific symptoms, other medications such as antidepressants (for cataplexy) or sodium channel blockers might be considered.
- Lifestyle Modifications:
- Regular Sleep Schedule: Maintaining a consistent sleep-wake schedule is crucial for regulating the circadian rhythm.
- Sufficient Sleep: Aiming for 7-9 hours of nighttime sleep is essential, though this can be challenging for individuals with narcolepsy.
- Napping Strategies: Short, planned naps (20-30 minutes) can help manage EDS, but excessive or long naps can worsen nighttime sleep.
- Healthy Diet and Exercise: A balanced diet and regular exercise can improve overall health and potentially reduce sleepiness.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): This therapy can help improve sleep habits and address any underlying sleep problems.
Treatment should be personalized based on individual symptom profiles and responses to medication. A multidisciplinary approach involving a sleep specialist, neurologist, and possibly a therapist is often beneficial.
Q 7. What are the potential side effects of commonly prescribed medications for narcolepsy?
Commonly prescribed medications for narcolepsy can have side effects, varying in severity and frequency among individuals. Some potential side effects include:
- Stimulants (methylphenidate, modafinil, armodafinil): These can cause insomnia, anxiety, headache, nausea, decreased appetite, increased blood pressure, and heart palpitations.
- Sodium oxybate (Xyrem): Common side effects include nausea, vomiting, headache, dizziness, and daytime sleepiness (paradoxically). Serious side effects, though rare, include respiratory depression.
It is crucial to discuss potential side effects with a healthcare provider before starting any medication. Regular monitoring is necessary to assess the effectiveness of the treatment and manage any side effects that may arise. Many side effects lessen over time as the body adjusts to the medication.
Q 8. How do you manage cataplexy in narcolepsy patients?
Cataplexy, a hallmark symptom of narcolepsy, involves sudden, brief episodes of muscle weakness or paralysis, often triggered by strong emotions like laughter or surprise. Managing cataplexy requires a multi-pronged approach focusing on medication and lifestyle adjustments.
Medication: Sodium oxybate (Xyrem) is often the first-line treatment for cataplexy, particularly for its effectiveness in reducing both cataplexy and nighttime sleep disruptions. Other medications, such as antidepressants like venlafaxine or atomoxetine, can also be effective in managing cataplexy. The choice of medication depends on the individual patient’s response and tolerance.
Lifestyle modifications: Patients can learn to identify and avoid triggers that provoke cataplexy. For example, limiting exposure to stressful situations or excessive laughter might be helpful. Regular sleep schedules, consistent sleep hygiene, and avoiding alcohol or caffeine are also important components of management. In severe cases, physical therapy may be considered to improve muscle strength and endurance. Close monitoring and adjustments to the treatment plan are essential to ensure optimal symptom control.
Q 9. Describe the role of sleep studies in diagnosing narcolepsy.
Sleep studies play a crucial role in diagnosing narcolepsy, serving as objective assessments of sleep architecture and daytime sleepiness. The gold standard includes polysomnography (PSG) and a multiple sleep latency test (MSLT).
Polysomnography (PSG): This overnight sleep study records brain waves (EEG), eye movements (EOG), muscle activity (EMG), heart rate, and breathing. It helps identify sleep disorders, such as sleep apnea or periodic limb movement disorder, and also assesses the presence of REM sleep intrusions (sleep onset REM periods) – a characteristic feature of narcolepsy. While the presence of sleep-onset REM periods isn’t solely diagnostic of narcolepsy, its presence is crucial for the diagnosis.
Multiple Sleep Latency Test (MSLT): This test assesses daytime sleepiness by measuring how quickly a person falls asleep during five nap opportunities spread throughout the day. Individuals with narcolepsy typically fall asleep very quickly (in less than 8 minutes), and show significant amounts of REM sleep during these short naps.
The combination of PSG and MSLT, demonstrating sleep-onset REM periods and excessive daytime sleepiness, provides strong evidence for a diagnosis of narcolepsy. Further, the results of sleep studies also rule out other sleep disorders mimicking narcolepsy.
Q 10. Explain the difference between multiple sleep latency test (MSLT) and maintenance of wakefulness test (MWT).
Both the Multiple Sleep Latency Test (MSLT) and the Maintenance of Wakefulness Test (MWT) are objective tests for evaluating sleepiness, but they serve different purposes.
Multiple Sleep Latency Test (MSLT): Measures how quickly a person falls asleep during five short nap opportunities throughout the day. It’s primarily used to assess excessive daytime sleepiness and the presence of sleep-onset REM periods, a key characteristic of narcolepsy.
Maintenance of Wakefulness Test (MWT): Measures a person’s ability to stay awake during four 40-minute intervals throughout the day. This test is used to quantify daytime alertness and assess the severity of excessive daytime sleepiness. It’s often used to assess the effectiveness of treatment or the impact of certain conditions on daytime wakefulness. A person with narcolepsy would demonstrate significant difficulty staying awake during the MWT.
In essence, the MSLT assesses how easily a person falls asleep, while the MWT assesses how well they can stay awake. They are often used together to provide a more complete picture of a patient’s sleepiness.
Q 11. How do you differentiate narcolepsy from other sleep disorders with similar symptoms?
Differentiating narcolepsy from other sleep disorders with similar symptoms, such as idiopathic hypersomnia, sleep apnea, or restless legs syndrome, requires a thorough clinical evaluation and objective testing.
Key Differentiators: Narcolepsy is characterized by the distinctive presence of cataplexy and sleep-onset REM periods (as revealed by PSG and MSLT). Idiopathic hypersomnia presents with excessive daytime sleepiness but lacks cataplexy and sleep-onset REM periods. Sleep apnea involves disrupted breathing during sleep, often resulting in daytime sleepiness, but PSG will show apneic episodes. Restless legs syndrome is characterized by uncomfortable sensations in the legs, prompting leg movements and disrupting sleep.
Diagnostic Process: A detailed medical history including sleep patterns and symptoms, a thorough neurological examination, and polysomnography (PSG) combined with a multiple sleep latency test (MSLT) are crucial steps. The specific diagnostic criteria for narcolepsy as defined by the International Classification of Sleep Disorders (ICSD) must be met.
Therefore, comprehensive evaluation considering both subjective reports and objective test results is crucial for accurate diagnosis. If there’s doubt, further investigations or consultation with sleep specialists are warranted.
Q 12. Discuss the challenges in diagnosing narcolepsy in children and adolescents.
Diagnosing narcolepsy in children and adolescents poses unique challenges because their sleep patterns are naturally variable, and they may struggle to articulate their symptoms effectively. Also, they may not experience the full range of symptoms seen in adults.
Challenges: Cataplexy, a key feature of narcolepsy, can be subtle or infrequent in children. Furthermore, children might not be able to accurately describe their sleep problems or the nature of their daytime sleepiness. They might simply be mislabeled as lazy or inattentive. The subjective nature of their reported experiences and the lack of awareness regarding narcolepsy among parents and healthcare providers pose additional hurdles.
Strategies for Diagnosis: Detailed parental history is crucial; asking targeted questions about sleep behaviors and daytime incidents that might hint at cataplexy or excessive daytime sleepiness. Observational approaches, where parents or educators provide information, also play a vital role. PSG and MSLT, whilst challenging to conduct with young children (requiring careful preparation and potentially medication), are still the gold standard for objective assessment. Early diagnosis is crucial, as prompt intervention can significantly impact the child’s quality of life and academic performance. A multidisciplinary approach, involving sleep specialists, neurologists, and child psychologists, is often essential.
Q 13. What are the long-term consequences of untreated narcolepsy?
Untreated narcolepsy can lead to significant long-term consequences that severely impact all aspects of daily life.
Physical Health: Chronic sleep deprivation compromises the immune system, increasing susceptibility to infections and illnesses. The lack of restorative sleep negatively affects cardiovascular health, potentially contributing to increased risks of hypertension and other conditions. In addition, the potential for injury due to sleep attacks, particularly in situations like driving, is a major concern. Cataplexy, if left unmanaged, can lead to falls and injuries.
Mental Health: Untreated narcolepsy is often associated with high levels of emotional distress, anxiety, depression, and reduced quality of life. The significant impact on social, academic, and professional life can lead to isolation and feelings of inadequacy.
Social and Occupational Impacts: The constant sleepiness and frequent sleep attacks severely affect daily activities, relationships, employment prospects, and education. Many people with untreated narcolepsy struggle to maintain employment, leading to economic hardship.
Early diagnosis and treatment are paramount in mitigating these long-term consequences and improving the overall quality of life for individuals with narcolepsy.
Q 14. How do you counsel patients and their families about living with narcolepsy?
Counseling patients and their families about living with narcolepsy involves a multifaceted approach focusing on education, support, and practical strategies for managing the condition.
Education: A thorough explanation of narcolepsy, its symptoms, and its impact on daily life is essential. Providing information on available treatment options and their potential benefits and side effects is key. Patients should understand the importance of adhering to their treatment plan and seeking medical attention when needed.
Support: Emphasizing the importance of self-care, stress management techniques, and connecting patients with support groups is crucial. Families need education to understand the challenges faced by the patient and how they can best offer support and avoid triggering cataplexy.
Practical Strategies: Counseling sessions can incorporate practical strategies for managing sleepiness and cataplexy, such as implementing regular sleep schedules, adapting their daily routines, and learning to identify and avoid personal triggers. Discussion around safety measures, especially concerning driving and operating machinery, is critical. In summary, a compassionate and informative approach, along with strong emphasis on a collaborative approach for management, is essential for empowering patients and their families to live full and productive lives.
Q 15. Describe the role of patient education in managing narcolepsy.
Patient education is paramount in managing narcolepsy. It empowers individuals to understand their condition, actively participate in their treatment, and improve their quality of life. This isn’t just about explaining symptoms; it’s about equipping patients with the knowledge and skills to manage their daily challenges.
- Understanding the Disease: Patients need a clear understanding of narcolepsy’s core features: excessive daytime sleepiness (EDS), cataplexy (sudden muscle weakness), sleep paralysis, and hypnagogic/hypnopompic hallucinations. We explain that these aren’t simply laziness or poor sleep habits but symptoms of a neurological disorder affecting brain chemicals that regulate sleep-wake cycles.
- Medication Management: We thoroughly discuss medication options, their benefits, potential side effects, and the importance of adherence. We emphasize the need for regular blood tests to monitor medication levels and adjust dosages as needed. We also emphasize the importance of open communication regarding any side effects so adjustments can be made.
- Lifestyle Modifications: This is a crucial aspect. We advise patients on strategies for managing EDS, such as regular sleep schedules, short naps, and avoiding sleep-depriving activities. We discuss the importance of diet, exercise, and stress management. For example, a patient struggling with daytime sleepiness might benefit from scheduling regular short power naps throughout the day instead of one long sleep.
- Support and Resources: We connect patients with support groups, online communities, and relevant resources to foster a sense of community and provide emotional support. Knowing they’re not alone in their struggle is immensely valuable.
For instance, I recently worked with a young woman who was initially hesitant to take medication. After a thorough discussion about her concerns and the benefits of treatment, she felt empowered to begin her medication regime, leading to a significant improvement in her daily functioning.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the current research directions in narcolepsy?
Current research in narcolepsy focuses on several key areas:
- Improved Diagnostics: Researchers are exploring more accurate and less invasive diagnostic methods. This includes developing biomarkers to identify narcolepsy earlier and more reliably.
- Understanding Etiology: Further research is needed to unravel the precise mechanisms involved in the development of narcolepsy, particularly the role of genetics and environmental triggers. The focus is on identifying specific genes and environmental factors that contribute to the disease process.
- Novel Treatments: Significant effort is dedicated to developing new and more effective treatments, including exploring novel drug targets and non-pharmacological interventions like neuromodulation techniques.
- Personalized Medicine: The goal is to tailor treatment strategies to individual patients based on their genetic makeup, symptom profiles, and other factors. This promises more effective and safer treatment outcomes.
- Comorbidities: Studies are investigating the complex interplay between narcolepsy and comorbid conditions like attention-deficit/hyperactivity disorder (ADHD), depression, and anxiety, aiming to develop more comprehensive treatment approaches.
For example, exciting advancements are being made in understanding the role of hypocretin (orexin) deficiency in narcolepsy and developing potential therapies that could address this deficiency more effectively.
Q 17. Discuss the impact of narcolepsy on daily life and productivity.
Narcolepsy significantly impacts daily life and productivity. The hallmark symptom, excessive daytime sleepiness (EDS), makes concentrating, working, and engaging in social activities extremely challenging. Imagine trying to drive, attend a meeting, or even have a conversation when you’re constantly battling overwhelming fatigue.
- Workplace Challenges: EDS can lead to reduced work performance, absenteeism, and difficulty maintaining employment. Simple tasks can become Herculean efforts, impacting career progression and financial stability.
- Social Life: The unpredictable nature of narcolepsy’s symptoms can disrupt social interactions and relationships. The fear of falling asleep unexpectedly, experiencing cataplexy in public, or struggling to stay awake during social events can lead to social isolation and anxiety.
- Safety Concerns: Cataplexy, a sudden loss of muscle tone triggered by strong emotions, can pose significant safety risks, particularly while driving or engaging in activities requiring alertness. Sleep paralysis and hallucinations can also be distressing and frightening.
- Mental Health: Living with narcolepsy often leads to increased rates of depression and anxiety. The chronic nature of the illness, coupled with its social and occupational impacts, can be emotionally taxing.
For instance, I’ve seen patients who have lost their jobs due to their inability to maintain consistent work performance because of EDS. Others struggle to maintain relationships due to the unpredictability of their symptoms. Early diagnosis and comprehensive management are essential to mitigate these negative impacts.
Q 18. How do you assess the severity of narcolepsy in a patient?
Assessing narcolepsy severity involves a multi-faceted approach. We don’t simply rely on a single test; instead, we use a combination of methods to get a comprehensive picture.
- Clinical Evaluation: A detailed history taking to identify the presence and severity of core symptoms (EDS, cataplexy, sleep paralysis, hallucinations). We use standardized questionnaires like the Epworth Sleepiness Scale (ESS) to quantify EDS.
- Polysomnography (PSG): This overnight sleep study is crucial for ruling out other sleep disorders and identifying characteristic sleep architecture abnormalities in narcolepsy, such as early onset of REM sleep.
- Multiple Sleep Latency Test (MSLT): This test measures how quickly a person falls asleep during the day. Short sleep latencies and the presence of REM sleep during these short naps strongly suggest narcolepsy.
- Hypocretin-1 (Orexin) Blood Test: This test measures the level of hypocretin-1 in the cerebrospinal fluid. Low levels are highly indicative of narcolepsy type 1.
By combining these assessments, we can determine the severity of the condition, identify the type of narcolepsy (type 1 or type 2), and tailor treatment accordingly. A patient with frequent cataplexy and severe EDS will have a different treatment plan compared to a patient with primarily EDS.
Q 19. What are the ethical considerations in treating patients with narcolepsy?
Ethical considerations in treating narcolepsy center around several key areas:
- Informed Consent: Patients must be fully informed about the risks and benefits of different treatment options, including medication side effects and potential long-term consequences. They must have the autonomy to make informed decisions about their care.
- Confidentiality: Maintaining patient confidentiality is crucial. Information about their diagnosis and treatment should only be shared with their consent, unless legally required.
- Balancing Benefits and Risks: We need to carefully weigh the potential benefits of treatment against the potential risks and side effects of medications. This requires ongoing monitoring and open communication with the patient.
- Access to Care: Ensuring equitable access to quality diagnosis and treatment for all patients, regardless of their socioeconomic status or geographic location, is a critical ethical concern.
- Driving Safety: When a patient’s narcolepsy poses a safety risk to themselves or others (e.g., driving), we have an ethical obligation to discuss these risks and explore strategies to mitigate them. This might involve recommending driving restrictions or suggesting alternative transportation.
For example, discussing the potential side effects of stimulants, such as anxiety or insomnia, and working collaboratively with the patient to find the right balance between symptom control and side-effect management is an ethical imperative.
Q 20. Describe your experience with managing comorbid conditions in narcolepsy patients.
Managing comorbid conditions in narcolepsy patients is a significant part of my practice. Many patients with narcolepsy also experience other conditions, such as ADHD, depression, anxiety, and obesity. These conditions can complicate treatment and worsen the overall impact of narcolepsy on daily life.
- Integrated Approach: We take a holistic, integrated approach, addressing both the narcolepsy and the comorbid conditions simultaneously. This may involve coordinating care with other specialists, such as psychiatrists or therapists.
- Medication Management: Careful consideration is given to medication interactions and potential additive side effects when prescribing medications for both narcolepsy and comorbid conditions.
- Lifestyle Interventions: Lifestyle changes like regular exercise, healthy diet, and stress management techniques can be beneficial for managing both narcolepsy and many comorbid conditions.
- Therapy: Cognitive behavioral therapy (CBT) for insomnia and other therapies can be valuable in addressing mental health comorbidities and improving coping mechanisms.
For instance, a patient with both narcolepsy and depression might require medication for both conditions, along with psychotherapy to address the underlying depression. Careful monitoring and adjustment of medication dosages are crucial to ensure safety and efficacy.
Q 21. Explain the role of genetic factors in the etiology of narcolepsy.
Genetic factors play a significant role in the etiology of narcolepsy, particularly type 1. While narcolepsy isn’t simply inherited in a Mendelian fashion, genetic susceptibility significantly increases the risk of developing the disease.
- HLA-DQB1*06:02 Gene: The strongest genetic association with narcolepsy type 1 is with the human leukocyte antigen (HLA) gene, specifically the DQB1*06:02 allele. Individuals carrying this allele have a substantially higher risk of developing narcolepsy type 1 compared to those who do not.
- Other Genes: Beyond HLA-DQB1*06:02, other genes are being identified that contribute to the risk, highlighting the complex genetic architecture of this disorder.
- Environmental Triggers: While genetic predisposition is crucial, environmental factors are also essential. In some cases, a viral infection or other environmental triggers might act as a catalyst in individuals with a genetic predisposition to develop narcolepsy.
Understanding the genetic underpinnings of narcolepsy is crucial for developing more precise diagnostic tools, identifying individuals at high risk, and potentially designing targeted therapies in the future.
Q 22. What are the limitations of current diagnostic tools for narcolepsy?
Current diagnostic tools for narcolepsy, while improved, still have limitations. The gold standard, the Multiple Sleep Latency Test (MSLT), measures daytime sleepiness but doesn’t definitively diagnose narcolepsy. A short sleep latency (falling asleep quickly during the test) is suggestive, but it’s not specific to narcolepsy; other sleep disorders can show similar results. Similarly, the overnight polysomnography (PSG), which assesses sleep architecture, can reveal the presence of REM sleep without cataplexy, a hallmark of narcolepsy. The absence of hypocretin-1 (orexin) in cerebrospinal fluid (CSF) is a strong indicator, but CSF testing is invasive and not always readily available. Therefore, diagnosis often relies on a combination of clinical symptoms, patient history, and these tests, sometimes leading to delays or misdiagnosis.
For example, a patient might experience excessive daytime sleepiness and cataplexy, but their MSLT might not be conclusive if other sleep issues are present. This highlights the need for careful clinical judgment and a comprehensive approach to diagnosis.
Q 23. Discuss the use of stimulant medications in the treatment of narcolepsy.
Stimulant medications, such as methylphenidate and amphetamine-based drugs, are a cornerstone of narcolepsy treatment. They act by increasing dopamine and norepinephrine levels in the brain, promoting wakefulness and reducing daytime sleepiness. These are generally well-tolerated, but side effects like anxiety, insomnia, and increased heart rate can occur. Dosage must be carefully adjusted to maximize benefit while minimizing side effects. Stimulants are most effective for managing EDS (Excessive Daytime Sleepiness), a major symptom of narcolepsy. However, they don’t address cataplexy or other sleep disturbances associated with the condition.
For instance, a patient might start on a low dose of methylphenidate and gradually increase it over several weeks based on their response and tolerance. Regular monitoring for side effects is crucial, and adjustments are made as needed. It’s important to remember stimulants are not a cure; they help manage the symptoms.
Q 24. What are the non-pharmacological approaches to managing narcolepsy?
Non-pharmacological approaches play a significant role in managing narcolepsy. These strategies focus on improving sleep hygiene, lifestyle modifications, and cognitive-behavioral therapy (CBT). Good sleep hygiene involves maintaining a regular sleep schedule, creating a conducive sleep environment (dark, quiet, cool), and avoiding caffeine and alcohol close to bedtime. Regular exercise can improve sleep quality, but should be avoided close to bedtime. CBT for insomnia (CBT-I) is particularly useful in addressing sleep-related difficulties and improving sleep efficiency. Other lifestyle changes such as stress reduction techniques (yoga, meditation) and planned naps can also aid in managing symptoms.
Imagine a patient who struggles with insomnia. CBT-I could help them identify and modify unhelpful sleep behaviors, improve sleep efficiency, and reduce anxiety related to sleep, thus improving their overall sleep quality and daytime functioning.
Q 25. How do you monitor the effectiveness of treatment in narcolepsy patients?
Monitoring treatment effectiveness in narcolepsy involves a multi-faceted approach. Regular follow-up appointments are crucial, where subjective measures like patient-reported daytime sleepiness (using scales like the Epworth Sleepiness Scale – ESS) are assessed. Objective measures, such as repeat MSLTs, may be conducted to gauge the impact of treatment on sleep latency and daytime sleepiness. Furthermore, we assess the patient’s overall functional status – their ability to perform daily tasks, work productivity, and quality of life. We closely monitor for side effects of medication and make necessary adjustments. Changes in cataplexy frequency and severity are also tracked.
For example, a significant decrease in ESS score combined with improved work performance and reduced cataplexy episodes indicates successful treatment.
Q 26. Describe your approach to adjusting medication dosages in narcolepsy patients.
Adjusting medication dosages in narcolepsy is a gradual process guided by individual patient response and tolerance. We start with a low dose and titrate upwards based on clinical response, carefully monitoring for side effects. The increase should be incremental, with regular assessments of daytime sleepiness, alertness, and any adverse effects. If side effects are prominent, the dose may need to be reduced or a different medication considered. Patient feedback is crucial throughout the adjustment process. This requires a collaborative approach, where open communication and shared decision-making are key.
For example, if a patient reports increased anxiety on a particular dose, we might reduce it slightly and monitor for improvement. If the daytime sleepiness is still significant despite medication, we would explore alternative medications or consider adding other therapeutic approaches such as CBT-I.
Q 27. What are the key indicators of treatment success in narcolepsy?
Key indicators of treatment success in narcolepsy include a significant reduction in daytime sleepiness (as measured by the ESS or MSLT), improved alertness and concentration, fewer cataplexy episodes, and an overall enhancement in quality of life. Patients should report improved ability to perform daily activities, better work productivity, and increased participation in social and recreational activities. Subjective measures, like the patient’s self-reported experience of daytime functioning and sleep quality, are equally crucial in determining treatment success. Objective measures provide quantifiable data, but patient perception of their own improvement is essential.
A successful outcome might be a patient who previously experienced severe daytime sleepiness and frequent cataplexy, but after treatment, can now maintain a regular work schedule, engage in social activities without excessive fatigue, and experience a significant decrease in cataplexy episodes.
Q 28. How do you address patient concerns and anxieties related to narcolepsy?
Addressing patient concerns and anxieties related to narcolepsy involves a compassionate and empathetic approach. Many patients experience significant emotional distress due to the chronic nature of the illness and its impact on daily life. It’s important to actively listen to their concerns, validate their feelings, and provide accurate information in a clear, understandable way. Educating patients about narcolepsy, its management, and available resources is vital. Referral to support groups and counseling can provide additional emotional support and coping strategies. Open communication, empathy, and a collaborative treatment approach build trust and facilitate successful management of the condition.
For example, a patient might fear the long-term implications of narcolepsy. Addressing this might involve discussing strategies for managing the condition throughout their life, emphasizing the potential for improvement with treatment, and connecting them with other patients who have successfully adapted to living with narcolepsy.
Key Topics to Learn for Narcolepsy Interview
- Diagnosis and Classification: Understand the different types of narcolepsy (type 1 and type 2), their diagnostic criteria, and the role of polysomnography and multiple sleep latency tests.
- Pathophysiology: Grasp the underlying mechanisms of narcolepsy, including the role of hypocretin/orexin deficiency, and the impact on sleep-wake regulation.
- Symptoms and Management: Be familiar with the characteristic symptoms (excessive daytime sleepiness, cataplexy, sleep paralysis, hypnagogic hallucinations), and various treatment approaches including medication, lifestyle modifications, and behavioral therapies.
- Differential Diagnosis: Know how to differentiate narcolepsy from other sleep disorders and medical conditions that present with similar symptoms.
- Impact on Daily Life: Discuss the significant effects narcolepsy has on patients’ daily lives, including social, occupational, and safety implications.
- Research and Future Directions: Be aware of ongoing research in narcolepsy, potential advancements in treatment, and unmet needs in patient care.
- Patient Education and Counseling: Understand the importance of patient education in managing narcolepsy effectively and improving quality of life. Discuss strategies for providing empathetic and informative counseling.
- Ethical Considerations: Be prepared to discuss ethical dilemmas that may arise in the diagnosis and management of narcolepsy, such as informed consent and treatment decisions.
Next Steps
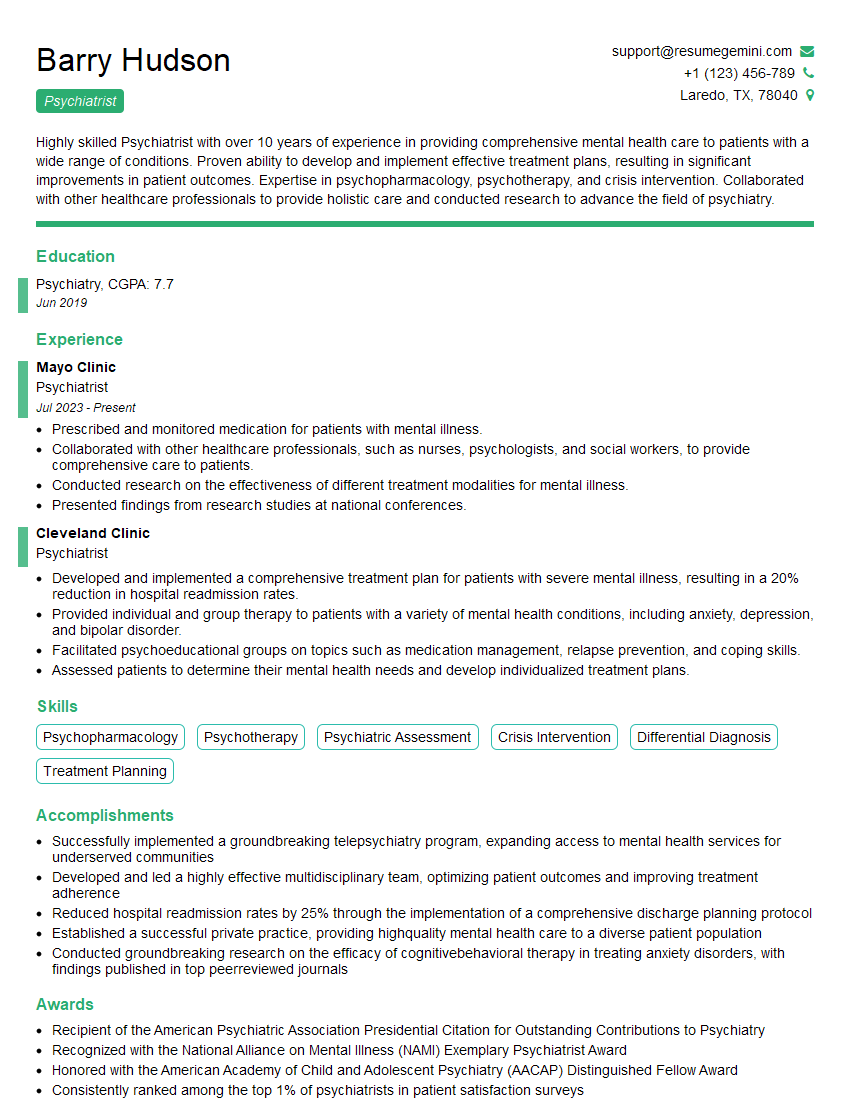
Mastering your understanding of narcolepsy is crucial for career advancement in the field of sleep medicine and related areas. A strong grasp of the disease’s complexities demonstrates expertise and dedication. To significantly improve your job prospects, creating an ATS-friendly resume is vital. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to showcasing expertise in Narcolepsy are available within ResumeGemini to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.