Preparation is the key to success in any interview. In this post, we’ll explore crucial Neuropsychological Report Writing interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Neuropsychological Report Writing Interview
Q 1. Describe the standard components of a comprehensive neuropsychological report.
A comprehensive neuropsychological report follows a standardized structure to ensure clarity and consistency. Think of it like a well-organized house – each room (section) serves a specific purpose.
- Identifying Information: This section includes the patient’s name, date of birth, referral source, and date of testing. It’s the foundation – essential for accurate identification.
- Reason for Referral: This explains why the patient was referred for neuropsychological testing. For instance, it might be due to a suspected traumatic brain injury, cognitive decline, or learning disability. This sets the context for the entire report.
- History: This section provides background information, including medical history, social history, educational history, and family history. Think of it as the blueprint – understanding the patient’s past helps interpret the present findings.
- Behavioral Observations: This describes the patient’s behavior during the testing session. Were they cooperative? Anxious? These qualitative observations add crucial context to the test results.
- Test Procedures: This lists all the neuropsychological tests administered, including the specific versions used. This section ensures transparency and reproducibility of the assessment.
- Test Results: This section presents the quantitative data from the tests, often including scores, percentiles, and standardized scores. It’s the raw data – the foundation for interpretation.
- Interpretation: This is the core of the report. It integrates quantitative and qualitative data to provide a comprehensive interpretation of the patient’s cognitive strengths and weaknesses. This is where the puzzle pieces come together.
- Summary and Conclusions: This summarizes the key findings and provides a concise statement of the neuropsychological diagnosis or conclusions. It’s the final verdict – clear and to the point.
- Recommendations: This section outlines recommendations for treatment, rehabilitation, or further evaluation. This section guides the next steps in the patient’s care.
Q 2. Explain the importance of clear and concise language in neuropsychological report writing.
Clear and concise language is paramount in neuropsychological report writing because the report’s audience may include clinicians, attorneys, patients, and educators, each with varying levels of understanding of neuropsychology. Imagine trying to explain complex brain functions using highly technical jargon to a patient who is already stressed and confused – it would be ineffective.
Using simple, straightforward language ensures that the key findings and recommendations are easily understood, regardless of the audience’s background. Avoiding jargon, employing active voice, and structuring the report logically are all crucial for clarity. A well-written report minimizes misinterpretations and facilitates effective communication, ensuring the report serves its purpose – informing and guiding the reader.
Q 3. How do you integrate qualitative and quantitative data in your reports?
Integrating qualitative and quantitative data is essential for a comprehensive and nuanced interpretation. Quantitative data, such as test scores and percentiles, provide objective measurements. However, they don’t tell the whole story. Qualitative data, such as observations of the patient’s behavior and effort during testing, provide crucial context.
For example, a patient might score poorly on a memory test (quantitative data). However, behavioral observations might reveal that they were highly anxious or distracted during the test (qualitative data). This information is crucial for accurate interpretation. We don’t want to misinterpret low scores as indicating a severe memory impairment if anxiety was a significant factor. Integrating both types of data allows for a more accurate and holistic understanding of the patient’s cognitive abilities.
Q 4. What strategies do you use to ensure the accuracy and reliability of your reports?
Ensuring accuracy and reliability is the cornerstone of ethical and responsible neuropsychological assessment. I employ several strategies:
- Using standardized tests: Standardized tests have established norms and procedures, reducing bias and increasing reliability.
- Adhering to strict testing protocols: Following the test manual precisely ensures consistency and minimizes errors.
- Thorough review of test data: I carefully examine scores, patterns of performance, and any inconsistencies before drawing conclusions. This includes checking for possible errors in data entry or administration.
- Consulting relevant literature: I constantly update my knowledge on the latest research and best practices in neuropsychology to ensure my interpretations are current and accurate.
- Peer review (when applicable): In complex cases, I may seek feedback from colleagues to ensure objectivity and rigor.
- Maintaining detailed records: Comprehensive documentation of the testing process allows for review and verification of the findings, improving accountability and transparency.
By combining these methods, I aim to produce reports that are not only accurate but also transparent and defensible.
Q 5. How do you tailor your report writing style to different audiences (e.g., clinicians, attorneys, patients)?
Tailoring my report writing style is crucial for effective communication. For clinicians, I use more technical language and focus on diagnostic implications. For example, I might discuss specific cognitive deficits in terms of their neuroanatomical correlates.
For attorneys, I maintain a clear, concise, and objective style, emphasizing the legal relevance of my findings. I avoid jargon and ensure the language is easily understood in a legal context.
For patients, I use simple, direct language and avoid technical terminology. I focus on explaining the results in a way that is easy to understand and relevant to their daily lives. The goal is to empower patients by giving them a clear understanding of their cognitive strengths and weaknesses. A simple analogy might be used to make complex concepts more relatable.
Q 6. Explain your approach to interpreting neuropsychological test results.
Interpreting neuropsychological test results involves a multifaceted approach that goes beyond simply looking at individual scores. It’s like solving a complex puzzle where each piece (test result) contributes to the overall picture.
My approach involves:
- Considering the pattern of strengths and weaknesses: A profile of cognitive abilities is more informative than individual scores. For instance, a patient may have relatively preserved verbal abilities but significant impairments in visual-spatial skills.
- Considering the patient’s premorbid functioning: Understanding the patient’s cognitive abilities before the onset of any neurological condition or injury is essential for accurate interpretation. This might involve using demographic data or collateral information from family members.
- Evaluating the consistency of findings across different tests: Convergent evidence strengthens the conclusions. If multiple tests point towards a specific cognitive deficit, the interpretation is more reliable.
- Integrating qualitative data with quantitative data: As mentioned before, behavioral observations and other qualitative information are crucial for interpreting test scores accurately.
- Considering the impact of confounding variables: Factors like medication, fatigue, or anxiety can affect test performance. Careful consideration is needed to disentangle their impact from underlying cognitive deficits.
Ultimately, the goal is to develop a comprehensive and nuanced understanding of the patient’s cognitive profile, which may inform diagnosis and treatment planning.
Q 7. Describe your experience with different types of neuropsychological tests and their interpretations.
My experience encompasses a wide range of neuropsychological tests, each designed to assess specific cognitive domains. I have extensive experience with tests assessing:
- Memory: Tests like the Wechsler Memory Scale (WMS), California Verbal Learning Test (CVLT), and Rey Auditory Verbal Learning Test (RAVLT) are frequently used to assess various aspects of memory, including immediate recall, delayed recall, and recognition memory. Interpretation involves analyzing the pattern of performance across different memory tasks.
- Attention and Executive Functions: Tests such as the Trail Making Test (TMT), Stroop Color-Word Test, and Wisconsin Card Sorting Test (WCST) assess attention, processing speed, and executive functions. These functions are critical for higher-level cognitive processes.
- Language: Tests assessing verbal fluency, comprehension, and naming skills provide insights into language processing. The Boston Naming Test is a common example.
- Visuospatial skills: Tests such as the Rey-Osterrieth Complex Figure Test (RCFT) and the Visual Reproduction subtest of the WMS assess visual perception, constructional abilities, and visual memory. These abilities are essential for activities like reading maps or drawing.
- Intelligence: The Wechsler Adult Intelligence Scale (WAIS) and the Wechsler Intelligence Scale for Children (WISC) are frequently used to assess general cognitive ability, providing a benchmark for comparison with other cognitive abilities.
The interpretation of each test result is always considered within the context of the patient’s overall neuropsychological profile and clinical presentation. No single test provides a complete picture; it’s the integration of multiple measures that allows for a thorough and accurate assessment.
Q 8. How do you handle discrepancies between test results and clinical observations?
Discrepancies between test results and clinical observations are common in neuropsychology and require careful consideration. It’s crucial to avoid simply dismissing one in favor of the other. Instead, a thorough analysis is needed to understand the underlying reasons for the discrepancy.
- Consider the Test’s Limitations: Some tests may be sensitive to specific factors like fatigue, anxiety, or cultural background, which might not be apparent during clinical observation. For example, a patient might perform poorly on a timed visual-spatial task due to anxiety, not a true cognitive deficit. Clinical observation of their relaxed demeanor during other parts of the assessment would flag this potential confound.
- Explore Alternative Explanations: Is the discrepancy due to a genuine cognitive deficit or a secondary factor (e.g., medication side effects, malingering)? A patient reporting severe memory problems might score normally on memory tests if they’re intentionally underperforming. Observing their effort and consistency throughout the testing session is critical.
- Qualitative Data Integration: Qualitative data from the clinical interview and observation are invaluable. For instance, a patient’s self-report of difficulties with planning and organization might contradict relatively preserved executive function test scores. Integrating the qualitative data might reveal that their difficulties are primarily related to task initiation rather than planning itself.
- Further Investigation: In some cases, the discrepancy warrants further investigation, potentially involving additional testing or consultation with other specialists. For example, inconsistencies might point to a need for a more in-depth assessment of attention or a referral to a psychiatrist.
In the report, I clearly articulate the discrepancy, present all relevant data (both quantitative and qualitative), offer plausible explanations, and justify my final conclusions. Transparency is key; I aim to present a comprehensive and nuanced picture to aid in accurate diagnosis and treatment planning.
Q 9. How do you maintain patient confidentiality and adhere to ethical guidelines in report writing?
Maintaining patient confidentiality and adhering to ethical guidelines are paramount. My practice strictly follows the ethical principles outlined by professional organizations like the American Psychological Association (APA) and the National Academy of Neuropsychology (NAN).
- HIPAA Compliance: I ensure all reports and patient information are stored securely, following HIPAA regulations for electronic protected health information (ePHI). This includes password protection, secure servers, and adherence to data breach protocols.
- Informed Consent: Before testing, I obtain informed consent, clearly explaining the purpose of the assessment, the types of information gathered, how it will be used, and the limits of confidentiality.
- Confidentiality in Reporting: I avoid including unnecessary identifying information in reports. I use identifiers when sharing information with other healthcare professionals, such as initials rather than full names. I never disclose protected health information to unauthorized individuals.
- Ethical Considerations in Reporting: I carefully consider the language used and avoid making assumptions or value judgments about the patient’s behaviors or circumstances. I maintain objectivity in the interpretation of test results and avoid projecting my own personal biases into the report. For example, I will carefully interpret low scores in a way that is supportive and helpful.
Furthermore, I am well-versed in relevant laws and regulations governing the practice of neuropsychology within my jurisdiction, ensuring that all my actions align with ethical standards.
Q 10. Explain your process for formulating diagnostic impressions and recommendations.
Formulating diagnostic impressions and recommendations is a multi-step process that requires careful consideration of all available data.
- Data Integration: I begin by comprehensively reviewing all the collected data: test results, clinical observations, interview information, collateral information from family or caregivers, and any relevant medical history.
- Pattern Analysis: I analyze the pattern of strengths and weaknesses revealed by the assessment data, not just focusing on individual scores. This process looks for consistent patterns of performance across different measures. A consistent pattern of poor performance on visual-spatial tests across multiple measures is far more indicative of a specific deficit than an isolated low score on one test.
- Differential Diagnosis: Using my knowledge of neuropsychological literature and clinical experience, I develop a differential diagnosis, considering alternative explanations for the observed pattern. This considers possible cognitive deficits and other factors that could contribute to the patient’s presentation.
- Diagnostic Impression: Based on the data analysis and differential diagnosis, I formulate a diagnostic impression, which is a concise summary of the most likely explanation of the patient’s neuropsychological profile.
- Recommendations: Finally, I develop individualized recommendations for treatment, rehabilitation, or further assessment based on the diagnostic impression. This includes suggestions for specific interventions, referral to other professionals, and strategies for managing identified challenges. For instance, recommendations might involve cognitive remediation therapy, occupational therapy, or medication adjustments.
The entire process is iterative, with ongoing refinement as new information emerges or as the patient’s condition evolves.
Q 11. How do you ensure your reports are free of bias and culturally sensitive?
Ensuring reports are free of bias and culturally sensitive is critical for accurate and equitable care. I actively work to mitigate bias throughout the assessment and reporting process.
- Test Selection: I carefully select neuropsychological tests that are appropriate for the patient’s age, cultural background, and language proficiency. I am aware of potential cultural biases in tests and interpret results cautiously, considering how cultural factors might influence performance.
- Culturally Sensitive Interviewing: I conduct culturally sensitive interviews to understand the patient’s experiences, values, and perspectives, and I tailor the language and style of the interview to the patient’s comfort level.
- Awareness of Biases: I am constantly aware of my own biases and strive for objectivity in the interpretation of results. I am conscious of gender, racial, ethnic, and other biases that might influence test interpretation.
- Interpretation of Results: I avoid making generalizations or assumptions based on demographic factors. For example, I avoid attributing poor performance on a test solely to age or cultural background without considering other factors.
- Clear and Concise Language: I use clear and concise language in reports that is accessible to the patient and other stakeholders. I avoid jargon and technical terms unless absolutely necessary, providing explanations when used.
My reports clearly state any limitations of the assessment due to cultural or linguistic factors, and I actively seek consultation or supervision when needed to ensure culturally competent assessments and interpretations.
Q 12. Describe your experience writing reports for diverse populations (e.g., age, culture, language).
I have extensive experience working with diverse populations across various age groups, cultural backgrounds, and language proficiencies.
- Pediatric Neuropsychology: I’m proficient in adapting testing procedures and interpreting results for children and adolescents, understanding developmental norms and the impact of developmental disorders on cognitive functioning.
- Geriatric Neuropsychology: I’m experienced in assessing older adults, considering age-related changes in cognitive abilities and the impact of age-related illnesses or injuries. This involves using age-appropriate tests and adjusting administration procedures to accommodate physical limitations.
- Multilingual Patients: I have experience working with patients from various linguistic backgrounds and employ appropriate translation services or utilize tests available in multiple languages. I am aware of the challenges posed by linguistic differences and strive to accurately interpret test results while considering potential language barriers.
- Culturally Diverse Populations: I am adept at tailoring assessment procedures and interpreting results in ways that are sensitive to cultural differences and avoid biases in test interpretation. I use tools and resources that are developed and validated in relevant cultural contexts, when possible.
My experience has equipped me with the skills and sensitivity needed to provide comprehensive and equitable neuropsychological services to diverse populations, adapting my methods to best meet individual needs while adhering to high ethical and professional standards.
Q 13. What software or tools do you utilize for neuropsychological report writing?
I utilize a variety of software and tools to enhance efficiency and accuracy in neuropsychological report writing.
- Test Administration Software: Many neuropsychological tests are now administered via computer software. This software often provides immediate scoring and generates basic reports that can be imported into word processing documents. Examples include programs for administering the Weschler Adult Intelligence Scale (WAIS) or the Rey Auditory Verbal Learning Test (RAVLT).
- Word Processing Software: I utilize Microsoft Word for report generation, employing templates for consistent formatting and structure. Templates ensure consistency in organization, section headers, and style, saving time and enhancing readability.
- Database and Reporting Software: I use specialized software to manage patient data and generate initial reports with structured information from different assessments. This helps consolidate quantitative data, often including charting and graphing functionalities.
- Reference Management Software: I use reference management software (e.g., EndNote, Zotero) to manage and cite the neuropsychological literature I refer to in my reports.
My selection of software reflects a balance of functionality, user-friendliness, and compliance with data security and privacy regulations.
Q 14. How do you manage time constraints when writing neuropsychological reports?
Managing time constraints is a constant challenge in neuropsychological report writing. Efficient workflow and prioritization are essential.
- Templates and Standardized Formats: I use standardized report templates to expedite the writing process. These templates provide a structured framework, allowing me to focus on the content rather than formatting.
- Prioritization and Time Allocation: I allocate specific time blocks for each phase of the report writing process, including data analysis, interpretation, writing, and editing. Prioritizing tasks, focusing on the most important sections first, is crucial for effective time management.
- Dictation and Transcription: For sections of the report that involve extensive descriptive writing, I often utilize dictation software. This allows me to focus on the content while simultaneously completing other tasks.
- Efficient Data Management: Efficient software and data management practices are important for minimizing the time spent searching for and compiling data.
- Delegation: In some cases, I delegate tasks like data entry or transcription to trained assistants, freeing up more time for the more complex aspects of report writing and interpretation.
While accuracy and thoroughness are non-negotiable, I strive to develop efficient systems to manage time constraints without compromising the quality of the reports.
Q 15. How do you deal with challenging or complex cases in report writing?
Challenging cases, such as those with atypical presentations or comorbid conditions, require a systematic approach. I begin by meticulously reviewing all available data, including the referral question, medical history, and test results. This detailed review helps me identify the core issues and formulate hypotheses. Then, I systematically analyze the data, looking for patterns and inconsistencies. This might involve comparing performance across different cognitive domains or comparing results to normative data. If there’s uncertainty about an interpretation, I consult relevant literature and, if necessary, seek consultation from colleagues. I also prioritize clear and transparent language in the report to fully explain complex findings and potential limitations. For example, if a patient shows inconsistent performance across memory tests, I’d explain this variability in the report, exploring possible contributing factors like fatigue or medication side effects, rather than simply reporting the discrepancies.
Consider a case with a patient exhibiting memory problems but also showing significant mood disturbances. A simple diagnosis would be insufficient. Instead, I would explore the interplay between potential cognitive deficits and mood disorder, meticulously detailing the assessment results supporting these considerations and acknowledging the limitations in definitively separating the contributions of each. The report would clearly outline the clinical presentation, assessment findings, differential diagnoses, and recommendations tailored to this complex clinical picture. This approach ensures the report is not only accurate but also actionable for the referring physician and patient.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure the readability and comprehensibility of your reports?
Readability is paramount. I use clear, concise language, avoiding jargon whenever possible. I structure my reports logically, using headings and subheadings to guide the reader through the key information. I employ active voice and short, declarative sentences to enhance understanding. I always prioritize the referral question, ensuring that the report directly addresses it. Before submitting the report, I conduct a thorough review, often reading it aloud to catch awkward phrasing or unclear sentences. Think of it like writing a story – you want the reader to follow the narrative easily and understand the conclusions. I also carefully consider the audience – the report for a physician will differ from one intended for a family member, adjusting the complexity of the language accordingly.
For instance, instead of writing, ‘The patient demonstrated significant deficits in verbal fluency,’ I might write, ‘The patient struggled to name words quickly, suggesting a potential problem with language processing.’ The second example is more accessible and avoids the potentially confusing term ‘verbal fluency.’ Moreover, I consistently use tables and graphs to present complex data efficiently, making it easier to digest the information at a glance.
Q 17. What are some common errors to avoid in neuropsychological report writing?
Common errors include overinterpretation of data, insufficient explanation of findings, and neglecting to address the referral question. Overinterpretation might involve drawing conclusions based on a single test score rather than the overall pattern of performance. Insufficient explanation means failing to provide enough context for the results, making it difficult for the reader to understand their significance. Neglecting the referral question renders the report irrelevant and unhelpful.
Other common errors include making unqualified statements, using jargon without clear definitions, or not properly referencing normative data. For example, saying ‘The patient is clearly suffering from Alzheimer’s disease’ based solely on memory test scores is an overinterpretation that ignores other potential causes. A more cautious approach would acknowledge the memory deficits but also discuss other possibilities and limitations of the findings. It’s crucial to maintain objectivity and present data in a balanced manner.
Q 18. Describe your experience in using different report templates and formats.
Throughout my career, I’ve used various templates and formats, adapting my approach based on the specific needs of the referral source and the complexity of the case. Some templates are highly structured, providing specific sections for demographic information, test results, qualitative observations, and interpretations. Others are more flexible, allowing for greater customization. I am proficient in using both. I am also adept at using electronic health record (EHR) systems to integrate my reports seamlessly into patient records. My experience includes using standardized formats preferred by specific institutions or healthcare systems, adapting to their requirements to ensure efficient integration into their workflows.
Choosing a template depends on several factors: the specific needs of the referring physician or agency, the type of assessment conducted, and the patient’s individual circumstances. For instance, a concise template might suffice for a straightforward case, while a more detailed template may be necessary for a complex case requiring extensive analysis. Flexibility is key. I can adapt to various formats without sacrificing the clarity and comprehensiveness of the report.
Q 19. How do you stay updated with the latest research and best practices in neuropsychological assessment?
Staying current in neuropsychology requires continuous professional development. I regularly attend conferences, workshops, and webinars to learn about new assessment techniques and research findings. I subscribe to relevant journals such as the Journal of the International Neuropsychological Society and the Archives of Clinical Neuropsychology, reviewing research articles that impact assessment practices and interpretation. I also actively participate in continuing education programs offered by professional organizations like the American Academy of Clinical Neuropsychology (AACN).
Moreover, I maintain professional memberships to receive updates on best practices and guidelines. This ensures that my reports reflect the most up-to-date scientific knowledge and adhere to current ethical standards. Staying current is not just about reading journals; it’s about critical evaluation of new research to assess its relevance to clinical practice. I actively engage in peer review and discussions to ensure my understanding reflects the newest consensus in the field.
Q 20. Explain your process for reviewing and revising your reports before submission.
My review process involves multiple stages. First, I review the report for accuracy and consistency. I check for any discrepancies between the data and interpretations. Then, I evaluate the clarity and flow of the report, ensuring it is well-organized and easy to read. I look for potential biases in my interpretations and ensure that I’ve addressed all relevant information. After this self-review, I take a break from the report before returning for a final review with a fresh perspective. This second review often helps to identify areas that need further clarification or refinement.
Finally, I often ask a colleague or supervisor to review the report, particularly for complex cases. This independent review helps to identify any potential oversights or areas for improvement. I view this feedback as a crucial part of the process, aiming for continuous improvement in my report writing. This multi-step approach ensures that the report is accurate, clear, and meets the highest professional standards before submission.
Q 21. How do you handle feedback from supervisors or colleagues on your report writing?
Feedback is essential for professional growth. I welcome constructive criticism from supervisors and colleagues. I actively listen to their comments, seeking to understand their perspectives. I don’t take criticism personally, instead viewing it as an opportunity to learn and improve my skills. If there’s a disagreement on interpretation, I engage in a thoughtful discussion, revisiting the data and literature to clarify any misunderstandings. I always document the feedback received and any revisions made in response.
I often integrate the feedback by revising the report to address the concerns raised. For example, if a supervisor suggests that I could strengthen a particular section by providing more detailed information, I will diligently address this in the revised report. I believe that through thoughtful consideration of feedback, I can consistently enhance the quality and accuracy of my reports. Constructive feedback is invaluable and ensures the highest level of professionalism and accuracy in my work.
Q 22. Describe your experience with different types of report delivery methods.
My experience encompasses a variety of report delivery methods, tailored to the specific needs of the referral source and the patient’s situation. This includes traditional hard-copy reports mailed directly to referring physicians or therapists. I also frequently utilize secure electronic health record (EHR) portals for delivery, ensuring HIPAA compliance and efficient communication. Increasingly, I’m utilizing secure file-sharing platforms to transmit reports to clients and their authorized representatives, offering convenient access and improving overall communication flow. For instance, I’ve found that using a secure portal significantly reduces the time it takes for a referring physician to receive and review a report, leading to faster intervention for the patient.
In cases requiring a more immediate response, such as urgent situations, I’ve utilized phone consultations to offer preliminary feedback, followed by a formal written report. This approach enables immediate action while maintaining the comprehensive detail of a full report. The method of delivery is always determined after careful consideration of the patient’s circumstances, the urgency of the findings, and the preferences of the referring party.
Q 23. What are some common challenges you face in neuropsychological report writing, and how do you address them?
One common challenge is balancing conciseness with comprehensiveness. Neuropsychological reports contain substantial data, and distilling that into a clear, accessible narrative can be time-consuming. I address this through careful organization, using clear headings and subheadings, and employing visual aids like graphs or tables to summarize complex data effectively. Another challenge is managing the emotional impact of the findings on the patient and their family. I strive for empathy and sensitivity in my writing, avoiding jargon and presenting information in a supportive way.
A further challenge is ensuring the report remains unbiased and objective, especially in complex or emotionally charged cases. To address this, I carefully review my writing to ensure my language avoids subjective inferences, using data-driven conclusions. I consistently employ a structured approach, following a standardized template to minimize bias and ensure thoroughness.
Q 24. How do you collaborate with other healthcare professionals when writing reports?
Collaboration is crucial. I regularly communicate with referring physicians, therapists, and other healthcare professionals involved in the patient’s care. This often involves pre-report consultations to discuss the patient’s presentation and treatment goals. After the report is completed, I proactively reach out to discuss my findings and recommendations, clarifying any questions or concerns. This collaborative approach enables a more holistic and effective treatment plan for the patient.
For instance, I recently collaborated with a psychiatrist on a case involving a patient with traumatic brain injury. I shared my neuropsychological findings, and he integrated those with his psychiatric observations, resulting in a more targeted and comprehensive treatment strategy. The exchange of information ensures everyone is working towards the same goals for the patient.
Q 25. How do you ensure your reports are legally compliant?
Legal compliance is paramount. I strictly adhere to HIPAA regulations regarding patient privacy and confidentiality. All reports are maintained in secure, password-protected electronic databases. My reports avoid subjective or speculative language, focusing on objective data and scientifically supported conclusions. I carefully consider the legal implications of any findings, ensuring the language used is clear and unambiguous to prevent misinterpretations. This includes using appropriate terminology and avoiding any potentially misleading statements.
Moreover, I am always mindful of the potential use of the report in legal proceedings and maintain meticulous documentation of my assessment procedures. This ensures that the report is defensible and meets the highest standards of professional and legal practice.
Q 26. Describe your experience with using technology to enhance the efficiency of neuropsychological report writing.
Technology plays a significant role in my workflow. I utilize dedicated neuropsychological assessment software packages for test administration, scoring, and report generation. These programs significantly enhance efficiency, reducing the time spent on manual scoring and report writing. Furthermore, secure electronic data storage protects patient data and simplifies record keeping. I also use electronic communication tools for efficient collaboration with other healthcare professionals.
For example, the software I utilize automatically generates graphs and tables summarizing test results, saving me valuable time and improving the clarity of the reports. These technologies allow me to allocate more time to the crucial aspects of the assessment and patient interaction.
Q 27. How do you balance the need for brevity with the need for thoroughness in your reports?
Balancing brevity and thoroughness is a constant challenge. I address this through a structured, organized approach. I start with a concise summary of the key findings upfront, followed by a detailed explanation of the assessment procedures and results. I use clear, straightforward language, avoiding technical jargon when possible. I also employ visual aids such as graphs and tables to summarize complex data effectively, enabling readers to grasp the essential information quickly.
I often utilize a hierarchical approach, presenting the most pertinent information first and then providing more detailed analyses as needed. This ensures that the report is easily accessible to both specialists and non-specialists, and avoids overwhelming the reader with unnecessary detail. The goal is to ensure the report is both comprehensive and easily digestible.
Q 28. What are your strengths and weaknesses in neuropsychological report writing?
My strengths include my strong organizational skills and ability to communicate complex information clearly and concisely. I’m proficient in using technology to enhance efficiency and maintain meticulous documentation. I also pride myself on my empathetic approach, ensuring reports are written in a way that is both informative and supportive to the patient and their family.
An area for ongoing development is further refining my skills in integrating qualitative data, such as observational notes, into the quantitative findings more seamlessly. While I am proficient in this area, continuous improvement is always a priority in this ever-evolving field. I’m currently focusing on incorporating more advanced statistical analyses to better interpret and present nuanced data.
Key Topics to Learn for Neuropsychological Report Writing Interview
- Understanding the Purpose and Audience: Mastering the art of tailoring your report to the specific needs and understanding of the intended reader (e.g., physician, attorney, educator).
- Organizing Information Effectively: Developing a clear and logical structure that facilitates easy comprehension of complex neuropsychological findings. This includes mastering techniques for presenting data concisely and efficiently.
- Interpreting Test Results Accurately: Demonstrating a strong understanding of various neuropsychological tests and their clinical implications. This involves accurately interpreting scores within the context of the individual’s background and presenting the interpretation in a manner that is both clear and clinically relevant.
- Formulating Diagnostic Impressions: Formulating well-supported and defensible diagnostic statements based on the integrated findings from the neuropsychological assessment. This requires a solid grasp of relevant diagnostic criteria and the ability to justify conclusions with appropriate evidence.
- Writing Style and Clarity: Crafting reports that are concise, grammatically correct, and free from jargon. Prioritizing clarity and readability for diverse audiences is crucial.
- Ethical Considerations: Understanding and adhering to ethical guidelines in neuropsychological assessment and report writing, including issues of confidentiality, informed consent, and cultural sensitivity.
- Practical Application: Case Studies: Analyze and discuss example case studies, focusing on how different findings are integrated and interpreted to form a coherent narrative in the final report.
- Problem-Solving and Critical Thinking: Developing the ability to identify and address discrepancies in test data, formulating alternative hypotheses, and articulating the rationale behind conclusions.
- Legal and Forensic Applications (if applicable): Understanding the specific requirements and considerations for report writing in forensic contexts, if the job requires it.
Next Steps
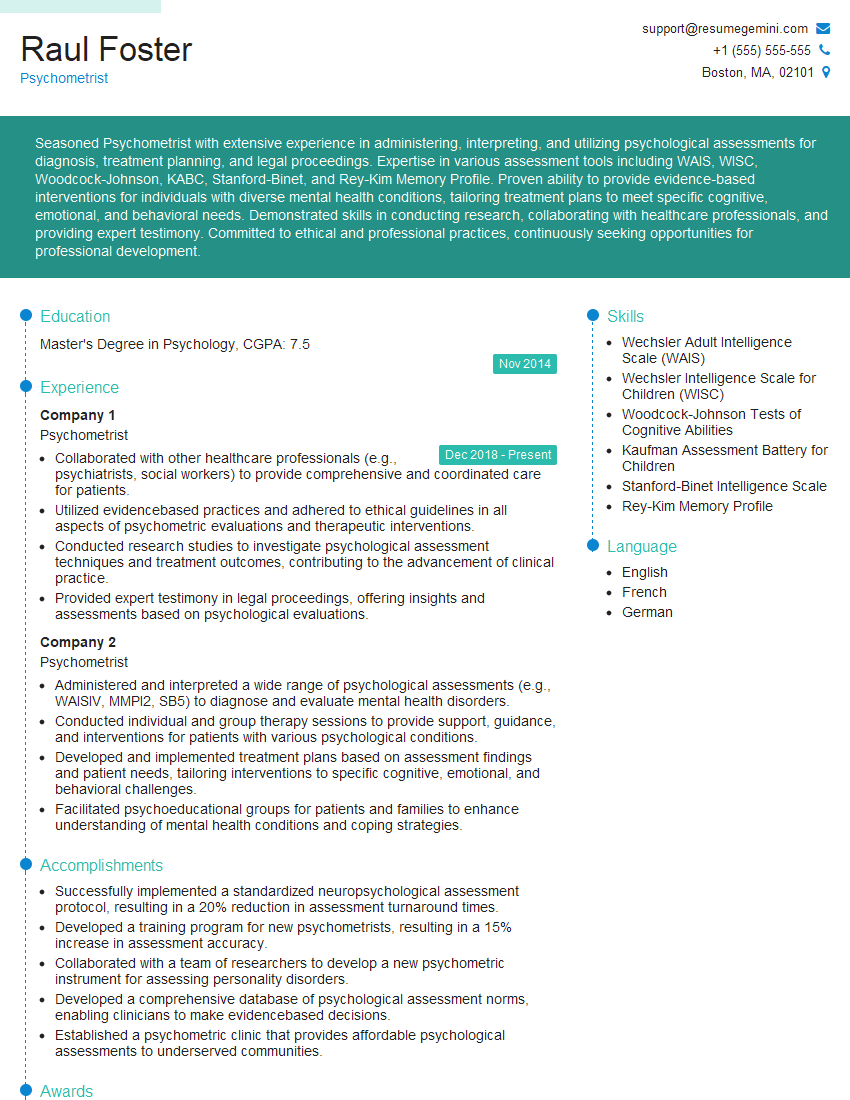
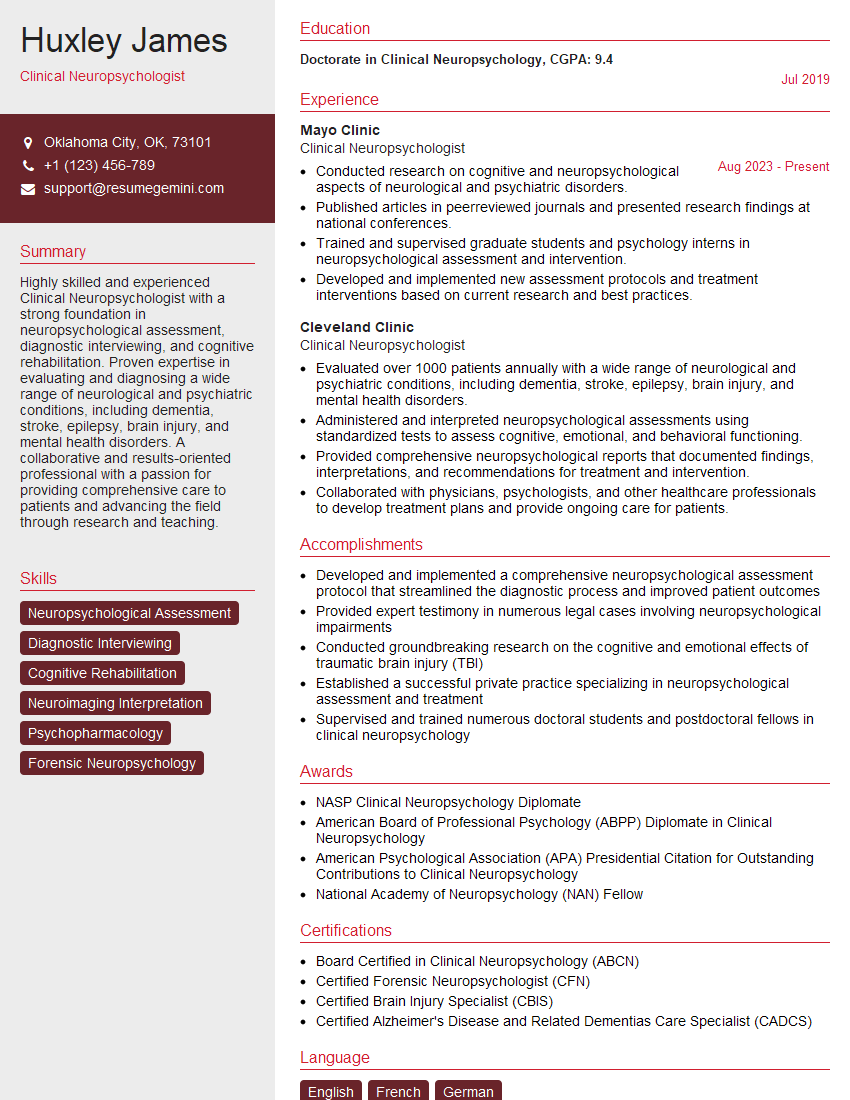
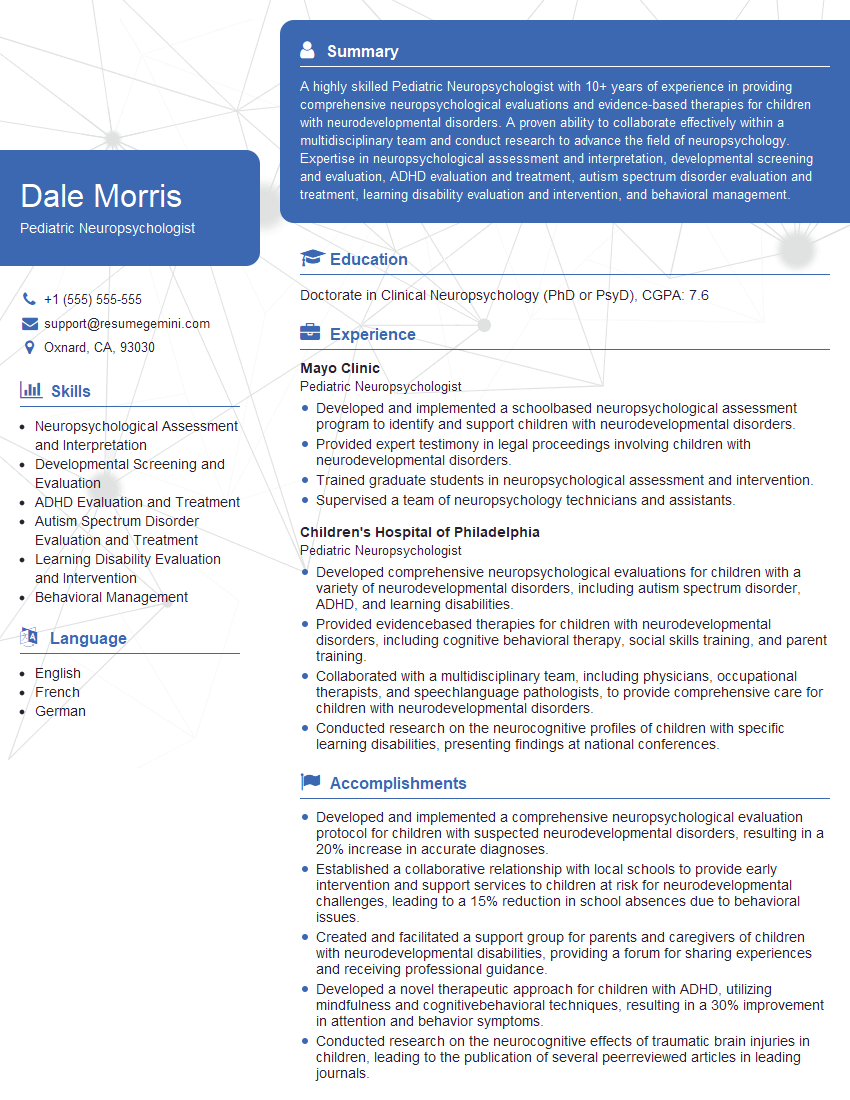
Mastering neuropsychological report writing is crucial for career advancement in this field. It demonstrates competence, professionalism, and a deep understanding of the clinical process. To significantly improve your job prospects, it’s essential to present your skills effectively. Creating an ATS-friendly resume is key to getting noticed by recruiters and hiring managers. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to highlight your neuropsychological report writing expertise. Examples of resumes specifically designed for neuropsychological report writing professionals are available through ResumeGemini, providing you with valuable templates and inspiration for crafting your own.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.