The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Non-Invasive Ventilation (NIV) interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Non-Invasive Ventilation (NIV) Interview
Q 1. What are the indications for Non-Invasive Ventilation (NIV)?
Non-invasive ventilation (NIV) is used to support breathing without the need for an endotracheal tube or tracheostomy. Its indications are diverse and depend heavily on the underlying respiratory pathology and the patient’s clinical status. Generally, NIV is indicated when a patient is experiencing acute respiratory failure and requires ventilatory support but is not yet requiring intubation. Key indications include:
- Acute exacerbations of chronic obstructive pulmonary disease (COPD): NIV is often the first-line treatment to prevent intubation in COPD patients experiencing acute exacerbations characterized by increased dyspnea, tachypnea, and elevated CO2 levels.
- Cardiogenic pulmonary edema: NIV can help reduce pulmonary congestion and improve oxygenation in patients with heart failure leading to fluid buildup in the lungs.
- Pneumonia: In selected patients with severe pneumonia and respiratory distress, NIV can improve oxygenation and reduce the need for invasive ventilation.
- Acute respiratory distress syndrome (ARDS) (early stages): In certain cases, NIV can be attempted early in the course of ARDS to avoid intubation, though this is highly dependent on individual patient characteristics and severity.
- Obstructive sleep apnea (OSA): Continuous positive airway pressure (CPAP) is a form of NIV commonly used for treating OSA.
The decision to initiate NIV is made on a case-by-case basis, considering the severity of respiratory failure, the patient’s overall condition, and the presence of contraindications.
Q 2. What are the contraindications for NIV?
Contraindications to NIV are situations where the benefits of NIV are likely outweighed by the risks. These can be broadly categorized into:
- Hemodynamic instability: Patients with severe hypotension or arrhythmias may not tolerate the increased intrathoracic pressure associated with NIV.
- Apnea or severe central hypoventilation: NIV is not effective in patients who are unable to initiate spontaneous breaths.
- Inability to cooperate or protect the airway: NIV requires patient cooperation to maintain a good mask seal and protect the airway from aspiration. Patients who are agitated, uncooperative, or at high risk of aspiration are not suitable candidates.
- Facial trauma or severe deformities: These can make it difficult or impossible to obtain an adequate mask seal.
- Profuse vomiting or excessive secretions: The risk of aspiration is significantly increased in these patients.
- Recent upper gastrointestinal surgery: Increased risk of aspiration.
- Severe respiratory acidosis with low pH: In cases of severe respiratory acidosis, NIV might not be sufficient to correct the imbalance quickly enough.
Careful assessment of the patient’s condition is crucial before initiating NIV to ensure the absence of contraindications and to optimize the chances of success.
Q 3. Describe different modes of NIV delivery (e.g., CPAP, BiPAP, SIPPV).
Several modes of NIV delivery exist, each offering different levels of respiratory support. The most common are:
- CPAP (Continuous Positive Airway Pressure): This mode delivers a constant positive pressure throughout the entire respiratory cycle, preventing airway collapse and improving oxygenation. Think of it like gently inflating a balloon – keeping the airways open.
- BiPAP (Bilevel Positive Airway Pressure): This mode delivers two different levels of pressure: an inspiratory positive airway pressure (IPAP) and an expiratory positive airway pressure (EPAP). IPAP assists inspiration, while EPAP provides a lower level of pressure during expiration, preventing airway collapse. It’s like providing extra assistance with each breath while still allowing for natural exhalation.
- SIPPV (Synchronized Intermittent Mandatory Ventilation): This mode combines elements of both CPAP/BiPAP and conventional mechanical ventilation. It delivers breaths at a set rate and volume, synchronized with the patient’s spontaneous breaths. This offers more control over ventilation but is still non-invasive.
The choice of mode depends on the patient’s respiratory needs and response to therapy. For example, CPAP might suffice for mild hypoxemia, while BiPAP may be needed for patients with more severe respiratory distress. SIPPV is usually reserved for patients who are unable to maintain adequate ventilation on their own.
Q 4. Explain the physiological effects of CPAP and BiPAP.
Both CPAP and BiPAP exert their physiological effects primarily by improving lung mechanics and gas exchange.
- CPAP: By applying continuous positive pressure, CPAP prevents airway collapse during both inspiration and expiration, increasing functional residual capacity (FRC) – the amount of air left in the lungs after exhalation. This increased FRC improves oxygenation and reduces work of breathing. Think of it as keeping the airways propped open, allowing for easier breathing.
- BiPAP: BiPAP builds on CPAP’s effects. The higher inspiratory pressure (IPAP) assists the patient’s inspiratory efforts, further reducing the work of breathing. The lower expiratory pressure (EPAP) still prevents airway collapse, maintains FRC, and helps to reduce the feeling of breathlessness. It provides a more tailored and powerful support during inspiration.
Both modes can improve oxygenation (PaO2) and reduce carbon dioxide retention (PaCO2), ultimately improving respiratory function and reducing the need for invasive ventilation.
Q 5. How do you assess the effectiveness of NIV?
Assessing the effectiveness of NIV involves a combination of clinical assessment and objective measurements. We look for improvements in:
- Respiratory rate: A decrease in respiratory rate indicates reduced respiratory effort.
- Oxygen saturation (SpO2): An increase in SpO2 indicates improved oxygenation.
- Heart rate: A decrease in heart rate often reflects reduced respiratory distress.
- Blood gas analysis: Arterial blood gas measurements (PaO2, PaCO2, pH) provide objective data on gas exchange and acid-base balance. Improvements in these values indicate effective NIV.
- Clinical improvement: Assessing the patient’s subjective experience of dyspnea (shortness of breath) is crucial. A reduction in breathlessness and improved comfort are important indicators of success.
- Work of breathing: Observe for reduction in use of accessory muscles and improved ease of breathing.
Regular monitoring and reassessment are essential to ensure the NIV is effective and to adjust settings as needed. Failure to show improvement might necessitate a switch to invasive mechanical ventilation.
Q 6. What are the common complications associated with NIV?
Several complications can arise during NIV, including:
- Skin breakdown: Pressure from the mask can cause skin irritation or breakdown, especially on the bridge of the nose, cheeks, and behind the ears. Regular skin checks and the use of appropriate padding are essential for prevention.
- Claustrophobia and anxiety: The mask can induce anxiety and claustrophobia in some patients, requiring careful patient education and the use of sedation if necessary.
- Aspiration pneumonia: If the patient vomits or has excessive secretions, aspiration into the lungs can occur. This risk is higher in patients with impaired swallowing reflexes.
- Gastric distension: Air can enter the stomach during NIV, causing bloating and discomfort. Strategies like using different mask interfaces and ensuring proper patient positioning can help to minimize this.
- Dry mouth and eyes: The air delivered by the ventilator can be dry, leading to discomfort. Humidification can help alleviate this problem.
- Pneumomediastinum or pneumothorax: In rare cases, high airway pressures can cause air to leak into the mediastinum or pleural space.
Careful monitoring and proactive measures can help minimize the risk and severity of these complications.
Q 7. How do you troubleshoot common NIV problems (e.g., leaks, patient discomfort)?
Troubleshooting NIV problems requires a systematic approach:
- Leaks: Leaks around the mask are common and reduce the effectiveness of NIV. Check for proper mask fit, seal integrity, and any facial hair interfering with the seal. Consider using different mask sizes or types, or adding padding. If the leak is substantial, re-assess mask fit and consider alternative ventilation strategies.
- Patient discomfort: Address patient concerns about claustrophobia or skin irritation. Explain the procedure thoroughly, use appropriate padding, and adjust the pressure settings as tolerated. Sedation might be necessary in cases of severe discomfort or agitation.
- Ineffective ventilation: If the NIV is not improving oxygenation or reducing respiratory distress, reassess the patient’s clinical status, blood gases, and ventilator settings. Check for any contraindications that may have developed. If improvement isn’t seen, consider escalation to invasive ventilation.
- Altered mental status: This could signify worsening respiratory distress or other complications. Re-evaluate the patient’s clinical status, check blood gases, and adjust NIV settings as needed. Consult the medical team to determine further management.
Effective troubleshooting involves careful assessment, systematic problem-solving, and close communication with the medical team to ensure optimal patient care.
Q 8. How do you select appropriate NIV settings for a patient?
Selecting appropriate NIV settings is a crucial step, requiring a careful assessment of the patient’s individual needs and respiratory status. It’s not a one-size-fits-all approach; it’s more like tailoring a suit. We consider several factors:
- Respiratory Drive and Work of Breathing: We assess the patient’s respiratory rate, tidal volume, and effort. A patient struggling significantly may need higher pressure support or increased flow.
- Blood Gas Analysis: Arterial blood gas (ABG) results provide vital information on oxygenation (PaO2) and carbon dioxide levels (PaCO2). These help determine the need for oxygen supplementation and the effectiveness of the current ventilation settings.
- Underlying Disease: The cause of respiratory failure, such as COPD, neuromuscular disease, or pneumonia, guides setting selection. For example, a patient with COPD might benefit from pressure support ventilation, while a patient with neuromuscular weakness might require volume-targeted ventilation.
- Patient Comfort and Tolerance: We start with conservative settings and gradually increase them while closely monitoring the patient’s response. Excessive pressures can lead to discomfort and potential complications like barotrauma (lung injury from excessive pressure). We aim for the lowest effective settings.
- Type of NIV: The choice between pressure support ventilation (PSV), volume-assured pressure support (VAPS), or bilevel positive airway pressure (BiPAP) depends on the patient’s individual needs and response.
Example: A patient with acute exacerbation of COPD might initially be set to BiPAP with an IPAP (inspiratory positive airway pressure) of 15 cm H2O and an EPAP (expiratory positive airway pressure) of 5 cm H2O and an oxygen flow to maintain SpO2 above 90%. We would then closely monitor their response, adjusting settings as needed.
Q 9. Describe the process of weaning a patient from NIV.
Weaning from NIV is a gradual process aimed at restoring the patient’s spontaneous breathing ability. It requires careful monitoring and titration of settings. The goal is to reduce ventilator support while ensuring adequate gas exchange and minimal respiratory distress. We typically follow these steps:
- Assessment: We assess the patient’s respiratory rate, tidal volume, oxygen saturation, and work of breathing. We also look for signs of respiratory fatigue.
- Gradual Reduction of Support: We start by gradually decreasing the pressure support level or the pressure difference between IPAP and EPAP in BiPAP, allowing the patient to take over more of the work of breathing.
- Trial Periods: We conduct short trials of reduced support, typically for 1-2 hours, observing for any signs of respiratory distress. We monitor their respiratory rate, oxygen saturation, and heart rate.
- Titration: Based on the trial, we adjust the settings further, continuing the weaning process as tolerated.
- Frequent Monitoring: Close monitoring of vital signs, respiratory effort, and blood gases is crucial throughout the weaning process.
- Extubation: Once the patient consistently maintains adequate gas exchange and respiratory effort with minimal support, we proceed with extubation (removal of the NIV device).
Example: If a patient is on BiPAP with IPAP 12 and EPAP 4, we might decrease the IPAP to 10, observe for an hour, and then further reduce it based on the response. If the patient experiences respiratory distress, we would temporarily stop the weaning process and revert to the previous settings.
Q 10. What are the key parameters to monitor during NIV?
Monitoring during NIV is crucial to ensure patient safety and treatment effectiveness. Key parameters include:
- Respiratory Rate and Pattern: Changes in respiratory rate and rhythm can indicate respiratory distress or deterioration.
- Oxygen Saturation (SpO2): Monitoring oxygen levels helps assess the effectiveness of oxygen therapy and the overall respiratory status.
- Heart Rate: Changes in heart rate can reflect the patient’s response to NIV or potential complications.
- Blood Pressure: Blood pressure monitoring helps identify potential cardiovascular effects of NIV.
- Respiratory Effort: We assess the patient’s effort and use of accessory muscles. Increased effort may signify insufficient ventilation.
- Arterial Blood Gases (ABGs): ABGs provide detailed information on oxygenation and carbon dioxide levels, crucial for adjusting settings.
- Ventilator Settings: Monitoring the pressure, volume, flow, and other NIV settings ensures they are delivering effective ventilation.
- Patient Comfort and Tolerance: Regularly assess patient comfort, noting any signs of discomfort, such as skin irritation or air leaks.
Continuous monitoring through pulse oximetry and regular ABG analysis are usually part of the routine.
Q 11. How do you manage patient discomfort during NIV?
Managing patient discomfort during NIV involves a multi-pronged approach focusing on addressing both physical and psychological aspects:
- Mask Fit and Interface: Proper mask selection and fitting are essential to prevent skin breakdown, pressure sores, and air leaks. Regular checks and adjustments are important.
- Pressure Settings: High pressures can cause discomfort and potential complications. Optimizing pressure settings while maintaining adequate ventilation is key.
- Humidification: Adding humidification helps prevent drying of the nasal passages and mouth, improving comfort.
- Pain Management: If the patient has underlying pain, adequate analgesia may improve comfort and tolerance of NIV.
- Mouth Care: Regular mouth care helps maintain oral hygiene and reduces the risk of infection.
- Positioning: Proper positioning can improve patient comfort and reduce pressure points. Experimenting with different positions can help find what works best for individual patients.
- Communication and Reassurance: Open communication with the patient is critical. Addressing their concerns and providing reassurance can significantly improve their experience.
Example: If a patient complains of a stuffy nose, we might try a different mask type or add humidification. If pressure sores develop, we may need to adjust the mask fit or add padding.
Q 12. How do you address patient anxiety related to NIV?
Addressing patient anxiety related to NIV requires a compassionate and empathetic approach. Many patients are apprehensive about the mask, the equipment, and the potential for claustrophobia. Strategies include:
- Education and Explanation: Thoroughly explain the purpose and function of NIV, emphasizing its benefits in improving breathing and overall well-being. Use clear, simple language, avoiding technical jargon.
- Demonstration and Practice: Allowing patients to practice using the mask and becoming familiar with the equipment before initiating therapy can reduce anxiety.
- Relaxation Techniques: Teaching relaxation techniques, such as deep breathing exercises or mindfulness, can help patients manage anxiety.
- Medication: In some cases, mild anxiolytics may be necessary to reduce anxiety, especially in severely anxious patients.
- Support System: Encourage family involvement and support to ease the patient’s anxieties.
- Positive Reinforcement: Positive reinforcement and encouragement, celebrating milestones like successful weaning attempts, boost confidence and reduce anxiety.
Example: Demonstrating the mask’s ease of removal and the ability to pause therapy briefly for breaks can alleviate claustrophobia. Explaining that the NIV helps reduce breathlessness can increase confidence and acceptance.
Q 13. Explain the importance of patient education regarding NIV.
Patient education regarding NIV is paramount for successful therapy and improved outcomes. Educated patients are better able to participate actively in their care and manage their condition. Key aspects of patient education include:
- Purpose of NIV: Explain clearly why NIV is needed and how it will improve their breathing.
- How NIV Works: Describe the function of the machine and the mask in simple terms.
- Mask Use and Care: Explain how to use the mask properly, how to clean it, and when to seek help for problems.
- Troubleshooting: Educate patients on common problems such as air leaks and how to address them or seek assistance.
- Medication and Other Therapies: Explain how NIV interacts with other medications or therapies.
- Expected Outcomes: Discuss realistic expectations for improvement and potential side effects.
- Weaning Process: Explain the weaning process and what patients can expect.
- Emergency Contacts: Provide contact information for healthcare providers in case of emergency.
Example: Providing written materials, videos, or interactive sessions tailored to the patient’s literacy level and understanding can aid in effective education. Encouraging questions and open communication promotes a collaborative approach.
Q 14. How do you determine the appropriate mask size and type for a patient?
Determining the appropriate mask size and type is crucial for effective and comfortable NIV. An ill-fitting mask can lead to air leaks, skin breakdown, and patient discomfort. The selection process involves:
- Patient Assessment: Assess the patient’s facial features, size, and any underlying conditions like facial deformities or skin sensitivities.
- Mask Type Selection: Several mask types exist, including nasal masks, full-face masks, and oronasal masks. The choice depends on patient tolerance, the type of NIV being used, and the presence of nasal congestion or mouth breathing.
- Mask Sizing: Use a measuring tape to determine the appropriate mask size based on the manufacturer’s guidelines. An appropriate fit is snug but not excessively tight.
- Trial and Adjustment: Allow the patient to try several mask sizes and types to determine the best fit and comfort. Adjustments can be made to achieve a snug seal without causing discomfort.
- Leakage Assessment: After fitting, assess for air leaks by observing for air escaping around the mask edges. Minor leaks can be addressed with adjustments; significant leaks require a different mask size or type.
Example: A patient with facial hair might require a full-face mask or a nasal mask with a specially designed seal. A patient with nasal congestion might benefit from an oronasal mask. Careful attention to size and fit is essential in every case.
Q 15. What are the differences between different NIV interfaces (masks, helmets)?
Non-invasive ventilation (NIV) interfaces are crucial for delivering respiratory support without the need for endotracheal intubation. The primary interfaces are masks and helmets, each with its own set of advantages and disadvantages.
- Masks: These are the most common NIV interfaces, offering varying levels of coverage.
- Nasal masks: Cover only the nose, offering good patient comfort but potentially leading to nasal dryness or irritation. They are suitable for patients with mild to moderate respiratory distress.
- Oral masks: Cover the mouth and nose, offering better ventilation than nasal masks but potentially causing mouth dryness, discomfort and pressure sores.
- Full face masks: Cover the entire mouth and nose, providing the best seal and highest level of ventilation, but can be less comfortable and claustrophobic for some patients.
- Helmets: These enclose the entire head, creating a sealed environment for ventilation. They are often preferred for patients with facial trauma or who find masks uncomfortable. Helmets offer excellent ventilation but can be more challenging to fit and clean and might feel more claustrophobic for some.
The choice of interface depends on factors such as the patient’s condition, comfort level, and the severity of respiratory compromise. For instance, a patient with mild COPD exacerbation might tolerate a nasal mask, while a patient with severe acute respiratory distress syndrome (ARDS) might require a full face mask or helmet for optimal ventilation.
Career Expert Tips:
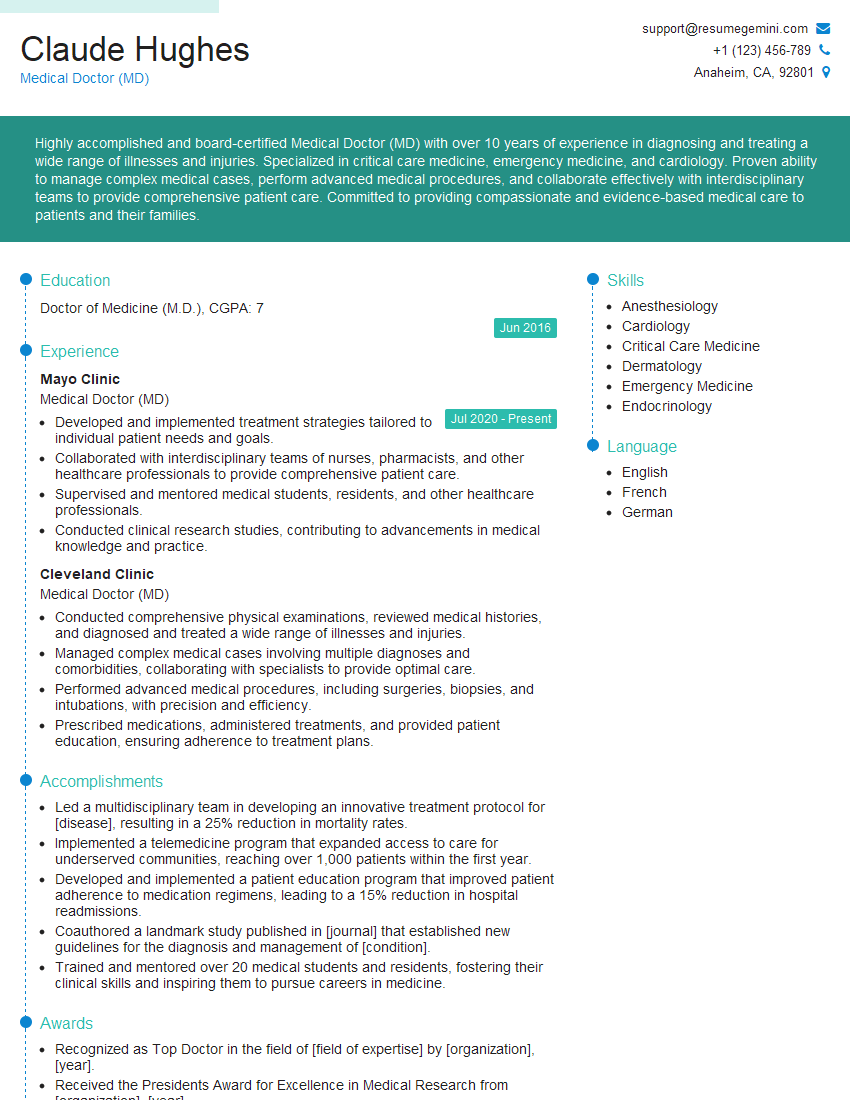
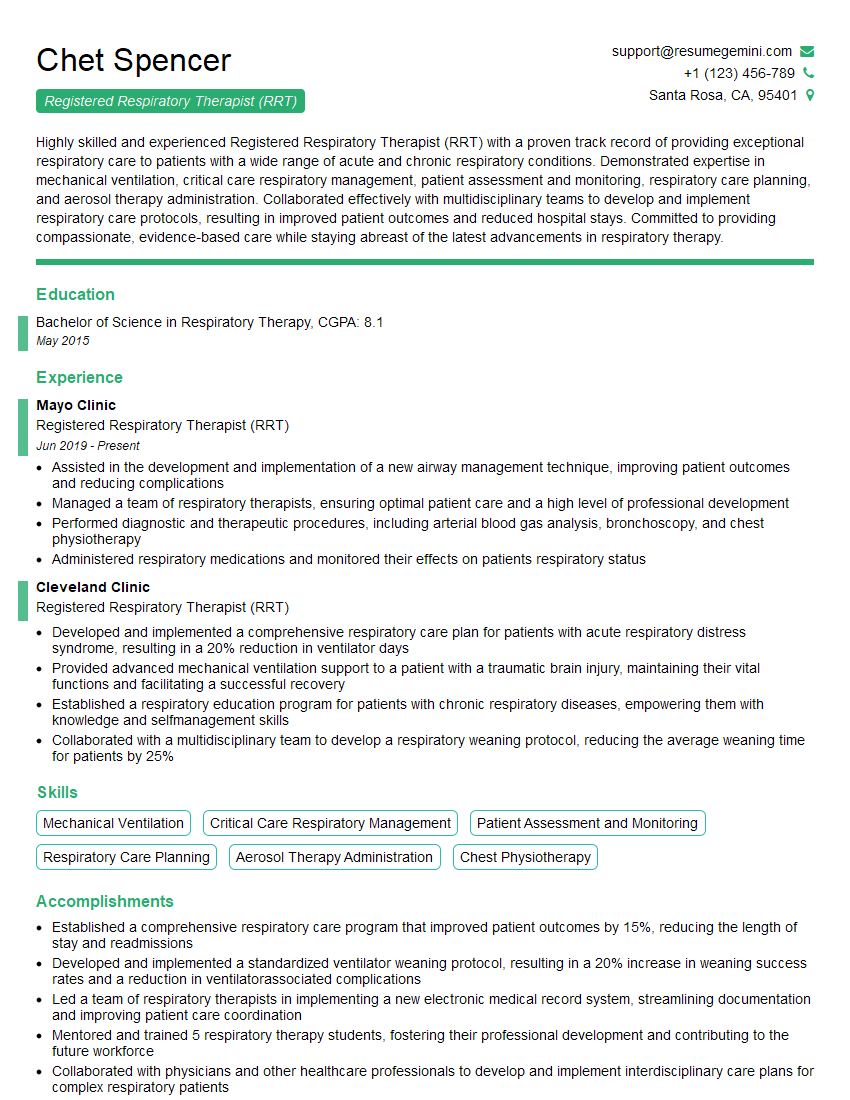
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the role of NIV in the management of acute respiratory failure.
In acute respiratory failure, NIV plays a vital role as a non-invasive alternative to endotracheal intubation and invasive mechanical ventilation (IMV). It helps to improve oxygenation and ventilation, reducing the workload on the respiratory muscles. NIV is often considered the first-line treatment for patients with hypercapnic respiratory failure (elevated carbon dioxide levels) and, in selected cases, for hypoxemic respiratory failure (low blood oxygen levels).
The key is early intervention. By providing respiratory support early on, NIV can potentially prevent the need for IMV, reducing complications associated with intubation, like ventilator-associated pneumonia (VAP) and prolonged ICU stays. However, it is crucial to carefully select patients based on factors like their level of consciousness, ability to cooperate, and the severity of respiratory distress. Patients who do not respond to NIV within a specific timeframe may require escalation to invasive mechanical ventilation.
Q 17. Describe the role of NIV in the management of chronic obstructive pulmonary disease (COPD).
In chronic obstructive pulmonary disease (COPD), NIV is used primarily during acute exacerbations, characterized by worsening shortness of breath and increased respiratory distress. It can significantly improve dyspnea (shortness of breath), reduce hospital length of stay, and decrease mortality rates in select patients. NIV achieves this by reducing the work of breathing, improving ventilation, and improving oxygenation.
NIV may also be used in specific COPD patients for long-term home ventilation in cases of severe hypoxemia (low blood oxygen levels) or hypercapnia (high carbon dioxide levels). This can dramatically improve their quality of life, allowing them more independence and mobility. However, it requires careful patient selection and education. Long-term NIV success depends on the patient’s commitment to adherence to therapy and regular follow-up.
Q 18. How does NIV compare to invasive mechanical ventilation?
NIV and invasive mechanical ventilation (IMV) both aim to support respiration, but they differ significantly in their delivery method and implications. IMV requires endotracheal intubation – a procedure where a tube is inserted into the airway to deliver ventilation. This is an invasive procedure carrying risks of infection, trauma, and discomfort.
NIV, on the other hand, delivers respiratory support through a mask or helmet without intubation, making it less invasive and better tolerated by many patients. While NIV can effectively manage many cases of respiratory failure, its efficacy is limited by patient cooperation and tolerance. If NIV fails to improve respiratory parameters or if a patient’s condition deteriorates rapidly, then IMV is usually necessary.
In essence, NIV is a valuable first-line approach, offering a less invasive alternative to IMV, but IMV remains essential for patients who don’t respond to NIV or require more aggressive respiratory support.
Q 19. What are the advantages and disadvantages of NIV?
NIV offers several advantages, including its non-invasive nature, reducing the risk of complications associated with intubation, such as infection and trauma. It generally allows for greater patient comfort and mobility compared to IMV. NIV can be used in various settings, including hospital wards, and even at home with appropriate training.
However, NIV also has limitations. Not all patients can tolerate NIV due to factors like claustrophobia, agitation, or inability to cooperate. It may be less effective in patients with severe respiratory failure or those requiring high levels of ventilatory support. Failure to improve respiratory parameters despite NIV necessitates a timely transition to IMV. The efficacy of NIV also depends on proper patient selection, mask fit, and ongoing monitoring of respiratory parameters.
Q 20. How do you assess patient tolerance to NIV?
Assessing patient tolerance to NIV involves a multifaceted approach, focusing on both physiological and subjective measures. Physiological parameters include monitoring respiratory rate, heart rate, blood pressure, oxygen saturation (SpO2), and arterial blood gas levels to ensure that ventilation and oxygenation are improving or at least stable. We look for signs of respiratory distress like increased work of breathing, use of accessory muscles, and altered mental status.
Subjective assessment is just as crucial. We regularly ask patients about their comfort levels, including any feelings of claustrophobia, discomfort, dryness, or skin irritation. We observe for signs of anxiety, agitation, or restlessness. Regular communication with the patient and adjusting settings as needed are crucial for achieving good tolerance. Poor tolerance may necessitate changing the NIV interface, adjusting pressure settings, or switching to alternative therapies including IMV.
Q 21. What are the different types of NIV devices available?
A variety of NIV devices are available, differing primarily in their ventilation modes and pressure delivery systems. These include:
- Volume-cycled NIV: Delivers a preset tidal volume (amount of air per breath). Less commonly used than pressure-cycled systems.
- Pressure-cycled NIV: Delivers a preset pressure for a set time, allowing for a more natural breathing pattern. This is the most common type.
- Pressure support ventilation (PSV): Augments the patient’s own breaths by providing pressure assistance during inspiration.
- Continuous positive airway pressure (CPAP): Delivers a constant positive pressure throughout the respiratory cycle, improving oxygenation.
- Bi-level positive airway pressure (BiPAP): Delivers different pressures during inspiration and expiration, enhancing both ventilation and oxygenation.
The choice of device and ventilation mode depends on the patient’s individual needs and respiratory status. For example, CPAP might be sufficient for patients with mild hypoxemia, while BiPAP or pressure support may be necessary for those with more severe respiratory impairment. The selection should be guided by clinical judgment and careful monitoring of respiratory parameters.
Q 22. What are the maintenance requirements for NIV equipment?
Maintaining NIV equipment involves a multi-faceted approach focusing on both the ventilator and the interface. Regular cleaning and disinfection are paramount. The specific procedures vary depending on the manufacturer’s instructions, but generally involve wiping down the ventilator’s exterior with a suitable disinfectant, and replacing filters as per the schedule (often monthly or as indicated by pressure drop indicators). The tubing and mask/interface require even more meticulous attention. This typically involves daily cleaning with appropriate disinfectants (following manufacturer recommendations) and regular replacement of components like the tubing (frequency varies depending on the type of tubing and patient condition, ranging from daily to weekly). Proper documentation of all maintenance activities is crucial for tracking and ensuring compliance.
For example, a common cleaning protocol involves wiping down the ventilator exterior with a 70% isopropyl alcohol solution, and daily replacement of the NIV circuit for patients with heavy secretions. Regular inspection for cracks, leaks, or damage on the ventilator housing and tubing is also critical to prevent malfunctions and ensure safe and effective operation.
Q 23. How do you ensure proper hygiene and infection control with NIV equipment?
Hygiene and infection control are paramount in NIV, as the close-proximity nature of the equipment increases risk. A crucial first step is meticulous hand hygiene by all personnel before and after handling the equipment or the patient. The NIV circuit itself needs rigorous attention. Daily replacement of the circuit is often the best practice in high-risk situations or for patients with high secretion loads, significantly minimizing the risk of ventilator-associated pneumonia (VAP). If single-use components are not feasible, the circuit should be cleaned and disinfected thoroughly after each use according to manufacturer instructions, often using a suitable enzymatic detergent and a subsequent disinfection with a solution like hydrogen peroxide. The mask interface requires individualised cleaning according to the material; reusable masks need to be meticulously cleaned and sterilized following specific guidelines to maintain hygiene and prevent transmission of microorganisms.
We always emphasize that proper training of healthcare personnel in these procedures is essential. A dedicated infection control protocol specific to our NIV procedures, incorporating all aspects from hand hygiene to appropriate disinfection methods, is vital.
Q 24. Explain the importance of regular NIV circuit checks.
Regular NIV circuit checks are crucial for both patient safety and effective ventilation. These checks detect potential issues before they escalate, preventing complications. Routine checks should include visually inspecting the circuit for kinks, leaks, or disconnections. Checking the connection points to the ventilator and mask is very important. The pressure settings on the ventilator should be verified against the prescribed settings. Auditory assessment—listening for leaks or unusual sounds within the circuit—is also a critical component. Any detected leak can significantly compromise ventilation efficiency and lead to patient distress. Furthermore, regular monitoring of the ventilator’s alarms and pressure readings is essential. Any deviations from normal values, such as abnormally high pressures, could indicate a problem requiring immediate attention.
For instance, a kink in the tubing can restrict airflow, leading to inadequate ventilation. Similarly, a leak might necessitate a circuit replacement to maintain the correct pressure and flow for the patient.
Q 25. How do you manage a patient experiencing respiratory distress despite NIV?
Respiratory distress despite NIV indicates treatment failure and requires immediate action. First, we assess the patient thoroughly—checking vital signs, respiratory rate, oxygen saturation, and work of breathing. We then systematically investigate potential causes: a leak in the system, incorrect ventilator settings, an inadequate mask fit, patient-related factors like secretions, or worsening underlying disease. Addressing these potential causes is prioritized. If a leak is present, the circuit is inspected and replaced if necessary. Ventilator settings may need adjustments, guided by the patient’s response. If secretions are the issue, suctioning may be required. However, if the distress persists despite these measures, immediate escalation of care is necessary, including considering intubation and mechanical ventilation. Close monitoring and frequent reassessment of the patient’s status are crucial during this process.
For example, I recently managed a patient experiencing respiratory distress despite NIV. Initial assessment revealed a significant leak in the system. Once replaced, the patient’s condition improved dramatically. But sometimes, escalation to invasive ventilation becomes necessary.
Q 26. How do you differentiate between NIV failure and worsening underlying disease?
Differentiating between NIV failure and worsening underlying disease can be challenging but is crucial for appropriate management. NIV failure is typically manifested by persistent respiratory distress despite optimal settings and troubleshooting. The patient may show signs of increased work of breathing, worsening oxygenation, and elevated respiratory rates. Worsening underlying disease, on the other hand, might present similarly initially, but a careful review of clinical presentation and diagnostic tools helps distinguish. We look for trends and consider factors like the patient’s overall condition, changes in blood gas analysis, and chest imaging. If there is no improvement despite appropriate settings and troubleshooting, or if there are clear signs of disease progression, it might point towards disease worsening. Careful patient assessment and regular monitoring are crucial to make this determination.
For instance, a patient with COPD on NIV might experience worsening dyspnea due to a superimposed infection, rather than NIV failure per se. Chest X-ray might then reveal the presence of pneumonia, explaining the deteriorating condition.
Q 27. Describe your experience with NIV in specific patient populations (e.g., neuromuscular disease, obesity hypoventilation syndrome).
I have extensive experience with NIV across diverse patient populations. In patients with neuromuscular diseases, such as amyotrophic lateral sclerosis (ALS) and muscular dystrophy, NIV plays a crucial role in maintaining respiratory function and preventing respiratory failure. These patients often benefit from long-term NIV use and require careful monitoring and individualized settings to address their specific needs. We often involve multidisciplinary teams, including respiratory therapists, neurologists, and nurses, for optimal management.
In patients with obesity hypoventilation syndrome (OHS), NIV helps improve ventilation and oxygenation. These patients often require individualized pressure support settings to address their specific needs. Weight management and other lifestyle modifications are often incorporated into the overall care plan to improve long-term outcomes. Success in these cases often depends on patient adherence to therapy and addressing the underlying sleep apnea component.
Q 28. What are the latest advancements in NIV technology?
Recent advancements in NIV technology focus on improving patient comfort, efficacy, and ease of use. Auto-adjusting NIV systems offer improved patient-ventilator synchrony and reduce the risk of adverse events. More sophisticated algorithms allow for personalized ventilation, and newer interfaces, like heated humidifiers, and advanced masks, minimize skin irritation and improve patient tolerance. Advancements in monitoring capabilities allow for remote monitoring of patient data, enabling timely interventions and improving patient outcomes. There is also growing research on non-invasive ventilation interfaces that are designed to minimize the side effects that often impede their tolerance and effectiveness such as facial skin breakdown or claustrophobia.
For example, the development of non-invasive ventilation devices with integrated sensors that continuously measure patient parameters and automatically adjust ventilation settings as needed represents a significant leap forward in improving the overall effectiveness and safety of NIV therapy.
Key Topics to Learn for Non-Invasive Ventilation (NIV) Interview
- Physiological Principles of NIV: Understand the mechanics of breathing, gas exchange, and how NIV supports these processes. Consider the differences between various modes of NIV.
- NIV Modes and Settings: Become proficient in explaining different NIV modes (e.g., pressure support ventilation, volume assist control) and their appropriate applications based on patient physiology and clinical presentations. Understand how to adjust settings based on patient response.
- Patient Selection and Assessment: Master the criteria for selecting appropriate candidates for NIV. Practice explaining how you would assess a patient’s suitability, including their respiratory status, hemodynamics, and overall clinical picture.
- Complications and Management: Be prepared to discuss common complications associated with NIV (e.g., air leaks, skin breakdown, patient discomfort) and how to effectively manage and mitigate these issues. Showcase your problem-solving skills.
- Monitoring and Weaning Strategies: Explain how you would monitor patients receiving NIV, focusing on key indicators of efficacy and potential complications. Describe your approach to weaning patients from NIV safely and effectively.
- Equipment and Technology: Familiarize yourself with the different types of NIV equipment, their functionalities, and troubleshooting common technical issues. Understand the importance of proper equipment maintenance and safety protocols.
- Ethical Considerations: Be prepared to discuss the ethical implications of NIV, including patient autonomy, shared decision-making, and end-of-life care when appropriate.
Next Steps
Mastering Non-Invasive Ventilation is crucial for career advancement in respiratory care. A strong understanding of NIV principles and practical applications will significantly improve your interview performance and open doors to exciting opportunities. To maximize your chances, create a compelling and ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource for building professional resumes that stand out. They offer examples of resumes tailored specifically to Non-Invasive Ventilation (NIV) roles to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.