Cracking a skill-specific interview, like one for Oophorectomy, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Oophorectomy Interview
Q 1. Describe the different types of oophorectomy procedures.
Oophorectomy, the surgical removal of one or both ovaries, can be performed in several ways, depending on the reason for the surgery and the patient’s individual circumstances. The primary distinction lies in the surgical approach:
- Unilateral oophorectomy: Removal of only one ovary.
- Bilateral oophorectomy: Removal of both ovaries. This is often done concurrently with a hysterectomy (removal of the uterus).
- Salpingo-oophorectomy: Removal of both the ovary and the fallopian tube on one or both sides. This is a common procedure, particularly when dealing with conditions affecting both structures.
The surgical approach itself can also vary:
- Laparotomy: A larger incision in the abdomen. This approach is typically used when there is a need for more extensive surgery or if there’s difficulty visualizing structures with minimally invasive techniques.
- Laparoscopy: A minimally invasive procedure using small incisions and specialized instruments. This is generally preferred due to smaller scars, less pain, and faster recovery times.
- Robotic-assisted laparoscopy: Uses a robotic surgical system to enhance precision and dexterity during laparoscopic surgery, particularly beneficial in complex cases.
Choosing the right type of oophorectomy depends on a careful assessment of the patient’s medical history, the nature of the condition being addressed, and the surgeon’s expertise.
Q 2. Explain the indications for prophylactic oophorectomy.
Prophylactic oophorectomy, the removal of ovaries to prevent future disease, is primarily indicated in individuals with a significantly increased risk of ovarian cancer. This increased risk is often associated with:
- Strong family history of ovarian or breast cancer: A genetic predisposition, particularly mutations in BRCA1 and BRCA2 genes, significantly elevates the risk.
- Personal history of breast cancer: Women with breast cancer often have a heightened risk of developing ovarian cancer.
- High-risk genetic testing results: Positive results for specific gene mutations known to increase cancer risk.
The decision to undergo prophylactic oophorectomy is highly personal and requires careful discussion between the patient, her family, and a multidisciplinary team of healthcare professionals, including a genetic counselor and oncologist. It involves weighing the benefits of cancer prevention against the potential risks and side effects of surgery, such as premature menopause.
Q 3. What are the potential complications of an oophorectomy?
While oophorectomy is generally a safe procedure, several potential complications exist. These can include:
- Postoperative pain: This is common but usually manageable with medication.
- Infection: As with any surgery, there is a risk of infection at the incision site or internally.
- Bleeding: Excessive bleeding is rare but a possibility.
- Injury to surrounding organs: Damage to nearby structures like the bladder or bowel is a potential risk, though thankfully infrequent with experienced surgeons.
- Premature ovarian failure (if bilateral): This leads to immediate menopause, with associated symptoms like hot flashes, vaginal dryness, and mood changes.
- Thromboembolism: Blood clots can form in the legs or lungs, a serious, albeit rare, complication.
- Adhesions: Scar tissue can form and potentially cause problems later on.
The risk of these complications varies depending on factors like the patient’s overall health, the surgical technique used, and the surgeon’s experience.
Q 4. How do you manage postoperative pain after an oophorectomy?
Postoperative pain management after an oophorectomy is crucial for patient comfort and recovery. A multi-modal approach is generally employed, including:
- Analgesics: Pain relievers, such as opioids (in the short-term) and non-steroidal anti-inflammatory drugs (NSAIDs), are prescribed to manage pain.
- Regional anesthesia: Techniques like nerve blocks can provide effective pain relief for a longer duration.
- Non-pharmacological methods: Strategies such as ice packs, proper positioning, and regular movement can help manage pain and reduce inflammation.
Pain management is tailored to the individual patient’s needs and response to treatment. Regular assessment of pain levels and adjustment of the pain management plan are essential.
Q 5. Discuss the role of laparoscopy in oophorectomy.
Laparoscopy has revolutionized oophorectomy, offering significant advantages over traditional laparotomy. In laparoscopic oophorectomy, the surgeon makes several small incisions in the abdomen and inserts specialized instruments and a camera to perform the surgery. This minimally invasive approach results in:
- Smaller incisions and scars: Leading to improved cosmesis.
- Less pain and discomfort: Patients typically experience less postoperative pain and recover faster.
- Shorter hospital stay: Many patients can go home the same day or the day after surgery.
- Reduced risk of infection and complications: Smaller incisions reduce the risk of infection and other complications.
Laparoscopic oophorectomy is the preferred approach for most patients unless contraindications exist.
Q 6. What are the advantages and disadvantages of robotic-assisted oophorectomy?
Robotic-assisted laparoscopic oophorectomy utilizes a robotic surgical system to enhance the precision and dexterity of laparoscopic surgery. This offers several advantages:
- Enhanced visualization: The robotic system provides a high-definition, 3D view of the surgical field, improving the surgeon’s ability to see and manipulate tissues.
- Increased precision and dexterity: The robotic arms allow for finer movements and greater control than traditional laparoscopy.
- Minimally invasive approach: Still benefits from the minimally invasive nature of laparoscopy, with smaller incisions, less pain, and faster recovery.
However, there are also some disadvantages:
- Higher cost: Robotic surgery is more expensive than traditional laparoscopy.
- Longer operating time: The set-up and use of the robotic system can increase the duration of surgery.
- Specialized training required: Surgeons require specialized training to use the robotic system effectively.
The decision of whether to use robotic-assisted surgery depends on individual patient factors, the complexity of the case, and surgeon expertise. In many cases, conventional laparoscopy provides excellent results.
Q 7. How do you counsel patients regarding the risks and benefits of oophorectomy?
Counseling patients regarding oophorectomy is a crucial aspect of responsible medical practice. This process involves a thorough discussion of:
- Risks and benefits: The potential benefits of the procedure (e.g., cancer prevention, treatment of certain conditions) need to be carefully weighed against the potential risks (e.g., premature menopause, surgical complications).
- Alternatives: Other treatment options should be explored and discussed, allowing the patient to make an informed choice.
- Long-term effects: The potential long-term consequences of oophorectomy, especially premature menopause and its impact on bone health, cardiovascular health, and overall well-being, need to be thoroughly explained.
- Hormone replacement therapy (HRT): The role of HRT in mitigating the effects of premature menopause should be addressed, including its benefits, risks, and suitability for individual patients.
- Emotional aspects: The psychological impact of oophorectomy, particularly the loss of fertility and the experience of early menopause, should be acknowledged and addressed with empathy and support.
This process requires clear communication, active listening, and patient empowerment to ensure the patient feels understood, informed, and confident in her decision.
For example, I would explain to a patient considering prophylactic oophorectomy due to a BRCA1 mutation that while it significantly reduces the risk of ovarian cancer, it also induces early menopause, which can significantly impact their life. We would discuss options like hormone replacement therapy and emotional support strategies to help them navigate this complex decision.
Q 8. Describe your experience with managing ovarian torsion pre-operatively.
Managing ovarian torsion pre-operatively centers on stabilizing the patient and preparing for surgery. It’s a surgical emergency because the twisted ovary compromises its blood supply, leading to ischemia and potentially necrosis. My approach begins with pain management – usually intravenous analgesics – and administering fluids to correct any dehydration. Imaging, typically a Doppler ultrasound, is crucial to confirm the diagnosis and assess the viability of the ovary. If the ultrasound shows compromised blood flow, immediate surgical intervention is necessary. Pre-operative counseling involves explaining the urgency of the situation and the potential need for oophorectomy (removal of the ovary) if the tissue is irreversibly damaged. In cases where the torsion isn’t complete or the ovary appears salvageable, untwisting the ovary during surgery (detorsion) is attempted. However, if the ovary is necrotic, oophorectomy is the only option to prevent further complications like infection or sepsis.
Q 9. Explain your approach to a patient presenting with suspected ovarian cancer requiring oophorectomy.
Suspected ovarian cancer requires a multidisciplinary approach. Initially, a detailed history and thorough physical examination are essential. This includes assessing for symptoms like abdominal bloating, pelvic pain, early satiety, and changes in bowel habits. Imaging studies, including transvaginal ultrasound and CT scans, are crucial for staging and assessing the extent of the disease. Biopsy is critical to confirm the diagnosis and determine the tumor’s histological type and grade. Once ovarian cancer is confirmed, the patient is referred to an oncology team for discussion of treatment options. The patient needs to be informed about all the possibilities in detail, including the risks and benefits of each surgery or alternative treatment option. Surgical intervention, usually including a total abdominal hysterectomy and bilateral salpingo-oophorectomy (removal of the uterus, fallopian tubes, and both ovaries), is typically part of the treatment strategy, but the approach is tailored to the individual patient and cancer stage. Post-operative management usually includes chemotherapy and other supportive therapies.
Q 10. How do you differentiate between benign and malignant ovarian masses pre-operatively?
Differentiating between benign and malignant ovarian masses pre-operatively is challenging, and often requires a combination of approaches. Ultrasound characteristics, such as size, solid versus cystic components, and presence of septations, provide initial clues. However, these features are not definitive. CA-125, a tumor marker, can be elevated in malignant cases, but it is not specific for ovarian cancer and can also be elevated in benign conditions. MRI can often provide more detailed information about the mass’s characteristics, including vascularity. The most reliable method is a biopsy, obtained either through laparoscopy or, less commonly, through an open surgical approach. A combination of imaging and biomarker analysis alongside the patient’s clinical history (age, family history, symptoms) are all considered in the preoperative decision-making process to assess the likelihood of malignancy.
Q 11. What are the key steps involved in performing a total abdominal oophorectomy?
A total abdominal oophorectomy involves the removal of both ovaries and the uterus. The key steps are: 1. Incision: A midline or Pfannenstiel incision is typically used, providing adequate exposure. 2. Uterine mobilization: The uterus is gently mobilized to gain access to the ovaries and fallopian tubes. 3. Ovarian ligation: The ovarian vessels are carefully identified and ligated (tied off) using clips or sutures to prevent hemorrhage. 4. Ovarian removal: Each ovary is dissected from its surrounding structures and removed. 5. Uterine removal: The uterus is removed after the ovaries and fallopian tubes are excised. 6. Hemostasis: Meticulous hemostasis (control of bleeding) is crucial throughout the procedure. 7. Closure: The abdominal wall is closed in layers. Postoperative pain management is crucial to ensure patient comfort and promote recovery.
Q 12. Describe your technique for performing a unilateral oophorectomy.
A unilateral oophorectomy involves the removal of only one ovary. The technique is similar to the steps involved in a total abdominal oophorectomy, but it focuses on only one ovary. The incision is typically smaller, allowing for minimally invasive surgery if feasible. The ovarian vessels are identified and carefully ligated using surgical clips or sutures. The ovary is then dissected from its attachments to the broad ligament and fallopian tube. The fallopian tube from that side is typically removed (salpingectomy) with the ovary. The remaining structures are inspected, and meticulous hemostasis is ensured before wound closure. The approach can be either through a laparotomy (open surgery) or laparoscopy (minimally invasive surgery), with laparoscopy being preferred whenever possible for its benefits of reduced pain, scarring, and hospital stay.
Q 13. How do you manage hemorrhage during an oophorectomy?
Hemorrhage during an oophorectomy is a serious complication that needs immediate attention. Prevention is key. Careful dissection and meticulous identification of the ovarian vessels before ligation are crucial. Using appropriate surgical techniques and instruments minimizes bleeding. Should hemorrhage occur, the initial step involves direct pressure on the bleeding site. Surgical clips and sutures are used to control bleeding from vessels. If bleeding persists despite these measures, electrocautery (heat to seal the vessels) may be used. In rare cases of uncontrollable bleeding, packing the area with gauze or other hemostatic agents may be necessary as a temporary measure while the surgeon assesses the situation and implements the best course of action. Severe cases may require a blood transfusion and more extensive surgical measures.
Q 14. What are the common postoperative complications and their management strategies?
Common postoperative complications after oophorectomy include:
- Infection: Prophylactic antibiotics are routinely used to reduce the risk, and any signs of infection are promptly treated with appropriate antibiotics.
- Hematoma formation: Close monitoring for signs of bleeding and pain is essential. If a hematoma develops, it may require surgical evacuation.
- Adhesions: These are fibrous bands that can form between organs and cause pain or bowel obstruction. Preventive measures include gentle surgical technique and minimizing tissue trauma. Adhesions sometimes require surgical intervention.
- Thromboembolic events (DVT, PE): Risk factors are assessed pre-operatively, and preventative measures such as early ambulation and anticoagulation are taken.
- Postoperative pain: Analgesics, including opioids and non-opioid medications, are used for pain control. Other strategies include nerve blocks or epidural analgesia.
Q 15. Discuss the role of imaging (e.g., ultrasound, MRI) in preoperative assessment for oophorectomy.
Preoperative imaging plays a crucial role in planning for oophorectomy. Ultrasound is often the initial imaging modality, providing a relatively inexpensive and readily available way to visualize the ovaries, assess their size and appearance, and detect any obvious masses or abnormalities. For example, ultrasound can help identify ovarian cysts or tumors, guiding the surgeon in their approach and potentially influencing the surgical technique chosen (e.g., laparoscopic versus open). MRI, on the other hand, offers superior soft tissue contrast and is particularly useful in characterizing complex ovarian masses, determining their extent, and identifying involvement of adjacent structures. This is particularly important when dealing with suspected malignancy. In cases of suspected malignancy, a CT scan may also be used to assess for metastatic disease. Ultimately, the choice of imaging modality depends on the clinical context and the specific concerns regarding the patient’s condition.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess a patient’s suitability for minimally invasive oophorectomy?
Assessing a patient’s suitability for minimally invasive oophorectomy (laparoscopic or robotic) involves a multifaceted evaluation. First, we thoroughly assess the patient’s overall health, considering factors such as age, comorbidities (like heart or lung disease), and body habitus. Secondly, we analyze the imaging findings, ruling out any contraindications such as severe adhesions (scar tissue) from prior surgeries, large ovarian masses that might compromise visualization or necessitate a larger incision, or involvement of surrounding organs. Thirdly, we discuss the patient’s preferences and expectations, ensuring they understand the benefits (smaller incisions, less pain, faster recovery) and potential limitations (difficulty accessing complex anatomical structures) of minimally invasive surgery. If the patient’s anatomy, medical history, and the findings on imaging are favorable, then minimally invasive oophorectomy is a viable option. If any of these factors point towards increased risk or technical difficulty, an open surgical approach may be more appropriate.
Q 17. What are the long-term effects of oophorectomy on a patient’s health?
Oophorectomy, the surgical removal of one or both ovaries, significantly impacts a woman’s hormone levels, especially estrogen and progesterone. This leads to several long-term effects, including the onset of surgical menopause, characterized by vasomotor symptoms (hot flashes, night sweats), sleep disturbances, vaginal dryness, and mood changes. The risk of osteoporosis and cardiovascular disease also increases. Furthermore, there’s evidence linking oophorectomy to an increased risk of cognitive decline and reduced bone density in the long-term. The severity of these effects varies depending on factors like age at surgery, whether one or both ovaries were removed, and the presence of other risk factors. For example, a younger woman undergoing bilateral oophorectomy will experience more severe menopausal symptoms compared to an older woman undergoing unilateral oophorectomy. Close monitoring and management strategies like hormone replacement therapy are critical for mitigating these long-term consequences.
Q 18. How do you counsel patients about hormone replacement therapy (HRT) after oophorectomy?
Counseling patients about hormone replacement therapy (HRT) after oophorectomy is a crucial aspect of patient care. I always begin by explaining the benefits of HRT in alleviating menopausal symptoms and reducing the long-term risks of osteoporosis and cardiovascular disease. However, I also openly discuss the potential risks and side effects of HRT, which can include increased risk of blood clots, stroke, and certain types of cancer, emphasizing the importance of individualized risk assessment. The decision to initiate HRT is always patient-centered and depends on their age, individual risk factors, symptom severity, and personal preferences. I present a balanced view, highlighting both the benefits and risks, allowing patients to make informed decisions about their care. For example, some patients might choose to manage symptoms with lifestyle modifications and alternative therapies initially, delaying or forgoing HRT altogether. This tailored approach is critical for building trust and ensuring patient satisfaction.
Q 19. Describe your experience with managing post-operative infections after oophorectomy.
Post-operative infections after oophorectomy, while relatively uncommon with proper surgical technique and aseptic precautions, are a serious concern. My approach involves strict adherence to sterile surgical techniques during the procedure, and careful attention to wound care in the post-operative period. Prophylactic antibiotics are often administered before and during surgery. Patients are closely monitored for signs of infection, such as fever, pain, redness, or swelling at the incision site. If an infection is suspected, prompt blood tests and cultures are performed to identify the causative organism and guide antibiotic therapy. In some cases, surgical drainage or debridement (removal of infected tissue) might be necessary. Early detection and aggressive management are critical to preventing serious complications, such as sepsis or abscess formation. For instance, a recent case highlighted the importance of regular wound assessments; a patient presented with subtle signs of infection early on and prompt antibiotic treatment prevented serious escalation.
Q 20. What are the indications for prophylactic salpingectomy with oophorectomy?
Prophylactic salpingectomy (removal of the fallopian tubes) along with oophorectomy is increasingly recommended, particularly in women with a family history of ovarian or breast cancer or those undergoing risk-reducing surgery. The rationale behind this is that the majority of ovarian cancers, particularly those of the fallopian tube, may originate in the fallopian tubes. By removing the fallopian tubes, the risk of developing these cancers is substantially reduced. This decision is made on a case-by-case basis, considering the patient’s individual risk factors, family history, and personal preferences. There’s ongoing debate regarding the extent of the benefits, but the current consensus is that the potential benefits of reducing ovarian cancer risk frequently outweigh the minimal additional risks associated with the removal of the fallopian tubes in the context of an oophorectomy.
Q 21. Discuss the role of genetic testing in the decision-making process for oophorectomy.
Genetic testing plays an increasingly important role in the decision-making process for oophorectomy, particularly in the context of risk-reducing surgery. Testing for mutations in genes like BRCA1 and BRCA2, known to significantly increase the risk of ovarian and breast cancer, can help identify women at high risk. If a woman tests positive for these mutations, she may be offered risk-reducing bilateral salpingo-oophorectomy (removal of both fallopian tubes and ovaries) to significantly reduce her lifetime risk of developing these cancers. Genetic counseling is crucial before and after testing to ensure patients understand their genetic risk, the implications of testing positive or negative, and the various options available to them, including prophylactic surgery. This is a complex decision, and providing comprehensive information ensures the patient makes an informed choice aligned with their values and preferences.
Q 22. How do you manage a patient who experiences early menopause after oophorectomy?
Managing early menopause after oophorectomy is crucial for patient well-being. Oophorectomy, the surgical removal of one or both ovaries, eliminates the primary source of estrogen production, leading to symptoms similar to natural menopause. These can include hot flashes, night sweats, vaginal dryness, mood swings, sleep disturbances, and decreased libido. Our approach is multifaceted and personalized.
- Hormone Replacement Therapy (HRT): This is often the first-line treatment, carefully considering the patient’s risk factors for cardiovascular disease, breast cancer, and other conditions. We discuss the benefits and risks thoroughly, tailoring the type and dosage of HRT to individual needs. For example, a patient with a strong family history of breast cancer might benefit from a lower dose of estrogen or a combination therapy including progesterone.
- Non-hormonal options: These are explored for patients who are not suitable candidates for HRT. These may include lifestyle modifications (regular exercise, healthy diet, stress management), over-the-counter treatments for vaginal dryness, and selective serotonin reuptake inhibitors (SSRIs) to manage mood swings and sleep disturbances.
- Regular monitoring: We schedule regular follow-up appointments to monitor the patient’s symptoms and adjust treatment as needed. This includes monitoring bone density to assess the risk of osteoporosis, a common consequence of estrogen deficiency.
For example, a 45-year-old patient experiencing severe hot flashes and insomnia after a bilateral oophorectomy might be started on a low-dose estrogen/progesterone HRT regimen. We would closely monitor her for any adverse effects and adjust the dosage accordingly. We also incorporate lifestyle advice, such as relaxation techniques for sleep improvement.
Q 23. Describe the differences in surgical approach between a bilateral and unilateral oophorectomy.
The surgical approach differs significantly between bilateral and unilateral oophorectomy. A unilateral oophorectomy involves the removal of only one ovary, while a bilateral oophorectomy removes both ovaries. The surgical technique itself – laparoscopic or abdominal – can be the same in both, but the extent of the surgery differs.
In a unilateral oophorectomy, the surgeon focuses on isolating and removing the affected ovary while preserving the other ovary, fallopian tube, and surrounding structures as much as possible. The incision size is smaller in laparoscopic procedures.
In contrast, a bilateral oophorectomy involves removing both ovaries and often both fallopian tubes (salpingo-oophorectomy). This requires a more extensive dissection and may involve larger incisions, depending on the surgical approach. This wider area of operation increases the risks associated with surgery.
For instance, a patient with a benign ovarian cyst on one ovary would undergo a unilateral oophorectomy, while a patient with a high risk of ovarian cancer might opt for a bilateral salpingo-oophorectomy as a preventative measure.
Q 24. What are the key differences in recovery between a laparoscopic and abdominal oophorectomy?
Recovery differs significantly between laparoscopic and abdominal oophorectomy. Laparoscopic oophorectomy uses small incisions and specialized instruments to perform the surgery. This minimally invasive approach typically results in less pain, shorter hospital stays (often outpatient), quicker recovery times, and smaller, less noticeable scars compared to abdominal surgery.
Abdominal oophorectomy involves a larger incision in the abdomen to access the ovaries. This more invasive approach generally results in more post-operative pain, a longer hospital stay, slower recovery, and larger, more visible scars. Patients can experience more significant discomfort and potentially require stronger pain medication.
For example, a patient undergoing a laparoscopic oophorectomy might experience minimal discomfort and return to normal activities within a week. In contrast, a patient undergoing an abdominal oophorectomy might experience significant pain, requiring stronger pain medications and a longer recovery period of several weeks.
Q 25. How do you handle unexpected findings during an oophorectomy?
Unexpected findings during an oophorectomy require careful assessment and prompt action. These findings can range from endometriosis to unsuspected ovarian masses (benign or malignant). Our approach involves:
- Immediate assessment: A thorough visual inspection and palpation are done to determine the nature of the finding. In the case of an unsuspected mass, frozen section biopsy might be performed for immediate histopathological evaluation.
- Surgical revision: Depending on the finding, the surgical procedure might be revised to address the unexpected issue. This might involve a more extensive resection or additional procedures such as lymph node sampling or staging laparotomy.
- Patient consultation: The patient is informed of the unexpected finding and the necessary changes to the surgical plan. We discuss the implications of the findings, including potential treatment options, and involve a multidisciplinary team (oncologist, pathologist) if needed.
- Post-operative management: Post-operative management is adjusted based on the unexpected findings. For example, if an unsuspected malignancy is discovered, further investigations and treatments like chemotherapy or radiation might be required.
Imagine finding an unexpected large ovarian cyst during a scheduled unilateral oophorectomy. After careful assessment to determine its nature, we might expand the procedure to include a complete oophorectomy (removal of the affected ovary) to prevent complications and potentially rule out malignancy. The patient would be informed of this change in the surgical plan and appropriate post-operative plans would be put in place.
Q 26. What is your approach to preventing surgical site infections after oophorectomy?
Preventing surgical site infections (SSIs) after oophorectomy is a top priority. Our strategy focuses on several key elements:
- Pre-operative measures: This includes a thorough patient history and physical exam to assess the risk factors for SSIs (diabetes, obesity, smoking). Patients are often prepped with chlorhexidine antiseptic washes to reduce skin flora.
- Surgical techniques: Maintaining sterile surgical fields, using appropriate surgical instruments, and minimizing tissue trauma during surgery contribute greatly to minimizing the risk of infection.
- Post-operative care: This involves timely removal of drains, meticulous wound care, and prompt administration of prophylactic antibiotics (based on patient’s risk factors and our clinical guidelines). We also closely monitor the wound for signs of infection.
- Patient education: We emphasize the importance of proper wound care to patients after discharge, providing detailed instructions on wound cleaning, dressing changes, and signs of infection.
For instance, we might use prophylactic antibiotics for patients with diabetes undergoing oophorectomy, as they are at increased risk for SSIs. Post-operatively, we would meticulously monitor the patient’s wound for any signs of redness, swelling, or drainage, and immediately address any concerns.
Q 27. Describe your experience with managing adhesion formation after oophorectomy.
Adhesion formation is a common complication after any abdominal or pelvic surgery, including oophorectomy. These adhesions are bands of scar tissue that can bind organs together, causing pain, bowel obstruction, and infertility. Our management focuses on prevention and treatment.
- Prevention: Minimally invasive techniques (laparoscopy) are preferred to reduce the risk of adhesions. Gentle tissue handling during surgery and the use of adhesion-barrier products are also important preventative measures.
- Treatment: If adhesions form and cause symptoms, treatment might involve laparoscopic adhesiolysis (surgical removal of adhesions) or medication to manage pain. In cases of severe bowel obstruction caused by adhesions, an open surgical intervention might be necessary.
For example, if a patient develops chronic pelvic pain after oophorectomy, we would investigate for the presence of adhesions. If confirmed, we might recommend laparoscopic adhesiolysis or pain management strategies. We would carefully explain the treatment options and their potential benefits and risks to the patient.
Q 28. Explain your approach to a patient experiencing significant post-operative pain.
Managing significant post-operative pain after oophorectomy is critical for patient comfort and recovery. Our approach is multi-modal and individualized.
- Analgesic regimen: We utilize a combination of medications, such as NSAIDs (nonsteroidal anti-inflammatory drugs) and opioids, to provide adequate pain relief. The choice of analgesics and dosage are tailored to the individual patient’s needs and risk profile.
- Non-pharmacological measures: We recommend non-pharmacological pain management strategies, including heat or ice packs, gentle stretching exercises, and relaxation techniques.
- Nerve blocks: In cases of severe or persistent pain, nerve blocks might be considered to provide targeted pain relief.
- Regular monitoring: We closely monitor the patient’s pain levels and adjust the pain management plan accordingly. We encourage open communication so patients can report any pain-related concerns.
If a patient reports severe pain despite receiving standard post-operative analgesics, we would investigate potential causes such as wound infection, adhesions, or nerve damage. We might consider stronger analgesics, nerve blocks, or further investigations to determine the underlying cause of the pain and provide effective treatment.
Key Topics to Learn for Oophorectomy Interview
- Types of Oophorectomy: Understand the differences between unilateral and bilateral oophorectomy, and their implications for patients.
- Indications for Oophorectomy: Master the medical reasons for performing an oophorectomy, including ovarian cancer, endometriosis, and other related conditions. Be prepared to discuss the decision-making process.
- Surgical Techniques: Familiarize yourself with various surgical approaches (e.g., laparoscopic, abdominal) and their advantages and disadvantages. Be ready to discuss pre-operative, intra-operative, and post-operative considerations.
- Post-Operative Management: Discuss potential complications and their management, including pain control, hormone replacement therapy (HRT), and monitoring for recurrence.
- Patient Counseling and Education: Understand the importance of patient education regarding the procedure, potential risks, and long-term consequences, such as hormonal changes and fertility implications.
- Ethical and Legal Considerations: Be prepared to discuss informed consent, patient autonomy, and potential ethical dilemmas related to oophorectomy.
- Case Studies and Problem Solving: Practice analyzing hypothetical scenarios involving patient presentation, diagnosis, treatment planning, and post-operative care. Focus on your problem-solving approach and decision-making skills.
- Relevant Anatomy and Physiology: Possess a strong understanding of the female reproductive system and its interaction with other bodily systems.
Next Steps
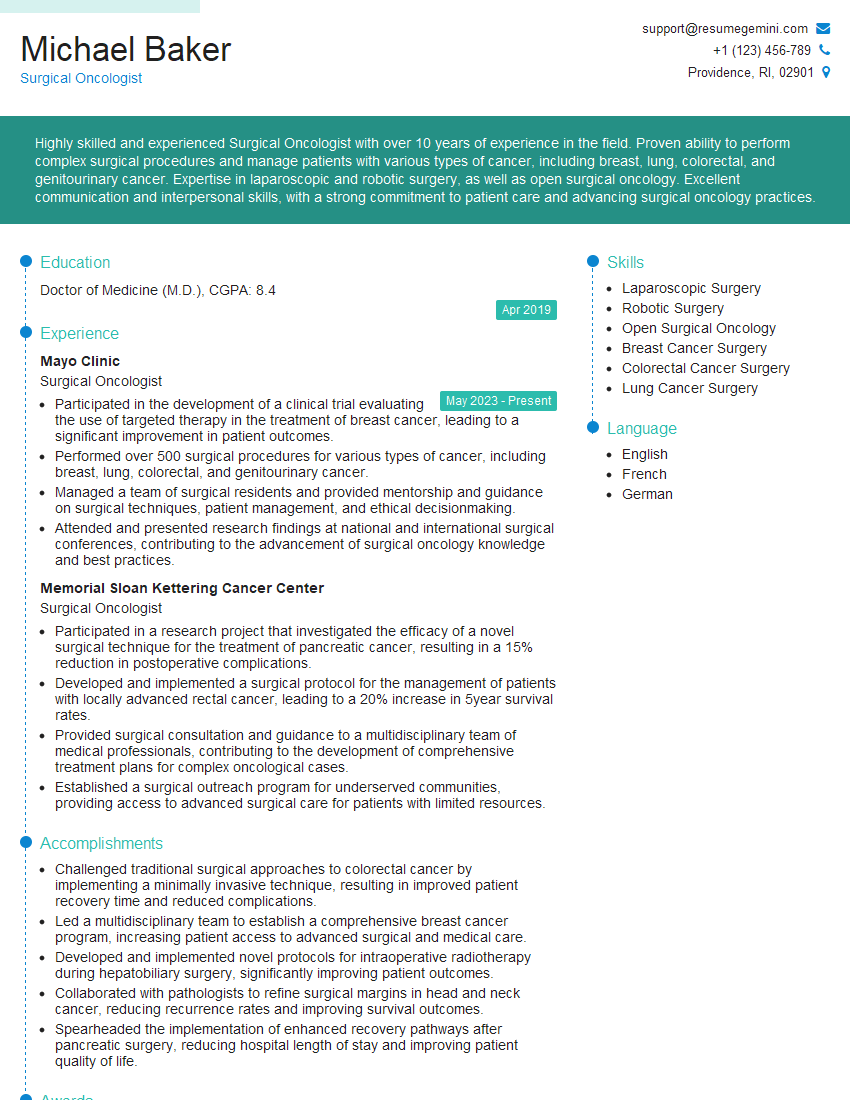
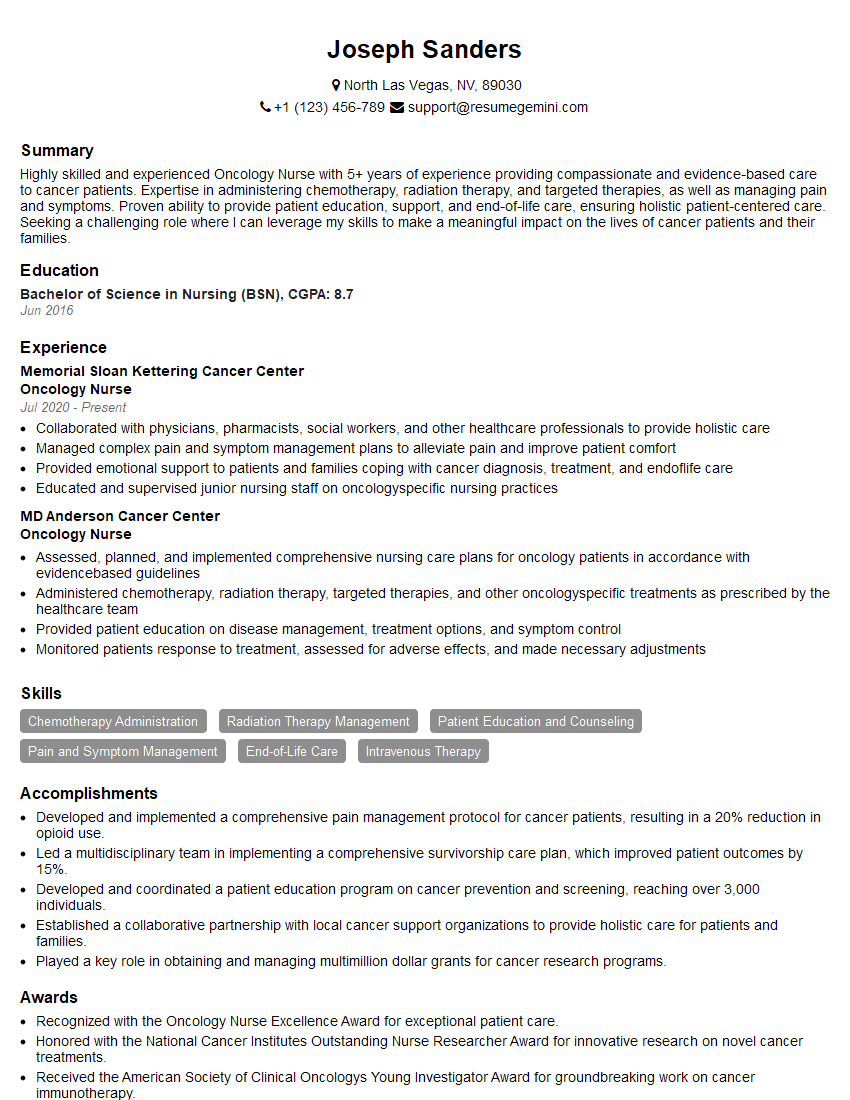
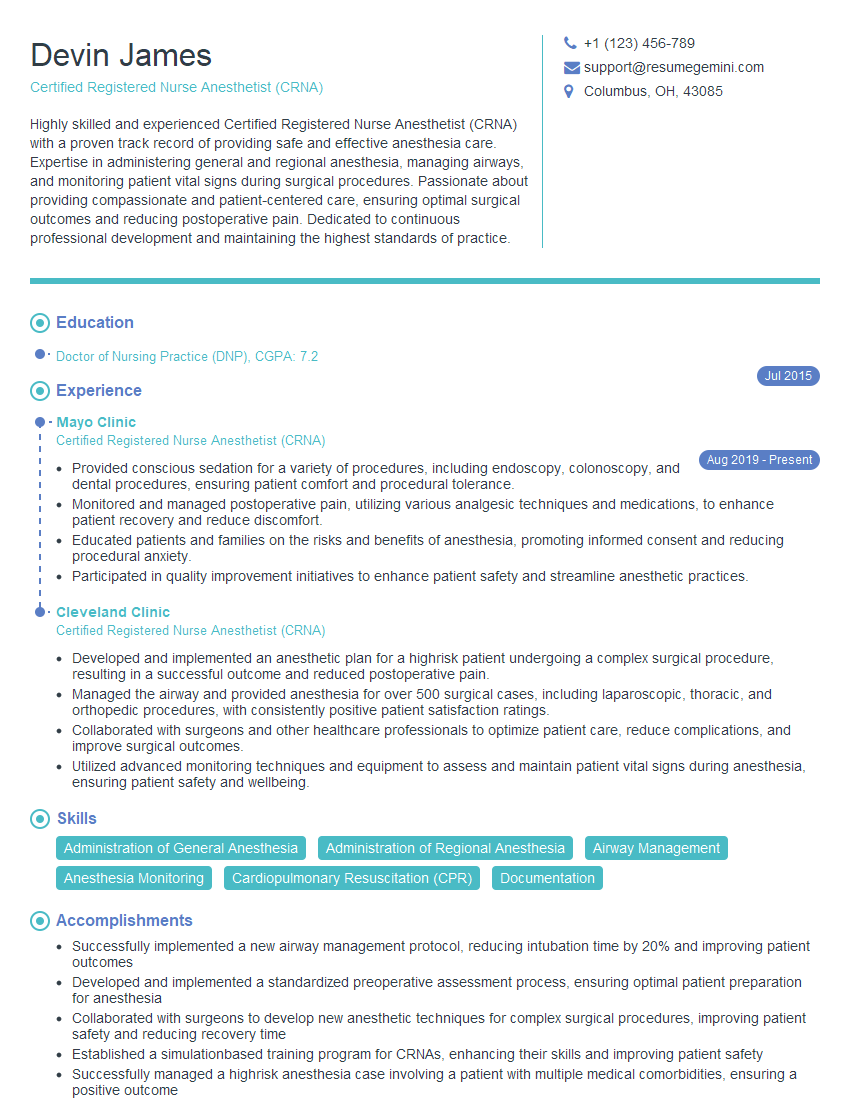
Mastering the intricacies of oophorectomy significantly enhances your career prospects in the medical field, opening doors to specialized roles and advanced opportunities. A well-crafted resume is crucial for showcasing your expertise and securing interviews. To maximize your chances of success, build an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource for creating professional and impactful resumes. They offer examples of resumes tailored to Oophorectomy specialists, providing valuable guidance to help you present yourself as the ideal candidate. Take the next step toward your dream job today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.