Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Orthopedic Footwear Prescribing interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Orthopedic Footwear Prescribing Interview
Q 1. What are the key differences between custom and prefabricated orthotics?
The primary difference between custom and prefabricated orthotics lies in their manufacturing process and level of personalization. Custom orthotics are individually crafted for a specific patient’s foot using a plaster cast or 3D scan. This allows for precise correction of foot deformities and biomechanical issues. Think of them as bespoke suits, tailored to fit perfectly. Prefabricated orthotics, on the other hand, are mass-produced in standard sizes. While they offer a more economical option, they lack the precise fit and customization of custom orthotics, akin to buying off-the-rack clothing – they might fit reasonably well, but won’t be as effective for complex biomechanical problems.
- Customization: Custom orthotics offer superior customization, addressing specific foot and biomechanical needs. Prefabricated orthotics provide limited adjustability.
- Cost: Custom orthotics are generally more expensive due to the individualized manufacturing process. Prefabricated orthotics are more affordable.
- Fit: Custom orthotics provide a superior fit, resulting in better comfort and support. Prefabricated orthotics offer a more general fit, potentially causing discomfort or inadequate support.
- Effectiveness: Custom orthotics are often more effective in treating complex foot and lower extremity conditions. Prefabricated orthotics may be suitable for milder conditions or as a temporary solution.
Q 2. Describe the process of taking a patient’s foot measurement for custom orthotics.
Taking accurate foot measurements for custom orthotics is crucial for their effectiveness. The process typically involves these steps:
- Patient History and Assessment: Begin by reviewing the patient’s medical history, including any existing foot conditions, injuries, or symptoms. This helps determine the areas needing specific attention.
- Visual Inspection: Observe the patient’s feet for any deformities, calluses, or other abnormalities. Note any signs of swelling or inflammation.
- Weight-Bearing Examination: Observe the patient’s foot posture and gait while standing. This helps identify any biomechanical issues, such as pronation or supination.
- Foot Measurement and Casting: For plaster casting, the foot is positioned correctly, and a plaster bandage is carefully applied to create a three-dimensional model of the foot. Modern methods increasingly use 3D scanning for a precise digital model avoiding the plaster cast.
- Cast Trimming and Refinement: Any excess plaster is carefully removed, ensuring the cast accurately reflects the foot’s shape.
- Model Preparation: The plaster cast or digital model is used to create a positive model that forms the basis for the orthotic construction.
For example, a patient with plantar fasciitis might require a custom orthotic with a deep heel cup and medial arch support to help alleviate the pain. Careful attention to detail during the measurement process is vital to ensuring the orthotic effectively addresses this specific condition.
Q 3. Explain the role of biomechanics in selecting appropriate orthopedic footwear.
Biomechanics plays a fundamental role in selecting appropriate orthopedic footwear. It’s the study of movement and the forces acting on the body. Understanding a patient’s biomechanics helps identify the underlying causes of foot and lower extremity problems and guides the choice of orthotic or footwear modification. For instance, a patient with excessive pronation (inward rolling of the foot) will need footwear that provides increased medial support to correct the alignment. Similarly, someone with excessive supination (outward rolling) would benefit from footwear providing lateral support.
Analyzing gait (the way a person walks), foot posture, and the alignment of the lower limbs provides crucial insights into their specific biomechanical needs. This analysis guides the choice of features within the orthopedic footwear – such as arch support, heel cushioning, and the type of sole – to address these specific issues.
Q 4. How do you assess a patient’s gait to determine the need for orthopedic footwear?
Assessing a patient’s gait is crucial for determining the need for orthopedic footwear. This involves observing their walking pattern from different angles, noting any deviations from normal gait. We look for:
- Gait Deviations: Such as limping, uneven step length, foot slap, or excessive pronation/supination.
- Foot Posture: Assessing foot posture during the stance phase, noting any deformities or abnormalities.
- Limb Alignment: Observing the alignment of the knees, hips, and spine during the gait cycle.
- Pain Location: Determining whether pain is present in specific areas of the foot, ankle, knee, or hip during walking.
For example, a patient with a noticeable limp and pain in the knee during the stance phase may require orthotic intervention to correct biomechanical issues causing the pain and altered gait. Observational gait analysis provides the necessary clues. More advanced gait labs can provide kinematic and kinetic data giving a more precise analysis.
Q 5. What are the common indications for prescribing orthopedic footwear?
There are numerous indications for prescribing orthopedic footwear. Some common ones include:
- Diabetes: To prevent foot ulcers and protect against neuropathy.
- Arthritis: To reduce pain and improve joint function.
- Plantar Fasciitis: To provide arch support and reduce heel pain.
- Bunions and Hammertoes: To alleviate pressure and improve comfort.
- Metatarsalgia: To redistribute pressure and reduce pain in the ball of the foot.
- Heel Spurs: To reduce stress on the heel and alleviate pain.
- Pes Planus (Flat Feet): To provide arch support and improve stability.
- Pes Cavus (High Arches): To improve shock absorption and reduce pressure points.
- Post-surgical rehabilitation: To provide support and protection during the healing process.
The specific type of orthopedic footwear will depend on the individual’s condition and biomechanical needs. The choice extends beyond simply shoe selection, it encompasses the design, fit, and material selection of the supportive devices or orthoses.
Q 6. Describe different types of orthopedic footwear modifications.
Orthopedic footwear modifications are diverse and tailored to individual needs. Common modifications include:
- Heel lifts/wedges: Used to correct leg length discrepancies or alleviate heel pain.
- Arch supports: Provide support for the medial longitudinal arch, addressing conditions like flat feet and plantar fasciitis.
- Metatarsal pads: Relieve pressure on the metatarsal heads, alleviating pain associated with metatarsalgia.
- Shoe Modifications: This can involve stretching, widening, or adding padding to accommodate specific foot shapes or deformities.
- Ankle Support: Additional straps or braces can provide support for the ankle joint.
- Toe Boxes: Larger toe boxes can prevent crowding of toes and reduce pressure in individuals with bunions or hammertoes.
The choice of modification depends on a comprehensive assessment of the patient’s condition and their biomechanical needs. For example, a patient with significant leg length discrepancy will require heel lifts, while someone with plantar fasciitis will benefit from custom orthotics with added arch support.
Q 7. How do you counsel patients on the proper care and maintenance of their orthotics?
Counseling patients on the proper care and maintenance of their orthotics is crucial for their longevity and effectiveness. This includes:
- Cleaning: Instruct patients to clean their orthotics regularly with mild soap and water, allowing them to air dry completely to prevent the growth of bacteria and fungi.
- Drying: Emphasize the importance of allowing orthotics to air dry completely after cleaning. Avoid placing them in direct sunlight or near heat sources, as this can damage the materials.
- Storage: Advise patients to store their orthotics in a cool, dry place when not in use to maintain their shape and integrity.
- Inspection: Encourage regular inspection of the orthotics for any signs of wear and tear, such as cracks or breaks in the material. Promptly report any damage.
- Replacement: Explain that orthotics typically have a limited lifespan, and replacement may be necessary every 6-12 months or sooner if significant wear and tear is evident. They should be replaced if they are damaged or no longer provide adequate support.
Using relatable analogies, such as comparing the care of orthotics to caring for expensive footwear, can improve patient understanding and compliance. Emphasizing the relationship between proper care and the longevity and effectiveness of the devices is key to ensuring continued benefit for the patient.
Q 8. What are the common materials used in the construction of orthotics?
Orthotics utilize a variety of materials, each chosen for its specific properties contributing to comfort, support, and durability. The selection depends on the patient’s needs and the orthotic’s design.
- Polypropylene: A common material for the base of many orthotics. It’s lightweight, durable, and can be easily molded to the foot’s shape. Think of it as a strong, adaptable foundation.
- Ethylene Vinyl Acetate (EVA): A softer material often used as a cushioning layer. It provides shock absorption and comfort, similar to the cushioning in athletic shoes.
- Leather: A natural material offering breathability and good moisture-wicking properties. However, it’s less durable than other materials and requires more care.
- Cork: A natural, lightweight material with good shock absorption properties. It’s often used in combination with other materials.
- Carbon Fiber: Used in high-performance orthotics, offering superior stiffness and support, especially beneficial for athletes or individuals with significant biomechanical needs. It’s lightweight but more expensive.
- Other materials: Various foams, plastics, and composites are used to achieve specific properties such as increased stiffness or cushioning in particular zones of the orthotic.
The combination of these materials allows for the creation of custom orthotics tailored to individual needs, addressing issues such as arch support, plantar fasciitis, and metatarsalgia.
Q 9. Explain the concept of pressure relief in relation to orthopedic footwear.
Pressure relief in orthopedic footwear is crucial for preventing pain and promoting healing. It involves distributing weight evenly across the foot, minimizing pressure on sensitive areas like bony prominences or inflamed tissues. This reduces pain and prevents further damage.
For example, a patient with a plantar ulcer will benefit from an orthotic that redistributes pressure away from the ulcer site onto healthier areas of the foot. This is achieved through various design features:
- Metatarsal pads: These elevate the metatarsal heads, reducing pressure on the forefoot. Think of them as strategically placed cushions.
- Heel cups: Provide support and cushioning to the heel, absorbing shock and reducing pressure on the heel bone.
- Arch supports: Support the arches of the feet, improving foot alignment and distributing weight more evenly. This prevents excessive stress on any one area.
- Custom-molded orthotics: Allow for precise pressure relief tailored to the individual’s foot shape and specific areas needing relief. These are the equivalent of a bespoke suit for the foot.
Proper pressure relief not only alleviates pain but also promotes faster healing of foot conditions and helps prevent future problems.
Q 10. How do you address patient concerns about the cost of custom orthotics?
Cost is a valid concern for many patients considering custom orthotics. My approach involves open and honest communication, outlining the long-term benefits and addressing concerns proactively.
Firstly, I explain the significant difference in quality and effectiveness between custom and over-the-counter orthotics. Custom orthotics provide superior support, pressure relief, and comfort, tailored precisely to their individual needs. It’s like comparing a well-fitted suit to off-the-rack clothing.
Secondly, I explore various payment options, including insurance coverage, financing plans, or payment schedules. Many insurance plans cover medically necessary orthotics, and I assist patients in navigating the process of obtaining authorization. Sometimes, a less costly option like a semi-custom orthotic might be explored if it fits the patient’s needs and budget.
Finally, I emphasize the long-term cost savings. Addressing foot problems promptly with proper orthotics can prevent more expensive treatments such as surgery or prolonged periods of disability, making the investment in custom orthotics a financially wise decision in the long run.
Q 11. Describe your experience with different types of footwear for various foot conditions.
My experience encompasses a wide range of footwear and conditions. For instance, patients with plantar fasciitis often benefit from shoes with good arch support, cushioned heels, and a firm, but flexible sole. Running shoes with good shock absorption can be a good choice.
Patients with diabetic neuropathy might require footwear with extra-depth to accommodate custom orthotics and to reduce pressure points. Seamless construction is important to minimize the risk of skin irritation and ulcer formation.
Individuals with arthritis might benefit from shoes with supportive uppers, good ankle stability, and wider toe boxes to reduce stress on the joints. Slip-on shoes or shoes with easy closures are often preferred for ease of use.
For patients with hallux valgus (bunion), footwear with a wider toe box is essential to prevent rubbing and pain. Shoes with a softer, more pliable upper material can also be helpful.
Each case is unique. My approach involves a thorough assessment of the patient’s condition, gait, and activity level to select or recommend appropriate footwear in conjunction with orthotics, ensuring optimal comfort, support, and functionality.
Q 12. How do you handle a situation where a patient experiences discomfort with their orthotics?
Discomfort with orthotics is not uncommon, especially initially. My protocol involves a systematic approach to identify and address the source of discomfort.
Step 1: Thorough Assessment: I re-evaluate the patient, checking the orthotics’ fit, alignment, and the patient’s footwear. This often involves visual inspection and gait analysis.
Step 2: Identify the Source: Common causes include pressure points, incorrect sizing, improper adjustment, or an underlying condition that requires modification to the orthotic.
Step 3: Implement Corrective Measures: Depending on the source of discomfort, solutions might include:
- Adjustments: Minor adjustments to the orthotic, such as adding padding or modifying the shell.
- Modification: More significant modifications might be necessary, requiring a return to the lab for adjustments.
- Trial Period: A gradual increase in wear time to allow the patient to adapt.
- Alternative Design: In some cases, a different design or material might be needed.
- Referral: If discomfort persists despite these measures, referral to a podiatrist or other specialist may be warranted.
Open communication and regular follow-up appointments are key to ensuring a successful outcome and patient satisfaction.
Q 13. What are the legal and ethical considerations related to prescribing orthotics?
Prescribing orthotics involves significant legal and ethical responsibilities. Maintaining accurate records is paramount. This includes obtaining informed consent from the patient, accurately documenting the assessment findings, treatment plan, and progress. It is also crucial to remain within the scope of practice and refer patients to appropriate specialists when needed. This might include a podiatrist or other medical professional.
Ethical considerations include:
- Patient Autonomy: Respecting the patient’s right to choose their treatment options and providing them with all necessary information to make informed decisions.
- Beneficence: Acting in the best interests of the patient, ensuring their safety and well-being.
- Non-maleficence: Avoiding actions that could cause harm.
- Justice: Providing equitable and fair access to orthotic care.
- Confidentiality: Protecting the privacy of patient information.
Adherence to professional standards and regulations, such as those set by relevant professional organizations, is essential. Maintaining appropriate professional liability insurance also protects both the patient and the practitioner.
Q 14. Explain the process of documenting your assessment and recommendations.
Documentation is crucial for legal and clinical reasons. My documentation process involves a structured approach, ensuring comprehensive and accurate records.
Initial Assessment: This includes a detailed patient history, including medical conditions, symptoms, and medications; a physical examination focusing on the foot and lower limb; gait analysis; and assessment of footwear. Any findings are recorded with supporting images or sketches if needed.
Treatment Plan: This outlines the prescribed orthotics, including materials, design features, and intended outcomes. The patient’s understanding and agreement with the plan are documented through obtaining informed consent. I always include photos of the patient’s feet and gait analysis for detailed tracking.
Progress Notes: Regular follow-up visits document the patient’s progress, any adjustments made to the orthotics, changes in symptoms, and any other relevant information. These notes detail the duration, the nature of follow-up visits, and any changes in treatment or referrals.
Discharge Summary: Once the treatment is complete, a discharge summary summarizes the course of care, final recommendations, and any further advice. This summarizes everything done and all recommendations provided.
All documentation is maintained securely and in accordance with relevant privacy regulations. This thorough approach ensures continuity of care, facilitates communication with other healthcare professionals, and provides a comprehensive record of the patient’s treatment.
Q 15. Describe your experience working with different healthcare professionals (e.g., podiatrists, physicians).
My experience collaborating with healthcare professionals is extensive and crucial to successful orthopedic footwear prescribing. I regularly work with podiatrists, physicians (especially orthopedists and physiatrists), physical therapists, and sometimes even occupational therapists. Podiatrists often provide the initial diagnosis and assessment of foot and ankle pathologies, outlining specific needs for orthotic intervention. Physicians, particularly orthopedists, contribute their expertise on underlying musculoskeletal conditions influencing footwear choices. For example, a patient with rheumatoid arthritis will require a different approach to footwear than someone with a plantar fasciitis diagnosis. Physical therapists provide valuable insights into the patient’s gait analysis and functional limitations, guiding orthotic design for improved mobility and reduced pain. Effective communication and collaboration ensure a holistic and patient-centered approach.
I’ve found that a structured communication process using shared patient charts or electronic health records improves the efficiency and accuracy of referrals and follow-ups. Regular team meetings also help address complex cases collaboratively. One memorable case involved a diabetic patient with peripheral neuropathy. Through collaborative efforts with the podiatrist and primary physician, we were able to design custom orthotics that significantly reduced pressure points and prevented further complications.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you stay updated on the latest advancements in orthopedic footwear technology?
Staying abreast of advancements in orthopedic footwear technology is essential. I achieve this through a multi-pronged approach. Firstly, I actively participate in continuing education courses and professional conferences, such as those offered by the American Academy of Orthopaedic Surgeons or the American Podiatric Medical Association. These events often feature presentations on the latest materials, design techniques, and research findings in the field.
Secondly, I maintain subscriptions to relevant professional journals and online publications. I regularly review articles on new biomechanical principles, material innovations (e.g., advancements in carbon fiber composites or 3D-printed orthotics), and clinical studies evaluating the efficacy of various orthotic designs. Thirdly, I stay connected with industry leaders and manufacturers through attending trade shows and networking events, which provides exposure to new technologies and product development firsthand. Finally, I make an effort to maintain a network of colleagues and experts within the field, sharing knowledge and learning from their experiences.
Q 17. How do you determine the appropriate level of support needed for a patient’s orthotics?
Determining the appropriate level of support for a patient’s orthotics is a nuanced process requiring a thorough assessment. It begins with a comprehensive patient history, including their medical history, current symptoms, activity levels, and any prior orthotic use. A physical examination follows, focusing on the foot’s structure, gait analysis, and range of motion. This assessment helps identify specific areas of instability, pressure points, or deformities.
I utilize several tools to quantify the level of support needed. For example, static posturography or pressure mapping can objectively measure weight distribution and identify areas requiring offloading or added support. Radiographic imaging (X-rays) provides insights into bony structures and alignment abnormalities. Based on this combined information, I determine the need for custom-made orthotics versus prefabricated options. The level of support can range from simple cushioning to complex designs incorporating custom molds, arch supports, metatarsal pads, and heel lifts. Each case is unique, and selecting the right level of support is essential for achieving the therapeutic goals and avoiding complications.
Q 18. What are the contraindications for prescribing certain types of orthopedic footwear?
Contraindications for prescribing specific types of orthopedic footwear are important to consider. For instance, patients with severe peripheral arterial disease (PAD) may have reduced blood flow to their feet, making tight or constrictive footwear detrimental. Improper fit can impede circulation further, potentially leading to ulcers or tissue necrosis. Patients with active infections or open wounds on their feet should avoid any type of footwear that could further irritate the affected area until the infection is properly managed.
Certain types of rigid orthotics may be contraindicated in patients with significant joint deformities or severe neurological conditions that compromise sensation and protective reflexes. For example, a patient with Charcot foot should not use a very rigid orthotic which could lead to further bone damage. Always ensure a detailed evaluation of the patient’s overall health condition before making any orthotic recommendations. Patient education about proper care and monitoring of their feet after receiving new footwear is also a crucial component.
Q 19. Describe your experience with different casting methods for custom orthotics.
My experience encompasses various casting methods for custom orthotics. Traditionally, we use foam box casting, where the patient’s foot is placed in a foam box, and a plaster of Paris or resin material is poured in to create a negative mold. This method provides a relatively inexpensive and readily accessible way to capture foot morphology. However, it can be challenging to ensure consistent pressure distribution and capture all the intricate details of the foot’s anatomy.
More recently, I’ve utilized digital scanning technology, using a 3D scanner to create a precise digital impression of the patient’s foot. This technology offers superior accuracy and detail compared to traditional casting, allows for better reproducibility and facilitates easy storage and modification of the digital model. This process minimizes casting time and allows for more efficient production of custom orthotics. The choice between traditional and digital casting depends on factors like access to technology, patient preference, and the complexity of the orthotic design needed.
Q 20. How do you select the appropriate shoe last for a patient’s custom orthotics?
Selecting the appropriate shoe last for a patient’s custom orthotics is critical for ensuring comfort, fit, and effectiveness. The shoe last refers to the shape of the mold around which a shoe is made. It significantly influences the overall fit and feel of the final product. I consider several factors when making this selection. Firstly, the patient’s foot shape and size are paramount. We need a last that accurately reflects the patient’s metatarsal width, heel shape, and arch height to accommodate the orthotic without causing constriction or excessive space.
Secondly, the patient’s activity level and footwear preferences are taken into account. An athletic individual might require a last designed for stability and support, while someone with a sedentary lifestyle might need a more comfortable and flexible last. Thirdly, any underlying foot pathologies will influence the choice. Patients with hallux valgus (bunion) might need a wider last, whereas those with pes cavus (high arch) might require a last with more arch support. Close collaboration with the patient throughout this process and a clear understanding of their needs ensure a successful outcome.
Q 21. Explain the concept of offloading in relation to foot and ankle pathology.
Offloading, in the context of foot and ankle pathology, refers to the strategic reduction of pressure on specific areas of the foot to alleviate pain, promote healing, and prevent further complications. This is particularly important in conditions like diabetic foot ulcers, plantar fasciitis, and stress fractures. The goal is to redistribute weight away from the sensitive or injured area to adjacent, healthier tissues.
Techniques for offloading vary depending on the specific condition and location of the affected area. Orthotic devices play a crucial role, employing features such as custom-molded supports, metatarsal pads, heel wedges, or rocker-bottom soles to redistribute pressure. In severe cases, total contact casts or specialized footwear, such as therapeutic shoes or crutches, might be necessary to completely remove weight from the affected region. The success of offloading relies heavily on accurate assessment of pressure points, appropriate orthotic design, and close patient monitoring to ensure efficacy and prevent recurrence. Careful patient education on appropriate footwear and activity modifications is key to long-term management.
Q 22. What are the key components of a proper footwear prescription?
A proper footwear prescription isn’t just about the shoe; it’s a holistic assessment of the patient’s needs. It’s a detailed plan encompassing several key components.
- Patient History and Examination: This involves a thorough understanding of the patient’s medical history, current complaints (pain, swelling, deformity), activity levels, and lifestyle. A physical examination assesses the feet, ankles, and lower extremities for any structural abnormalities, gait deviations, or signs of pathology.
- Diagnosis: Accurate identification of the underlying foot or ankle condition, such as plantar fasciitis, bunions, diabetic neuropathy, or arthritis, is crucial. This guides the selection of appropriate footwear and orthotic considerations.
- Footwear Recommendations: The prescription will specify the type of shoe (e.g., athletic, dress, casual), material (e.g., leather, synthetic), features (e.g., depth, width, heel height, arch support), and any modifications required (e.g., extra depth, stretch panels).
- Orthotic Recommendations (if needed): This section details the type of orthotic (e.g., custom, prefabricated), its design features (e.g., arch support, metatarsal pads, heel cups), materials, and any adjustments needed. It also includes instructions for orthotic care and maintenance.
- Follow-up Plan: This outlines the frequency and purpose of follow-up appointments to assess the effectiveness of the prescribed footwear and orthotics and to make any necessary adjustments.
For example, a patient with plantar fasciitis might receive a prescription for shoes with good cushioning, a rigid sole, and a moderate heel height, possibly combined with a custom orthotic with a deep heel cup and medial arch support.
Q 23. How do you communicate effectively with patients regarding their footwear needs?
Effective communication is paramount in orthopedic footwear prescribing. I prioritize clear, empathetic communication, tailored to the patient’s understanding.
- Active Listening: I start by actively listening to the patient’s concerns and description of their symptoms, using open-ended questions to encourage detailed responses. This helps build rapport and ensures I fully understand their needs and expectations.
- Visual Aids: I often use diagrams, models, or images to illustrate anatomical structures and explain the rationale behind footwear and orthotic recommendations. This simplifies complex concepts and promotes understanding.
- Plain Language: I avoid medical jargon and explain terms in simple, easy-to-understand language. I use analogies when appropriate to explain complex concepts. For example, I might compare an orthotic to a ‘foundation’ for the foot.
- Shared Decision-Making: I encourage patients to participate actively in the decision-making process, involving them in the choice of shoes and orthotics whenever possible, considering their preferences and lifestyle.
- Written Instructions: I always provide clear, written instructions on how to wear, care for, and maintain their prescribed footwear and orthotics. This serves as a reliable reference for patients after their appointment.
For instance, when explaining the importance of custom orthotics, I might say something like, ‘Imagine your foot is like a building; the orthotic is the foundation, providing stability and support to avoid further damage.’
Q 24. What are the potential complications associated with improper orthotic fitting?
Improper orthotic fitting can lead to a range of complications, significantly impacting patient comfort and recovery.
- Increased Pain: Incorrectly fitted orthotics can worsen existing pain or create new pain points by applying excessive pressure or failing to provide adequate support. This might lead to pressure sores, skin irritation, or nerve compression.
- Gait Alterations: Poorly fitted orthotics can alter a patient’s gait, leading to compensatory movements in other joints (knees, hips, back), potentially causing pain or further injury.
- Delayed Healing: Inadequate support can impede the healing process of underlying foot conditions. For example, improper arch support in plantar fasciitis can prevent adequate stretching of the plantar fascia.
- Recurrence of Symptoms: If the root cause of the problem isn’t addressed or if the orthotics don’t provide the necessary correction, symptoms may recur or worsen.
- Foot Deformities: In some cases, improper footwear or orthotics can even worsen existing foot deformities or contribute to new ones.
For example, a patient with a high arch might experience increased pain if fitted with an orthotic that doesn’t provide enough support to their arch, leading to over-pronation.
Q 25. Describe your experience with different types of foot pathologies.
My experience encompasses a wide spectrum of foot pathologies, each requiring a unique approach to footwear management.
- Plantar Fasciitis: I frequently manage patients with plantar fasciitis, prescribing shoes with good shock absorption and arch support, often combined with custom orthotics featuring a deep heel cup and medial arch support.
- Diabetic Neuropathy: Patients with diabetic neuropathy require footwear that minimizes pressure points and protects the feet from injury. This includes deep, wide shoes with seamless interiors and soft, flexible materials.
- Hallux Valgus (Bunions): Bunions necessitate footwear with a roomy toe box to reduce pressure on the bunion. Orthotics can help realign the foot and reduce pain.
- Pes Planus (Flat Feet): Patients with flat feet benefit from shoes with good arch support and possibly custom orthotics to provide structural support and prevent over-pronation.
- Rheumatoid Arthritis: Patients with rheumatoid arthritis may experience pain and inflammation in their feet, requiring shoes that are comfortable, easy to slip on and off, and accommodate joint swelling. Orthotics can help improve joint alignment and reduce pressure.
I consistently adapt my approach based on the specific needs of each patient, carefully selecting footwear and orthotics to address their unique symptoms and limitations. For instance, a patient with severe rheumatoid arthritis might need specialized shoes with adjustable straps and extra-depth options, while a patient with milder symptoms might need only supportive insoles.
Q 26. How do you ensure the proper fit and function of an orthotic device?
Ensuring proper fit and function of an orthotic device is critical for its effectiveness. This requires a multi-step process.
- Accurate Casting and Modeling (for custom orthotics): Precise casting techniques are crucial to capture the unique shape and dimensions of the patient’s foot. Any inaccuracies in the model will result in poorly fitting orthotics.
- Biomechanical Evaluation: I perform gait analysis and observe the patient’s weight-bearing patterns to determine the appropriate orthotic design and features (e.g., arch support, posting, heel modifications).
- Initial Fitting and Adjustments: The initial fitting involves careful assessment of the orthotic’s fit and comfort. Adjustments are made as needed to ensure proper alignment and pressure distribution.
- Patient Education: Patients receive thorough instructions on proper orthotic wear, care, and maintenance. This ensures they use the orthotics correctly and extend their lifespan.
- Follow-up Assessments: Regular follow-up appointments are essential to monitor the effectiveness of the orthotics, assess for any complications (e.g., pressure sores, skin irritation), and make any necessary modifications.
I use a combination of clinical observation, patient feedback, and pressure mapping (when available) to assess the fit and function of orthotics, ensuring optimal comfort and support. For example, I might use pressure mapping to identify areas of excessive pressure which would indicate the need for adjustments to the orthotic.
Q 27. What are your strategies for managing patients with complex foot and ankle problems?
Managing patients with complex foot and ankle problems requires a collaborative and comprehensive approach.
- Multidisciplinary Collaboration: I often work closely with other healthcare professionals, such as podiatrists, physiatrists, or orthopedic surgeons, to develop a holistic treatment plan. This ensures coordinated care and addresses all aspects of the patient’s condition.
- Advanced Imaging and Diagnostic Techniques: I utilize advanced imaging techniques, such as X-rays, MRI, or CT scans, to obtain detailed information about the patient’s foot and ankle structure and pathology.
- Custom Orthotic Design: For complex cases, I may recommend custom-fabricated orthotics with advanced design features to address specific biomechanical needs. This might involve specialized materials or complex adjustments to control foot motion and reduce pressure.
- Serial Casting or Bracing: In some cases, serial casting or bracing may be necessary to correct significant deformities or provide additional support and immobilization.
- Surgical Consultation: I refer patients to orthopedic surgeons when conservative management fails to provide adequate relief or when surgical intervention is necessary.
For example, a patient with severe Charcot neuroarthropathy might require custom orthotics, offloading footwear, regular wound care, and potentially surgical intervention to manage the condition.
Q 28. How do you handle patient complaints or dissatisfaction with their orthotic footwear?
Patient complaints or dissatisfaction are opportunities to improve care and ensure optimal outcomes.
- Active Listening and Empathy: I start by actively listening to the patient’s concerns, demonstrating empathy and understanding. I avoid interrupting and allow them to fully express their feelings.
- Thorough Examination and Assessment: I conduct a comprehensive examination of the patient’s feet, orthotics, and footwear to identify potential causes of the discomfort. This may involve reviewing the initial prescription and comparing it to the patient’s current condition.
- Adjustments and Modifications: Based on the assessment, I may make adjustments to the orthotics or recommend alternative footwear options. This may involve modifying existing orthotics, creating new ones, or suggesting different shoe types.
- Patient Education and Re-education: I provide clear and concise education on proper orthotic use, care, and maintenance. I ensure patients understand the importance of adherence to the treatment plan.
- Open Communication and Follow-up: I maintain open communication with patients throughout the process, providing regular follow-up appointments to monitor progress and address any further concerns. This ensures ongoing support and facilitates adjustment as needed.
For example, a patient complaining of a hot spot on their orthotic might require a simple adjustment to relieve pressure, while a patient with persistent pain despite proper orthotic use might need a reassessment of their underlying condition.
Key Topics to Learn for Orthopedic Footwear Prescribing Interview
- Biomechanics of the Foot and Ankle: Understanding gait analysis, common foot deformities (e.g., plantar fasciitis, hallux valgus), and their impact on footwear selection.
- Footwear Assessment: Practical application of assessing patient needs, analyzing existing footwear, and identifying areas for improvement in comfort and support. This includes understanding different shoe construction materials and their properties.
- Prescribing Principles: Knowing the criteria for recommending specific types of orthopedic footwear (e.g., custom orthotics, accommodative footwear, supportive footwear) based on patient diagnoses and functional limitations.
- Patient Communication and Counseling: Effectively communicating with patients regarding their footwear needs, explaining prescribing rationale, and addressing concerns. This includes active listening and empathy.
- Legal and Ethical Considerations: Understanding relevant regulations and ethical guidelines related to prescribing orthopedic footwear, including documentation and liability.
- Measurement and Fitting Techniques: Mastering accurate foot measurement techniques and applying them to ensure proper fit and function of prescribed footwear.
- Material Science in Orthopedic Footwear: Understanding the properties of various materials used in orthotic construction and their impact on patient outcomes.
- Rehabilitation and Follow-up Care: Understanding the role of footwear in the rehabilitation process and the importance of post-prescription follow-up to assess efficacy and make necessary adjustments.
Next Steps
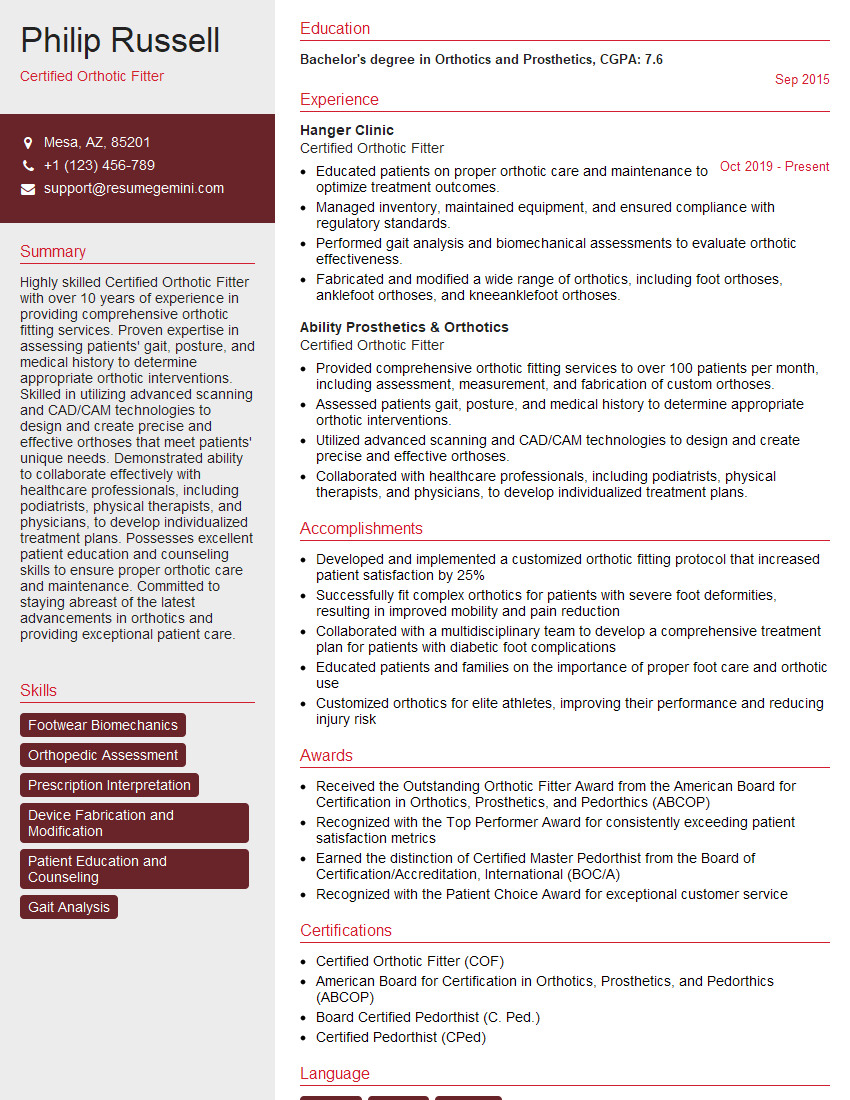
Mastering Orthopedic Footwear Prescribing significantly enhances your career prospects, opening doors to specialized roles and increased earning potential. A strong resume is crucial for showcasing your skills and experience to potential employers. To maximize your job search success, create an ATS-friendly resume that highlights your qualifications effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored specifically to Orthopedic Footwear Prescribing to help guide you in crafting your own compelling application materials.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.