Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Ovarian Cyst Management interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Ovarian Cyst Management Interview
Q 1. Describe the different types of ovarian cysts.
Ovarian cysts are fluid-filled sacs that develop on the ovaries. They’re surprisingly common, with many women experiencing them at some point in their lives. There are several types, categorized primarily by their location, contents, and association with the menstrual cycle.
- Follicular cysts: These are the most common type and arise from a follicle (the sac that holds the egg) that doesn’t rupture and release the egg during ovulation. They’re usually small and often resolve on their own.
- Corpus luteum cysts: These form after ovulation when the ruptured follicle fails to shrink properly. They can sometimes produce hormones.
- Dermoid cysts (teratomas): These are benign cysts containing various tissue types, like hair, teeth, or skin. They are often discovered incidentally.
- Endometriomas: These cysts are associated with endometriosis, a condition where endometrial-like tissue grows outside the uterus. They can be painful and contribute to infertility.
- Cystadenomas: These are more complex cysts, typically larger and lined with glandular or epithelial tissue. They can be further categorized as serous or mucinous based on the type of fluid they contain. Most are benign but some can be precancerous.
Understanding the different types is crucial for determining the appropriate management strategy. For example, a simple follicular cyst often needs only observation, while a large or symptomatic cystadenoma may require surgical intervention.
Q 2. Explain the diagnostic methods used to identify ovarian cysts.
Diagnosing ovarian cysts typically involves a combination of methods, starting with a thorough medical history and physical exam. The doctor will inquire about symptoms, menstrual cycles, and family history. Key diagnostic tools include:
- Pelvic Examination: A physical examination of the pelvis to feel for any abnormalities.
- Transvaginal Ultrasound: This is the most common imaging technique used to visualize the ovaries and assess the size, shape, and characteristics of the cyst. It provides a clear picture of the cyst’s internal structure, helping to differentiate between various types.
- Transabdominal Ultrasound: An alternative ultrasound method where the probe is placed on the abdomen. It’s less detailed than a transvaginal ultrasound but is suitable for some situations.
- CA-125 Blood Test: This blood test measures the level of CA-125, a tumor marker that can be elevated in certain ovarian cancers, but also in benign conditions like endometriosis. It’s not solely diagnostic for ovarian cysts but is used in conjunction with other tests, especially when there is suspicion of malignancy.
- MRI or CT Scan: These advanced imaging techniques are usually employed when the ultrasound results are inconclusive or when there’s suspicion of malignancy. They provide more detailed images than ultrasound.
The choice of diagnostic method depends on the patient’s individual circumstances, symptoms, and the initial findings of the physical examination.
Q 3. What are the common symptoms associated with ovarian cysts?
Many ovarian cysts are asymptomatic, meaning they cause no noticeable symptoms. However, when symptoms do occur, they can vary depending on the size and type of cyst. Common symptoms include:
- Pelvic pain: This can range from mild discomfort to severe, sharp pain, often felt on one side of the pelvis.
- Abdominal bloating or distension: A feeling of fullness or pressure in the abdomen.
- Menstrual irregularities: Changes in menstrual cycle length or flow, including heavier or more painful periods.
- Pain during intercourse (dyspareunia): Pain experienced during sexual activity.
- Nausea and vomiting: In some cases, cysts can cause gastrointestinal upset.
- Breast tenderness: Hormonal imbalances associated with some types of cysts can cause breast pain or tenderness.
It’s important to note that the absence of symptoms doesn’t necessarily mean the cyst is benign. Regular checkups and monitoring are crucial, especially if there are risk factors or family history of ovarian cancer.
Q 4. Outline the management strategies for asymptomatic ovarian cysts.
Management of asymptomatic ovarian cysts typically involves a ‘watch and wait’ approach, which is also known as conservative management. This involves regular monitoring through ultrasound scans to assess the cyst’s size and characteristics over time.
The frequency of follow-up scans depends on several factors, including the woman’s age, the cyst’s size and appearance on ultrasound, and the presence of any risk factors. Simple cysts that are small and appear benign on ultrasound may only require monitoring every 3-6 months. Larger or complex cysts may require more frequent follow-up.
This approach allows for early detection of any changes that might warrant further intervention. The goal is to avoid unnecessary treatment while ensuring timely management should the cyst grow or change in nature.
Q 5. Discuss the treatment options for symptomatic ovarian cysts.
Treatment for symptomatic ovarian cysts aims to alleviate symptoms and prevent complications. The treatment approach depends on the type, size, and symptoms of the cyst. Options include:
- Pain Management: Over-the-counter pain relievers such as ibuprofen or acetaminophen can often effectively manage mild to moderate pain.
- Hormonal Therapy: Oral contraceptives can help regulate hormone levels and may reduce the risk of cyst formation or recurrence in some cases. Other hormonal medications may be used depending on the specific type of cyst.
- Laparoscopic Cystectomy: A minimally invasive surgical procedure to remove the cyst, often preferred for symptomatic cysts that don’t resolve spontaneously or for those that show characteristics that raise concerns.
The decision on the best treatment strategy should be made in consultation with a healthcare professional after considering the individual circumstances and a thorough assessment of the cyst.
Q 6. When is surgical intervention necessary for ovarian cysts?
Surgical intervention for ovarian cysts is considered in several specific situations. These include:
- Large cysts (greater than 5-10cm): Larger cysts increase the risk of rupture or torsion (twisting of the ovary).
- Symptomatic cysts unresponsive to medical management: If pain or other symptoms persist despite medical treatment.
- Suspected malignancy: If the ultrasound appearance suggests cancer or if there are other concerning findings (e.g., elevated CA-125 levels).
- Torsion of the ovary: This is a medical emergency where the ovary twists on its stalk, cutting off its blood supply. It requires immediate surgical intervention.
- Rupture of the cyst: A ruptured cyst can cause internal bleeding and requires prompt surgical attention.
- Cysts that continue to grow or change during monitoring: Persistent growth or concerning changes in the cyst’s characteristics warrant surgical evaluation.
The decision to proceed with surgery is based on a comprehensive assessment of the patient’s condition, the cyst’s characteristics, and the potential risks and benefits of surgery.
Q 7. Explain the different surgical techniques used for ovarian cyst removal.
Several surgical techniques are used for ovarian cyst removal, with the choice influenced by factors like the cyst’s size, location, and characteristics, and the surgeon’s expertise. Common methods include:
- Laparoscopic Cystectomy: A minimally invasive procedure using small incisions and a laparoscope (a thin, lighted instrument) to visualize and remove the cyst. This is often preferred for smaller cysts and leads to less pain, scarring, and faster recovery time.
- Laparotomy: A more invasive open surgery involving a larger incision to access the ovary. It’s usually reserved for larger or complex cysts or in situations where laparoscopy isn’t feasible.
- Oophorectomy: Surgical removal of the ovary. This is considered when the cyst is suspicious for cancer or when preserving the ovary poses significant risk.
- Salpingo-oophorectomy: Removal of both the ovary and the fallopian tube. This is often performed if there is cancer or severe endometriosis.
Each procedure has its own advantages and disadvantages. The decision on the most suitable surgical technique should be made on a case-by-case basis by a qualified surgeon after a detailed discussion with the patient.
Q 8. What are the potential complications of ovarian cyst surgery?
Ovarian cyst surgery, while generally safe, carries potential complications. These can range from minor to severe, and their likelihood depends on factors like the size and type of cyst, the patient’s overall health, and the surgical technique employed.
- Bleeding: Minor bleeding is common, but major hemorrhaging is a rare but serious risk.
- Infection: As with any surgery, infection at the incision site or internally is a possibility. Prophylactic antibiotics are often used to minimize this risk.
- Damage to adjacent organs: The ovaries are close to other vital structures like the bladder and intestines. Accidental damage during surgery, though uncommon with experienced surgeons, is a risk.
- Adhesions: Scar tissue formation (adhesions) can occur after surgery, potentially causing pain or complications in future pregnancies.
- Ovarian dysfunction: In some cases, surgery might affect ovarian function, leading to irregular periods or decreased fertility. This risk is usually higher with more extensive surgeries.
- Recurrence: Depending on the type of cyst, there’s a chance of recurrence. For example, functional cysts often resolve on their own, while others might need further intervention.
- Anesthesia complications: Risks associated with general anesthesia, such as allergic reactions or respiratory problems, also need to be considered.
It’s crucial to remember that these are potential complications, and the majority of women undergoing ovarian cyst surgery experience no major issues. A thorough discussion with the surgeon beforehand helps patients understand the risks involved and make informed decisions.
Q 9. How do you counsel patients about the risks and benefits of ovarian cyst treatment?
Counseling patients about ovarian cyst treatment requires a balanced approach, carefully weighing the risks and benefits of each option. I start by explaining the nature of the cyst, its size, and its characteristics based on imaging reports. Then, we discuss the various treatment strategies, including watchful waiting (for small, asymptomatic cysts), medication (for certain types of cysts), or surgery (if the cyst is large, symptomatic, or concerning for malignancy).
For each option, I clearly explain the potential benefits – for example, pain relief, reduced risk of rupture, or definitive diagnosis – alongside the potential risks and side effects. This often includes a discussion of the potential complications outlined earlier, as well as the possibility of complications related to medication, such as hormonal side effects. I use visual aids like diagrams and flowcharts to enhance understanding. I also answer all their questions frankly and honestly, ensuring they understand that the final decision rests with them. The goal is to empower them to make an informed choice that aligns with their individual values and preferences.
For example, a young woman with a small functional cyst might opt for watchful waiting and regular ultrasound monitoring, while a woman with a large, complex cyst causing significant pain may opt for surgery immediately. Every patient’s situation is unique and requires a tailored counseling approach.
Q 10. Describe the post-operative care for patients who have undergone ovarian cyst surgery.
Post-operative care for ovarian cyst surgery is crucial for a successful recovery. The immediate post-operative period usually involves monitoring vital signs, pain management, and assessing for any signs of complications like bleeding or infection. Patients are typically given pain medication and instructions on how to manage pain effectively.
- Pain management: Pain levels are assessed and managed with analgesics.
- Incision care: Patients are instructed on proper wound cleaning and dressing changes to prevent infection.
- Activity restrictions: Initially, patients are advised to rest and avoid strenuous activities. Gradual resumption of normal activities is encouraged as tolerated.
- Dietary advice: A healthy, balanced diet contributes to healing.
- Follow-up appointments: Regular check-ups are essential to monitor healing progress and assess for any complications.
- Medication: Antibiotics may be prescribed to prevent infection. Other medications, such as anti-inflammatory drugs or laxatives may also be used.
Patients are also advised on recognizing potential signs of complications, such as excessive bleeding, severe pain, fever, or increased abdominal swelling, and to seek immediate medical attention if they experience any of these.
The duration of recovery varies depending on the extent of the surgery and the patient’s overall health. Some patients might need a few days of hospitalization, while others can recover at home with appropriate support.
Q 11. What are the long-term consequences of ovarian cysts?
The long-term consequences of ovarian cysts depend heavily on several factors: the type of cyst, its size, whether it was treated surgically or medically, and the patient’s overall health. Many functional cysts (follicular or corpus luteum cysts) resolve spontaneously without long-term effects.
- Infertility: Large or complicated cysts, or those requiring extensive surgery, can potentially affect fertility, although this is not always the case. It’s important to note that many women with a history of ovarian cysts go on to have successful pregnancies.
- Chronic pelvic pain: In some cases, ovarian cysts can cause persistent pelvic pain, even after treatment. This might require ongoing pain management strategies.
- Ovarian torsion: Large cysts increase the risk of ovarian torsion (twisting of the ovary), a painful and potentially serious complication that can lead to ovarian damage or removal.
- Cancer risk: While most ovarian cysts are benign, some can be cancerous. Regular check-ups and monitoring are crucial to detect any cancerous changes early.
Regular follow-up appointments with a gynecologist are recommended, particularly for women with a history of ovarian cysts, to monitor for any long-term complications and ensure timely intervention if needed.
Q 12. How do you differentiate between benign and malignant ovarian cysts?
Differentiating between benign and malignant ovarian cysts is a critical aspect of ovarian cyst management. It’s not always possible to definitively distinguish between them based on symptoms alone; imaging and further tests are crucial.
Benign cysts are generally functional cysts (follicular, corpus luteum), dermoid cysts (containing tissues like hair and teeth), or endometriomas (associated with endometriosis). Malignant cysts, which are cancerous, represent a much smaller percentage of ovarian cysts.
- Imaging: Ultrasound, CT scans, and MRIs provide valuable information about the cyst’s size, shape, internal characteristics (e.g., solid or cystic components), and relationship to surrounding structures. Suspicious features on imaging can raise concerns for malignancy.
- CA-125 levels: This blood test measures a protein often elevated in cancerous ovarian tissue, although it can also be elevated in benign conditions.
- Biopsy: In cases where imaging is inconclusive or suspicion of malignancy is high, a biopsy (tissue sample) may be necessary for definitive diagnosis under microscopic examination. This can be done laparoscopically or through other minimally invasive techniques.
The combination of clinical evaluation, imaging findings, and biomarker analysis (CA-125) helps physicians determine whether a cyst is benign or malignant. If malignancy is suspected, further investigations and specialized management by an oncologist are needed.
Q 13. What role does imaging play in the diagnosis and management of ovarian cysts?
Imaging plays a pivotal role in the diagnosis and management of ovarian cysts. It provides non-invasive ways to visualize the cysts, assess their size, and characterize their internal structure.
- Transvaginal ultrasound: This is the most commonly used imaging technique for ovarian cysts. It provides detailed images of the ovaries and helps determine the cyst’s size, shape, and internal characteristics (e.g., solid vs. fluid-filled).
- Pelvic ultrasound (abdominal): An abdominal ultrasound can also visualize the ovaries, but it may not provide the same level of detail as transvaginal ultrasound.
- CT scan and MRI: These advanced imaging techniques can provide more detailed information about the cyst and its relationship to surrounding structures, particularly if there is a concern for malignancy or complex cysts.
Imaging helps in several aspects of management:
- Diagnosis: Identifying the type of cyst (functional, dermoid, endometrioma, etc.).
- Monitoring: Tracking the size and characteristics of cysts over time to assess their growth or regression.
- Treatment planning: Guiding decisions about whether to adopt a watchful waiting approach, medical management, or surgical intervention.
- Post-operative evaluation: Assessing for residual cysts or complications after surgery.
The choice of imaging modality depends on the clinical scenario and the information needed. In many cases, a simple transvaginal ultrasound is sufficient, while more advanced imaging techniques may be necessary if there are concerns about malignancy or complex cysts.
Q 14. Discuss the use of hormonal therapy in the management of ovarian cysts.
Hormonal therapy isn’t a first-line treatment for all ovarian cysts, but it can be effective in managing certain types, particularly functional cysts. It primarily aims to suppress ovarian function and reduce the production of hormones that contribute to cyst formation.
- Oral contraceptives: These are often used to regulate menstrual cycles and prevent the formation of new functional cysts. They can also help reduce the risk of recurrence. The choice of specific oral contraceptives depends on the individual patient’s needs and medical history.
- Gonadotropin-releasing hormone (GnRH) agonists/antagonists: These medications temporarily suppress ovarian function, leading to a decrease in hormone production. They are used primarily for symptomatic endometriomas (cysts associated with endometriosis). Because they suppress ovarian function, they are generally used for a limited period due to potential side effects like bone loss.
The use of hormonal therapy needs to be carefully considered and personalized based on factors such as the patient’s age, desire for future fertility, and overall health. Close monitoring is essential to assess the effectiveness of treatment and to address any side effects that may arise. It is important to remember that hormonal therapy is not a cure for ovarian cysts but can help to manage symptoms and prevent new cyst formation in select cases. In some cases, it might be used in conjunction with other treatments, such as surgery.
Q 15. Explain the role of laparoscopy in the diagnosis and treatment of ovarian cysts.
Laparoscopy plays a crucial role in both diagnosing and treating ovarian cysts. It’s a minimally invasive surgical procedure where a small incision is made, and a thin, lighted tube with a camera (laparoscope) is inserted into the abdomen. This allows for direct visualization of the ovaries and surrounding structures.
Diagnosis: Laparoscopy provides a definitive diagnosis by directly visualizing the cyst, determining its size, location, and characteristics (e.g., solid, cystic, or complex). It can differentiate between benign and potentially malignant cysts, guiding further management. For instance, a simple functional cyst might be easily identified and observed, while a suspicious lesion might require biopsy or removal.
Treatment: In many cases, laparoscopy allows for the surgical removal of the cyst (cystectomy) or the entire ovary (oophorectomy), depending on the cyst’s characteristics, the patient’s age, and reproductive goals. This is particularly beneficial for large, symptomatic cysts, or those raising concerns for malignancy. The minimally invasive nature of laparoscopy leads to faster recovery times, less pain, and reduced scarring compared to open surgery.
Example: A 35-year-old woman presents with a large ovarian cyst causing pelvic pain. Laparoscopy confirms a dermoid cyst (benign). The surgeon performs a laparoscopic cystectomy, removing the cyst while preserving the ovary. The patient recovers quickly and experiences minimal postoperative discomfort.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage ovarian cysts in pregnant women?
Managing ovarian cysts in pregnant women requires a cautious approach balancing maternal and fetal well-being. The primary concern is the potential for complications like rupture, torsion, or hemorrhage. Most functional cysts resolve spontaneously during pregnancy, so close monitoring is often sufficient.
Management Strategy: Regular ultrasound scans are crucial to track the cyst’s size and characteristics throughout the pregnancy. Small, asymptomatic cysts often require only watchful waiting with serial ultrasounds. However, if the cyst grows rapidly, causes significant pain, or displays features suggestive of malignancy, intervention might be necessary.
Intervention Considerations: Surgical intervention is generally avoided during the first trimester unless absolutely necessary due to potential risks to the fetus. In later trimesters, laparoscopy or laparotomy might be considered for large, symptomatic, or concerning cysts. The choice of procedure and timing depends on the specific circumstances and a thorough risk-benefit assessment. The risks of surgery are carefully weighed against the potential complications of leaving the cyst untreated.
Example: A pregnant woman presents with a large, rapidly growing ovarian cyst causing abdominal pain. An ultrasound reveals a complex cyst with suspicious features. After careful consideration and consultation with a specialist, a laparoscopic approach is chosen in the second trimester to remove the cyst and minimize risks to the pregnancy.
Q 17. What are the common causes of ovarian cysts?
Ovarian cysts are fluid-filled sacs on or within the ovaries. Several factors can lead to their development.
- Functional cysts: These are the most common type and are related to the normal menstrual cycle. Follicular cysts develop when a follicle (egg sac) fails to rupture and release an egg, while corpus luteum cysts form from the follicle after ovulation.
- Dermoid cysts (teratomas): These are benign cysts containing various tissues like hair, teeth, and fat.
- Endometriomas: These cysts are associated with endometriosis, a condition where endometrial tissue grows outside of the uterus.
- Cystadenomas: These are typically benign cysts that can be serous (watery fluid) or mucinous (thick, sticky fluid).
- Ovarian cancer: Although less common, ovarian cysts can sometimes be associated with malignant tumors.
Underlying factors: Hormonal imbalances, genetic predisposition, and pelvic inflammatory disease can contribute to the development of some types of ovarian cysts.
Q 18. How do you assess the risk of ovarian torsion in patients with ovarian cysts?
Ovarian torsion, the twisting of the ovary on its supporting ligaments, is a surgical emergency that can lead to ovarian ischemia and necrosis. The risk is significantly higher in patients with ovarian cysts, particularly large or complex ones.
Risk Assessment: Factors influencing the risk of torsion include:
- Cyst size and characteristics: Large or heavy cysts increase the risk of twisting.
- Mobility of the ovary: A more mobile ovary is at greater risk.
- History of torsion: Previous episodes increase the risk of recurrence.
- Pregnancy: Hormonal changes during pregnancy can increase the risk.
- Physical activity: Strenuous activity may increase the risk.
Clinical Presentation: Patients at high risk should be closely monitored for symptoms suggestive of torsion, such as sudden onset of severe pelvic pain, nausea, vomiting, and a palpable adnexal mass. Immediate medical attention is crucial if torsion is suspected.
Q 19. What are the criteria for referring a patient with an ovarian cyst to a specialist?
Referral to a specialist, such as a gynecologist or gynecologic oncologist, is warranted in several situations:
- Suspicion of malignancy: Ultrasound findings suggestive of cancer (e.g., solid components, irregular borders, ascites), or elevated CA-125 levels warrant immediate referral.
- Large or complex cysts: Cysts larger than 5-10cm, or those with complex internal features, require specialist evaluation.
- Symptomatic cysts: Persistent or severe pain, despite conservative management, indicates a need for specialist assessment.
- Failure to resolve: Functional cysts that persist for several months require further investigation.
- Age and reproductive plans: Premenopausal women with concerning cysts should be referred to discuss management options that consider their fertility.
Example: A 45-year-old woman with a 7cm complex ovarian cyst and elevated CA-125 levels should be urgently referred to a gynecologic oncologist for evaluation and management.
Q 20. Describe the process of obtaining informed consent for ovarian cyst surgery.
Obtaining informed consent for ovarian cyst surgery is a crucial ethical and legal step. The process involves a detailed discussion between the surgeon and the patient to ensure the patient understands the procedure, its risks, benefits, and alternatives.
Steps Involved:
- Diagnosis explanation: Clearly explain the diagnosis, including the nature and characteristics of the cyst.
- Procedure explanation: Describe the surgical procedure, including the type of anesthesia, surgical approach (laparoscopy or laparotomy), and potential complications.
- Risks and benefits: Discuss potential risks such as bleeding, infection, injury to adjacent organs, and the need for further surgery. Also, emphasize the benefits of surgery, including pain relief and prevention of complications.
- Alternatives: Explain alternative management options, such as watchful waiting or medical management.
- Question and answer session: Allow ample time for the patient to ask questions and express concerns.
- Documentation: Ensure proper documentation of the consent process, including the patient’s understanding and agreement to the procedure.
Example: Before a laparoscopic cystectomy, the surgeon thoroughly explains the procedure, including the small incisions, use of a camera, and potential risks like bleeding and infection. The patient is given a chance to ask questions and expresses her understanding before signing the consent form.
Q 21. How do you address patient anxiety and concerns related to ovarian cysts?
Addressing patient anxiety and concerns related to ovarian cysts is vital for optimal care. Many women experience fear and uncertainty when diagnosed with an ovarian cyst, particularly if there are concerns about malignancy or fertility.
Strategies for Addressing Anxiety:
- Empathetic listening: Actively listen to the patient’s concerns and validate their feelings.
- Clear and concise communication: Explain the diagnosis and management plan in a clear, understandable way, avoiding medical jargon.
- Provide reassurance: Reassure the patient that most ovarian cysts are benign and treatable. Explain the likelihood of different outcomes based on the specific type and characteristics of the cyst.
- Answer questions thoroughly: Address all the patient’s questions patiently and honestly.
- Personalized approach: Tailor the communication style to the patient’s individual needs and preferences.
- Follow-up and support: Provide information on support groups or resources for patients coping with ovarian cysts.
Example: A young woman anxious about the possibility of infertility after a cyst diagnosis is reassured that most functional cysts do not affect fertility. The doctor explains the management plan, answers her questions, and provides contact details for a support group if she feels the need.
Q 22. What are the latest advancements in the management of ovarian cysts?
Advancements in ovarian cyst management are constantly evolving, driven by improvements in imaging techniques, minimally invasive surgical approaches, and a deeper understanding of the underlying causes.
- Improved Imaging: High-resolution ultrasound, MRI, and CT scans allow for more precise diagnosis, better characterization of cysts (size, composition, blood flow), and accurate identification of potential complications, minimizing unnecessary surgeries.
- Minimally Invasive Surgery: Laparoscopic and robotic-assisted surgery are increasingly preferred over open surgery. These techniques lead to smaller incisions, reduced pain, shorter hospital stays, and faster recovery times. They also allow for better visualization, leading to more precise cyst removal.
- Targeted Medical Management: Advances in understanding hormonal imbalances associated with conditions like PCOS (Polycystic Ovary Syndrome) and endometriosis have led to more effective medical management strategies. This includes improved hormonal therapies and targeted medications to address the underlying cause and shrink or resolve cysts.
- Focus on Personalized Medicine: We are moving away from a one-size-fits-all approach. Treatment is becoming increasingly personalized based on factors such as the patient’s age, overall health, type of cyst, and desire for future fertility. For instance, a young woman wanting to preserve fertility might receive different management than a post-menopausal woman.
Q 23. Describe your experience with managing complex cases of ovarian cysts.
I have extensive experience managing complex ovarian cyst cases, including those with atypical features on imaging, large or complicated cysts requiring extensive surgical intervention, and cases involving comorbidities such as endometriosis or PCOS. For example, I recently managed a patient with a large endometrioma (a type of cyst filled with blood associated with endometriosis) that was causing significant pelvic pain and impacting her fertility. We opted for a laparoscopic excision, meticulously removing the cyst while preserving ovarian tissue to maximize her chances of future conception. Post-surgery, she received tailored hormonal therapy to manage her endometriosis and prevent recurrence. The outcome was excellent; the patient’s pain resolved, and she subsequently conceived naturally.
Another challenging case involved a patient with a large, complex ovarian cyst suspected to be malignant. Utilizing advanced imaging techniques and pre-operative markers, we were able to accurately assess the risk. We opted for a minimally invasive approach, performing a laparoscopic cystectomy (removal of the cyst). The pathology report confirmed a benign cyst, avoiding unnecessary extensive surgery. This highlights the importance of a cautious yet decisive approach in such situations.
Q 24. How do you stay current with the latest research and guidelines in ovarian cyst management?
Staying current is crucial in this rapidly evolving field. My approach is multi-faceted:
- Professional Organizations: Active membership in organizations such as the American College of Obstetricians and Gynecologists (ACOG) provides access to the latest guidelines, research updates, and continuing medical education opportunities.
- Peer-Reviewed Journals: I regularly review leading journals in reproductive endocrinology and infertility, gynecologic oncology, and minimally invasive surgery.
- Conferences and Workshops: Attending national and international conferences keeps me abreast of the most recent advancements in surgical techniques, diagnostic methods, and medical therapies.
- Online Resources: Reputable online platforms offer access to updated guidelines, research abstracts, and expert opinions.
This comprehensive approach ensures I consistently provide the most current and effective care to my patients.
Q 25. Explain your approach to documenting patient care related to ovarian cysts.
Meticulous documentation is paramount. My approach involves a structured system employing electronic health records (EHR) to ensure comprehensive and readily accessible information. This includes:
- Detailed History: Thorough documentation of the patient’s medical history, including menstrual cycles, previous surgeries, family history of ovarian cancer, and symptoms.
- Physical Examination Findings: Precise recording of the physical exam, including pelvic examination findings.
- Imaging Reports: Inclusion of all relevant imaging studies (ultrasound, MRI, CT) with detailed descriptions and interpretations.
- Diagnostic and Treatment Plans: Clear documentation of the diagnostic process, rationale behind the chosen management strategy (surgery, medication, or watchful waiting), and planned follow-up.
- Progress Notes: Regular updates reflecting the patient’s response to treatment, any complications, and modifications to the treatment plan.
- Surgical Reports: Detailed operative reports including specifics of the surgical technique employed, any complications encountered, and pathology results.
This ensures clarity, continuity of care, and facilitates communication among healthcare professionals.
Q 26. How do you ensure effective communication with other healthcare professionals involved in the care of a patient with an ovarian cyst?
Effective communication is crucial. I utilize several strategies:
- Direct Communication: I directly communicate with referring physicians, surgeons, and other specialists involved in the patient’s care through phone calls, secure messaging systems, and formal letters.
- Shared Electronic Health Records: Utilizing EHR systems allows for secure sharing of patient information with other healthcare providers, promoting collaborative decision-making.
- Formal Consultations: I schedule formal consultations when complex cases require input from multiple specialists. This allows for collaborative discussion and agreement on the optimal management strategy.
- Patient Involvement: I actively involve patients in the communication process, ensuring they understand their diagnosis, treatment plan, and any potential risks or complications.
This collaborative approach ensures seamless and effective care, minimizing misunderstandings and promoting the best possible patient outcomes.
Q 27. How do you handle unexpected complications during ovarian cyst surgery?
Unexpected complications during ovarian cyst surgery are addressed with a calm, decisive, and patient-centered approach. My strategy involves:
- Rapid Assessment: Immediate assessment of the nature and severity of the complication.
- Appropriate Intervention: Prompt and appropriate intervention, ranging from minor adjustments to the surgical technique to more extensive procedures like blood transfusion or conversion to open surgery if necessary.
- Teamwork: Collaboration with the surgical team, anesthesiologist, and other specialists to address the complication effectively.
- Post-operative Management: Intensive post-operative monitoring and management to minimize risks and ensure optimal recovery.
- Open Communication: Honest and transparent communication with the patient and their family regarding the complication, its management, and the expected outcome.
The key is to remain calm under pressure, utilize available resources effectively, and prioritize patient safety.
Q 28. What is your experience with managing ovarian cysts in patients with specific medical conditions (e.g., endometriosis, PCOS)?
Managing ovarian cysts in patients with endometriosis or PCOS requires a nuanced approach. In endometriosis, cysts (endometriomas) are often filled with old blood and require careful surgical removal, preserving ovarian tissue as much as possible. Post-surgical management often involves hormonal therapies to suppress endometriosis and prevent recurrence. In PCOS, cysts are often associated with hormonal imbalances. Management can involve lifestyle modifications (diet, exercise), weight management, and medication such as hormonal birth control pills or medications to regulate ovulation. The goal is not just to treat the cysts but also to address the underlying hormonal imbalances and improve overall reproductive health.
For instance, a patient with both endometriosis and PCOS might require a combination of laparoscopic surgery to remove endometriomas, followed by a personalized hormonal therapy regimen to manage both the endometriosis and hormonal irregularities associated with PCOS. Regular follow-up is crucial to monitor the patient’s response to treatment and make necessary adjustments. The focus is always on improving the patient’s symptoms, overall health, and fertility prospects, if desired.
Key Topics to Learn for Ovarian Cyst Management Interview
- Ovarian Cyst Types and Classification: Understanding the different types of ovarian cysts (follicular, corpus luteum, dermoid, endometrioma, etc.) and their characteristic features is crucial. Be prepared to discuss their diagnostic criteria and potential complications.
- Diagnosis and Imaging Techniques: Familiarize yourself with various diagnostic methods used to identify and characterize ovarian cysts, including transvaginal ultrasound, MRI, and CA-125 levels. Practice explaining the interpretation of imaging results and their clinical significance.
- Conservative Management Strategies: Master the principles of watchful waiting and the role of pain management in the non-surgical management of ovarian cysts. Understand when medical intervention is necessary and the appropriate medication choices.
- Surgical Management Techniques: Be prepared to discuss various surgical approaches to ovarian cyst management, including laparoscopy and laparotomy. Understand the indications for each procedure and potential risks and benefits.
- Post-operative Care and Follow-up: Learn about the importance of post-operative care, including pain management, infection prevention, and monitoring for complications. Be familiar with typical follow-up schedules and diagnostic tests.
- Differential Diagnosis and Related Conditions: Develop your ability to differentiate ovarian cysts from other conditions that present with similar symptoms, such as ectopic pregnancy, appendicitis, and pelvic inflammatory disease.
- Risk Factors and Prevention: Understand the known risk factors associated with ovarian cyst development and discuss strategies for prevention and early detection.
- Patient Counseling and Communication: Practice explaining complex medical information in a clear and concise manner to patients. Develop strategies for addressing patient concerns and providing emotional support.
Next Steps
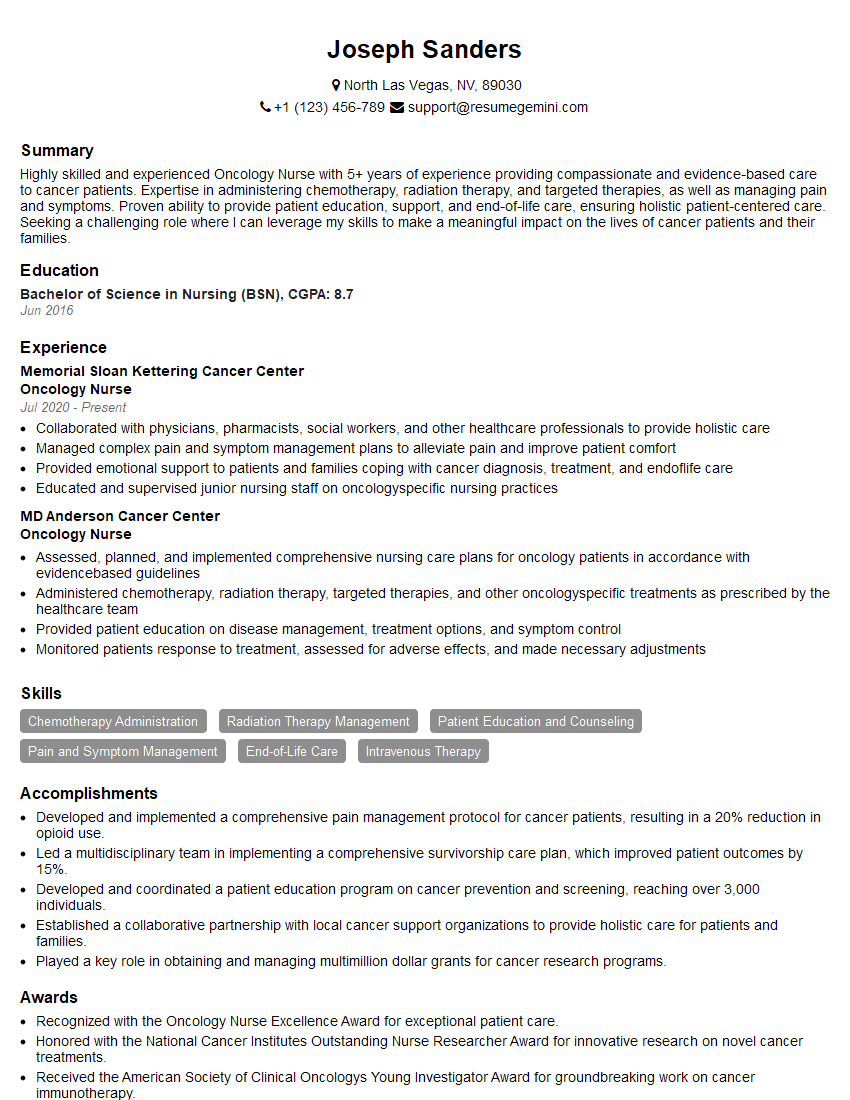
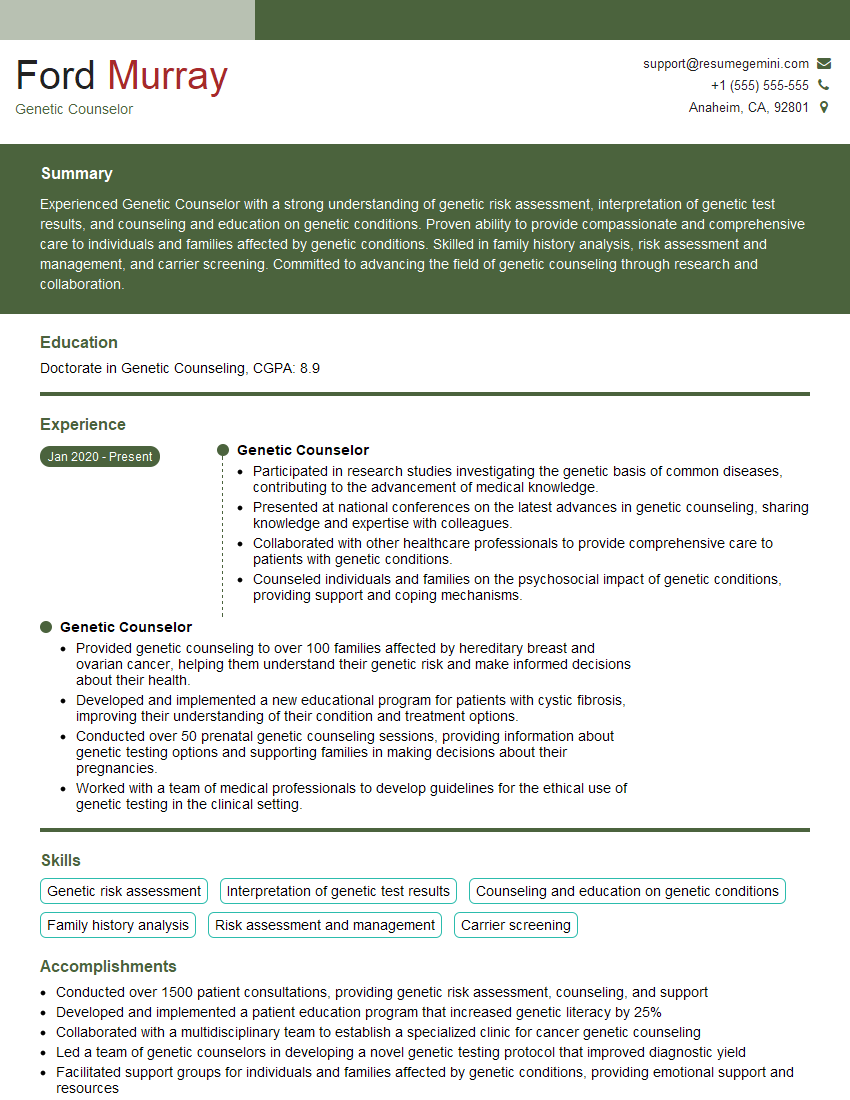
Mastering Ovarian Cyst Management is key to advancing your career in women’s health. A strong understanding of these concepts demonstrates expertise and commitment to patient care, making you a highly desirable candidate. To significantly boost your job prospects, focus on creating an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored to Ovarian Cyst Management to guide you through the process. Let us help you present yourself in the best possible light to prospective employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.