Preparation is the key to success in any interview. In this post, we’ll explore crucial Patient Chart Management and Organization interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Patient Chart Management and Organization Interview
Q 1. Describe your experience with different electronic health record (EHR) systems.
Throughout my career, I’ve gained extensive experience with a variety of EHR systems, including Epic, Cerner, and Meditech. My familiarity extends beyond basic data entry; I’m proficient in utilizing advanced features such as report generation, data analysis, and system customization. For instance, at my previous role, we transitioned from a legacy system to Epic. I played a key role in training staff, developing workflows, and ensuring a smooth transition, minimizing disruption to patient care. With each system, I’ve learned to adapt quickly, understanding the unique nuances and functionalities. I’m comfortable navigating different interfaces and readily adopt best practices to maximize efficiency and data integrity.
Working with Epic, I became adept at utilizing its robust reporting capabilities to track key metrics such as medication reconciliation rates and appointment adherence. This allowed us to identify areas for improvement and implement targeted interventions. My experience with Cerner involved optimizing the system’s workflow to reduce the time spent on documentation, leading to increased physician satisfaction and improved patient flow. In essence, my experience isn’t simply about using different systems; it’s about understanding how to leverage each system’s strengths to optimize patient care and streamline processes.
Q 2. How do you ensure patient data accuracy and integrity?
Ensuring patient data accuracy and integrity is paramount. My approach is multi-faceted and involves several key strategies. First, I meticulously follow established protocols for data entry, utilizing standardized terminology and double-checking all information before saving. Think of it like carefully proofreading a crucial document – attention to detail is key. Second, I regularly participate in audits and quality control checks to identify and correct any discrepancies or errors. This proactive approach prevents small mistakes from escalating into larger problems.
Third, I actively participate in continuous education and training to stay updated on best practices and regulatory requirements. Staying current on these changes is essential for maintaining data integrity. Finally, I utilize the built-in tools within the EHR systems – such as data validation checks and automated alerts – to flag potential errors and inconsistencies in real-time. This is comparable to using a spell-checker while writing – it helps catch errors before they become major issues. By employing a combination of careful data entry, regular audits, ongoing learning, and system-based tools, I contribute to a culture of accuracy and reliability in patient data management.
Q 3. Explain your process for managing patient chart requests.
Managing patient chart requests involves a structured and compliant process. First, I verify the requester’s identity and authorization to access the requested information, adhering strictly to HIPAA regulations. This initial step is crucial for protecting patient privacy. Next, I locate the requested chart, either electronically or physically. For electronic requests, I use the system’s search function, employing keywords or patient identifiers for efficient retrieval.
Once located, I review the request to ensure I’m providing only the necessary information and redacting any irrelevant or protected health information (PHI). This is where my knowledge of HIPAA guidelines is indispensable. Finally, I securely transmit the information to the requester using approved methods, keeping a detailed audit trail of every step. This includes documenting the request, the date of fulfillment, and the method of transmission. This meticulous process ensures compliance, maintains patient privacy, and provides a clear record of all chart access.
Q 4. What methods do you use to maintain the confidentiality of patient information?
Maintaining patient confidentiality is a top priority, and my approach involves a multi-layered strategy. First, I strictly adhere to all HIPAA regulations and facility policies regarding access, use, and disclosure of PHI. This isn’t simply a matter of compliance; it’s a fundamental ethical responsibility. Second, I use strong passwords and follow security protocols to protect electronic health records from unauthorized access. This includes logging out of the system when not in use and immediately reporting any suspicious activity.
Third, I only access patient information when necessary for legitimate clinical or administrative purposes. This is akin to a librarian carefully handling sensitive documents – only accessing what’s needed and handling it with appropriate care. Fourth, I’m meticulous about securing physical charts, storing them in locked cabinets or secure areas, accessible only to authorized personnel. In summary, safeguarding patient confidentiality is not just a procedure but a mindset that informs every aspect of my work.
Q 5. How do you prioritize tasks in a high-volume environment?
Prioritizing tasks in a high-volume environment requires a structured approach. I use a combination of techniques to manage my workload effectively. First, I utilize a task management system, often a combination of a digital calendar and a prioritized to-do list. This helps me visually organize my tasks and track progress. Secondly, I prioritize tasks based on urgency and importance, often using a matrix that categorizes tasks as urgent/important, important/not urgent, etc. This allows me to focus on time-sensitive requests while ensuring that crucial but less urgent tasks are not neglected.
Thirdly, I proactively communicate with colleagues and supervisors to manage expectations and ensure that I’m working on the most critical tasks. This collaborative approach ensures that everyone is on the same page. Finally, I regularly review my workload and adjust my priorities as needed. This flexibility is crucial in a dynamic environment, allowing me to adapt to changing circumstances and ensure that I’m always working on the most pressing tasks. It’s a balancing act, much like a conductor leading an orchestra, ensuring that all parts work in harmony to achieve a common goal.
Q 6. Describe your experience with chart audits and quality control measures.
I have extensive experience with chart audits and quality control measures. I’ve participated in both internal and external audits, reviewing patient charts for completeness, accuracy, and compliance with regulatory standards. These audits aren’t just about finding errors; they’re about identifying areas for improvement in our processes and ensuring that we are providing the highest quality of care. During these audits, I carefully review documentation for missing information, inconsistencies, or any deviations from established protocols.
For example, in a recent audit, I identified a trend of incomplete medication reconciliation documentation. This led to the implementation of a new checklist and training program to address this issue. This proactive approach to quality control ensures that we continuously improve our processes and maintain the highest standards of accuracy and compliance. The process is similar to a mechanic regularly inspecting a vehicle – identifying small issues early can prevent larger, more costly problems down the line.
Q 7. What is your experience with HIPAA regulations and compliance?
My understanding of HIPAA regulations and compliance is thorough and practical. I’m intimately familiar with the Privacy Rule, Security Rule, and Breach Notification Rule, and I consistently apply these regulations in my daily work. This includes understanding patient rights, implementing appropriate safeguards to protect PHI, and following proper procedures for handling data breaches. I’ve completed HIPAA training and remain current on any updates or changes to the regulations.
For example, I understand the importance of obtaining proper authorization before releasing patient information to third parties. I’m also knowledgeable about the different levels of PHI protection and implement appropriate security measures, both physical and electronic, to safeguard sensitive data. In essence, HIPAA compliance isn’t just a set of rules; it’s a fundamental principle guiding my work, ensuring that patient privacy is always prioritized.
Q 8. How do you handle discrepancies or missing information in patient charts?
Discovering discrepancies or missing information in patient charts is a critical aspect of ensuring accurate and comprehensive care. My approach involves a multi-step process. First, I meticulously review the chart for any inconsistencies or gaps, noting the specific missing data points. This might involve checking for missing lab results, incomplete medication lists, or absent progress notes. Second, I initiate a systematic search for the missing information. This could involve contacting the referring physician, reviewing other related medical records, or even requesting a repeat test if necessary. For example, if a crucial blood pressure reading is missing from a post-operative report, I would contact the surgical team directly to obtain the missing data. Third, I meticulously document all actions taken to locate and resolve the discrepancy, including dates, times, and individuals contacted. This detailed documentation provides an audit trail, which is vital for transparency and accountability. Finally, once the missing information is found, I update the patient chart with the new details. Any discrepancies that remain unresolved after thorough investigation are documented and flagged for further review by the appropriate medical personnel.
Q 9. Explain your experience with medical terminology and coding.
My experience with medical terminology and coding is extensive. I’ve worked with various coding systems, including ICD-10 and CPT codes, allowing me to accurately translate medical diagnoses and procedures into standardized codes. This ensures that patient data is consistently documented and readily accessible for billing, research, and epidemiological studies. For instance, I’m proficient in identifying the appropriate ICD-10 code for a patient’s diagnosis of pneumonia based on the specifics in their chart. Moreover, I can translate physician’s notes into structured data points allowing for efficient data analysis. I understand the nuances of medical language and can accurately interpret complex medical reports, ensuring that all relevant information is captured and organized effectively. This competence extends to understanding modifiers that affect the coding of services and ensures proper billing. For example, distinguishing between a routine office visit and a critical care visit requires nuanced understanding.
Q 10. Describe your proficiency in data entry and record-keeping software.
I’m proficient in several data entry and record-keeping software applications, including Epic, Cerner, and Meditech. My skills extend beyond basic data entry to include using advanced features within these systems like automated report generation, query creation, and data analysis. For example, I can efficiently utilize Epic’s SmartForms to capture and document patient data in a standardized manner. I’m also adept at using these systems to generate reports on various metrics such as patient demographics or treatment outcomes. Further, I understand the importance of data integrity and security, ensuring compliance with HIPAA regulations and maintaining confidentiality. I consistently utilize these systems to streamline workflows, improve accuracy, and enhance efficiency in managing patient records. I also regularly update my skills through professional development courses on new features and updates to the software systems. This ensures I maintain the highest level of competency and adapt to evolving technological advancements.
Q 11. How do you manage conflicting requests for patient information?
Managing conflicting requests for patient information requires a strong understanding of HIPAA regulations and the establishment of clear protocols. I always start by verifying the requester’s identity and authorization to access the patient’s information. This might involve reviewing their credentials or obtaining proper consent forms. For instance, if a family member requests access, I need to verify their relationship and assess if the patient has granted them access. Next, I carefully assess the request and its legitimacy. If a conflict arises between authorized individuals, I follow established organizational procedures to resolve the situation. This may involve escalating the issue to a supervisor or consulting the hospital’s legal counsel for guidance. Maintaining a detailed log of all information requests, the individuals who requested the information, and the actions taken, is essential for maintaining accountability and transparency. Documentation ensures protection against any misuse or unauthorized access to patient data.
Q 12. How do you organize and maintain both physical and digital patient charts?
Managing both physical and digital patient charts requires a comprehensive and organized system. For physical charts, I ensure that they are stored in a secure, easily accessible location, following a standardized filing system based on patient identification (e.g., alphabetical or numerical). Regular audits are conducted to ensure that charts are properly filed and readily retrievable. For digital charts, I leverage electronic health record (EHR) systems, using features like robust search functionalities and electronic filing to ensure quick and easy access. I use a color-coded tagging system within the EHR to highlight specific medical conditions or treatment plans for faster retrieval. Regular data backups and security protocols are employed to safeguard patient information. Moreover, both physical and digital charts are routinely checked for completeness and compliance with standards, ensuring data quality. For instance, I’d ensure all relevant lab results are associated with a particular patient’s digital file and that the physical chart is updated accordingly to mirror all the information.
Q 13. What strategies do you employ to improve efficiency in chart management?
Improving efficiency in chart management involves leveraging technology and implementing optimized workflows. This includes utilizing the EHR system’s features to automate tasks such as data entry, report generation, and scheduling. I also employ templates and standardized forms to expedite the documentation process. For example, using pre-populated forms for routine check-ups saves considerable time. Regular training on software updates and new functionalities keeps me updated and ensures efficient use of the systems. Moreover, I continually review and refine existing processes, identifying areas for improvement and implementing changes that streamline workflows. Working closely with other members of the healthcare team is essential to identify and eliminate bottlenecks and improve overall efficiency. For instance, implementing a system of shared inboxes and alerts to distribute tasks effectively can be transformative.
Q 14. Describe your experience with chart retrieval and filing systems.
My experience with chart retrieval and filing systems is extensive. I’m proficient in both manual and electronic systems. In manual systems, I’m adept at using various filing techniques, ensuring efficient chart retrieval and accurate record-keeping. With electronic systems, I efficiently navigate EHR software to retrieve charts, using advanced search filters and keywords to locate specific information quickly. I understand the critical importance of maintaining confidentiality and adhere to strict protocols to ensure patient privacy is maintained throughout the retrieval and filing processes. I’m also familiar with various chart organization methods such as alphabetic, numeric, or chronological sequencing depending on the specific requirements of the facility. My skills ensure that patient charts are consistently readily available when needed, supporting efficient patient care and minimizing delays.
Q 15. How do you ensure timely completion of chart preparation for audits or legal purposes?
Ensuring timely chart completion for audits or legal purposes requires a proactive and organized approach. Think of it like preparing for a meticulously planned event – you wouldn’t wait until the last minute! We need a robust system involving regular quality checks and a clearly defined timeline.
- Regular Chart Reviews: We conduct periodic reviews, perhaps monthly or quarterly depending on volume and regulatory requirements, to identify any missing documentation or discrepancies. This is like a pre-flight check for an airplane – identifying potential issues before they become major problems.
- Automated Reminders: Utilizing electronic health record (EHR) systems, we set up automated reminders for clinicians to complete documentation within a specific timeframe, say 48-72 hours post-patient encounter. This reduces the risk of critical information getting lost in the shuffle.
- Prioritization Matrix: We categorize chart preparation based on urgency and compliance needs. For instance, charts related to pending legal cases or high-risk patients are prioritized. This is like triage in an emergency room – attending to the most critical cases first.
- Designated Charting Specialist: In larger facilities, dedicated staff members are responsible for monitoring chart completion and follow-up. They act as air traffic controllers, ensuring smooth and efficient workflows.
This multi-faceted approach ensures that charts are not only complete but also consistently accurate, minimizing the risk of delays and potential issues during audits or legal proceedings.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with chart reconciliation processes?
Chart reconciliation is the process of verifying that all documentation related to a patient’s care is accurately accounted for and matches the patient’s medical record. Imagine it as balancing your checkbook – ensuring all transactions are recorded accurately. My experience includes:
- EHR Reconciliation: I’m proficient in using EHR systems to compare data from different sources – such as lab results, radiology reports, and nursing notes – to identify any discrepancies or missing information. This often involves using reporting tools and data analytics to pinpoint inconsistencies.
- Paper Chart Reconciliation: In situations involving legacy paper charts, I have experience meticulously reviewing each document, cross-referencing against other sources, and creating a comprehensive record. This requires patience, accuracy, and a keen eye for detail.
- Identifying and Resolving Discrepancies: When discrepancies arise, I follow established protocols to investigate the cause and ensure accurate correction. This might involve contacting the relevant clinicians or departments to clarify information.
Effective reconciliation ensures the integrity and accuracy of patient records, which is critical for patient safety and legal compliance.
Q 17. How familiar are you with different types of medical records (e.g., paper, electronic, imaging)?
My familiarity with various medical record types is extensive, encompassing paper, electronic, and imaging formats. Each requires a different approach to management and organization.
- Paper Records: I’m adept at managing paper-based systems, including filing, retrieval, storage, and archiving, following strict confidentiality protocols. Think of this as being a skilled librarian, knowing exactly where to locate specific information.
- Electronic Health Records (EHRs): I possess significant experience with various EHR systems, including data entry, management, querying, and reporting. My proficiency extends to utilizing EHR’s advanced features to enhance organization and retrieval efficiency. It’s like navigating a sophisticated database, utilizing advanced search functions to locate the exact information needed.
- Medical Imaging: My experience includes managing and retrieving medical images such as X-rays, CT scans, and MRIs using Picture Archiving and Communication Systems (PACS). This involves understanding image formats, metadata, and integration with EHRs. It’s like being a digital curator for medical images, ensuring their secure storage and easy access for healthcare professionals.
Regardless of the format, my approach prioritizes accuracy, security, and efficient retrieval of patient information.
Q 18. Describe your experience with release of information procedures.
Release of information (ROI) procedures involve carefully managing the dissemination of protected health information (PHI) to authorized individuals or entities. This is a critical area demanding strict adherence to regulations like HIPAA.
- Authorization Verification: Before releasing any information, I meticulously verify the authenticity of the request and the authorization provided by the patient. This is a critical step to prevent unauthorized access.
- Data Redaction: When appropriate, I redact protected health information that is not relevant to the request, safeguarding patient privacy. It’s like carefully editing a document to remove any unnecessary details.
- Secure Transmission: I utilize secure methods for transmitting PHI, such as encrypted email or secure portals, protecting against unauthorized access during transfer. This ensures the information remains confidential in transit.
- Maintaining Accurate Records: I diligently maintain records of all ROI requests and responses, which is crucial for auditing and compliance purposes. It’s like keeping a meticulous log of all transactions, maintaining accountability and transparency.
My experience ensures compliance with legal and ethical requirements while efficiently facilitating legitimate information requests.
Q 19. How do you handle requests for amendments or corrections to patient charts?
Requests for amendments or corrections to patient charts are handled with utmost care and precision, following strict protocols to ensure accuracy and compliance. Think of this as editing a crucial document, ensuring every detail is correct.
- Verification of Request: First, I verify the legitimacy of the request, ensuring it comes from an authorized source, often the patient themselves or their legal representative.
- Documentation Review: I carefully review the original documentation and the proposed correction, assessing the validity of the amendment.
- Amendment Process: The amendment is documented using the appropriate methods within the EHR or paper system, preserving the original entry while clearly indicating the correction. It’s like using “track changes” in a document, preserving the original while clearly showing the changes made.
- Clinical Oversight: In some cases, clinical oversight or review may be required before the amendment is accepted, ensuring the correction is medically sound.
The process emphasizes accuracy, transparency, and compliance with all applicable regulations.
Q 20. Explain your understanding of data security and privacy best practices.
Data security and privacy are paramount in patient chart management. Think of it as safeguarding a highly valuable asset – patient information is confidential, sensitive, and legally protected.
- HIPAA Compliance: I’m well-versed in HIPAA regulations and other privacy laws, understanding my responsibilities in protecting PHI. This includes the implementation of physical, administrative, and technical safeguards.
- Access Control: I strictly adhere to access control policies, ensuring only authorized personnel can access patient information based on their roles and responsibilities. This is like using a key to a secure vault – only those with authorization can gain entry.
- Data Encryption: I understand the importance of data encryption both at rest and in transit, protecting patient information from unauthorized access even in case of data breaches. This is like using a strong lock and key to secure a precious item.
- Regular Security Training: I actively participate in regular security awareness training to stay abreast of evolving threats and best practices. This is like maintaining a well-maintained security system, regularly updated and improved.
My commitment to data security and privacy ensures the protection of sensitive patient information.
Q 21. How do you manage large volumes of patient data effectively?
Managing large volumes of patient data effectively requires a strategic and technology-driven approach. Imagine organizing a vast library – efficient systems are crucial. My methods include:
- EHR Optimization: I leverage the full potential of the EHR system, utilizing its advanced search, filtering, and reporting features to efficiently retrieve and analyze data. It’s like using a powerful search engine to find specific information within a vast database.
- Data Analytics: I utilize data analytics tools to identify trends, patterns, and insights within patient data, which helps improve quality of care and operational efficiency. This is like using advanced tools to get a clearer picture of a complicated dataset.
- Workflow Automation: I advocate for the use of automated workflows, reducing manual data entry and enhancing efficiency. It’s like streamlining a process – reducing the time and effort involved.
- Cloud-Based Solutions: Where appropriate, I advocate for leveraging cloud-based solutions for secure data storage and access, providing scalability and reducing storage burden. This is like using cloud storage to store large files – easily accessible and well-organized.
This multifaceted strategy ensures that large datasets are not just manageable but also readily accessible for analysis and operational decision-making.
Q 22. Describe your experience working within a team environment in medical records.
Throughout my career, teamwork has been paramount in medical records. I’ve consistently collaborated with physicians, nurses, coders, and other healthcare professionals to ensure efficient and accurate chart management. For example, in my previous role at City General Hospital, our team utilized a sophisticated electronic health record (EHR) system. We held regular meetings to address workflow challenges, streamline processes (such as chart completion protocols), and improve communication. We even created an internal knowledge base wiki to document best practices and troubleshoot common issues. This collaborative approach fostered a supportive and high-performing environment where individual strengths complemented each other, resulting in improved patient care and reduced administrative burden.
- Improved Chart Completion Rates: Our collaborative efforts resulted in a 15% increase in timely chart completion rates.
- Reduced Errors: By standardizing processes, we saw a 10% decrease in chart-related errors.
Q 23. What is your understanding of the legal implications of improper chart management?
Improper chart management carries significant legal ramifications. HIPAA violations, for instance, can lead to substantial fines and reputational damage for healthcare organizations. Failing to maintain accurate and complete records can compromise patient care and result in medical malpractice lawsuits. Incomplete or inaccurate documentation can lead to misdiagnosis, improper treatment, and ultimately, harm to the patient. Legal repercussions extend to potential criminal charges in cases of intentional falsification or destruction of records. The penalties vary widely depending on the severity and nature of the violation, the state, and the specific regulations involved.
Think of it like this: medical charts are legal documents. They’re crucial evidence in any dispute involving patient care. A poorly managed chart weakens a healthcare provider’s defense in a malpractice suit. Conversely, meticulous and accurate chart management provides a strong defense against claims of negligence.
Q 24. How would you address a situation where a patient’s chart is incomplete or missing vital information?
Discovering an incomplete or missing vital information in a patient’s chart requires immediate action. My approach would involve several steps:
- Identify the Missing Information: First, I’d determine precisely what information is missing and its clinical significance. Is it a crucial lab result? A vital sign? A medication allergy? The severity of the missing information dictates the urgency of the response.
- Contact the Relevant Provider: I’d immediately contact the physician, nurse, or other healthcare professional responsible for providing the missing information. I would explain the situation and the need for immediate attention to rectify the issue.
- Document the Deficiency: I’d meticulously document the missing information, including the date, time, and the attempts made to retrieve it. This documentation provides an audit trail of the issue and the steps taken to resolve it.
- Implement Corrective Actions: Depending on the missing information and its urgency, I would escalate to the appropriate supervisor if the information cannot be obtained promptly. This may involve reviewing other documentation or contacting external facilities if necessary.
- Ensure Data Integrity: Upon receiving the missing information, I’d ensure its accuracy and proper entry into the patient’s electronic health record. Once updated, I would verify the completeness of the chart.
It’s crucial to follow established procedures and maintain a paper trail detailing all attempts to address the deficiency. This thorough approach helps to prevent future errors and mitigate potential legal risks.
Q 25. What is your experience with medical record retention policies and procedures?
My experience with medical record retention policies and procedures is extensive. I’m familiar with both state and federal regulations, including HIPAA, which dictates how long medical records must be kept and the appropriate methods of storage and disposal. I understand the importance of adhering to these policies to maintain patient confidentiality and comply with legal requirements. In my past roles, I have been directly responsible for implementing, monitoring, and ensuring compliance with our organization’s retention policies, including secure physical and electronic storage, regular audits, and systematic destruction of records according to established timelines.
For example, at County Medical Center, I assisted in transitioning our record-keeping system from a primarily paper-based system to a fully electronic one. This involved developing and implementing protocols for both the secure transition of existing physical records and the ongoing management of the electronic data, which included establishing a secure data backup and disaster recovery plan.
Q 26. How do you stay current with changes in healthcare regulations and technology?
Staying current in healthcare is crucial. I utilize several strategies:
- Professional Organizations: I am an active member of the American Health Information Management Association (AHIMA), attending conferences and webinars to stay abreast of regulatory changes and technological advancements.
- Continuing Education: I regularly pursue continuing education courses and certifications to maintain my knowledge and skills in patient chart management and EHR systems.
- Industry Publications: I subscribe to relevant journals and online resources, such as HIMSS (Healthcare Information and Management Systems Society) publications, to stay updated on industry trends and best practices.
- Online Resources: I utilize reputable online resources to learn about the latest EHR systems and data security protocols.
This multi-faceted approach ensures I maintain a high level of expertise in the ever-evolving field of healthcare.
Q 27. Describe a time you had to resolve a conflict related to patient chart access.
In one instance, a disagreement arose regarding access to a patient’s chart between a physician and a family member. The physician argued for restricted access due to the sensitive nature of the information, while the family member insisted on full access based on their relationship. I addressed this conflict by first reviewing the hospital’s policy on patient chart access and confidentiality. Then, I mediated a discussion between the physician and family member, clarifying the hospital’s policies and emphasizing the importance of maintaining patient confidentiality while balancing the family’s need for information.
We arrived at a compromise where the physician provided the family with a summary of the patient’s condition without disclosing protected health information (PHI). This solution respected both the physician’s responsibility to maintain confidentiality and the family’s desire for updates. I documented the entire process and the agreed-upon solution, ensuring a clear record of the resolution.
Q 28. How would you handle a situation where you identify a potential breach of patient confidentiality?
Identifying a potential breach of patient confidentiality is a serious matter. My immediate actions would be:
- Assess the situation: I’d first determine the nature and extent of the potential breach. Was PHI accidentally disclosed? Was there unauthorized access?
- Report the incident: I would immediately report the suspected breach to my supervisor and the organization’s designated privacy officer, following established internal protocols.
- Initiate corrective actions: This might involve disabling accounts, changing passwords, or conducting a thorough investigation to determine the cause of the breach and prevent future occurrences.
- Follow established procedures: I would diligently follow the organization’s procedures for handling breaches, which typically include documenting the incident, notifying affected patients, and potentially reporting to regulatory agencies (like the OCR) as required.
- Participate in the investigation: I’d fully cooperate with any internal or external investigation into the breach. My role would be to provide information and assist in rectifying the situation.
Protecting patient confidentiality is paramount. A prompt and thorough response to a suspected breach minimizes potential harm and demonstrates a commitment to data security and patient well-being.
Key Topics to Learn for Patient Chart Management and Organization Interview
- Data Integrity and Accuracy: Understanding the critical importance of maintaining accurate and complete patient information, including methods for error detection and correction.
- Charting Best Practices: Applying standardized charting methods (e.g., SOAP notes, problem-oriented medical records) to ensure clarity, consistency, and legal compliance.
- HIPAA Compliance and Confidentiality: Demonstrating knowledge of HIPAA regulations and applying appropriate security measures to protect patient privacy and sensitive health information.
- Electronic Health Record (EHR) Systems: Familiarity with various EHR systems, their functionalities (e.g., scheduling, billing, reporting), and efficient navigation techniques.
- Medical Terminology and Abbreviations: Proficiency in understanding and utilizing medical terminology and common abbreviations to effectively manage and interpret patient data.
- Organization and Retrieval Methods: Implementing efficient filing, indexing, and retrieval systems for both physical and electronic patient charts, ensuring quick access to necessary information.
- Data Analysis and Reporting: Understanding how to extract meaningful information from patient charts for reporting purposes, identifying trends, and supporting clinical decision-making.
- Problem-Solving and Troubleshooting: Demonstrating the ability to identify and resolve issues related to chart management, such as missing information, inconsistencies, or system errors.
- Workflow Optimization: Analyzing current processes and proposing improvements to enhance efficiency and reduce redundancies in patient chart management.
- Regulatory Compliance and Audits: Understanding relevant regulations and participating in audits to ensure adherence to standards and best practices.
Next Steps
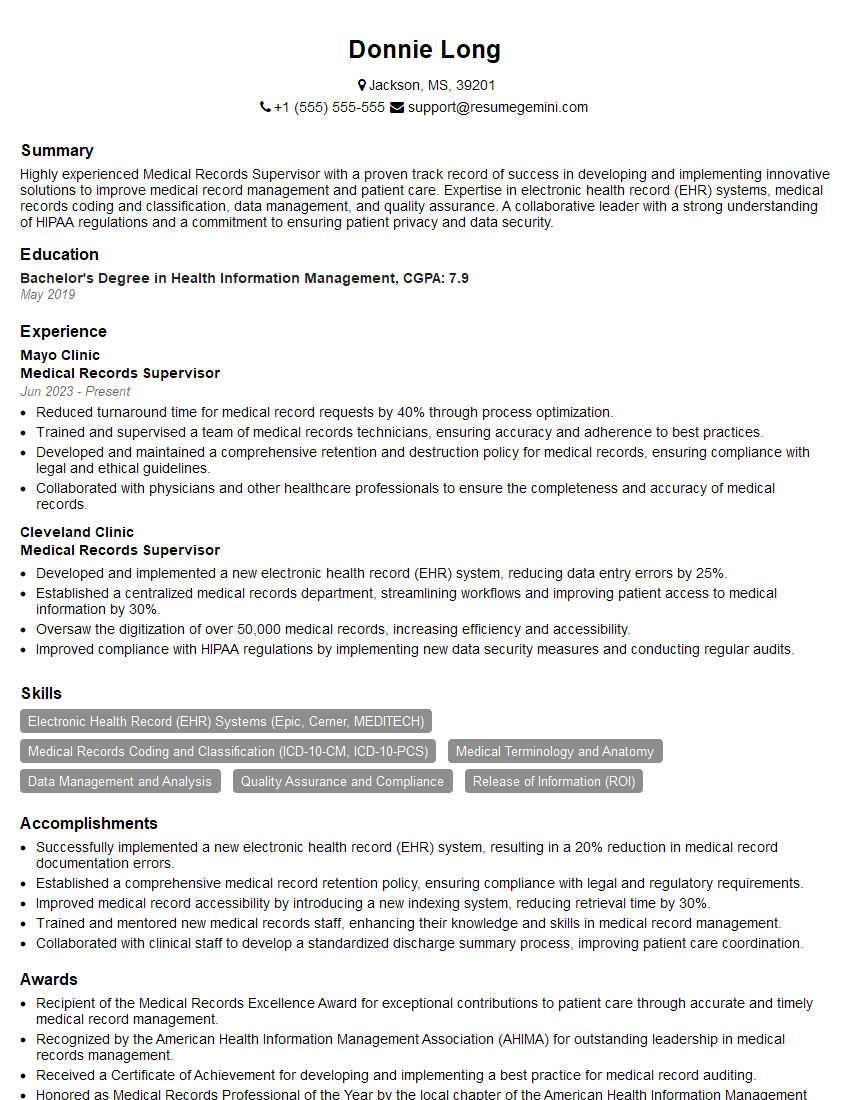
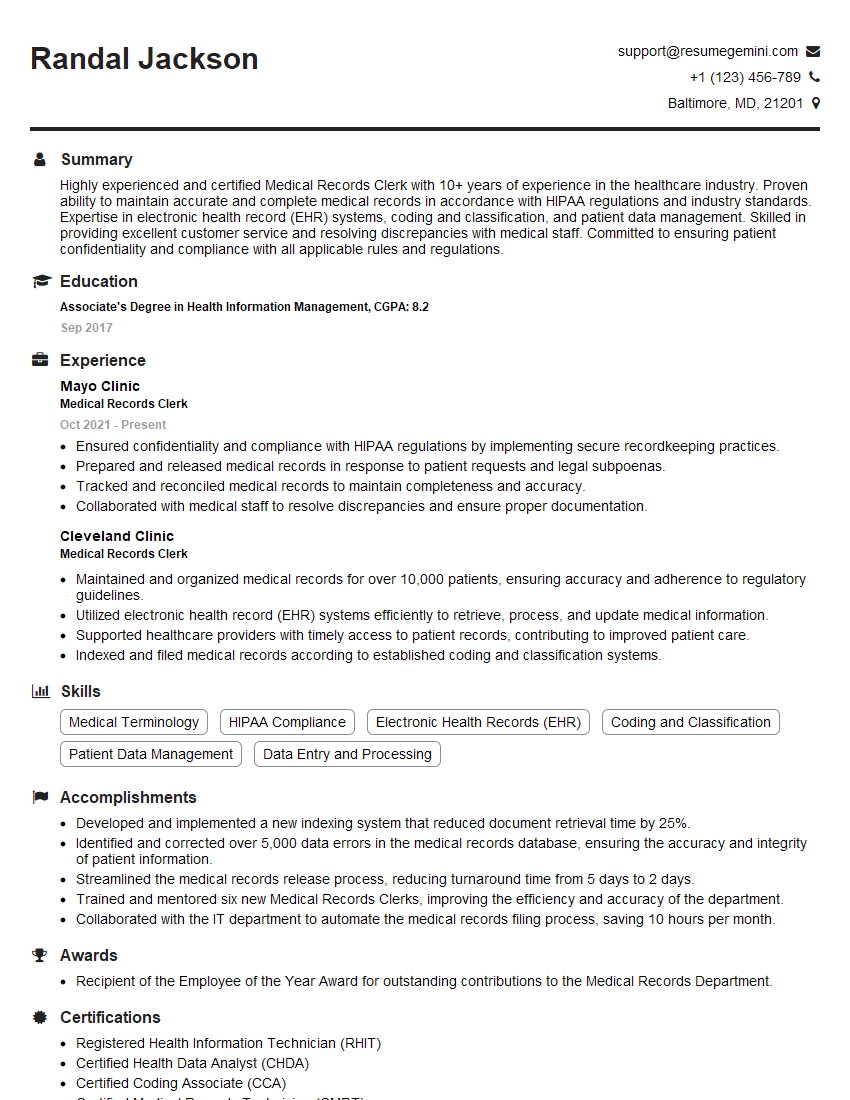
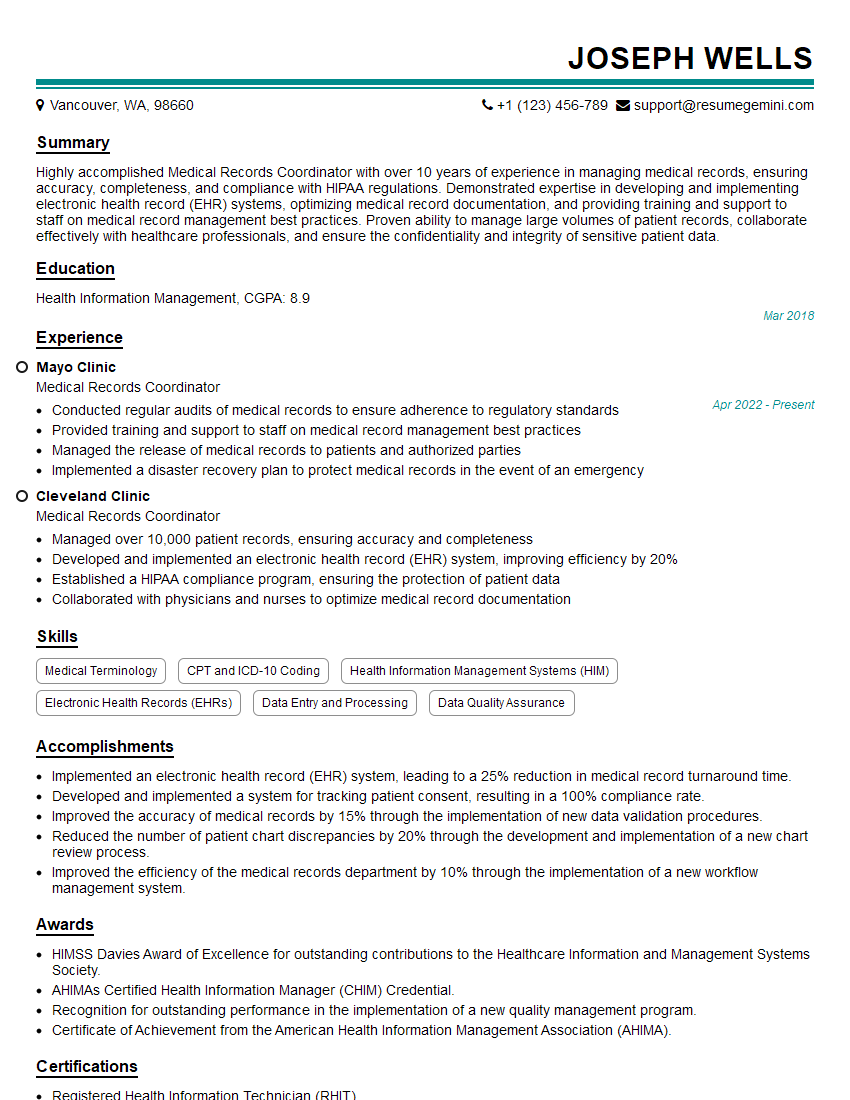
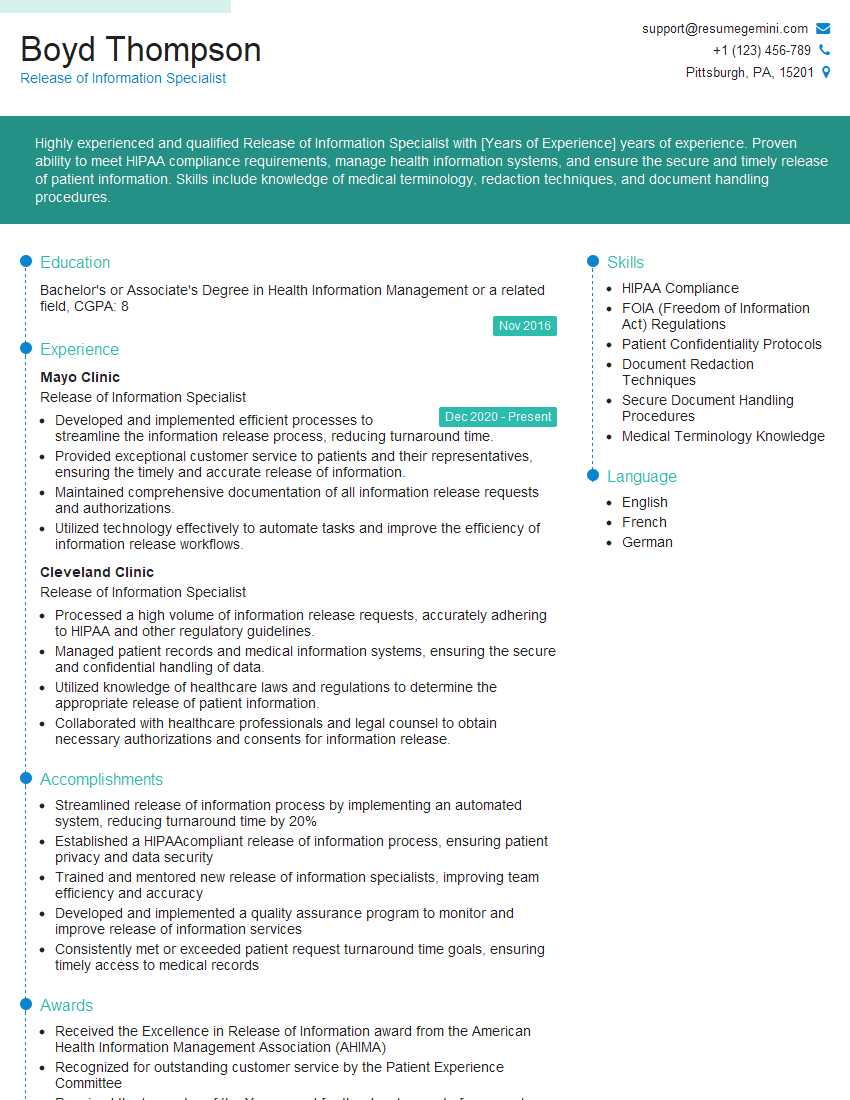
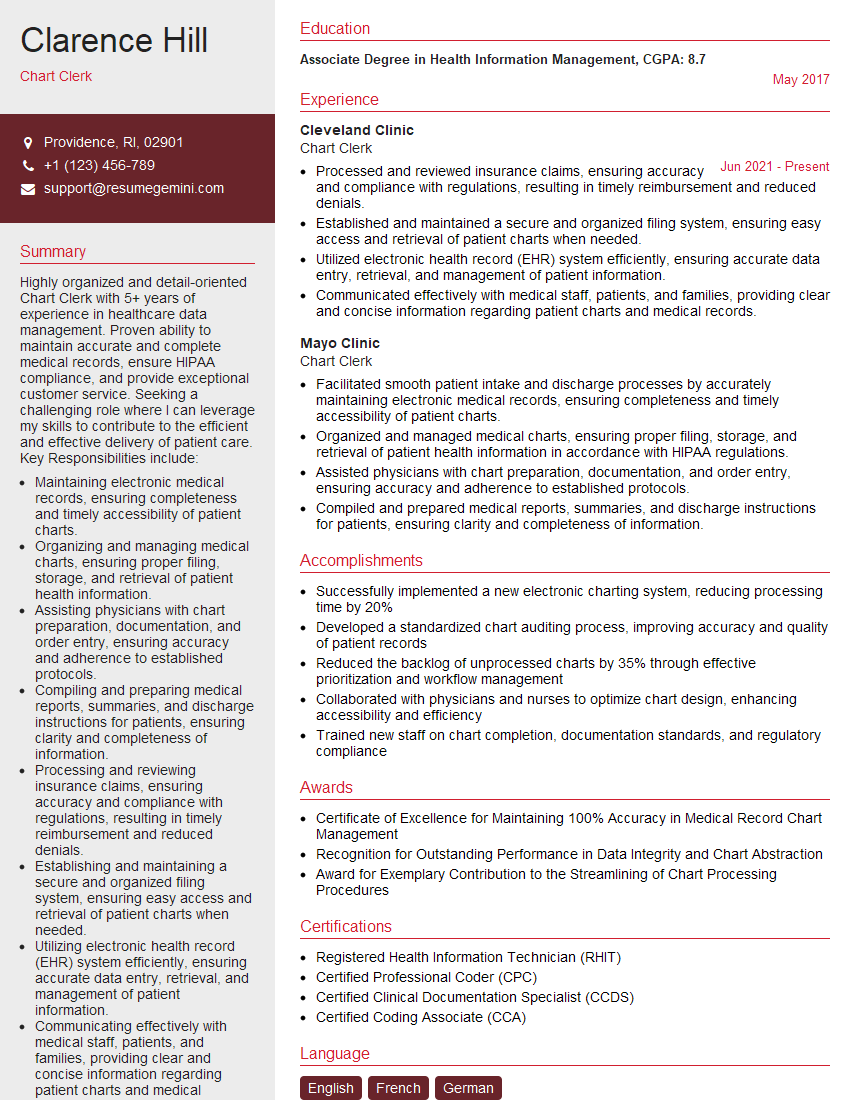
Mastering Patient Chart Management and Organization is crucial for career advancement in healthcare. A strong understanding of these principles demonstrates professionalism, efficiency, and commitment to patient care – all highly valued qualities in today’s competitive job market. To significantly boost your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored specifically to Patient Chart Management and Organization to help guide you. Invest the time to craft a compelling resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.