Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Pediatric Neuro-Pathology interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Pediatric Neuro-Pathology Interview
Q 1. Describe the histological features of periventricular leukomalacia.
Periventricular leukomalacia (PVL) is a form of white matter injury affecting premature infants. Histologically, it’s characterized by necrosis and gliosis in the periventricular white matter. Think of it as damage to the brain’s ‘wiring’ near the ventricles (fluid-filled spaces).
- Necrosis: We see areas of dead white matter, appearing as cystic spaces or rarefaction (thinning) on microscopy. These areas represent the sites of initial injury.
- Gliosis: This refers to the reactive proliferation of glial cells (astrocytes and microglia) in response to the damage. It’s like the brain’s attempt to ‘clean up’ the mess, but this often results in scarring.
- Inflammation: There might be evidence of an inflammatory response, with infiltration of inflammatory cells like macrophages and lymphocytes.
- Myelin loss: The myelin sheaths, which insulate nerve fibers, are disrupted or absent in the affected areas. This impacts the efficiency of nerve signal transmission.
Imagine a garden hose with holes in it – the water (nerve impulses) leaks out, affecting the brain’s function. PVL’s severity varies, leading to different neurological outcomes ranging from subtle developmental delays to severe cerebral palsy.
Q 2. Explain the diagnostic criteria for Tay-Sachs disease on a neuropathological level.
Tay-Sachs disease is a lysosomal storage disorder, meaning there’s a build-up of a specific substance within the cells due to an enzyme deficiency (β-hexosaminidase A). Neuropathologically, the hallmark is the accumulation of GM2 ganglioside within neurons. This leads to widespread neuronal damage and progressive neurodegeneration.
- Microscopic Findings: Microscopy reveals swollen neurons with a foamy or vacuolated cytoplasm due to the accumulated GM2 ganglioside. The neurons appear ‘ballooned’.
- Macroscopic Findings: Macroscopically (with the naked eye), we often observe a reduced brain size (microcephaly) and a pale, grayish appearance of the cerebral cortex. The cerebellum may also be affected.
- Cherry-red spot: Although a clinical rather than strictly neuropathological finding, the ‘cherry-red spot’ seen in the macula of the eye is characteristic and related to the same lysosomal storage problem.
It’s crucial to understand that these neuropathological changes are progressive and result in severe neurological dysfunction, ultimately leading to death. The diagnostic confirmation often relies on genetic testing in addition to the neuropathological findings.
Q 3. Differentiate between the neuropathological findings in Tuberous Sclerosis Complex and neurofibromatosis.
Tuberous sclerosis complex (TSC) and neurofibromatosis (NF) are both neurocutaneous disorders – meaning they affect both the nervous system and the skin. However, their neuropathological features differ significantly.
- TSC: Characterized by the presence of cortical tubers (dysplastic cortical lesions) which are abnormal growths of brain tissue. Subependymal giant cell astrocytomas (SEGAs) are also common, occurring in the ventricles. Histologically, tubers show disorganized neuronal and glial architecture. Imagine a poorly-constructed building—the cells are in the wrong places.
- NF: Characterized primarily by the presence of neurofibromas, which are benign tumors of the peripheral nerves. These are composed of Schwann cells and fibroblasts. These tumors can grow along nerves throughout the body, including those within the brain. Central nervous system involvement can include optic pathway gliomas and other less common tumors.
In essence, TSC primarily involves malformations of brain tissue, while NF mainly involves peripheral nerve tumors. While both involve tumors, their locations and histological compositions distinguish them completely. Imaging studies often play a crucial role in establishing the diagnosis alongside the neuropathological findings.
Q 4. Discuss the role of genetic testing in pediatric neuropathology.
Genetic testing has revolutionized pediatric neuropathology. It plays a crucial role in diagnosis, prognosis, and management of many neurological disorders. It helps us identify the underlying genetic defects that cause various conditions.
- Diagnostic Confirmation: Many genetic disorders manifest with overlapping clinical and neuropathological features. Genetic testing helps provide a definitive diagnosis when morphology alone may be insufficient.
- Prognostic Information: The specific genetic mutation can provide insights into the disease’s severity and likely progression, aiding in treatment planning.
- Family Counseling: Genetic testing allows for pre-symptomatic testing in family members at risk, facilitating informed decisions about family planning and preventative measures.
- Targeted therapies: Identification of the underlying genetic mutation sometimes allows for more targeted therapies to be considered.
For example, in cases of suspected lysosomal storage disorders or mitochondrial disorders, genetic testing is often crucial for precise identification and guiding the care team. It improves patient care by ensuring we’re treating the root cause, rather than only the symptoms.
Q 5. What are the key histological differences between pilocytic astrocytoma and glioblastoma in children?
Pilocytic astrocytoma and glioblastoma are both glial tumors (tumors arising from glial cells), but they differ significantly in their histological features and behavior.
- Pilocytic Astrocytoma: These are generally low-grade tumors, often seen in children. Histologically, they are characterized by a biphasic pattern: areas of spindle-shaped cells and Rosenthal fibers (eosinophilic, corkscrew-shaped structures) and areas of more loosely arranged cells. The cells often show minimal nuclear atypia (abnormalities in cell nuclei). They have a slow-growing, benign nature.
- Glioblastoma: These are high-grade, aggressive tumors with a very poor prognosis. Histologically, they demonstrate marked cellularity (high density of cells), significant nuclear atypia (abnormal nuclei), high mitotic activity (frequent cell divisions), and necrosis (cell death). They infiltrate surrounding brain tissue aggressively, making complete surgical removal difficult.
Imagine a well-organized garden (pilocytic astrocytoma) versus an overgrown, chaotic weed patch (glioblastoma). The histological features reflect the difference in their growth patterns and clinical behavior. The distinction is crucial for guiding treatment approaches, which differ significantly for low-grade versus high-grade tumors.
Q 6. Explain the pathogenesis of neonatal hypoxic-ischemic encephalopathy.
Neonatal hypoxic-ischemic encephalopathy (HIE) refers to brain damage caused by a lack of oxygen and blood flow to the brain during birth. The pathogenesis is complex and involves several mechanisms:
- Energy Failure: Deprivation of oxygen leads to mitochondrial dysfunction, disrupting ATP production. This results in neuronal energy depletion and eventual cell death.
- Excitotoxicity: The lack of oxygen triggers excessive release of excitatory neurotransmitters like glutamate. This overstimulation damages neurons and glial cells.
- Oxidative Stress: The lack of oxygen causes an imbalance between the production of reactive oxygen species (ROS) and the brain’s antioxidant defense mechanisms. ROS then causes damage to cellular components.
- Inflammation: The brain’s response to injury includes an inflammatory cascade, which further contributes to neuronal damage.
These processes are interconnected and lead to varying degrees of brain injury, from subtle white matter damage (similar to PVL) to widespread cortical necrosis. The severity of the injury depends on the duration and extent of the hypoxic-ischemic insult.
Q 7. Describe the neuropathological hallmarks of Alexander disease.
Alexander disease is a rare, progressive leukodystrophy (a disorder affecting the brain’s white matter) caused by mutations in the GFAP gene. The key neuropathological hallmarks involve the abnormal accumulation of glial fibrillary acidic protein (GFAP).
- Rosenthal fibers: These are eosinophilic, corkscrew-shaped aggregates of GFAP that are the characteristic finding in Alexander disease. They are found within astrocytes in both the white and gray matter.
- Astrocytic changes: Astrocytes show various morphological changes, including hypertrophy (enlargement) and abnormal cytoplasmic inclusions.
- White matter changes: There’s varying degrees of white matter demyelination (loss of myelin sheaths) and gliosis, leading to diffuse or focal areas of brain atrophy.
These changes cause progressive neurological dysfunction, affecting motor skills, cognitive abilities, and speech. The severity and distribution of the Rosenthal fibers are crucial in making the diagnosis. The abnormal GFAP accumulation is the central pathogenic mechanism, leading to astrocytic dysfunction and eventual widespread neurological impairment.
Q 8. How do you approach the diagnosis of a pediatric brain tumor based on histopathology?
Diagnosing pediatric brain tumors through histopathology is a multi-step process requiring meticulous examination of tissue samples under a microscope. We begin with assessing the overall architecture of the tumor – is it well-circumscribed or infiltrative? What is the cellularity (density of cells)? Then we move to the microscopic features of the individual cells. We examine their size, shape, nuclear characteristics (size, shape, chromatin pattern), and the presence of any mitotic figures (cells undergoing division) which indicates tumor aggressiveness. We also look for specific features like the presence of Rosenthal fibers (seen in pilocytic astrocytomas), Homer-Wright rosettes (seen in medulloblastomas), or psammoma bodies (seen in meningiomas). This visual assessment is crucial for initial classification.
For example, a highly cellular tumor with many mitotic figures and pleomorphic (irregularly shaped) cells might suggest a high-grade glioma, requiring more aggressive treatment. Conversely, a well-circumscribed tumor with fewer mitotic figures and uniform cells might point towards a low-grade glioma with a better prognosis. Finally, ancillary studies such as immunohistochemistry (IHC) and molecular testing are essential for precise diagnosis and subtyping, providing additional markers and genetic information to confirm the initial impression from the histological examination.
Q 9. What are the common causes of pediatric stroke, and how do they manifest neuropathologically?
Pediatric stroke, while less common than in adults, carries significant long-term consequences. The causes differ significantly from adult strokes, with congenital and acquired conditions playing key roles. Congenital causes include arteriovenous malformations (AVMs), where abnormal connections between arteries and veins bypass the capillary bed, leading to bleeding and ischemia (lack of blood flow). Another example is moyamoya disease, a rare condition with progressive narrowing of the arteries at the base of the brain.
Acquired causes are mainly related to infections (e.g., bacterial meningitis leading to vascular inflammation and thrombosis), dehydration, blood disorders, and cardiac issues. Neuropathologically, ischemic strokes (caused by blockage) show areas of neuronal necrosis (cell death), with evidence of inflammation and microglial activation. Hemorrhagic strokes (caused by bleeding) present with areas of hemorrhage and edema (swelling) depending on the location and extent of bleeding. The long-term consequences of both are scarring, gliosis (reactive glial cell proliferation), and varying degrees of neurological deficits.
Q 10. Discuss the challenges in diagnosing childhood neurodegenerative diseases.
Diagnosing childhood neurodegenerative diseases is challenging due to several factors. Firstly, the clinical presentation can be subtle and non-specific in early stages. Many symptoms, like developmental delay or motor incoordination, overlap with other childhood conditions. Secondly, the underlying genetic and molecular mechanisms are often complex and diverse, with considerable genetic heterogeneity even within the same disease entity. This makes genetic testing alone not always sufficient for diagnosis.
Thirdly, obtaining brain tissue samples for definitive pathological examination is rarely feasible. Brain biopsies carry significant risks, are invasive, and are not always diagnostic. Therefore, we rely heavily on clinical presentation, neuroimaging (MRI, CT), and ancillary investigations like metabolic testing and electroencephalography (EEG). Finally, the progression of these diseases can be slow and variable, making it difficult to establish a clear diagnosis early in the disease course and monitor effective treatment responses. A multidisciplinary approach involving neurologists, geneticists, and neuropathologists is crucial for optimal care.
Q 11. Explain the role of immunohistochemistry in pediatric neuropathology.
Immunohistochemistry (IHC) is an indispensable tool in pediatric neuropathology. It utilizes antibodies that specifically bind to certain proteins or antigens within the cells. By visualizing the location and intensity of these antigens, we can gain valuable information about the cell type, lineage, and differentiation status of the tumor or affected tissue.
For example, glial fibrillary acidic protein (GFAP) staining is used to identify astrocytes (a type of glial cell) and is helpful in diagnosing gliomas. Synaptophysin staining is used to identify neuronal differentiation and can be used to differentiate neuronal tumors from other types. IHC can also detect the presence or absence of specific receptors or molecules involved in cancer development and progression, aiding in diagnosis, prognosis, and treatment planning. IHC is not only used in tumor diagnostics but is also valuable in evaluating inflammatory and infectious conditions affecting the brain.
Q 12. How would you differentiate between different types of leukodystrophies on microscopy?
Differentiating between leukodystrophies on microscopy relies on identifying specific patterns of myelin (the insulating sheath around nerve fibers) disruption and the associated glial responses. This requires meticulous examination of white matter tracts with special stains like Luxol fast blue (LFB) for myelin and Bielschowsky silver stain for axons.
For instance, in metachromatic leukodystrophy (MLD), we see metachromatic granules within macrophages and oligodendrocytes due to the accumulation of sulfatide. In Krabbe disease, we observe globoid cells, which are macrophages laden with galactocerebroside. In adrenoleukodystrophy (ALD), we see an initial loss of myelin in the posterior white matter, often sparing the U-fibers. The patterns of myelin loss, the presence of specific inclusion bodies within cells, and the inflammatory responses help distinguish between these disorders. However, advanced molecular testing is often required for definitive diagnosis.
Q 13. Describe the neuropathological features of Rett syndrome.
Rett syndrome is a neurodevelopmental disorder almost exclusively affecting females. Neuropathologically, it’s characterized by subtle but consistent findings. The brain often appears smaller than expected for age (microcephaly) with no gross abnormalities. Microscopic examination reveals reduced neuronal size and density in certain brain regions. There are also alterations in glial cells, with evidence of abnormal myelination in some cases. However, these changes are not specific to Rett syndrome and overlap with findings seen in other neurodevelopmental disorders.
Recent research emphasizes alterations in synaptic structure and function as crucial contributors to Rett syndrome’s neurological manifestations. The neuropathological findings are not sufficiently specific for diagnosis, and the diagnosis primarily relies on clinical criteria and genetic testing identifying mutations in the MECP2 gene.
Q 14. What are the common artifacts encountered in pediatric brain biopsy specimens?
Pediatric brain biopsy specimens are particularly vulnerable to artifacts during processing and handling, impacting the accuracy of diagnosis. Common artifacts include:
- Ischemic changes: Insufficient blood supply during surgery or biopsy can lead to neuronal cell death and changes in tissue architecture, mimicking certain disease processes.
- Tissue compression: Squeezing the tissue during processing can distort the cellular arrangement and morphology, making accurate interpretation difficult.
- Freezing artifacts: Improper freezing and thawing can produce ice crystal formation, damaging cells and causing cell lysis.
- Fixation artifacts: Inadequate fixation can lead to poor preservation of tissue components, resulting in hazy structures and loss of cellular detail.
- Processing artifacts: Excessive dehydration or clearing agents can lead to shrinkage, distortion, and tissue damage during histological processing.
Minimizing these artifacts requires careful surgical technique, immediate fixation in appropriate solutions, and meticulous handling during processing. Recognition of these artifacts is crucial to avoid misinterpretation and ensure an accurate diagnosis.
Q 15. Discuss the ethical considerations in pediatric neuropathology.
Ethical considerations in pediatric neuropathology are paramount due to the unique vulnerability of child patients and their families. We must prioritize the child’s best interests while navigating complex situations involving diagnosis, prognosis, and treatment decisions. Key ethical considerations include:
- Informed Consent: Obtaining truly informed consent from parents or legal guardians is crucial. This requires explaining the diagnostic procedures, potential risks and benefits, and alternative options in a clear and understandable manner, tailored to the family’s level of understanding and emotional state. We must be sensitive to the emotional distress this diagnosis can cause and allow ample time for questions and processing of information.
- Privacy and Confidentiality: Protecting the child’s medical information is paramount. Strict adherence to HIPAA regulations and other relevant privacy laws is essential. Sharing information only with authorized individuals directly involved in the child’s care is vital.
- Balancing Treatment Benefits and Risks: Treatment decisions, especially those involving potentially toxic therapies, must carefully weigh potential benefits against risks. The long-term impact on the child’s development and quality of life must be a primary concern. This necessitates open communication and shared decision-making between the medical team and the family.
- Research Participation: When considering research participation, we must ensure that it is ethically sound, protects the child’s rights, and aligns with their best interests. This involves obtaining appropriate informed consent and minimizing any potential risks.
- Resource Allocation: Ethical considerations extend to resource allocation, ensuring equitable access to diagnostic testing and treatment, regardless of socioeconomic status or geographic location.
For example, a family may be struggling with the decision of whether to pursue aggressive treatment with significant side effects for a low-grade glioma with a potentially long survival period. Ethical discussions require careful navigation to ensure the decision aligns with the family’s values and the child’s best interests.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you interpret findings from neuroimaging studies in conjunction with neuropathological findings?
Neuroimaging, primarily MRI and CT scans, provides crucial anatomical information about brain tumors. Neuropathology, through microscopic examination of tissue samples, offers the definitive diagnosis, grading, and molecular characterization. The two are complementary and essential for comprehensive patient care.
For instance, an MRI might reveal a mass in the cerebellum, suggesting a possible tumor. Its size, location, and relationship to surrounding structures are all important. However, the MRI alone can’t definitively distinguish between different types of tumors (e.g., medulloblastoma vs. pilocytic astrocytoma). Neuropathological examination of a biopsy or resection specimen is necessary to provide a precise diagnosis, identify specific tumor subtypes based on histological features, and assess the grade (e.g., WHO grade).
By integrating both imaging and pathology findings, we build a complete picture of the tumor’s characteristics. For example, a highly cellular, densely packed tumor on microscopy (consistent with a high-grade glioma) may correlate with a rapidly enlarging, intensely enhancing mass on MRI. This integrated approach significantly impacts treatment planning and prognostication.
Q 17. Describe the different types of gliomas found in children.
Gliomas are the most common type of primary brain tumors in children. They arise from glial cells, which support neurons. Several subtypes exist, each with distinct characteristics:
- Pilocytic Astrocytoma (PA): Usually low-grade, often found in the cerebellum. Microscopically, they have characteristic Rosenthal fibers and often have a cystic component on imaging.
- Diffuse Astrocytoma (DA): More diffusely infiltrative than PA, often found in the cerebral hemispheres. Can be low-grade or high-grade (anaplastic astrocytoma).
- Glioblastoma (GBM): A highly aggressive, high-grade glioma characterized by necrosis (dead tissue) and significant vascular proliferation (new blood vessel growth) on microscopy. Usually has a poor prognosis.
- Ependymoma: Arises from the ependymal cells lining the ventricles. Can be found in various locations within the brain and spinal cord. They can be low-grade or high-grade.
- Oligodendroglioma: These are less common in children than other glioma subtypes. Characterized by cellular features that are distinct from astrocytomas.
It’s important to note that the classification and grading of gliomas are complex and often require advanced molecular techniques for precise categorization.
Q 18. What are the prognostic factors for pediatric brain tumors based on neuropathological findings?
Prognostic factors for pediatric brain tumors based on neuropathological findings are crucial for determining treatment strategies and predicting outcomes. Factors include:
- Tumor Histology: The specific type of tumor (e.g., medulloblastoma, pilocytic astrocytoma, ependymoma) significantly influences prognosis. High-grade tumors generally carry a worse prognosis than low-grade tumors.
- Tumor Grade: The WHO grading system (I-IV) reflects the aggressiveness of the tumor. Higher grades indicate faster growth and worse prognosis.
- Molecular Subtypes: Molecular profiling (e.g., gene expression analysis, DNA sequencing) reveals specific genetic alterations that further refine prognosis. For example, certain molecular subtypes of medulloblastoma have been associated with different responses to therapy and survival rates.
- Extent of Resection: The amount of tumor that can be surgically removed influences prognosis. Complete surgical resection is generally associated with improved survival.
- Presence of Microscopic Residual Disease: Even after seemingly complete surgical removal, microscopic tumor cells may remain, affecting prognosis.
- Age at Diagnosis: Age at diagnosis influences prognosis, with younger children sometimes having different responses to treatment compared to older children or adolescents.
For example, a child diagnosed with a high-grade glioma (GBM) at age 5 typically has a significantly worse prognosis than a child diagnosed with a low-grade pilocytic astrocytoma in the cerebellum at the same age.
Q 19. Explain the importance of molecular diagnostics in pediatric neuropathology.
Molecular diagnostics have revolutionized pediatric neuropathology. Techniques such as gene expression profiling, next-generation sequencing (NGS), and fluorescence in situ hybridization (FISH) provide detailed information about the genetic makeup of brain tumors. This information is crucial for:
- Precise Diagnosis: Molecular profiling helps differentiate between tumor subtypes, often beyond what’s possible with traditional histological examination alone. This improved diagnostic accuracy is particularly important in cases with ambiguous histological features.
- Risk Stratification: Molecular findings help identify high-risk patients who may benefit from more aggressive therapies or clinical trials. For example, specific genetic alterations in medulloblastomas can predict prognosis and treatment response.
- Targeted Therapy: Identifying specific genetic alterations can pave the way for targeted therapies that directly attack the tumor’s molecular vulnerabilities. This personalized medicine approach can potentially improve outcomes and reduce side effects.
- Monitoring Treatment Response: Molecular markers can be used to monitor the effectiveness of therapy and detect minimal residual disease (MRD).
For example, identifying a specific mutation in a tumor can inform the choice of targeted therapy, improving treatment efficacy and potentially reducing the need for more toxic treatments.
Q 20. Discuss the limitations of current diagnostic techniques in pediatric neuropathology.
Despite significant advancements, limitations remain in pediatric neuropathology diagnostic techniques:
- Sampling Limitations: Obtaining representative tissue samples for biopsy or resection can be challenging, particularly in deeply seated or diffusely infiltrative tumors. A small sample may not accurately reflect the tumor’s heterogeneity.
- Tumor Heterogeneity: Tumors are often heterogeneous, meaning they have areas of different cellular morphology and molecular characteristics within the same tumor. A single sample might not represent the entire tumor.
- Availability and Cost of Advanced Molecular Tests: Advanced molecular diagnostic tests (e.g., NGS) can be expensive and not readily available in all settings. This limits access for some patients.
- Interpretation Challenges: Interpreting complex molecular data requires expertise, and the significance of certain molecular findings may not always be fully understood.
- Lack of Biomarkers for Early Detection: Reliable biomarkers for early detection of childhood brain tumors are lacking, hindering early intervention.
Addressing these limitations requires continued research into new and improved diagnostic techniques, as well as efforts to improve access to existing technologies for all patients.
Q 21. How do you manage and interpret cases of unexpected neuropathological findings?
Unexpected neuropathological findings require a systematic and collaborative approach. The process involves:
- Reviewing the Clinical History: A thorough review of the patient’s clinical presentation, imaging findings, and treatment history is crucial to identify any clues that might explain the unexpected findings.
- Re-examining the Tissue Sample: The tissue sample should be re-examined by experienced neuropathologists, potentially with the use of additional immunohistochemical stains or molecular tests to confirm the diagnosis.
- Consulting with other specialists: Collaboration with other specialists (e.g., neuro-oncologists, neurosurgeons, geneticists) helps interpret the findings within the context of the patient’s overall clinical picture.
- Considering Differential Diagnoses: Generating a list of differential diagnoses helps determine alternative explanations for the unexpected findings. This may involve additional investigations, such as genetic testing.
- Reviewing the Literature: Searching the relevant medical literature helps determine the rarity of the finding, the typical clinical presentation, and prognosis.
- Communicating with the Family: Open and honest communication with the family is crucial, ensuring they understand the findings and their implications. This communication must be tailored to their emotional needs and understanding.
For example, finding a rare tumor subtype necessitates a detailed literature review to establish the appropriate treatment strategy and prognostic information. Careful explanation to the family is crucial given the unexpected and potentially concerning nature of the diagnosis.
Q 22. Describe your experience with different staining techniques used in pediatric neuropathology.
My experience with staining techniques in pediatric neuropathology is extensive, encompassing both routine and specialized methods crucial for accurate diagnosis and understanding disease mechanisms. Routine stains like Hematoxylin and Eosin (H&E) provide fundamental tissue architecture visualization, allowing us to identify cellular morphology and tissue organization. For example, H&E helps distinguish between grey and white matter, identify inflammatory infiltrates, and assess the degree of neuronal loss.
Beyond H&E, immunohistochemistry (IHC) is invaluable. We utilize numerous antibodies targeting specific proteins to pinpoint cellular constituents or highlight particular pathological processes. For instance, GFAP staining helps identify astrocytes and gliosis – a hallmark of many neurological disorders. Similarly, NeuN stains neurons, enabling us to quantify neuronal loss in conditions like cortical dysplasia. Myelin stains, such as Luxol Fast Blue, are crucial for evaluating myelination, vital in diagnosing demyelinating diseases like leukodystrophies. Finally, special stains like PAS (Periodic Acid-Schiff) are used for detecting glycogen and other carbohydrates, particularly helpful in certain metabolic disorders. Each stain offers a unique perspective, and skillful interpretation of their combined results is crucial for precise diagnosis.
Q 23. How do you approach a case of unexplained developmental delay with atypical neuropathological findings?
Approaching a case of unexplained developmental delay with atypical neuropathological findings requires a systematic and multidisciplinary approach. First, a thorough review of the clinical history, including family history, prenatal, perinatal, and postnatal events, is essential. Then, we meticulously examine the neuropathological findings, correlating them with clinical presentation. We look for subtle abnormalities that may be missed on initial review, such as subtle neuronal migration defects, subtle changes in white matter myelination, or alterations in specific neuronal populations.
Next, advanced techniques like molecular genetic testing (e.g., chromosomal microarray, next-generation sequencing) are critical to identify potential genetic causes. We also collaborate closely with clinicians, geneticists, and other specialists to integrate all available data. For instance, a child with developmental delay might show unusual glial cell morphology on biopsy. Genetic testing may then reveal a previously unknown mutation affecting glial development. This collaborative approach is crucial for reaching an accurate diagnosis and providing the most appropriate management plan. Even without a definitive diagnosis, understanding the underlying neuropathological features can help guide supportive care and management of the symptoms.
Q 24. What are the key differences between the neuropathological features of different types of epilepsy syndromes?
The neuropathological features vary significantly across different epilepsy syndromes, reflecting the diverse etiologies and mechanisms underlying seizures. For example, in focal cortical dysplasia (FCD), a common cause of drug-resistant epilepsy, we see abnormalities in cortical architecture, including disorganized neuronal lamination, balloon cells (giant dysmorphic neurons), and abnormal glial proliferation. In contrast, in Lennox-Gastaut syndrome, which is characterized by multiple seizure types, neuropathological findings might be less specific, potentially showing subtle abnormalities in neuronal organization or gliosis, but often no single definitive change.
The hallmark of tuberous sclerosis complex (TSC) is the presence of cortical tubers, which are nodules of abnormal neuronal and glial proliferation. In contrast, in many genetic epilepsies, there might be subtle abnormalities that require sophisticated techniques such as electron microscopy to detect changes in synaptic structures or mitochondrial abnormalities. The heterogeneity underscores the need for meticulous examination, correlating microscopic findings with clinical features and potentially employing advanced molecular techniques for diagnosis. It’s important to note that sometimes, despite thorough investigation, no clear neuropathological cause is found, highlighting the complex nature of epilepsy.
Q 25. Describe your experience with research in the field of pediatric neuropathology.
My research in pediatric neuropathology has primarily focused on understanding the underlying mechanisms of rare neurological disorders and developing novel diagnostic tools. One significant project involved investigating the neuropathological changes in a specific type of childhood leukodystrophy, aiming to identify early diagnostic markers. This involved advanced immunohistochemical analyses, genomic sequencing, and collaboration with clinical teams. We identified novel genetic mutations associated with the disease and discovered specific protein alterations detectable in early disease stages. This has potential implications for earlier diagnosis and potential therapeutic intervention.
Another area of my research explores the impact of environmental factors, such as prenatal exposure to toxins, on neurodevelopment. We use animal models and advanced imaging techniques to study how these exposures may lead to subtle yet significant alterations in brain structure and function. The ultimate goal is to define how these environmental insults affect brain development and to identify potential preventive strategies. This work directly contributes to improving our understanding of developmental brain disorders and guiding clinical practice.
Q 26. Discuss your understanding of the impact of neuropathological findings on patient management and prognosis.
Neuropathological findings are crucial for guiding patient management and prognosis in pediatric neurology. An accurate diagnosis often directs treatment decisions. For example, identifying a specific genetic mutation in a metabolic disorder helps to tailor interventions accordingly, such as dietary modifications or enzyme replacement therapy. In tumors, the specific subtype and grade significantly impact treatment strategies, influencing the need for surgery, chemotherapy, or radiotherapy. Similarly, the extent of neuronal loss or gliosis in conditions like hypoxic-ischemic encephalopathy can help predict long-term neurological outcomes, guiding families on expectations and providing appropriate support.
However, it is crucial to remember that neuropathological findings should be interpreted in the context of the overall clinical picture. The findings may only provide a partial picture, and other factors such as age, overall health, and response to treatment must also be considered when determining prognosis and managing patients. For instance, a child with a brain tumor may receive a positive prognosis based on complete surgical removal, even if the neuropathological assessment reveals a high-grade tumor. This highlights the collaborative nature of medical decision-making and the importance of integrating various data points for optimal patient care.
Q 27. How do you stay current with the latest advances in pediatric neuropathology?
Staying current in the rapidly evolving field of pediatric neuropathology requires a multi-pronged approach. I regularly attend national and international conferences, workshops, and seminars, keeping abreast of the latest research findings and diagnostic techniques. I actively participate in professional organizations such as the Child Neurology Society and the Society for Neuropathology, which provide access to continuing education opportunities and networking with peers. Furthermore, I meticulously review peer-reviewed journals, particularly those focusing on neuropathology, neurogenetics, and developmental neurobiology.
I also engage in continuous self-directed learning by reading textbooks and review articles, ensuring my knowledge remains comprehensive. Moreover, I value collaboration with researchers and clinicians worldwide. Through these interactions, I receive continuous feedback and exposure to a wide range of experiences, enriching my understanding and broadening my skill set. Active engagement in professional communities and a commitment to lifelong learning are essential for maintaining competence in this dynamic field.
Q 28. What are your long-term career goals within pediatric neuropathology?
My long-term career goals involve establishing myself as a leading expert in pediatric neuropathology, contributing significantly to advancements in the field. This includes further developing my research program, focusing on translational research that can bridge the gap between basic science discoveries and clinical applications. I aim to create innovative diagnostic tools and therapeutic strategies for pediatric neurological disorders, ultimately improving patient outcomes. A key aspect is mentoring future generations of pediatric neuropathologists and fostering a collaborative environment for research and education.
Specifically, I envision expanding my research into the application of artificial intelligence and machine learning for image analysis in neuropathology. I am passionate about developing automated diagnostic tools that can enhance the speed and accuracy of diagnosis, making a significant impact on patient care. These long-term ambitions involve a blend of research, clinical practice, teaching, and mentorship, all working towards improving the lives of children with neurological conditions.
Key Topics to Learn for Pediatric Neuro-Pathology Interview
- Developmental Neuropathology: Understanding the unique challenges in diagnosing and classifying neurological conditions in children, including the impact of developmental stage on disease presentation and progression. Consider practical applications like differentiating between congenital and acquired conditions.
- Genetic and Metabolic Disorders: Mastering the pathophysiology of genetic and metabolic disorders affecting the developing nervous system. Focus on the correlation between genotype and phenotype, and how this informs diagnostic and therapeutic strategies. Explore practical applications in case studies.
- Infections and Inflammatory Conditions: Deep dive into the pathogenesis and clinical manifestations of infectious and inflammatory diseases of the pediatric nervous system. Develop your ability to differentiate between various etiologies based on clinical and pathological findings. Practice problem-solving using case scenarios.
- Neoplasms of the Central and Peripheral Nervous System: Gain a thorough understanding of the diverse spectrum of pediatric brain and spinal cord tumors, including their classification, molecular characteristics, and treatment implications. Practice differential diagnosis of common pediatric CNS tumors.
- Neurodegenerative Diseases: Explore the mechanisms and clinical features of neurodegenerative conditions in children, such as leukodystrophies and other rare disorders. Focus on the challenges in early diagnosis and the importance of multidisciplinary approaches.
- Trauma and Injury: Understand the unique aspects of traumatic brain injury and spinal cord injury in the pediatric population, including the impact of age and developmental stage on prognosis and management. Explore the use of imaging techniques in evaluating traumatic injury.
- Diagnostic Techniques and Interpretation: Develop proficiency in interpreting various diagnostic tools used in pediatric neuropathology, including MRI, CT, and histological techniques. Practice analyzing images and correlating findings with clinical presentations.
Next Steps
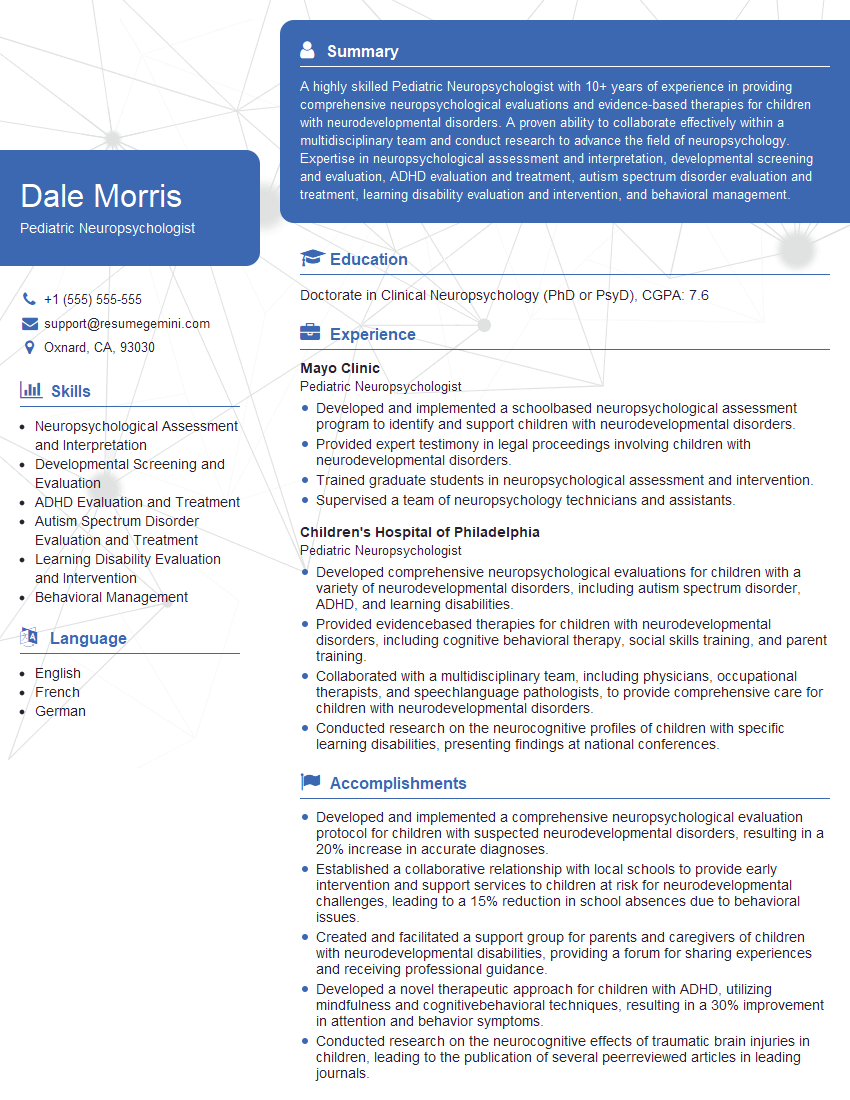
Mastering Pediatric Neuro-Pathology is crucial for a successful and rewarding career. A strong understanding of these complex conditions will position you as a highly sought-after specialist. To maximize your job prospects, it’s essential to present your qualifications effectively. Crafting an ATS-friendly resume is key to ensuring your application gets noticed by recruiters. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored specifically to Pediatric Neuro-Pathology, to give you a head start. Take the next step in your career journey and create a resume that showcases your expertise.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.