Cracking a skill-specific interview, like one for Polysomnography, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Polysomnography Interview
Q 1. Describe the different stages of sleep and their characteristic EEG patterns.
Sleep is characterized by distinct stages, each with unique electroencephalographic (EEG) patterns reflecting different brain activity levels. These stages cycle repeatedly throughout the night.
- Wakefulness: Characterized by low-voltage, mixed-frequency EEG activity. The brain is highly active, processing external stimuli.
- Stage N1 (Non-REM 1): This is the transitional stage between wakefulness and sleep. EEG shows theta waves (4-7 Hz), which are slower than the alpha waves of wakefulness. Hypnic jerks, brief muscle contractions, often occur.
- Stage N2 (Non-REM 2): This is the predominant sleep stage, comprising about 50% of total sleep time. EEG shows sleep spindles (bursts of 12-14 Hz activity) and K-complexes (high-amplitude, slow waves). These reflect brain’s active consolidation of memories.
- Stage N3 (Slow Wave Sleep or Non-REM 3): This is the deepest stage of sleep, characterized by high-amplitude, low-frequency delta waves (0.5-2 Hz). It’s crucial for physical restoration and growth hormone release. Individuals are difficult to arouse from this stage.
- REM (Rapid Eye Movement) Sleep: This stage is characterized by rapid eye movements, vivid dreams, and a paradoxical EEG pattern resembling wakefulness (low-voltage, mixed-frequency). Muscle atonia (paralysis) prevents acting out dreams. REM sleep is essential for memory processing and cognitive function.
Imagine it like this: Wakefulness is like a bustling city, N1 is the quiet suburbs, N2 is a peaceful town, N3 is a deep slumber in the countryside, and REM is a vibrant dreamland with busy brain activity but a paralyzed body.
Q 2. Explain the process of performing a polysomnography study.
A polysomnography (PSG) study involves comprehensive physiological monitoring during sleep. The process typically begins with a patient consultation to review their medical history and sleep complaints. Following this, electrodes are meticulously applied to the scalp (EEG), chin (EMG), legs (EMG), eyes (EOG), and chest (respiratory effort and heart rate). Sensors are also placed on the nasal cannula and/or thermistor to monitor airflow and oxygen saturation. Some studies also use other sensors to monitor leg movements or snoring.
The patient then sleeps in a comfortable, darkened room, usually overnight. During the sleep, all the signals are recorded and monitored by the PSG machine. The data, including EEG, EOG, EMG, airflow, respiratory effort, heart rate, and oxygen saturation are simultaneously recorded, stored, and later analyzed by a trained sleep technologist and physician.
After the study, the data is reviewed to identify sleep stages, diagnose sleep disorders such as apnea, insomnia, periodic limb movement disorder (PLMD), etc. A comprehensive report is then generated for the referring physician.
Q 3. What are the common artifacts encountered during polysomnography and how are they addressed?
Polysomnography is susceptible to various artifacts that can affect the accuracy of data interpretation. These artifacts can originate from the patient, the equipment, or the environment.
- Patient Movement: This is a common artifact, causing signal fluctuations and misinterpretations of sleep stages. Careful electrode placement and use of artifact reduction techniques during data scoring can help mitigate this.
- Electrode Impedance Changes: Poor contact of electrodes leads to high impedance and signal loss. Proper electrode placement, cleaning, and maintaining good skin contact help alleviate this.
- Environmental Noise: External sounds and light interference can introduce noise into the EEG recording. A quiet and darkened sleep environment is essential.
- Electrical Interference: Interference from nearby electrical equipment can corrupt signal quality. Appropriate grounding and shielding techniques are used to reduce this.
- Cable Movement: Movement of cables can create artifacts. Securing cables properly during sleep is important.
Addressing these artifacts involves a combination of meticulous techniques during data acquisition, careful examination of the recordings, and the use of signal processing techniques to minimize the impact of artifacts during scoring. Experienced sleep technologists are trained to identify and correct for these artifacts to ensure accurate data interpretation.
Q 4. How do you identify and score sleep apnea events?
Sleep apnea events are identified and scored by analyzing the relationship between respiratory effort, airflow, and oxygen saturation. Obstructive apnea is defined as the absence of airflow despite ongoing respiratory effort, whereas central apnea is characterized by the absence of both airflow and respiratory effort. Mixed apnea is a combination of both.
The scoring process involves carefully examining the PSG recording and applying standardized criteria (e.g., AASM scoring manual). An apnea is typically scored when there is a cessation of airflow for at least 10 seconds. Hypopneas (reduced airflow) are also scored based on predefined criteria that consider the reduction in airflow, oxygen desaturation, and arousal. The number and duration of these events are quantified to determine the severity of sleep apnea.
For example, an obstructive apnea would show a flat airflow trace despite the presence of respiratory muscle activity (seen via chest and abdominal effort belts) and, often, an associated oxygen desaturation.
Q 5. Differentiate between central, obstructive, and mixed sleep apnea.
The three main types of sleep apnea differ in the underlying cause of the breathing cessation or reduction:
- Obstructive Sleep Apnea (OSA): This is the most common type, occurring when the upper airway collapses during sleep, obstructing airflow. Respiratory effort is present but airflow is absent. Obesity, anatomical abnormalities, and neuromuscular weakness are contributing factors.
- Central Sleep Apnea (CSA): This is less common and occurs due to a dysfunction in the respiratory control center in the brain, leading to a lack of respiratory effort and airflow. CSA is sometimes associated with neurological conditions or heart failure.
- Mixed Sleep Apnea: This type combines elements of both OSA and CSA. An episode may begin as central apnea, followed by obstructive apnea as the airway collapses due to reduced respiratory effort. It’s a more complex condition and requires careful diagnostic evaluation.
Think of it as a blocked pipe (OSA), a non-functioning pump (CSA), and a pump that starts failing and then causes a blockage (mixed).
Q 6. What are the scoring criteria for REM and NREM sleep?
The scoring of REM and NREM sleep relies on visual analysis of the PSG data using standardized criteria (AASM Manual). The key differences are:
- REM Sleep: Characterized by low-voltage, mixed-frequency EEG activity, sawtooth waves (in some cases), rapid eye movements (EOG), and muscle atonia (EMG).
- NREM Sleep: Encompasses stages N1, N2, and N3. Distinguishing features include slow wave activity (delta waves in N3), sleep spindles and K-complexes (N2), and theta waves (N1). Muscle tone is present, but reduced compared to wakefulness.
The scoring process is based on the identification of these characteristic features in the EEG, EOG, and EMG tracings. Sleep technologists and sleep medicine physicians use the AASM manual as the standardized guide to consistently score sleep stages to allow accurate diagnosis and treatment planning.
Q 7. Describe your experience with different types of sleep studies (e.g., PSG, MSLT, MWT).
My experience encompasses a wide range of sleep studies, including polysomnography (PSG), multiple sleep latency test (MSLT), and maintenance of wakefulness test (MWT). I have extensive experience in conducting and interpreting PSG studies, identifying various sleep disorders, including sleep apnea, insomnia, narcolepsy, restless legs syndrome and periodic limb movement disorder.
The MSLT is a critical tool for diagnosing narcolepsy by measuring the latency to sleep onset during multiple daytime nap opportunities. A short sleep latency indicates excessive daytime sleepiness. I’ve performed numerous MSLTs, assisting in the diagnosis and management of this debilitating sleep disorder. Similarly, the MWT assesses the ability of an individual to remain awake under controlled conditions, which is helpful in evaluating excessive daytime sleepiness and circadian rhythm disorders. I have significant experience in MWT, helping to manage patient cases effectively and accurately.
In my career, I have worked with a range of patients, from infants to the elderly, each requiring a tailored approach to sleep study design and data interpretation, highlighting the importance of personalized medicine within the field of sleep medicine. Each study provides valuable insights into different facets of sleep architecture and helps in making targeted therapeutic decisions.
Q 8. How do you ensure patient safety and comfort during a polysomnography study?
Patient safety and comfort are paramount during a polysomnography (PSG) study. We prioritize this through several key strategies. First, we thoroughly explain the procedure to the patient, answering any questions and addressing concerns to alleviate anxiety. This often involves showing them the equipment and explaining how each sensor works. We emphasize the importance of remaining still but also assure them that they can move and adjust as needed. The sleep environment is crucial: we ensure the room is dark, quiet, and at a comfortable temperature. We adjust the bed and pillows to maximize comfort. During the study, we regularly check on the patient to ensure they are comfortable, addressing any issues promptly. If the patient experiences discomfort, we adjust sensors or bedding as needed. Continuous monitoring of vital signs such as heart rate, respiratory rate, and oxygen saturation provide crucial safety checks and allow for prompt intervention if any abnormalities occur. For instance, if oxygen saturation drops, we’ll take appropriate measures, which may include adjusting the position, supplying supplemental oxygen, or alerting the supervising physician. Finally, we have clear protocols for managing any potential emergencies, ensuring immediate access to medical assistance if required.
Q 9. Explain your understanding of sleep-related breathing disorders.
Sleep-related breathing disorders (SRBDs) are a group of conditions that affect breathing during sleep. The most common are obstructive sleep apnea (OSA) and central sleep apnea (CSA). In OSA, the airway collapses repeatedly during sleep, causing pauses in breathing. This is often due to factors like obesity, anatomical abnormalities (e.g., enlarged tonsils or adenoids), and nasal congestion. CSA, on the other hand, involves the brain failing to send the correct signals to the muscles that control breathing. This can be linked to heart conditions or neurological disorders. PSG is instrumental in diagnosing these conditions. We measure airflow, respiratory effort (chest and abdominal movements), oxygen saturation, and brainwave activity during sleep. Analyzing these signals allows us to identify apneas (cessations of breathing), hypopneas (decreases in breathing), and respiratory effort-related arousals. The Apnea-Hypopnea Index (AHI), calculated from these events per hour of sleep, determines the severity of the disorder. For example, an AHI above 5 is often considered indicative of OSA. The PSG also helps differentiate between OSA and CSA based on the relationship between respiratory effort and airflow. Finally, PSG can help identify other SRBDs, such as hypoventilation syndrome and sleep-disordered breathing.
Q 10. What are the common causes of insomnia and how are they assessed using polysomnography?
Insomnia, the difficulty falling asleep or staying asleep, has many potential causes. These can range from stress and anxiety to medical conditions like hyperthyroidism or chronic pain. Lifestyle factors such as irregular sleep schedules, excessive caffeine or alcohol consumption, and a poor sleep environment also play significant roles. PSG doesn’t directly diagnose the underlying *cause* of insomnia, but it helps rule out other sleep disorders that may be contributing to the problem. For example, periodic limb movement disorder (PLMD) or restless legs syndrome (RLS) can disrupt sleep and mimic symptoms of insomnia. PSG helps identify these movements during sleep and quantify their impact on sleep architecture. Furthermore, PSG can assess the quality of sleep obtained, revealing sleep fragmentation and reduced total sleep time which are common hallmarks of insomnia. It also helps detect the presence of other sleep disorders, like sleep apnea, which might be responsible for a patient’s feeling of poor sleep. While PSG isn’t the primary tool for diagnosing the root cause of insomnia, it’s essential for differentiating insomnia from other sleep disturbances.
Q 11. How do you calibrate and troubleshoot polysomnography equipment?
Calibration and troubleshooting are crucial for accurate PSG results. Calibration ensures that the equipment is functioning within its specified parameters. This typically involves using known signal sources (e.g., a calibration signal generator) to check the amplitude and frequency response of each channel. We meticulously document all calibration procedures. Troubleshooting involves identifying and resolving any equipment malfunctions. This could range from loose connections to sensor malfunctions or software errors. A systematic approach is vital: we first check for obvious problems like loose wires or improperly attached electrodes. Then, we examine the signal quality on the PSG monitor and identify which channels are affected. Our troubleshooting often involves replacing sensors, checking signal leads, restarting software, or performing system diagnostics as per the manufacturer’s guidelines. For instance, if a particular EEG channel displays high impedance, indicating a poor connection, we would check the electrode placement and ensure proper skin preparation. We maintain detailed records of troubleshooting actions, noting the issue, steps taken, and the resolution. This ensures data integrity and allows for future reference.
Q 12. Describe your experience with data analysis and report generation in polysomnography.
Data analysis and report generation are integral to PSG. After the study, I meticulously review the PSG data, which includes EEG, EOG, EMG, respiratory signals, and oxygen saturation. This involves visually inspecting the waveforms and using specialized software to automatically score sleep stages according to the AASM (American Academy of Sleep Medicine) guidelines. I identify and quantify sleep-related events like apneas, hypopneas, and periodic limb movements. I calculate indices such as the AHI, which is crucial for diagnosing sleep apnea. The analysis also involves assessing sleep architecture, including the percentage of time spent in each sleep stage (N1, N2, N3, REM). The final report summarizes all findings, including the sleep stages, the number and type of sleep-related events, and my interpretation of the findings. The report is clearly written and concise, providing a clinically relevant summary for the referring physician. I always ensure that the report is well-organized, easy to understand, and includes only relevant information. I make it a point to clearly describe the results and their clinical significance, minimizing the use of technical jargon whenever possible, so the report is easily accessible to the referring physician.
Q 13. Explain your understanding of the AASM scoring manual.
The AASM scoring manual is the gold standard for scoring polysomnography data. It provides detailed criteria for identifying and classifying sleep stages and respiratory events. Understanding this manual is fundamental to accurate interpretation of PSG results. The manual outlines the rules for identifying various sleep stages (wake, N1, N2, N3, REM) based on EEG, EOG, and EMG activity. It defines specific criteria for scoring sleep-related breathing events, such as apneas and hypopneas, providing clear guidelines for distinguishing between obstructive and central events. The manual also details the rules for scoring other sleep-related events, such as periodic limb movements. Adherence to the AASM scoring manual is critical to ensure consistency and reliability in PSG interpretation. Differences in scoring can lead to different diagnoses and treatment recommendations. Therefore, maintaining a high degree of accuracy in following the scoring rules is paramount for proper diagnosis and patient care.
Q 14. How do you handle challenging patients or situations during a sleep study?
Handling challenging patients or situations requires patience, adaptability, and a strong understanding of patient psychology. Some patients may be anxious or uncomfortable with the equipment. In these cases, we take extra time to explain the procedure, answer questions, and provide reassurance. We might offer relaxation techniques or adjust the study environment to make them more comfortable. Other patients may have difficulty staying still or maintaining sleep. We might utilize different strategies here, such as adjusting electrode placement, providing additional padding, or modifying the study schedule. Patients with cognitive impairments or behavioral problems require a more tailored approach. We often involve their caregivers or family members in the process, ensuring their cooperation and understanding. If a significant problem arises during the study, such as equipment malfunction or a patient experiencing distress, we address it immediately, following established protocols to ensure patient safety. Detailed documentation of the challenges faced and the strategies used is crucial for both continuity of care and to identify areas for improvement in our patient handling practices.
Q 15. What is your experience with different types of sleep staging software?
My experience with sleep staging software encompasses a wide range of programs, from commercially available systems like Alice and Somnolyzer to more specialized research platforms. I’m proficient in using these tools to visually review polysomnographic data, identify sleep stages according to the AASM (American Academy of Sleep Medicine) criteria, and generate comprehensive sleep reports. This includes experience with automated scoring algorithms and the crucial process of manual review and adjustment to ensure accuracy. For instance, I’ve used Alice to analyze data from patients with suspected sleep apnea, while Somnolyzer’s advanced features proved invaluable in studying patients with complex sleep disorders involving movement disorders.
My expertise extends to understanding the limitations of each software. Automated scoring, while efficient, requires careful manual review to detect subtle artifacts or atypical waveforms that could misclassify sleep stages. I can confidently address inconsistencies and ensure the final sleep staging report reflects the true sleep architecture of the patient. I am also comfortable working with the raw data files if needed for deeper analysis or troubleshooting.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your understanding of respiratory effort-related arousal (RERA).
Respiratory Effort-Related Arousal (RERA) refers to an episode during sleep where there’s an increased respiratory effort, often accompanied by slowing of the respiratory rate, but without a complete cessation of airflow (apnea) or a significant drop in oxygen saturation. Essentially, the respiratory system struggles, leading to an arousal from sleep. This arousal may not be consciously perceived by the patient but is detected by polysomnography as a change in EEG (brainwave activity).
Identifying RERA requires careful interpretation of multiple polysomnographic signals. We look for increased respiratory effort (seen in the respiratory effort belts), a reduction in airflow (indicated by nasal cannula or airflow pressure sensors), and a concurrent EEG arousal. Unlike apnea, the airflow reduction in RERA isn’t complete. A decrease in oxygen saturation (SpO2) might also be present, although it isn’t a required criterion for scoring. I’m skilled in distinguishing subtle RERAs from other respiratory events, considering the patient’s overall clinical picture and sleep architecture when making this determination.
Q 17. How do you identify and score periodic limb movement disorder (PLMD)?
Periodic Limb Movement Disorder (PLMD) is characterized by repetitive, stereotyped movements of the limbs during sleep, typically occurring every 20-40 seconds. These movements are often subtle and involve flexion or extension of the legs or arms.
Scoring PLMD involves reviewing the electromyography (EMG) signals from the lower limbs (often tibialis anterior and peroneal muscles). We look for repetitive bursts of EMG activity exceeding a certain amplitude and duration, usually lasting for more than 0.5 seconds with an inter-movement interval of 5–90 seconds. A significant number of these movements (e.g., > 5/hour of sleep) is required for diagnosis. I consider factors like patient age and sleep stage when assessing PLMD. For example, an increased occurrence during NREM sleep stages (non-rapid eye movement) is more typical. Manual scoring of PLMD requires careful attention to detail to differentiate them from other movement artifacts. I also consider other clinical information like the patient’s symptoms (daytime sleepiness, restless legs syndrome), medical history and physical examination when making the diagnosis.
Q 18. What is your experience with nocturnal seizures and their polysomnographic presentation?
My experience with nocturnal seizures on polysomnography involves recognizing their characteristic EEG patterns, distinguishing them from other sleep events, and collaborating with neurologists for diagnosis. Nocturnal seizures can manifest in various ways on a PSG, from subtle changes in brainwave activity to dramatic generalized convulsions. The identification often involves reviewing EEG along with other channels like EMG, EOG (electrooculogram), and ECG (electrocardiogram).
For example, I’ve encountered cases where patients experienced subtle ictal discharges (abnormal brainwave patterns during a seizure) on EEG, alongside changes in respiration or muscle tone. In other cases, the PSG recorded clear tonic-clonic activity accompanied by significant changes in other physiological parameters. The interpretation requires a deep understanding of EEG patterns, seizure semiology, and the context provided by the patient’s history and neurological examination. The collaborative nature of such interpretations is crucial and I am very comfortable with this interplay between neurology and sleep medicine.
Q 19. How familiar are you with CPAP titration studies?
I’m highly familiar with CPAP (Continuous Positive Airway Pressure) titration studies. These studies are crucial for determining the optimal CPAP pressure needed to treat obstructive sleep apnea (OSA). The procedure involves monitoring the patient’s respiratory parameters while gradually increasing the CPAP pressure until apnea and hypopnea events are effectively minimized, usually during a full night’s sleep.
My experience includes interpreting the polysomnographic data during and after titration, adjusting CPAP settings in response to observed respiratory events, and generating reports with recommendations for the optimal CPAP pressure. I understand the nuances of different titration protocols and the importance of ensuring patient comfort and tolerance during the study. My focus is on identifying the lowest effective CPAP pressure that maintains adequate respiratory function and reduces AHI (Apnea-Hypopnea Index) to an acceptable level.
Q 20. Describe the different types of respiratory events and their implications.
Polysomnography identifies several types of respiratory events, each with significant implications. The most common are:
- Apnea: A complete cessation of airflow for at least 10 seconds. Apneas significantly reduce oxygen saturation and can lead to cardiovascular complications, daytime sleepiness, and cognitive impairment.
- Hypopnea: A reduction in airflow by at least 50% along with a decrease in oxygen saturation or an increase in respiratory effort. Hypopneas, while less severe than apneas, also contribute to the overall sleep disruption and health consequences of sleep-disordered breathing.
- Respiratory Effort-Related Arousal (RERA): As previously explained, increased respiratory effort without complete airflow cessation resulting in an arousal from sleep. RERAs, while not always associated with significant drops in oxygen, still indicate respiratory instability and sleep disruption.
- Central Apnea: Absence of respiratory effort, often associated with neurological or cardio-respiratory diseases. This differs from obstructive apnea, where the effort is present but airflow is blocked.
The clinical implications of these events are significant, ranging from daytime sleepiness and cognitive impairment to cardiovascular disease, hypertension, stroke, and even sudden death in severe cases. Accurate identification and scoring are essential for proper diagnosis and treatment planning.
Q 21. What is your experience with patient education and communication related to sleep disorders?
Patient education and communication are paramount in my practice. I believe in a patient-centered approach, explaining complex polysomnographic findings and sleep disorder diagnoses in a clear, accessible manner. I tailor my communication style to each patient’s understanding, using analogies and visual aids whenever necessary. For instance, when explaining sleep apnea, I might compare the airway to a partially collapsed hose, illustrating how CPAP helps keep it open.
My approach includes explaining the purpose and procedure of the PSG in detail before the study, addressing any anxieties or concerns the patient might have. After the study, I provide a comprehensive explanation of the results, discuss the diagnosis, and clearly outline treatment options. This involves not only discussing the technical aspects, such as the AHI, but also the functional impact of the sleep disorder on the patient’s daily life. I actively encourage patients to ask questions and ensure they understand their condition and treatment plan. I believe strong communication fosters trust and improves patient adherence to treatment recommendations.
Q 22. How do you maintain accurate and detailed patient records?
Maintaining accurate and detailed patient records in polysomnography is paramount for ensuring proper diagnosis and treatment. We rely on a multi-faceted approach combining electronic health records (EHR) and meticulous manual documentation.
- EHR Systems: Our primary method involves utilizing a sophisticated EHR system designed specifically for sleep studies. This system allows for the digital recording of patient demographics, medical history, medication lists, study parameters (e.g., EEG montage, sensor placement), and detailed scoring of the sleep study data. It ensures data integrity and easy access for the sleep physician and other medical professionals.
- Manual Documentation: While EHRs are crucial, we also maintain detailed manual documentation. This includes pre-study questionnaires, technician notes observing patient behavior throughout the night (e.g., sleep position changes, medication administration), and any challenges faced during study setup. This ensures a complete record, particularly for events not easily captured by the automated system.
- Quality Control: Regular audits are conducted to ensure data accuracy and consistency. This includes spot checks of both EHR data and technician notes to verify completeness and identify any potential discrepancies. This allows for timely correction and continuous improvement of our record-keeping practices.
For example, if a patient experiences an unexpected event during the study, like a sleepwalking episode, we document this in detail in our notes alongside any related changes in physiological signals. This allows the physician to contextualize the data and make a more informed diagnosis.
Q 23. What are your strengths and weaknesses as a polysomnographic technologist?
My strengths as a polysomnographic technologist include my meticulous attention to detail, my proficiency in troubleshooting technical issues, and my ability to build rapport with patients. I pride myself on my ability to ensure high-quality data acquisition, even in challenging situations. I am also a very effective communicator, adept at explaining procedures to patients, reassuring anxious individuals, and working collaboratively with the sleep medicine team.
However, like anyone, I have areas for improvement. One area I’m focusing on is even more efficient time management during particularly busy nights, which can be stressful. To address this, I am working on optimizing my workflow and prioritizing tasks more effectively. I’m also actively seeking opportunities to enhance my expertise in advanced polysomnographic techniques, like advanced respiratory event scoring and the interpretation of certain artifacts.
Q 24. Describe a time you had to troubleshoot a technical issue during a sleep study.
During a recent sleep study, we encountered an issue with a patient’s EEG signal exhibiting excessive artifact. This made accurate scoring difficult. The artifact appeared to be related to a loose electrode.
- Initial Assessment: I first visually inspected the EEG channels and the corresponding electrode placement on the patient. The signal quality on several frontal electrodes was significantly degraded compared to the rest of the montage.
- Troubleshooting: I systematically checked the electrode connections at the patient’s scalp and at the connection points to the amplifier. I discovered that one of the frontal electrodes had come slightly loose during the patient’s sleep movements.
- Solution: After carefully re-applying the electrode and ensuring a secure connection, I re-evaluated the EEG signal. The artifact was significantly reduced, resulting in a cleaner EEG signal for the remainder of the study. I documented the issue and my resolution steps in the patient’s chart, ensuring transparency and a complete record.
This experience reinforced the importance of meticulous electrode placement and regular monitoring of signal quality. It’s a reminder that even small issues can significantly impact the reliability of study results.
Q 25. How do you manage your time effectively during a busy sleep lab shift?
Managing time effectively during a busy sleep lab shift requires a proactive and organized approach. My strategy centers on prioritization, efficient workflow, and effective communication.
- Prioritization: I prioritize tasks based on urgency and importance. Preparing the study room for the next patient while processing data from the previous study allows for optimal time management.
- Efficient Workflow: I develop a streamlined workflow for each stage of the sleep study process – from patient greeting and electrode placement to data acquisition and initial artifact review. This reduces unnecessary delays and ensures smooth transitions between tasks.
- Communication: Open and clear communication with the sleep physician and other lab staff is crucial. Addressing any immediate issues promptly prevents unnecessary delays and allows for efficient problem-solving.
For example, if I encounter unexpected delays with one patient, I inform the physician and other staff to coordinate the schedule and ensure the workflow is minimally disrupted. A proactive approach helps prevent delays from cascading throughout the night.
Q 26. What are your salary expectations?
My salary expectations are in line with the current market rate for experienced polysomnographic technologists with my qualifications and experience in this region. I am open to discussing a competitive compensation package that reflects my contributions and aligns with the position’s responsibilities. I am more interested in a position that provides opportunities for growth and professional development than in focusing solely on a specific number.
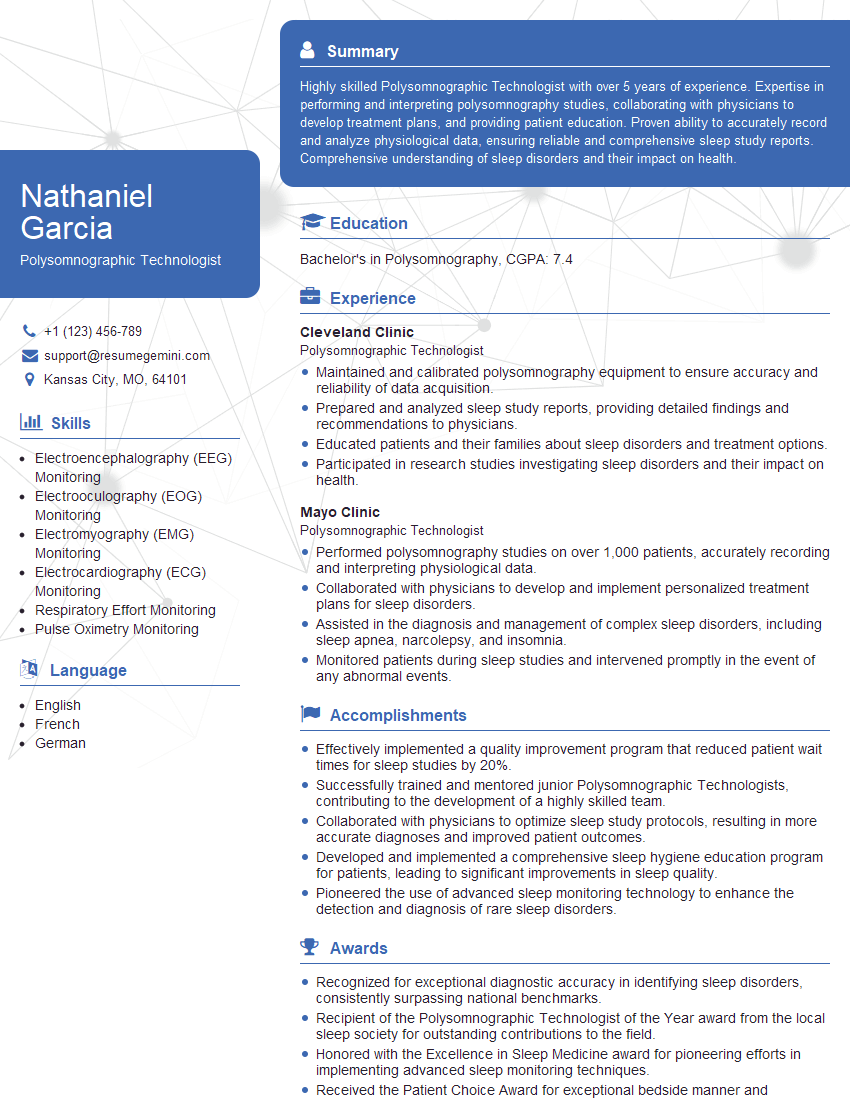
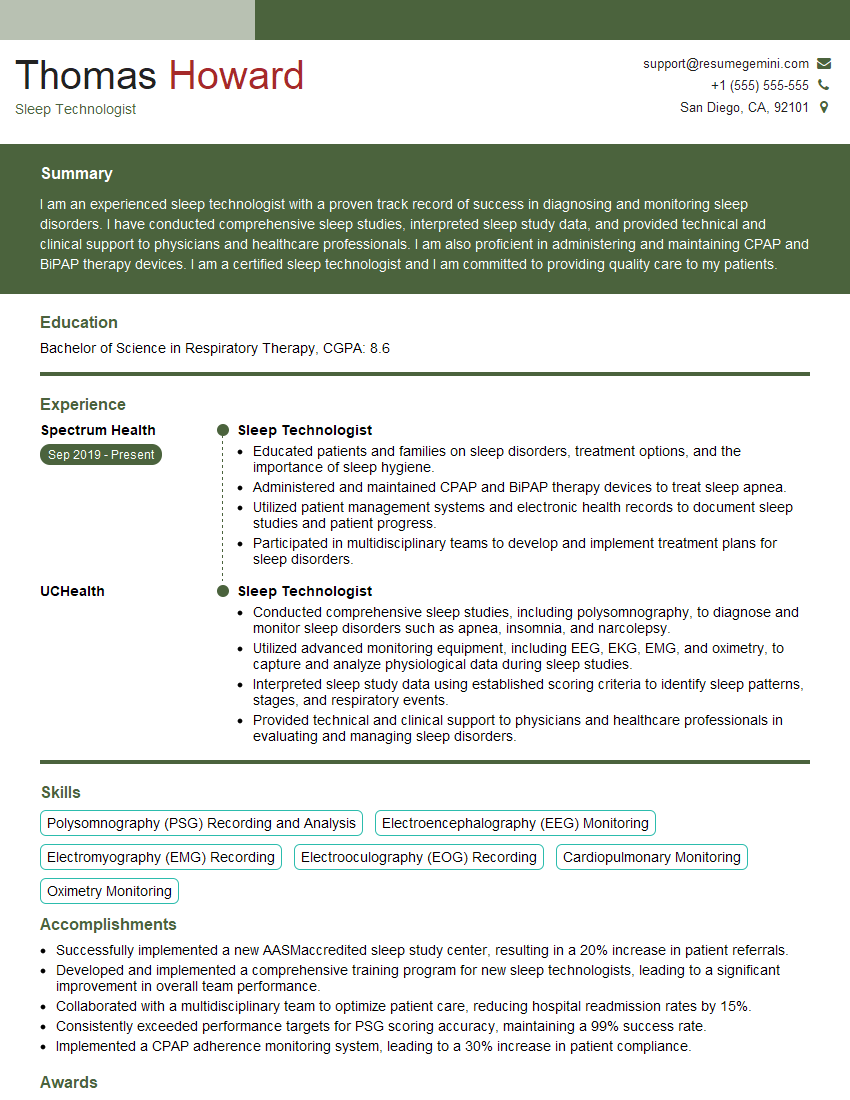
Q 27. What are your career goals in the field of polysomnography?
My career goals in polysomnography involve continuous professional development and expanding my expertise. I aspire to become a Registered Polysomnographic Technologist (RPSGT) and eventually pursue advanced roles in sleep medicine, such as a sleep lab supervisor. I am eager to stay abreast of emerging technologies and diagnostic techniques within the field, contributing to the highest standards of patient care and study accuracy.
Q 28. Why are you interested in this particular position?
I am particularly interested in this position because of [Company Name]’s reputation for excellence in sleep medicine and its commitment to providing high-quality patient care. The opportunity to work alongside experienced professionals in a well-equipped facility and contribute to a collaborative team environment is very appealing. Additionally, the position description aligns perfectly with my skills and career aspirations, offering exciting opportunities for professional growth and development within the field of polysomnography.
Key Topics to Learn for Your Polysomnography Interview
Ace your Polysomnography interview by mastering these key areas. Remember, demonstrating a thorough understanding of both theory and practical application is crucial.
- Sleep Stages and Scoring: Understand the different sleep stages (N1, N2, N3, REM), their characteristics, and the criteria used for scoring them according to AASM guidelines. Practice interpreting polysomnographic data to accurately identify these stages.
- Respiratory Events: Become proficient in identifying and differentiating various respiratory disturbances, including apnea, hypopnea, and respiratory effort-related arousals (RERAs). Know the scoring criteria and the implications of these events.
- Cardiac Arrhythmias: Familiarize yourself with common cardiac arrhythmias and their recognition on the polysomnogram. Understand how these are documented and their potential clinical significance.
- Artifact Identification and Management: Master the art of identifying and mitigating artifacts in polysomnographic data. This includes understanding the sources of artifacts (e.g., movement, electrode displacement) and strategies for minimizing their impact on interpretation.
- Polysomnography Equipment and Setup: Be prepared to discuss the various components of a polysomnography system, including electrodes, sensors, and recording devices. Demonstrate understanding of proper setup procedures and troubleshooting techniques.
- Patient Care and Safety: Highlight your understanding of patient safety protocols and procedures during a polysomnography study. This includes proper patient positioning, monitoring, and response to emergencies.
- Report Generation and Interpretation: Discuss your experience in generating clear and concise polysomnography reports that accurately reflect the findings of the study. Explain how you interpret the data and draw clinically relevant conclusions.
Next Steps: Launch Your Polysomnography Career
Mastering Polysomnography opens doors to a rewarding career with significant growth potential. To maximize your job prospects, it’s essential to present yourself effectively. A well-crafted, ATS-friendly resume is your first impression – make it count!
ResumeGemini is a trusted resource to help you build a professional resume that highlights your skills and experience. We provide examples of resumes tailored specifically to Polysomnography professionals, guiding you to create a document that gets noticed. Take the next step towards your dream career – build your winning resume with ResumeGemini today.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.