Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Positive End-Expiratory Pressure (PEEP) interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Positive End-Expiratory Pressure (PEEP) Interview
Q 1. What is Positive End-Expiratory Pressure (PEEP) and how does it work?
Positive End-Expiratory Pressure (PEEP) is a respiratory therapy technique where positive pressure is maintained in the airways at the end of exhalation. Instead of the lungs completely deflating, a small amount of air remains in the alveoli, keeping them open. Think of it like gently inflating a balloon – you wouldn’t let it fully deflate before the next breath.
It works by improving oxygenation and reducing work of breathing. By keeping the alveoli open, PEEP increases the surface area available for gas exchange, allowing for more efficient oxygen uptake. Additionally, it improves lung mechanics by preventing alveolar collapse and improving the distribution of ventilation.
Q 2. Explain the physiological effects of PEEP on the respiratory system.
PEEP’s physiological effects on the respiratory system are multifaceted. Firstly, it improves oxygenation by increasing functional residual capacity (FRC), the volume of air remaining in the lungs after a normal expiration. A higher FRC means more alveoli are open and participating in gas exchange. This leads to improved arterial oxygen tension (PaO2).
Secondly, PEEP reduces intrapulmonary shunting—blood flowing through the lungs without participating in gas exchange due to collapsed alveoli. By keeping alveoli open, it directs more blood flow to ventilated areas, improving the ventilation-perfusion (V/Q) ratio.
Thirdly, PEEP can reduce the work of breathing. By preventing alveolar collapse, it decreases the elastic recoil of the lungs, making it easier for the patient to breathe. However, excessively high PEEP can increase the work of breathing by increasing intrathoracic pressure.
Q 3. Describe the indications for using PEEP in critically ill patients.
PEEP is indicated in critically ill patients experiencing hypoxemia (low blood oxygen levels) despite receiving supplemental oxygen. Specific indications include:
- Acute respiratory distress syndrome (ARDS): PEEP is a cornerstone of ARDS management.
- Pneumonia: To improve oxygenation and reduce the work of breathing.
- Pulmonary edema: To help keep the alveoli open and facilitate gas exchange.
- Post-operative atelectasis: To prevent or treat the collapse of lung segments after surgery.
- Severe asthma or COPD exacerbations: In selected cases, to improve oxygenation.
The decision to use PEEP is individualized based on the patient’s clinical condition and response to therapy.
Q 4. What are the contraindications and potential complications of PEEP?
While PEEP is life-saving for many, it has contraindications and potential complications. Contraindications include:
- Severe hyperinflation of the lungs (air trapping): PEEP can worsen this condition.
- Uncontrolled hypertension: PEEP can increase intrathoracic pressure, potentially leading to increased blood pressure.
- Tension pneumothorax (collapsed lung): PEEP can worsen this life-threatening condition.
Potential complications include:
- Hypotension (low blood pressure): Due to increased intrathoracic pressure.
- Reduced cardiac output: Due to decreased venous return to the heart.
- Barotrauma (lung injury from excessive pressure): Can lead to pneumothorax or pneumomediastinum.
- Volutrauma (lung injury from excessive volume): Can also lead to lung injury.
Careful monitoring and titration of PEEP are crucial to minimize these risks.
Q 5. How do you determine the appropriate level of PEEP for a patient?
Determining the appropriate PEEP level is a complex process requiring clinical judgment and consideration of various factors. There’s no one-size-fits-all answer. It’s a dynamic process, adjusted based on the patient’s response.
Methods for determining PEEP include:
- Clinical assessment: Evaluating the patient’s oxygenation, respiratory rate, and work of breathing.
- Blood gas analysis: Monitoring arterial oxygen tension (PaO2) and carbon dioxide tension (PaCO2) to assess the effectiveness of PEEP.
- Lung mechanics: Assessing respiratory system compliance and resistance.
- PEEP titration strategies: Incrementally increasing PEEP until optimal oxygenation is achieved while minimizing adverse effects. This often involves monitoring hemodynamic parameters (blood pressure, heart rate).
- Evidence-based guidelines: Following recommendations from professional organizations for specific conditions (e.g., ARDS).
Experienced clinicians use a combination of these methods to tailor PEEP to individual patient needs.
Q 6. Explain the relationship between PEEP, oxygenation, and ventilation.
PEEP, oxygenation, and ventilation are intimately interconnected. PEEP primarily aims to improve oxygenation by increasing FRC and reducing intrapulmonary shunting. This leads to a higher PaO2.
However, the relationship isn’t always straightforward. Excessive PEEP can impair ventilation by increasing airway resistance or causing air trapping, leading to hyperinflation and potentially decreased PaCO2. The goal is to find the optimal PEEP level that maximizes oxygenation while maintaining acceptable ventilation and minimizing adverse effects.
A good analogy is a sponge. PEEP keeps the sponge (lungs) partially open, allowing more efficient absorption of water (oxygen). But squeezing it too much (over-PEEPing) can prevent it from absorbing as much water.
Q 7. Discuss the different methods for applying PEEP (e.g., ventilator settings).
PEEP can be applied using various ventilator settings:
- CPAP (Continuous Positive Airway Pressure): Provides continuous positive pressure throughout the respiratory cycle. Often used as a simpler form of PEEP.
- PEEP (as part of volume-controlled or pressure-controlled ventilation): Added to the inspiratory breath to maintain positive pressure at the end of exhalation. This is the most common method in critical care.
- Auto-PEEP (intrinsic PEEP): This is generated by the patient’s own breathing and is not intentionally set on the ventilator. It can be detrimental, leading to air trapping and increased work of breathing. Clinicians must be aware of its presence.
The choice of method depends on the patient’s clinical condition and the ventilator capabilities. Precise control and monitoring are crucial regardless of the method chosen.
Q 8. How do you monitor a patient receiving PEEP therapy?
Monitoring a patient on PEEP involves continuous assessment of several vital parameters to ensure the therapy is effective and safe. Think of it like carefully watching a delicate balance. We need to make sure the benefits outweigh the risks.
Respiratory Mechanics: We closely monitor respiratory rate, tidal volume (the amount of air breathed in and out), and minute ventilation (total air moved per minute). These tell us how well the lungs are functioning. Changes might indicate the need for adjustment.
Oxygenation: SpO2 (oxygen saturation) and PaO2 (partial pressure of oxygen in arterial blood) are crucial. We want to ensure adequate oxygen delivery to the body. A drop could signal a need to increase PEEP or address other underlying issues.
Blood Pressure and Heart Rate: PEEP can impact hemodynamics (the flow of blood through the body). We monitor blood pressure and heart rate to detect any adverse effects, like hypotension (low blood pressure).
Lung Sounds: Auscultation (listening to the lungs with a stethoscope) helps detect any abnormal sounds, such as wheezes or crackles, which could indicate complications like air leaks or atelectasis (collapsed lung segments).
Arterial Blood Gases (ABGs): ABGs provide detailed information about blood oxygen and carbon dioxide levels, pH, and other parameters. They are crucial in fine-tuning PEEP settings.
Chest X-ray: Chest X-rays are periodically performed to visualize the lungs and detect any signs of pneumothorax (collapsed lung) or other complications.
By constantly monitoring these parameters, we can adjust the PEEP level to optimize oxygenation and ventilation while minimizing complications.
Q 9. What are the signs and symptoms of PEEP-related complications (e.g., barotrauma)?
PEEP, while beneficial, can cause complications, primarily related to barotrauma (injury to the lungs and airways due to excessive pressure). Think of it like inflating a balloon too much – it might burst.
Barotrauma: This can manifest as pneumothorax (collapsed lung), pneumomediastinum (air in the chest cavity around the heart), or subcutaneous emphysema (air under the skin). Symptoms include sudden chest pain, shortness of breath, and decreased breath sounds on one side of the chest.
Volutrauma: Excessive tidal volumes, even without high pressure, can injure the lungs. This is less directly related to PEEP but is relevant in the context of overall ventilator management.
Atelectasis: While PEEP aims to prevent it, sometimes high levels can paradoxically cause collapse of some lung regions due to uneven pressure distribution. Symptoms can include decreased breath sounds and oxygen desaturation.
Hypotension: Increased intrathoracic pressure from PEEP can reduce venous return to the heart, leading to low blood pressure. This can manifest as dizziness, lightheadedness, and decreased urine output.
Decreased Cardiac Output: This is another consequence of reduced venous return related to increased intrathoracic pressure. This can lead to organ hypoperfusion and shock in severe cases.
These complications necessitate immediate attention and prompt adjustments to the ventilation strategy.
Q 10. How do you manage PEEP-related complications?
Managing PEEP-related complications requires a rapid and coordinated response. It’s like putting out a fire – quick and decisive action is key.
Addressing Barotrauma: This often necessitates immediate chest tube insertion for pneumothorax or pneumomediastinum to relieve pressure and allow the lung to re-expand. Supplemental oxygen is crucial.
Reducing PEEP: Lowering the PEEP level is the most direct way to alleviate pressure-related complications. This needs to be done cautiously and while closely monitoring the patient’s oxygenation and respiratory mechanics.
Optimizing Tidal Volumes and Respiratory Rate: Adjusting these parameters helps minimize volutrauma and improve overall ventilation.
Fluid Management: Maintaining adequate hydration but avoiding fluid overload is vital. Over-hydration can worsen lung edema.
Supporting Hemodynamics: For hypotension, administering fluids and vasopressors (medications to raise blood pressure) may be necessary.
Providing Supplemental Oxygen: Ensuring adequate oxygen delivery is paramount throughout the management process.
The approach is always tailored to the specific complication and the patient’s overall clinical picture. Close monitoring and collaboration between respiratory therapists, nurses, and physicians are vital for successful management.
Q 11. Describe the differences between PEEP and CPAP.
While both PEEP and CPAP (Continuous Positive Airway Pressure) apply positive pressure to the airways, they differ in their application and clinical goals. Think of it as two different tools for similar, but not identical, jobs.
PEEP: Is used intermittently during mechanical ventilation. It is applied only during the expiratory phase (when the patient is exhaling), keeping the alveoli (tiny air sacs in the lungs) open to improve oxygenation and prevent collapse. It’s part of a larger ventilation strategy.
CPAP: Applies continuous positive pressure to the airways, both during inspiration and expiration. It is frequently used non-invasively to support breathing in patients with sleep apnea or acute respiratory distress. It doesn’t require a ventilator.
In essence, PEEP is a component that can be part of mechanical ventilation, while CPAP is a standalone therapy. PEEP is aimed at improving oxygenation and preventing alveolar collapse, whereas CPAP’s goal is to maintain airway patency and improve ventilation.
Q 12. Explain the concept of auto-PEEP.
Auto-PEEP, also known as intrinsic PEEP, is unintentional positive pressure that remains in the lungs at the end of exhalation due to factors like airway obstruction, reduced expiratory flow, or high respiratory rates. Imagine trying to exhale completely but your airways are slightly blocked, causing some air to remain trapped.
Unlike intentional PEEP set by the ventilator, auto-PEEP is an undesirable phenomenon. It can negatively impact gas exchange and hemodynamics, potentially leading to increased airway pressures, decreased venous return, and increased risk of barotrauma. It’s crucial to identify and manage auto-PEEP to prevent these complications. Strategies include lowering respiratory rate, increasing expiratory time, and using airway maneuvers to improve expiratory flow.
Q 13. How does PEEP affect hemodynamics?
PEEP’s effect on hemodynamics is complex and can be both beneficial and detrimental. It’s a double-edged sword.
Negative Effects: Increased intrathoracic pressure from PEEP can hinder venous return to the heart, reducing preload (the amount of blood returning to the heart) and potentially leading to decreased cardiac output and hypotension. Think of it like squeezing a hose – less blood will flow through.
Positive Effects: In some cases, particularly in patients with hypoxemia (low blood oxygen), the improvement in oxygenation from PEEP can offset the negative hemodynamic effects. Improved oxygenation can also increase cardiac output indirectly by increasing overall tissue perfusion.
The net effect of PEEP on hemodynamics is patient-specific and depends on factors such as the severity of lung disease, the level of PEEP applied, and the patient’s overall cardiovascular status. Careful monitoring of blood pressure, heart rate, and cardiac output is crucial to assess and manage the hemodynamic consequences of PEEP.
Q 14. What is the role of PEEP in ARDS management?
In Acute Respiratory Distress Syndrome (ARDS), PEEP plays a critical role in improving oxygenation and preventing alveolar collapse. ARDS is like a severe lung injury, where the air sacs collapse and oxygen exchange is dramatically reduced. PEEP acts like a support system for the injured lungs.
By maintaining positive pressure at the end of exhalation, PEEP helps to recruit (re-open) collapsed alveoli, improve gas exchange, and reduce the work of breathing. The optimal PEEP level in ARDS is often determined through a trial-and-error approach, guided by arterial blood gas analysis and clinical assessment. This approach is known as PEEP titration and aims to find the level that optimizes oxygenation while minimizing the risks of barotrauma and hemodynamic compromise.
However, high PEEP levels aren’t always the answer. It’s essential to balance the benefits of increased oxygenation against the potential for adverse effects like barotrauma and hemodynamic instability. The latest ARDS management guidelines advocate for a lung-protective ventilation strategy which combines lower tidal volumes, appropriate PEEP, and adequate oxygenation.
Q 15. Discuss the use of PEEP in various respiratory diseases (e.g., pneumonia, asthma).
Positive End-Expiratory Pressure (PEEP) is a respiratory therapy technique that keeps the airways open by applying positive pressure to the lungs at the end of exhalation. In various respiratory diseases, PEEP helps improve oxygenation and ventilation.
In pneumonia, fluid build-up in the alveoli (tiny air sacs in the lungs) reduces lung volume and gas exchange. PEEP helps to recruit collapsed alveoli, improving oxygenation and reducing the work of breathing. Think of it like gently inflating a deflated balloon – PEEP helps ‘inflate’ these collapsed areas of the lung.
In asthma, bronchoconstriction (narrowing of the airways) restricts airflow. While PEEP’s primary effect isn’t directly on bronchoconstriction, it can improve gas exchange by keeping alveoli open and improving lung mechanics. However, it’s crucial to note that PEEP is generally not the first-line treatment for asthma, bronchodilators being the initial choice.
Other conditions where PEEP is utilized include acute respiratory distress syndrome (ARDS), pulmonary edema, and post-surgical lung complications. The specific PEEP level is determined based on the severity of the condition and the individual patient’s response.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you titrate PEEP based on patient response?
Titrating PEEP means adjusting the level of PEEP based on the patient’s clinical response. It’s a dynamic process, not a one-size-fits-all approach. We start with a low PEEP level and gradually increase it while closely monitoring the patient’s oxygenation (SpO2), respiratory rate, heart rate, and blood pressure.
We use clinical parameters to guide our decisions. For instance, if the patient’s oxygen saturation remains low despite increasing FiO2 (fraction of inspired oxygen), we might cautiously increase PEEP to improve oxygenation. However, excessive PEEP can lead to barotrauma (lung injury) and decreased cardiac output. Therefore, we must balance the benefits of improved oxygenation with the potential risks of over-distension.
Titration strategy example: A patient with ARDS might start with 5 cm H2O PEEP. We monitor their oxygenation and hemodynamics closely. If SpO2 remains low, we might incrementally increase PEEP by 2-3 cm H2O, reassessing after each adjustment. If we see a decrease in cardiac output or signs of barotrauma, we’ll reduce PEEP. This process is repeated until we achieve optimal oxygenation with minimal adverse effects.
Q 17. What are the advantages and disadvantages of using different PEEP strategies?
Different PEEP strategies exist, each with advantages and disadvantages:
- Low PEEP (5-8 cm H2O): Advantages: Minimizes barotrauma risk. Disadvantages: May not be sufficient for severe lung injury.
- High PEEP (10-20 cm H2O or higher): Advantages: Better oxygenation in severe cases like ARDS. Disadvantages: Increased risk of barotrauma, decreased cardiac output, and pneumothorax (collapsed lung).
- PEEP titration guided by P/F ratio (PaO2/FiO2): This strategy aims to maintain a specific target P/F ratio, reflecting oxygenation adequacy. Advantage: Data-driven approach. Disadvantage: Can be less responsive to individual patient needs.
- Lung-protective ventilation strategies (low tidal volumes, low respiratory rates): Often used in conjunction with PEEP to minimize lung injury. Advantage: Reduces ventilator-induced lung injury. Disadvantage: Requires careful monitoring.
The choice of PEEP strategy depends on the patient’s specific condition, severity of illness, and overall clinical picture. It’s not a one-size-fits-all approach, and careful assessment and monitoring are crucial.
Q 18. How does PEEP impact lung compliance?
PEEP increases lung compliance (the ease with which the lungs expand). It achieves this by preventing alveolar collapse at end-expiration. By keeping the alveoli open, PEEP reduces the work required to inflate the lungs during the subsequent breath. Think of it like stretching a rubber band – it becomes easier to stretch further after it’s been initially stretched. In the same way, by initially expanding the alveoli using PEEP, subsequent inflation becomes easier.
However, excessively high PEEP can have the opposite effect. If the pressure is too high, it can over-inflate the lungs, leading to decreased compliance and increased risk of barotrauma. This is because the alveoli can become overstretched and less elastic.
Q 19. How does PEEP affect airway pressure?
PEEP directly increases airway pressure. By keeping the alveoli open, PEEP creates a higher baseline pressure within the airways. This higher pressure facilitates gas exchange by improving alveolar ventilation.
However, increased airway pressure can have consequences. It can reduce venous return to the heart, leading to a decrease in cardiac output. This is why it’s crucial to monitor hemodynamic parameters while using PEEP, and to avoid excessive levels.
The relationship between PEEP and airway pressure is complex and depends on other factors such as lung compliance and respiratory system resistance.
Q 20. Explain the concept of recruitment maneuvers in relation to PEEP.
Recruitment maneuvers are techniques used to reopen collapsed alveoli. These maneuvers involve briefly applying a high level of PEEP or positive pressure ventilation to overcome the forces that keep the alveoli closed. This is often done at the beginning of mechanical ventilation in patients with severe lung injury, like ARDS.
The goal is to recruit (reopen) these collapsed alveoli, improving oxygenation. Once the recruitment maneuver is complete, the PEEP is typically reduced to a level that maintains the recruited alveoli without causing overdistension. Recruitment maneuvers are usually short-term interventions, followed by a more sustained lower level of PEEP.
There is ongoing discussion about the best way to perform recruitment maneuvers, and the risks versus benefits must be carefully weighed. The technique requires meticulous monitoring of the patient’s response to avoid lung injury.
Q 21. Discuss the use of PEEP in neonatal and pediatric patients.
In neonatal and pediatric patients, PEEP is used in similar ways as in adults but requires careful consideration due to the smaller size and different lung compliance of these patients.
In neonates, PEEP can be used to treat respiratory distress syndrome (RDS), a condition characterized by immature lungs with surfactant deficiency. PEEP supports alveolar patency and improves oxygenation. The PEEP levels used in neonates are generally lower than in adults, reflecting the smaller lung size and increased risk of complications.
In pediatric patients, PEEP may be utilized in various conditions such as bronchiolitis, pneumonia, and post-surgical respiratory complications. However, the principles of careful titration and monitoring are paramount, and PEEP levels must be adjusted based on the child’s size, age, and response.
The application of PEEP in pediatric and neonatal populations often involves a multidisciplinary team approach, including neonatologists, pediatricians, and respiratory therapists, to ensure the safest and most effective treatment.
Q 22. How do you adjust PEEP based on the patient’s age and comorbidities?
PEEP, or Positive End-Expiratory Pressure, is the amount of pressure remaining in the lungs at the end of exhalation. Adjusting PEEP based on age and comorbidities requires a nuanced approach, as both factors significantly influence lung mechanics and overall health. Generally, we start with lower PEEP values for older adults or those with pre-existing conditions like emphysema or heart failure, due to their potentially fragile lung tissues and increased risk of barotrauma (lung injury from excessive pressure).
For example, a younger, healthy adult with acute respiratory distress syndrome (ARDS) might tolerate a higher PEEP (e.g., 15 cm H2O) than an elderly patient with chronic obstructive pulmonary disease (COPD) who might require a much lower setting (e.g., 5 cm H2O) to avoid complications. The decision-making process involves careful consideration of the patient’s specific clinical picture, including their respiratory rate, oxygenation levels, and lung compliance (how easily the lungs expand). We always prioritize minimizing the risk of adverse effects while optimizing oxygenation.
Comorbidities like hypertension, coronary artery disease, and renal impairment also influence PEEP settings. These conditions might necessitate a more cautious approach, with slower PEEP titration (gradual increases) to monitor for potential hemodynamic instability (changes in blood pressure).
Q 23. What are the nursing considerations when caring for a patient receiving PEEP?
Nursing considerations for patients on PEEP are crucial for patient safety and optimal outcomes. Regular monitoring of vital signs is paramount, particularly blood pressure, heart rate, and oxygen saturation (SpO2). We need to closely observe for signs of complications like hypotension (low blood pressure), decreased urine output (indicating potential renal issues), and pneumothorax (collapsed lung).
- Respiratory Assessment: Frequent assessment of respiratory rate, depth, and effort, as well as auscultation (listening to lung sounds) to identify any abnormal findings like crackles or wheezes.
- Fluid Balance: Meticulous monitoring of fluid intake and output is necessary, as PEEP can affect fluid balance in the body.
- Skin Integrity: Patients on mechanical ventilation often require endotracheal intubation, increasing the risk of skin breakdown. Prophylactic measures like frequent repositioning and skin care are vital.
- Patient Comfort: We need to provide measures to improve patient comfort, including pain management, proper positioning, and emotional support. Anxiety and fear are common among mechanically ventilated patients, and reassuring communication can be very beneficial.
A recent case I managed involved an elderly patient with COPD and pneumonia. We had to be extremely cautious with PEEP titration, meticulously monitoring her blood pressure and urine output to avoid complications. Her response to PEEP was carefully evaluated, leading to a successful outcome.
Q 24. Explain the importance of patient monitoring during PEEP therapy.
Patient monitoring during PEEP therapy is not merely a routine procedure; it’s the cornerstone of safe and effective ventilation. Continuous monitoring is essential to detect early signs of complications and to adjust the PEEP settings accordingly. Imagine PEEP as a delicate balance—too little, and the patient may not get adequate oxygen; too much, and they risk complications. Thus, constant vigilance is crucial.
- Arterial Blood Gases (ABGs): Regular ABGs provide precise measurements of blood oxygen and carbon dioxide levels, guiding adjustments to PEEP and other ventilator settings.
- Hemodynamic Monitoring: Close observation of blood pressure and heart rate is crucial, as PEEP can impact cardiac output.
- Respiratory Mechanics: Parameters like peak inspiratory pressure (PIP), plateau pressure, and compliance are vital to assess lung mechanics and prevent overdistention.
- Clinical Assessment: Regular assessment of the patient’s overall condition, including mental status, skin color, and breath sounds, provides a holistic view of their response to PEEP.
For instance, a sudden drop in blood pressure during PEEP application could indicate decreased cardiac output, demanding immediate attention and potential PEEP reduction. Similarly, increasing plateau pressure might suggest lung overdistention, requiring careful reassessment of the ventilation strategy.
Q 25. What are some common mistakes to avoid when using PEEP?
Avoiding common mistakes in PEEP application is vital to prevent adverse events. Some crucial pitfalls to avoid include:
- Overly Rapid PEEP Titration: Sudden and substantial increases in PEEP can overwhelm the lungs and lead to barotrauma or hemodynamic compromise. Gradual titration, with close monitoring, is crucial.
- Ignoring Patient-Specific Factors: Failing to consider individual patient characteristics such as age, comorbidities, and overall health status can lead to inappropriate PEEP levels and complications.
- Neglecting Ongoing Monitoring: Continuous monitoring of vital signs, respiratory mechanics, and ABGs is essential to promptly detect and address potential issues.
- Insufficient Training and Experience: Proper training and experience are critical for safe and effective PEEP application. Inadequate knowledge can lead to incorrect settings and missed complications.
For example, applying a high PEEP to a patient with severe emphysema without close monitoring can result in lung damage. Similarly, failing to monitor for hypotension during PEEP titration can lead to circulatory collapse.
Q 26. Describe your experience with different types of ventilators and their PEEP capabilities.
My experience spans a variety of ventilators, including volume-cycled, pressure-cycled, and high-frequency oscillatory ventilators. Each ventilator has unique PEEP capabilities and functionalities. Volume-cycled ventilators deliver a predetermined tidal volume, with PEEP setting independent of tidal volume delivery. Pressure-cycled ventilators deliver breaths to a pre-set pressure, and PEEP is integrated into the pressure-support system. High-frequency oscillatory ventilators use rapid oscillations to deliver ventilation, with PEEP incorporated to maintain lung inflation.
I’ve worked extensively with Hamilton Medical ventilators (G5, H900), Draeger ventilators (Evita V500), and Philips ventilators (V60). These different models offer varying levels of sophistication in PEEP management, from simple manual adjustments to sophisticated auto-PEEP calculation and management algorithms. The choice of ventilator and its associated PEEP capabilities depends heavily on the patient’s condition and clinical needs. In my experience, the key is not necessarily the specific model but rather the clinician’s understanding of PEEP physiology and the ability to adjust it appropriately.
Q 27. How do you troubleshoot problems related to PEEP delivery?
Troubleshooting problems related to PEEP delivery involves a systematic approach. First, we must identify the specific problem – is the PEEP not being delivered at all, or is it delivering incorrectly?
- Check ventilator settings and connections: Verify that the PEEP setting is correctly programmed on the ventilator and that all connections, including the airway, are secure and free of leaks. Leaks are a common cause of inaccurate PEEP delivery.
- Assess the patient’s respiratory status: Evaluate the patient’s respiratory mechanics, including compliance and resistance. Increased airway resistance or decreased compliance can affect PEEP delivery.
- Review ABGs and other physiological data: Analyze ABGs and other vital signs to determine if oxygenation and ventilation are adequate. Inadequate oxygenation despite appropriate PEEP could suggest other issues, such as a shunt or ventilation-perfusion mismatch.
- Consider alternative causes: If all else fails, consider other possible causes, such as pneumothorax or other lung pathologies. Imaging studies, like chest X-rays, might be necessary.
For example, if the delivered PEEP is lower than set, we need to check for leaks, then reassess connections and ventilator settings. If oxygenation remains poor despite sufficient PEEP, we may need to investigate further, possibly with a chest X-ray to rule out pneumothorax. It’s a systematic, problem-solving approach based on careful observation and analysis.
Q 28. Explain how you would educate a patient and their family about PEEP therapy.
Educating patients and their families about PEEP therapy is crucial for their understanding and cooperation. We must explain the rationale behind the treatment in a clear, concise, and empathetic manner, avoiding overwhelming technical jargon.
I typically start by explaining that PEEP is a technique to help keep the lungs open and improve oxygen levels. I use simple analogies—imagine the lungs as a balloon. PEEP keeps the balloon slightly inflated even after exhaling, preventing collapse and enabling more efficient breathing. I explain that PEEP is delivered through a ventilator and that it’s a temporary measure to assist breathing during critical illness.
I also discuss potential side effects, such as low blood pressure or discomfort, emphasizing the importance of monitoring and the measures taken to minimize these risks. I encourage questions and answer them openly and honestly. Finally, I provide written materials and contact information to ensure consistent and readily available information for the patients and their loved ones. It’s about empowering them with knowledge and fostering a collaborative approach to their care.
Key Topics to Learn for Positive End-Expiratory Pressure (PEEP) Interview
- Physiological Effects of PEEP: Understand how PEEP impacts lung mechanics, gas exchange, and hemodynamics. Be prepared to discuss the effects on oxygenation, ventilation, and cardiac output.
- Indications and Contraindications for PEEP: Know the specific clinical situations where PEEP is beneficial (e.g., ARDS, pulmonary edema) and when it’s contraindicated (e.g., severe air trapping, tension pneumothorax). Be ready to explain your reasoning.
- PEEP Levels and Titration: Discuss the factors influencing the selection of appropriate PEEP levels and the process of titrating PEEP based on clinical response. This includes understanding the potential risks of excessive PEEP.
- Monitoring and Assessment: Describe the methods used to monitor the effectiveness of PEEP, such as arterial blood gas analysis, oxygen saturation, and clinical observation. Be prepared to discuss the interpretation of these parameters.
- Complications of PEEP: Outline potential adverse effects associated with PEEP, such as barotrauma, volutrauma, hypotension, and decreased cardiac output. Knowing how to mitigate these risks is crucial.
- PEEP Strategies and Modes: Familiarize yourself with different ventilation modes that utilize PEEP, including volume-controlled ventilation and pressure-controlled ventilation. Understand the advantages and disadvantages of each.
- Practical Application in Specific Patient Populations: Be prepared to discuss the application of PEEP in different patient populations, such as those with acute respiratory distress syndrome (ARDS) or chronic obstructive pulmonary disease (COPD), considering their unique physiological characteristics.
- Problem-Solving Scenarios: Practice analyzing hypothetical case studies where PEEP is involved. Consider scenarios where PEEP adjustments are needed to optimize ventilation and oxygenation.
Next Steps
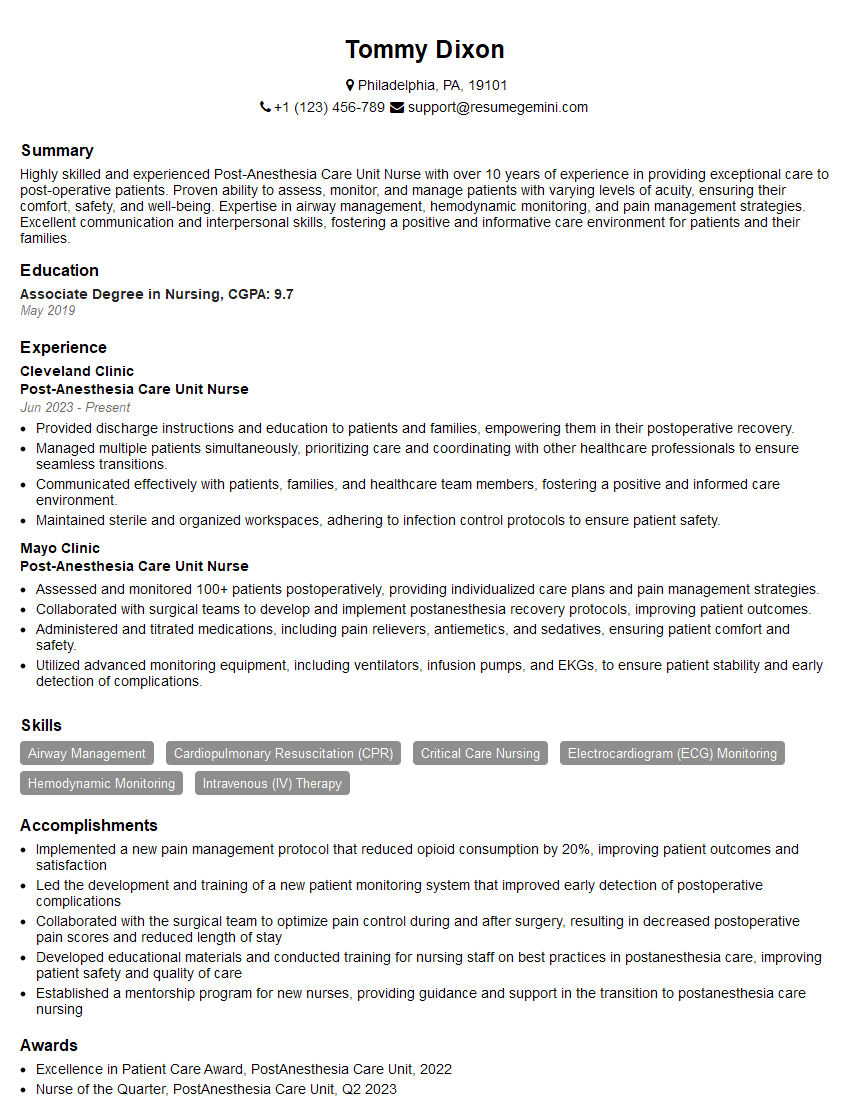
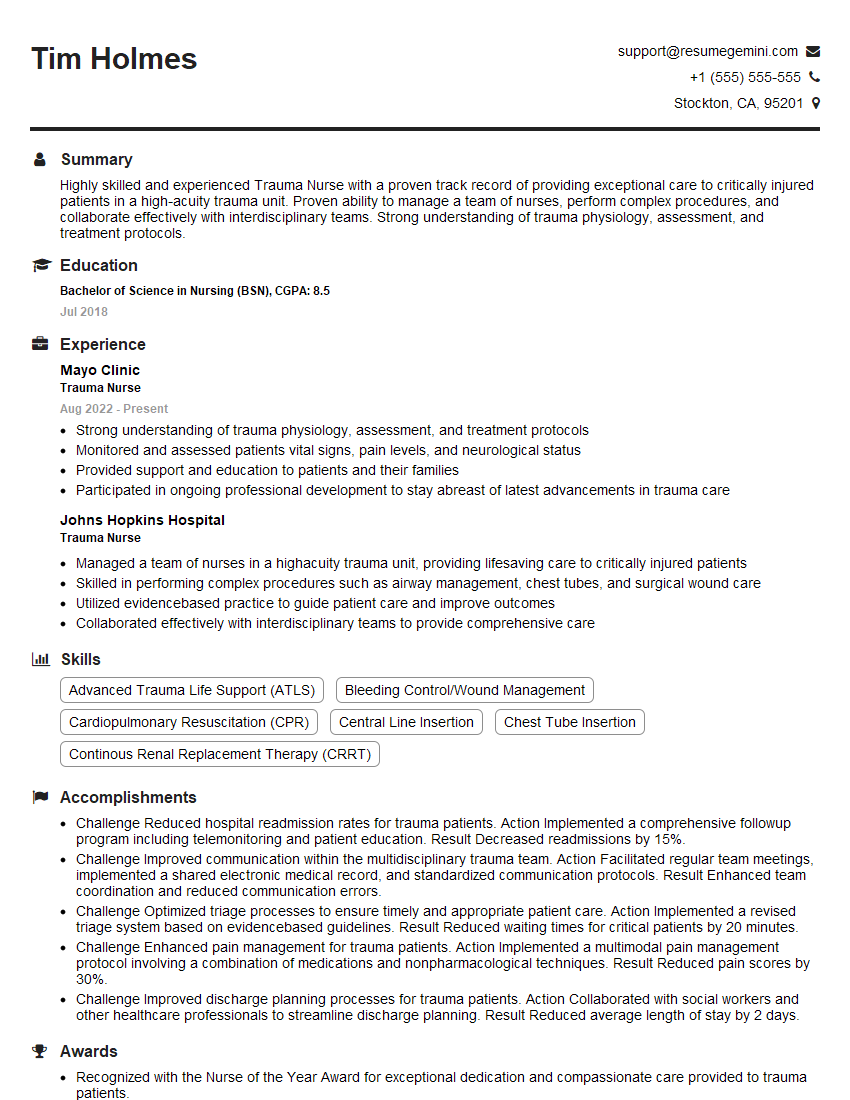
Mastering Positive End-Expiratory Pressure (PEEP) is crucial for career advancement in respiratory therapy and related fields. A strong understanding of PEEP demonstrates a high level of clinical competence and problem-solving skills, making you a valuable asset to any healthcare team. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Positive End-Expiratory Pressure (PEEP) related roles are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.