Unlock your full potential by mastering the most common Prepare and Maintain Medical Records interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Prepare and Maintain Medical Records Interview
Q 1. Explain the importance of accurate medical record keeping.
Accurate medical record-keeping is paramount for several reasons. It forms the cornerstone of high-quality patient care, ensuring continuity and consistency across treatments and providers. Think of it as a patient’s medical history book, constantly updated with every appointment, test result, or procedure. Without accurate records, misdiagnosis, medication errors, and duplicated procedures become significantly more likely. Accurate records also protect the healthcare provider, as they serve as legal documentation in case of malpractice claims or disputes.
- Improved Patient Care: Comprehensive records allow healthcare professionals to make informed decisions based on a complete understanding of a patient’s medical history.
- Legal Protection: Accurate documentation protects both the patient and provider in legal matters.
- Continuity of Care: Facilitates seamless transitions between healthcare settings and providers.
- Public Health Surveillance: Aggregated data from accurate medical records contributes to public health research and tracking disease outbreaks.
Q 2. Describe your experience with Electronic Health Record (EHR) systems.
I have extensive experience with various EHR systems, including Epic, Cerner, and Meditech. My expertise encompasses data entry, record maintenance, report generation, and system troubleshooting. In my previous role at [Previous Employer Name], I was responsible for training new staff on the use of our EHR system, Epic. I streamlined data entry processes, leading to a 15% increase in efficiency within the first quarter. I am proficient in using EHRs to access and update patient information, generate reports for regulatory compliance, and ensure data integrity. Furthermore, I’m adept at navigating different modules within these systems, including scheduling, billing, and patient portals. For example, I developed a customized report in Epic that tracked patient medication adherence, which significantly aided in improving patient outcomes.
Q 3. How do you ensure patient confidentiality when handling medical records?
Patient confidentiality is my utmost priority. I strictly adhere to HIPAA regulations and all relevant privacy laws. This means understanding and following access control protocols, utilizing secure systems for data storage and transmission, and never sharing patient information with unauthorized individuals. For example, I would never leave a patient chart unattended or discuss a patient’s case in public areas. I also utilize the built-in security features of the EHR system, such as password protection, audit trails, and access restrictions based on roles and responsibilities. Before accessing any patient information, I verify the patient’s identity using appropriate methods. Any breach or suspected breach is immediately reported according to established protocols.
Q 4. What is your process for correcting errors in medical records?
My process for correcting errors involves making a clear and concise amendment, never obliterating the original entry. I would add a correction using a standardized method, such as an addendum or a correction line, clearly indicating the date and time of the correction, and my initials or electronic signature. I’d never use correction fluid or attempt to erase information. The original entry remains visible, along with the correction, ensuring the complete and accurate record of events. This method maintains transparency and accountability, crucial for legal and ethical considerations. For example, if I incorrectly recorded a patient’s blood pressure, I would add a line stating: “Correction: Blood pressure previously recorded as 120/80 mmHg; corrected to 130/90 mmHg. [Initials] [Date/Time]”
Q 5. How do you handle requests for release of information?
Handling requests for release of information requires meticulous attention to detail and strict adherence to legal and ethical guidelines. I begin by verifying the identity of the requester and the authorization provided by the patient. Then I check if the request aligns with the patient’s consent and the permissible uses and disclosures defined by HIPAA. If authorization is valid, I will prepare the requested records ensuring they only contain the specific information authorized for release. I will also maintain a log of all requests and releases, documenting the date, recipient, and information released. If the request is not authorized or incomplete, I would clearly explain the reasons for denial or request additional information.
Q 6. What are the legal and ethical considerations related to medical record management?
Legal and ethical considerations in medical record management are paramount. HIPAA, state privacy laws, and professional codes of ethics (e.g., the AMA Code of Medical Ethics) dictate how we handle patient information. Key considerations include: confidentiality (protection of sensitive information), integrity (accuracy and completeness of data), availability (timely access to information), and security (protection against unauthorized access and disclosure). Non-compliance can lead to severe penalties, including fines and legal action. For instance, failure to maintain proper confidentiality can result in significant legal repercussions for the provider and the institution. Therefore, maintaining up-to-date knowledge of all relevant laws and regulations is essential for ethical and legal medical record management.
Q 7. Explain your experience with medical record coding and billing procedures.
My experience with medical record coding and billing procedures includes familiarity with ICD-10 and CPT coding systems. I understand the importance of accurate coding for proper reimbursement and compliance with regulatory guidelines. In a previous role, I worked with a billing team to improve coding accuracy, leading to a reduction in claim denials. I have experience with various billing software and am comfortable navigating insurance claim processes. This includes preparing and submitting claims, managing accounts receivable, and tracking payments. I also understand the importance of accurate documentation to support billing and coding practices to ensure correct reimbursement. For instance, I can identify and correct coding errors that might lead to claim denials or underpayment. I possess a strong understanding of the relationships between medical documentation, coding and proper reimbursement.
Q 8. How do you prioritize tasks when managing a large volume of medical records?
Prioritizing tasks in medical record management involves a strategic approach combining urgency, importance, and regulatory compliance. Think of it like a triage system in an emergency room – the most critical cases get immediate attention. I use a combination of methods:
- Urgency and Importance Matrix: I categorize tasks based on urgency (immediate, short-term, long-term) and importance (critical, important, less important). This helps visualize which tasks require immediate action and which can be scheduled.
- Regulatory Compliance: Tasks related to legal and regulatory requirements (like HIPAA compliance audits) always take precedence. These are crucial for maintaining the integrity of patient data and avoiding legal issues.
- Workflow Management Software: Utilizing a system that allows for task assignment, prioritization, and tracking ensures efficient allocation of resources and helps meet deadlines. This could include features like automated reminders and progress monitoring.
- Time Blocking: I allocate specific time blocks for high-priority tasks to minimize distractions and ensure focused work. For instance, a specific block might be dedicated to completing urgent chart requests.
For example, if I receive a subpoena for patient records, that immediately becomes a top priority, overriding other tasks. Conversely, routine chart maintenance might be scheduled for a specific time during the week.
Q 9. Describe your experience with medical record audits and compliance.
My experience with medical record audits and compliance is extensive. I’ve participated in numerous internal and external audits, ensuring compliance with HIPAA, state regulations, and accreditation standards. This involved:
- Chart Reviews: Thorough reviews of medical records to ensure completeness, accuracy, and adherence to established documentation standards. This includes verifying that all necessary information is present, legible, and properly documented according to legal requirements.
- Policy and Procedure Development: I’ve actively contributed to the development and updating of policies and procedures related to medical record management, ensuring they align with current regulations and best practices. This is crucial for maintaining regulatory compliance.
- Corrective Action Plans: I’ve developed and implemented corrective action plans to address any deficiencies identified during audits. This ensures continuous improvement in our record-keeping practices and safeguards patient information.
- Staff Training: I’ve provided training to staff on proper medical record documentation, including accurate coding and compliance with regulatory guidelines. This is vital in maintaining consistent quality across all records.
In one instance, an external audit identified a minor deficiency in our record-retention policies. I immediately developed and implemented a revised policy, ensuring compliance and providing documentation to the auditors.
Q 10. How do you maintain the integrity and security of electronic medical records?
Maintaining the integrity and security of electronic medical records (EMRs) requires a multi-faceted approach. This involves:
- Access Control: Implementing robust access control measures, including user authentication, authorization, and audit trails. Only authorized personnel should have access to patient information, and all accesses are tracked and monitored for security breaches.
- Data Encryption: Utilizing encryption technologies to protect data both in transit and at rest. This prevents unauthorized access even if the system is compromised.
- Regular Backups: Implementing a regular backup and recovery system to protect against data loss due to hardware failure, software errors, or cyberattacks. This is a vital component of ensuring data integrity and business continuity.
- Firewall and Anti-Virus Software: Utilizing firewalls and anti-virus software to prevent unauthorized access and protect against malware. This safeguards the system from external threats.
- Regular Security Audits: Conducting regular security audits and vulnerability assessments to identify and address any security weaknesses. This helps proactively mitigate potential risks.
- Employee Training: Educating employees on security policies and procedures to prevent human error, a major cause of data breaches. Regular training reinforces security protocols and best practices.
For example, our EMR system uses multi-factor authentication and encrypts all data at rest and in transit. We also conduct regular security audits and penetration testing to identify and address vulnerabilities.
Q 11. What is your experience with different types of medical record formats (paper, digital)?
I have extensive experience with both paper-based and digital medical record formats. Paper-based records require meticulous organization and storage to ensure easy retrieval and prevent damage. Digital records, while offering increased efficiency, require a strong understanding of data security and management protocols.
- Paper-based Records: My experience includes organizing, indexing, filing, and retrieving paper charts, ensuring they are properly labeled, stored in a secure environment, and protected from damage. I’m also proficient in converting paper records to digital formats when necessary.
- Digital Records (EMR/EHR): I’m experienced in using various EMR/EHR systems, managing patient data, generating reports, and ensuring data integrity. This includes proficiency in using system features for data entry, updating, and retrieval.
- Hybrid Systems: I’ve worked with organizations that utilize a combination of paper and digital records. This requires managing both systems effectively and ensuring data consistency between them.
In a previous role, we transitioned from a primarily paper-based system to a fully digital EMR. This required extensive planning, staff training, and data migration, which I played a key role in.
Q 12. How do you handle requests for amendments or corrections to medical records?
Handling requests for amendments or corrections to medical records requires careful adherence to legal and regulatory guidelines. The process typically involves:
- Verification of Request: Confirming the identity of the individual requesting the amendment and their authority to do so. This often includes verifying their relationship with the patient.
- Review of the Record: Carefully reviewing the portion of the record that requires amendment to understand the context and reason for the change request.
- Documentation of the Amendment: Documenting the amendment clearly and accurately, including the date, time, reason for the change, and the individual making the change. This maintains a complete audit trail.
- Attaching the Amendment: Attaching the amendment to the original record, rather than overwriting it. This preserves the original record and shows the history of any changes.
- Notification of Relevant Parties: Notifying relevant parties of the amendment, as required by regulatory guidelines and internal policies. This might include notifying the patient or referring physician.
For example, if a patient requests a correction to their allergy information, I carefully review the request, update the record with the correction, and document the change, including the date, time, reason, and my initials. This creates an auditable trail ensuring transparency and accuracy.
Q 13. Describe your experience with HIPAA regulations.
My understanding of HIPAA regulations is comprehensive. I’m familiar with all its key provisions, including:
- Privacy Rule: Protecting the privacy of individually identifiable health information (PII). This includes understanding permitted disclosures, patient rights, and requirements for obtaining authorization.
- Security Rule: Ensuring the confidentiality, integrity, and availability of electronic protected health information (ePHI). This involves implementing appropriate administrative, physical, and technical safeguards.
- Breach Notification Rule: Understanding the procedures for notifying individuals and regulatory authorities in the event of a data breach. This involves timely notification and reporting to the appropriate bodies.
- Enforcement Rule: Understanding the penalties for non-compliance with HIPAA regulations. This includes understanding civil and criminal penalties.
I’ve implemented numerous HIPAA-compliant procedures, including developing policies and procedures, conducting staff training, and managing data breaches according to HIPAA guidelines. We maintain detailed logs of all access to patient information and undergo regular HIPAA audits to ensure ongoing compliance.
Q 14. How do you ensure the timely completion of medical record tasks?
Ensuring timely completion of medical record tasks requires a combination of efficient workflow management, prioritization, and effective communication. I utilize:
- Prioritization techniques (as described in answer 1): This ensures that the most urgent and important tasks are addressed first.
- Clear Deadlines and Expectations: Setting clear deadlines for tasks and communicating those expectations to all involved parties. This maintains accountability and helps keep projects on track.
- Workflow Optimization: Streamlining workflows to eliminate unnecessary steps and improve efficiency. This includes reviewing processes regularly and identifying areas for improvement.
- Effective Communication: Maintaining open communication with all stakeholders to address any delays or roadblocks promptly. This could involve reporting progress to supervisors or addressing issues with other departments.
- Technology Utilization: Using technology to automate tasks and improve efficiency. This might include using workflow management software or electronic signature platforms.
For example, by implementing a new workflow for chart completion, we reduced the average processing time by 20%, improving turnaround times and increasing patient satisfaction.
Q 15. What are your strategies for managing stress and deadlines in a fast-paced environment?
Managing stress and deadlines in a fast-paced medical records environment requires a proactive and multifaceted approach. Think of it like a tightrope walk – you need balance and focus. My strategies revolve around prioritization, time management, and self-care.
- Prioritization: I utilize tools like daily task lists and prioritize tasks based on urgency and importance. For example, ensuring immediate completion of critical tasks, like emergency room records, before tackling less time-sensitive ones.
- Time Management Techniques: I employ the Pomodoro Technique, working in focused bursts with short breaks to maintain concentration and prevent burnout. This helps me avoid feeling overwhelmed by large tasks.
- Self-Care: Recognizing that burnout is a real risk, I prioritize sufficient sleep, regular exercise, and breaks throughout the day. Taking short walks or practicing mindfulness helps me stay refreshed and focused.
- Delegation (where applicable): If possible, I delegate tasks appropriately to ensure workload balance and effective resource utilization. This maximizes overall team efficiency.
By combining these strategies, I maintain a calm and productive workflow even during peak periods.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you use technology to improve efficiency in medical record management?
Technology is an indispensable tool for enhancing efficiency in medical record management. It allows for automation, improved accuracy, and enhanced accessibility.
- Electronic Health Records (EHR) Systems: Proficient use of EHR systems, such as Epic or Cerner, streamlines documentation, reduces paperwork, and facilitates quick retrieval of information. Features like automated data entry and templated notes significantly improve efficiency.
- Optical Character Recognition (OCR) Software: This technology digitizes paper documents, converting them into searchable text, greatly accelerating the indexing and retrieval process. Imagine the time saved in manually entering data from hundreds of paper charts!
- Data Analytics Tools: These tools can identify trends and patterns in patient data, enabling proactive quality improvements and more effective resource allocation. For example, identifying bottlenecks in the record processing workflow.
- Cloud-based storage: Secure cloud storage solutions provide easy access to records from anywhere, improving collaboration and reducing the risk of data loss.
Through the strategic utilization of these technologies, I can manage a larger volume of records with increased accuracy and speed, allowing me to focus more on the crucial task of ensuring data integrity.
Q 17. What is your understanding of the different types of medical record documentation?
Medical record documentation encompasses a wide array of formats and purposes, all aimed at providing a comprehensive picture of a patient’s health journey.
- Progress Notes: These chronicle the patient’s condition, treatment progress, and response to therapy. They often utilize SOAP notes (Subjective, Objective, Assessment, Plan) format.
- Physician Orders: These include instructions for medications, treatments, and tests. They are crucial for coordinating patient care.
- Laboratory and Radiology Reports: These provide objective findings from diagnostic tests, such as blood work, X-rays, and MRIs.
- Consultation Reports: These document the opinions and recommendations from specialists who have examined the patient.
- Discharge Summaries: These summarize the patient’s hospital stay, including diagnosis, treatment received, and post-discharge instructions.
- Medication Reconciliation Records: These lists track all medications a patient is currently taking, comparing current medications with previous records.
Understanding the nuances of each type is essential for ensuring the accuracy and completeness of the medical record.
Q 18. Describe your experience with data entry and verification procedures.
My experience with data entry and verification is extensive and emphasizes accuracy and attention to detail. Data entry is more than just typing; it’s about ensuring data integrity.
- Data Entry Techniques: I am proficient in utilizing various data entry methods, from keyboard entry to utilizing scanning and OCR technologies. I consistently double-check my work to minimize errors.
- Verification Procedures: I rigorously follow established verification procedures to ensure accuracy and consistency. This includes cross-referencing data from multiple sources, verifying spellings and medical terminology, and flagging inconsistencies for further review.
- Data Quality Control Measures: I proactively look for inconsistencies or missing data. This might involve comparing lab results to physician’s notes, verifying dosages, or comparing medication lists against insurance records. I utilize data validation tools within EHR systems.
Maintaining data integrity is paramount. A small error in a medical record can have significant consequences, so my commitment to precision is unwavering.
Q 19. How do you identify and resolve discrepancies in medical records?
Discrepancies in medical records can arise from various sources, including manual errors, conflicting information, or missing documentation. Identifying and resolving these discrepancies is critical for maintaining patient safety and accurate record-keeping.
- Identification of Discrepancies: I use a combination of automated flagging systems within EHRs and manual review processes. Automated systems highlight conflicting information, while manual reviews involve careful comparison of information across different parts of the record.
- Resolution Strategies: Once a discrepancy is identified, I investigate its source. This might involve contacting the physician or other healthcare professionals who contributed to the record. Clarification, additional testing, or amended notes might be necessary.
- Documentation of Corrections: All corrections and resolutions are meticulously documented, including the date, time, and reason for the change. This preserves audit trails and ensures transparency.
Resolving discrepancies requires attention to detail and a methodical approach. The goal is to ensure that the record accurately reflects the patient’s health status and treatment.
Q 20. How do you maintain the organization and accessibility of medical records?
Maintaining the organization and accessibility of medical records is crucial for efficient workflow and patient care. Think of it as a well-organized library – easy to find what you need when you need it.
- Filing Systems: I utilize both electronic and physical filing systems, depending on the institution’s procedures. Whether electronic or paper, the system must be logical and easy to navigate, using standardized naming conventions and clear indexing methods.
- Data Security & Privacy: Strict adherence to HIPAA regulations is essential. Access control mechanisms must ensure only authorized personnel can access specific records, and all systems must be secure to prevent unauthorized access or data breaches.
- Regular Audits: Periodic audits are conducted to ensure records are properly filed, accessible, and meet compliance standards. This prevents data loss and ensures continued efficient access.
- Record Retention Policies: I ensure compliance with relevant record retention policies, properly archiving records as needed and securely destroying outdated documents when necessary.
By implementing these strategies, I create a system that balances efficiency, security, and compliance.
Q 21. Explain your knowledge of medical terminology and abbreviations.
A strong understanding of medical terminology and abbreviations is fundamental to accurately preparing and maintaining medical records. It’s like learning a specialized language for clear communication.
- Terminology: I possess a comprehensive understanding of medical terms related to anatomy, physiology, diseases, and treatments. This allows me to accurately interpret and transcribe clinical information.
- Abbreviations: I am familiar with common medical abbreviations, such as
prn(as needed),bid(twice daily),qhs(at bedtime), and numerous others. Knowing their meanings is essential for correctly interpreting physician orders. - Resources: I regularly consult medical dictionaries and online resources to ensure accuracy, particularly when encountering unfamiliar terms or abbreviations.
- Contextual Understanding: I understand that context is key. The meaning of an abbreviation or term can depend on the clinical context. For example,
BPcould mean blood pressure, or in another context, it might mean bone pain.
Maintaining accuracy in medical records requires a detailed understanding of the language used. A wrong interpretation of a term or abbreviation can have serious consequences. My commitment to continuous learning ensures that my medical terminology remains up to date and accurate.
Q 22. How do you handle sensitive patient information with discretion?
Handling sensitive patient information requires unwavering adherence to privacy regulations like HIPAA. Think of it like guarding a national treasure – every precaution must be taken. This starts with understanding the information’s sensitivity. For example, diagnoses of mental health conditions or sexually transmitted infections require a higher level of confidentiality than, say, a patient’s blood type.
Practically, this means limiting access to patient records only to authorized personnel who have a legitimate need to know. We use secure access systems with unique passwords and logins, and we never leave patient files unattended. Physical records are locked away, and electronic records are protected by robust encryption and firewalls. Furthermore, I always follow the principle of ‘need to know,’ meaning I only share information with individuals directly involved in a patient’s care. If I’m unsure whether I can share information, I always consult with my supervisor or the relevant compliance officer.
Q 23. Describe your experience working within a team setting.
I thrive in collaborative team environments. In my previous role, our team consisted of physicians, nurses, medical assistants, and other record-keeping professionals. We worked closely together to ensure efficient and accurate record management. For example, we regularly held team meetings to discuss workflow improvements, address challenges with record completion, and share best practices. My role often involved coordinating with nurses to ensure that all relevant information was documented after procedures and assisting physicians with obtaining specific patient records for consultations.
I excel at delegating tasks effectively, providing support to colleagues, and contributing actively to a positive team dynamic. Open communication and mutual respect are essential, and I’m adept at actively listening to different viewpoints to find the best solutions to problems.
Q 24. What are your skills in using medical record software?
I’m proficient in several leading medical record software systems, including Epic, Cerner, and Meditech. My skills encompass all aspects of these systems, from data entry and chart retrieval to generating reports and managing electronic signatures. For instance, in my last position at [Previous Employer Name], I used Epic to streamline patient check-in procedures, reducing wait times by 15%. I’m also adept at troubleshooting software issues and providing training to colleagues on new features. Understanding these software systems isn’t just about using them; it’s about maximizing their efficiency for better patient care.
Beyond proficiency in specific software, I am quick to learn new systems. The healthcare IT landscape is ever-evolving, and staying updated is critical for effective record management.
Q 25. How do you prioritize patient privacy when sharing information?
Prioritizing patient privacy when sharing information is paramount. It’s not just about following the rules; it’s about upholding a moral obligation. We follow strict protocols, adhering to HIPAA and other relevant regulations. Before sharing any information, I verify the recipient’s identity and their right to access the information. I only share the minimum necessary information required for the specific purpose, ensuring I’m not divulging unnecessary details.
For instance, if a physician needs to consult a specialist about a patient’s condition, I would only share the relevant medical history, test results, and current treatment plan. I would never share personal details unrelated to the medical reason for the consultation, such as financial information or social habits.
Q 26. Describe your experience with record retention policies and procedures.
Experience with record retention policies is crucial for compliance and efficient record management. I understand that these policies vary depending on the type of record and governing regulations. I’m familiar with state and federal laws regarding the retention periods for both electronic and paper-based records. This includes adhering to requirements for storing records securely and ensuring accessibility when needed.
In my previous role, I was responsible for reviewing and updating our record retention policy annually to ensure compliance with legal and accreditation standards. We used a combination of physical and electronic storage systems for records with different retention periods. For example, some records were archived after seven years, while others needed to be maintained indefinitely, depending on the type of record and relevant legislation. Regular audits were also conducted to ensure our adherence to the policy.
Q 27. How familiar are you with the different types of medical record requests?
I’m very familiar with the diverse types of medical record requests. These range from routine requests from patients accessing their own records to subpoenas for legal proceedings or requests from other healthcare providers for consultations or transfers of care. Each request type has its own specific procedures and legal requirements.
For example, patient requests usually require verification of identity, and access may be limited based on specific laws. Legal requests involve careful review and adherence to the legal process, potentially requiring consultation with legal counsel. Requests from other healthcare providers usually require authorized release forms and a careful consideration of the patient’s privacy rights.
Q 28. What steps do you take to ensure the confidentiality of patient information during data entry?
Ensuring confidentiality during data entry is a core tenet of my work. This starts with logging into the system using my secure, unique credentials. I always ensure that I’m entering data in a secure location, away from prying eyes. I also double-check all data entered to prevent errors that may compromise confidentiality. For example, I ensure that all patient identifiers are accurate and consistent throughout the record.
Further, I never leave my computer unattended while logged into the patient records system and immediately log out when I’m finished. I also regularly update my passwords to maintain strong security protocols. Any suspected security breaches or data compromises are reported immediately to the appropriate authorities.
Key Topics to Learn for Prepare and Maintain Medical Records Interview
- Medical Terminology and Abbreviations: Understanding common medical terms and abbreviations is fundamental for accurate record-keeping. Practice deciphering and correctly interpreting medical jargon.
- Electronic Health Record (EHR) Systems: Become proficient in navigating and utilizing various EHR systems. Understand data entry procedures, data retrieval methods, and maintaining data integrity within these systems. Practice with common EHR software if possible.
- Medical Record Organization and Structure: Learn the principles of organizing medical records for efficient retrieval and compliance with regulations (e.g., HIPAA). Understand the importance of chronological order and accurate indexing.
- Data Privacy and Confidentiality: Master the legal and ethical considerations surrounding patient data privacy and confidentiality. Understand HIPAA regulations and best practices for protecting sensitive information.
- Record Maintenance and Retention Policies: Familiarize yourself with various record retention policies and procedures. Understand how to manage both physical and digital records, including archiving and destruction protocols.
- Chart Auditing and Quality Control: Learn how to perform chart audits to ensure accuracy, completeness, and compliance. Understand techniques for identifying and correcting errors or inconsistencies in medical records.
- Problem-Solving in Record Management: Practice identifying and resolving common challenges in medical record management, such as missing information, discrepancies, or access issues. Develop strategies for effective troubleshooting.
- Coding and Billing (if applicable): Depending on the specific role, understanding basic medical coding and billing principles can be beneficial. This will demonstrate a broader understanding of the healthcare revenue cycle.
Next Steps
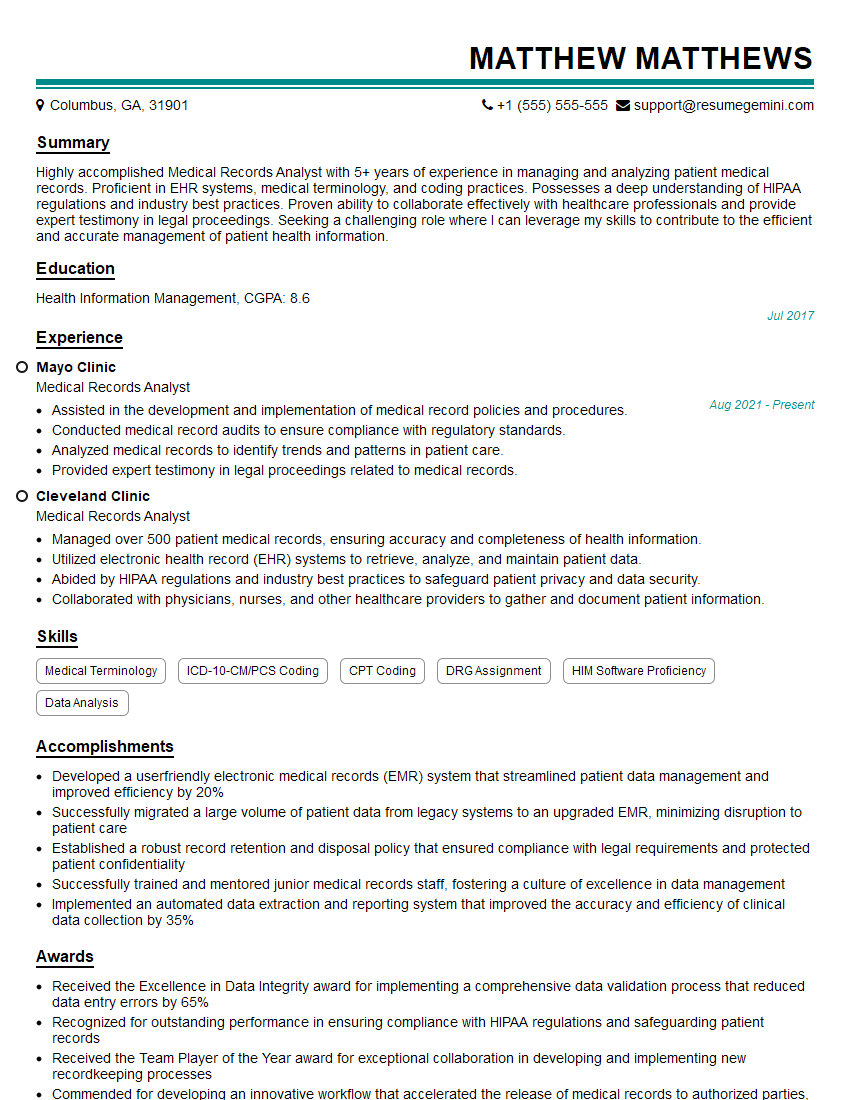
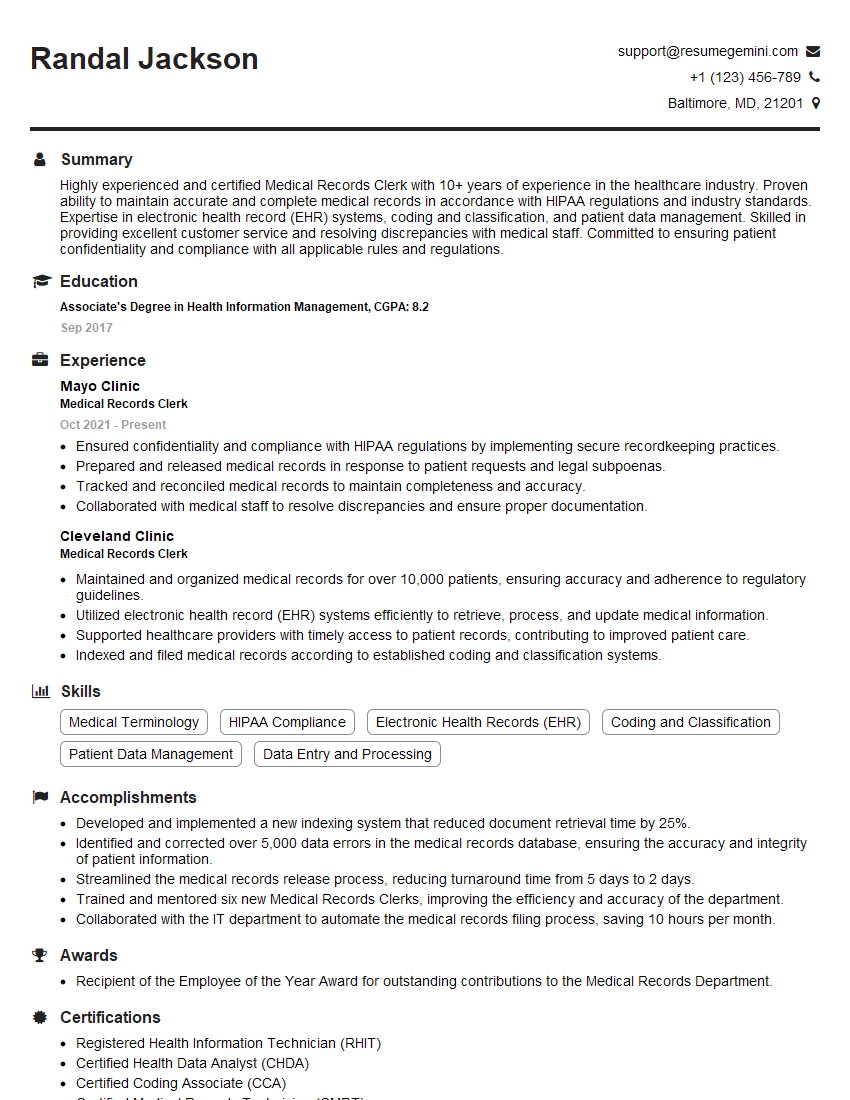
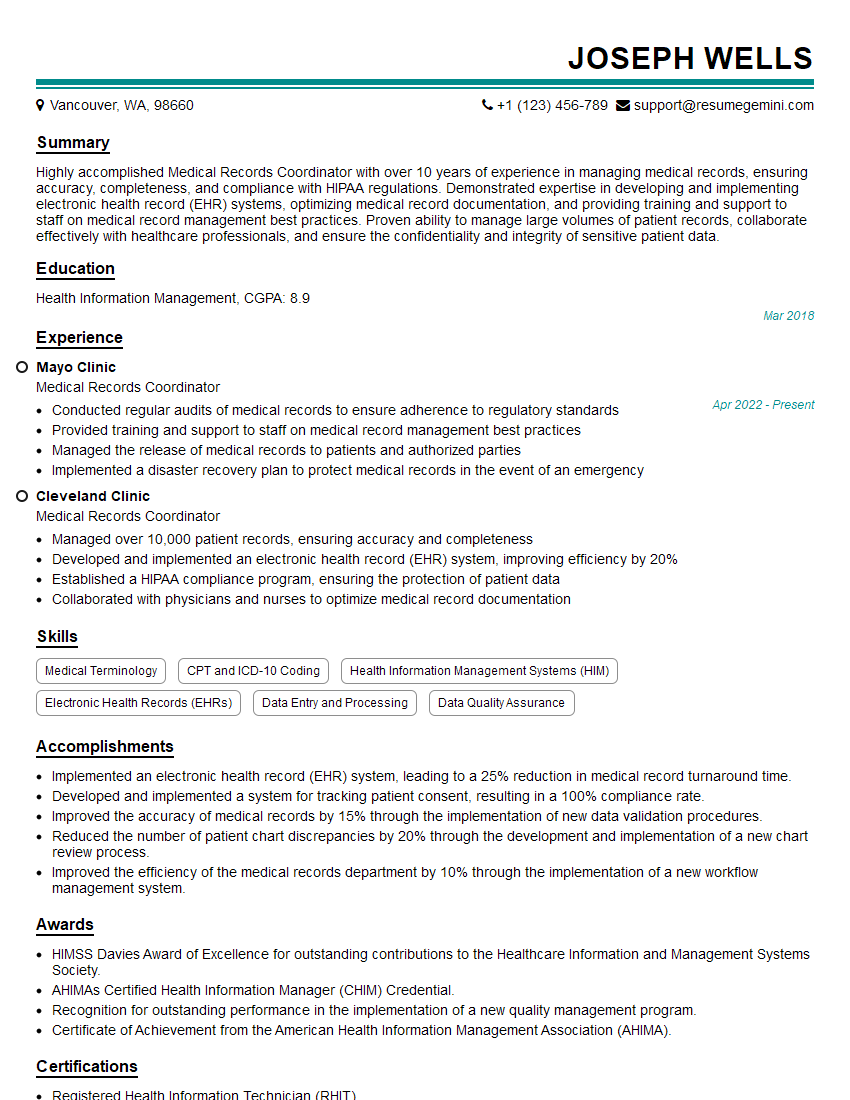
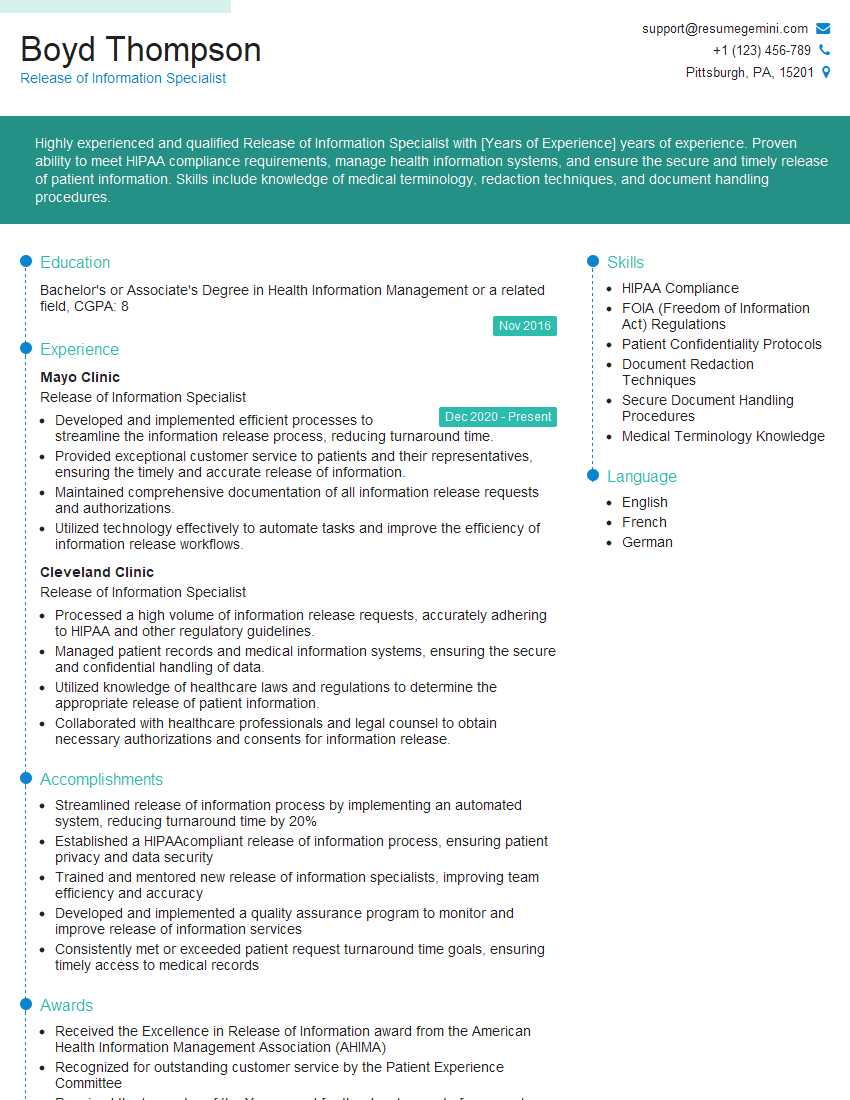
Mastering the art of preparing and maintaining medical records is crucial for a successful and rewarding career in healthcare. It demonstrates your attention to detail, your commitment to accuracy, and your understanding of vital legal and ethical considerations. To significantly boost your job prospects, crafting an ATS-friendly resume is essential. This ensures your qualifications are effectively highlighted to recruiters and applicant tracking systems. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Examples of resumes tailored to Prepare and Maintain Medical Records are available to guide you, making your job search more efficient and effective.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.