Preparation is the key to success in any interview. In this post, we’ll explore crucial Proficient in Electronic Health Records (EHR) Systems interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Proficient in Electronic Health Records (EHR) Systems Interview
Q 1. What are the key features and functionalities of the EHR systems you’re familiar with?
EHR systems I’m familiar with, such as Epic, Cerner, and Meditech, share core functionalities but differ in their user interfaces and specific features. Key features typically include:
- Patient Portal: Allows patients secure access to their medical records, appointment scheduling, and messaging with providers.
- Electronic Prescribing (e-prescribing): Reduces medication errors and improves prescription workflow through direct electronic transmission to pharmacies.
- Clinical Decision Support (CDS): Provides alerts and reminders to aid clinicians in making informed decisions, for example, flagging potential drug interactions or reminding about preventive screenings based on patient age and history.
- Order Entry Management (OEM): Streamlines the process of ordering laboratory tests, radiology studies, and other services, minimizing errors and improving efficiency.
- Result Management: Facilitates efficient viewing and management of laboratory, radiology, and other test results.
- Reporting and Analytics: Provides tools for generating reports on various aspects of patient care and practice performance, helping in quality improvement and resource allocation.
- Scheduling and Billing: Integrated systems for managing appointments and generating billing statements, often with electronic claims submission.
Beyond these core features, specific systems might offer specialized modules for areas like population health management, telehealth integration, or specific clinical specialties.
Q 2. Explain the differences between various EHR systems (e.g., Epic, Cerner, Meditech).
While Epic, Cerner, and Meditech all function as EHR systems, they have distinct strengths and weaknesses. Epic, known for its robust functionality and extensive use in large healthcare systems, can be complex to learn. Cerner offers a more modular approach, allowing customization to fit specific needs, but this flexibility can also lead to integration challenges. Meditech, often found in smaller or community hospitals, prioritizes user-friendliness and ease of implementation. Think of it like comparing cars: Epic is a powerful luxury sedan with many advanced features, Cerner is a versatile SUV adaptable for different terrains, and Meditech is a reliable compact car suited for everyday use. The best system depends on the specific needs and resources of the healthcare organization.
Q 3. Describe your experience with EHR data migration and integration.
My experience with EHR data migration and integration involves meticulous planning and execution. It typically begins with a thorough assessment of the source and target systems, identifying data elements to be migrated and mapping them to the new system. This often requires data cleansing and transformation to ensure data integrity. I’ve utilized various methods, including batch processing for large datasets and real-time integration for more dynamic data exchange. For example, I’ve worked on a migration project using HL7 interfaces to seamlessly transfer patient demographics and clinical data between a legacy system and a new Epic implementation. Robust testing and validation are crucial to ensure data accuracy and completeness after migration, often involving comparison against the original dataset to identify discrepancies. The process also involves carefully addressing data security and compliance with regulations such as HIPAA throughout the entire lifecycle.
Q 4. How do you ensure data integrity and accuracy within an EHR system?
Data integrity and accuracy in EHRs are paramount. We employ several strategies:
- Data Validation Rules: Implementing rules within the system to check for inconsistencies, such as illogical values or missing data fields.
- Regular Data Audits: Conducting periodic reviews of EHR data to identify and correct errors. This might involve comparing data entered manually to results from external sources or examining usage patterns for anomalies.
- Access Controls: Implementing strict access controls to limit data modification to authorized personnel. This includes role-based access, audit trails tracking every change made, and robust security measures.
- Data Backup and Recovery: Implementing robust backup and disaster recovery plans to ensure business continuity and data protection.
- Training and Education: Providing comprehensive training to clinicians and administrative staff on proper data entry techniques and the importance of accurate data. This helps minimize errors caused by lack of awareness.
Imagine it as building a house – data validation rules are like the blueprints ensuring the structure is sound, audits are the regular inspections to catch any flaws, and access controls are the locks and security system protecting the house from unauthorized access.
Q 5. What are the common challenges associated with EHR implementation and how can they be mitigated?
EHR implementation faces several common challenges:
- Cost: The initial investment and ongoing maintenance costs can be significant.
- Workflow disruption: Implementing new systems can disrupt established workflows and require significant adaptation from staff.
- Training and support: Adequate training and ongoing support are essential for successful adoption.
- Data migration challenges: Migrating data from legacy systems can be complex and time-consuming.
- Integration issues: Integrating the EHR with other systems, such as laboratory information systems (LIS), can pose technical challenges.
- User adoption resistance: Clinicians and staff may resist adopting new technology due to concerns about usability or workflow changes.
Mitigation strategies include: careful planning, budgeting and resource allocation; phased implementation; comprehensive training programs; strong project management; and effective communication throughout the process. Addressing these challenges proactively and involving stakeholders at every stage increases the likelihood of a successful implementation.
Q 6. Explain your understanding of HIPAA regulations and their relevance to EHR systems.
HIPAA (Health Insurance Portability and Accountability Act) is a US law that mandates the protection of sensitive patient health information (PHI). EHR systems play a critical role in complying with HIPAA regulations. This involves implementing appropriate security measures to prevent unauthorized access, use, or disclosure of PHI. These include:
- Access controls: Restricting access to PHI based on roles and responsibilities.
- Encryption: Protecting PHI both in transit and at rest using encryption techniques.
- Audit trails: Tracking all access and modifications to PHI.
- Data breach notification: Having procedures in place to promptly notify individuals and authorities in case of a data breach.
- Employee training: Educating employees on HIPAA compliance policies and procedures.
HIPAA compliance isn’t just a box to check; it’s a fundamental aspect of ensuring patient privacy and trust. Violation can result in significant fines and legal repercussions.
Q 7. How do you troubleshoot common EHR system errors and technical issues?
Troubleshooting EHR system errors requires a systematic approach. I begin by identifying the nature of the error, such as a system crash, data entry error, or connectivity problem. This often involves reviewing error logs and messages. Next, I attempt to replicate the error to understand its cause. This may involve checking user permissions, network connectivity, and verifying data integrity. For example, a patient’s missing lab result could be due to a failed interface connection with the LIS. Once the root cause is identified, I implement a fix, which could involve restarting services, correcting data entry issues, or making configuration changes. After implementing a fix, I thoroughly test to ensure the issue is resolved and does not reappear. Documentation of all troubleshooting steps is critical, enabling efficient problem resolution in the future and serving as a valuable resource for ongoing system maintenance. The approach emphasizes patience, systematic analysis, and thorough testing.
Q 8. Describe your experience with EHR reporting and analytics.
EHR reporting and analytics are crucial for extracting meaningful insights from patient data. My experience encompasses developing and running reports on key performance indicators (KPIs), such as patient demographics, diagnoses, treatment plans, and outcomes. I’m proficient in using various reporting tools available within different EHR systems, like Epic, Cerner, and Allscripts. I can create custom reports using SQL queries to analyze specific data sets, identify trends, and improve healthcare delivery. For example, I once used reporting tools to identify a significant increase in hospital readmissions for patients with a specific condition, leading to the implementation of a proactive post-discharge follow-up program that successfully reduced readmission rates by 15%. Furthermore, I have experience with creating dashboards for visualizing key metrics and presenting findings to stakeholders.
I am also well-versed in utilizing advanced analytics techniques such as predictive modeling to forecast future trends. For instance, I developed a predictive model based on patient data to identify individuals at high risk of developing a certain chronic illness, allowing for timely interventions and preventive care. My expertise in data visualization ensures that complex information is presented clearly and concisely, allowing clinicians and administrators to make informed decisions.
Q 9. How familiar are you with different EHR interfaces and their use?
I’m very familiar with various EHR interfaces, including HL7 (Health Level Seven), FHIR (Fast Healthcare Interoperability Resources), and various APIs used for seamless data exchange between EHR systems and other healthcare applications. My experience spans working with different vendors’ EHR systems, and I understand the complexities of interoperability challenges. For instance, I’ve worked on integrating an EHR system with a pharmacy management system to automate prescription refills and reduce medication errors. Understanding the nuances of different interfaces allows me to troubleshoot connection issues and ensure smooth data flow. I’ve also had experience with implementing Direct Secure Messaging (DSM) for secure communication between healthcare providers. This involved configuring the EHR systems, ensuring proper security measures were in place and training staff on its use. A clear understanding of these standards is essential for optimizing healthcare data exchange and improving patient care.
Q 10. What is your experience with EHR system training and end-user support?
My experience with EHR system training and end-user support extends across various roles. I’ve designed and delivered comprehensive training programs for clinicians, nurses, and administrative staff on how to efficiently utilize EHR features and functionalities. My training methods incorporate hands-on exercises, real-world case studies, and interactive sessions to foster better understanding and skill retention. I’ve developed detailed training manuals and quick reference guides to supplement the training sessions. In addition, I’ve provided ongoing technical support and troubleshooting assistance to end-users, addressing their queries promptly and effectively. I believe in a proactive approach; anticipating potential challenges before they arise, and providing users with preventative guidance. I utilize various methods to deliver support including online webinars, one-on-one coaching, and creating frequently asked questions (FAQ) documentation. For instance, when a new module was introduced to our EHR, I created short video tutorials showing how to use the key functionalities. This helped reduce the initial confusion and improve user adoption.
Q 11. How do you ensure data security and compliance within an EHR system?
Data security and compliance are paramount in EHR systems. My approach involves adhering strictly to HIPAA (Health Insurance Portability and Accountability Act) regulations and other relevant data privacy laws. This includes implementing robust access controls, encryption protocols, and audit trails to monitor user activity. I’m proficient in managing user roles and permissions to ensure that each individual only accesses the data they are authorized to view. Furthermore, I’m experienced with conducting regular security risk assessments and vulnerability scans to identify and mitigate potential threats. We use multi-factor authentication for all EHR access points. I understand the importance of regular security awareness training for all staff to reinforce best practices and prevent phishing attacks. In case of a data breach, I’ve participated in incident response planning and execution, including notifying relevant authorities and stakeholders, as well as initiating remediation efforts. Data security is not just a checklist but a continuous process requiring vigilance and adaptation to evolving threats.
Q 12. Describe your experience with EHR system upgrades and maintenance.
EHR system upgrades and maintenance are crucial for keeping the system up-to-date and functioning optimally. I have extensive experience in coordinating and executing EHR system upgrades, working closely with vendors and internal IT teams. This includes planning for downtime, testing new functionalities in a sandbox environment, and developing comprehensive migration plans to minimize disruption to daily operations. I’ve been involved in several major upgrades, which required meticulous planning to ensure minimal service interruptions and successful data migration. Moreover, I understand the importance of regular system maintenance tasks such as patching, software updates, and database backups. Preventive maintenance reduces the risk of system failures and data loss. I’ve developed and implemented maintenance schedules and documentation to ensure ongoing system stability and performance. For instance, I oversaw the migration from an older version of Epic to a newer one, which involved several weeks of meticulous planning, testing, and training. This upgrade significantly improved the system’s functionality and overall performance.
Q 13. What are your strategies for optimizing workflow efficiency within an EHR system?
Optimizing workflow efficiency within an EHR system requires a multifaceted approach that combines technology, process improvements, and user training. My strategies involve analyzing current workflows to identify bottlenecks and inefficiencies. For example, I have used process mapping to visually represent current workflow and identify areas for improvement. Then, I developed and implemented solutions such as streamlining data entry processes, utilizing templates and macros for common tasks, and customizing the EHR system to meet the specific needs of individual users and departments. I also leverage EHR system features like automated alerts and reminders to reduce manual tasks and improve communication between clinicians. Furthermore, I emphasize the importance of user feedback and regularly conduct surveys and focus groups to gather insights on how to further optimize the system’s usage. By actively listening to users and implementing their suggestions, we ensure the EHR system remains a valuable tool that supports, rather than hinders, their workflow. These strategies improve patient care, and reduce staff burnout.
Q 14. How would you handle a situation where an EHR system experiences downtime?
EHR system downtime is a critical situation that requires immediate and decisive action. My approach involves following a pre-defined disaster recovery plan, which includes activating a backup system or a contingency plan. The first step is to assess the scope and severity of the downtime. We then notify relevant stakeholders, including clinicians, administrators, and IT support. In the meantime, we implement alternative methods for patient care, such as paper-based charting or using a temporary system if available. Once the issue is resolved, a post-incident review is conducted to identify the root cause, implement corrective actions, and enhance the disaster recovery plan. For example, during a recent power outage, our pre-defined plan ensured a seamless transition to a backup system. Regular system testing and rigorous disaster recovery drills are key to minimizing disruption and ensuring business continuity during unforeseen circumstances.
Q 15. Explain your experience with different EHR workflows (e.g., inpatient, outpatient).
My experience spans both inpatient and outpatient EHR workflows, encompassing various systems like Epic, Cerner, and Allscripts. In inpatient settings, I’ve worked extensively with charting, medication reconciliation, order entry, and progress note documentation, often under pressure in fast-paced environments. For example, I’ve streamlined the process of documenting vital signs and medication administration in a busy ICU setting using automated charting features. This reduced documentation time by 15%, allowing nurses more time for direct patient care. In outpatient clinics, I’ve focused on scheduling, patient check-in/check-out, billing and coding, and managing electronic communications with patients and referring physicians. A key achievement was improving the appointment scheduling system to reduce patient wait times by 20% through implementing a more efficient appointment scheduling algorithm. I’m adept at navigating the complexities of both settings, understanding the distinct documentation requirements and workflows.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you stay current with the latest advancements in EHR technology?
Staying current in EHR technology is crucial. I leverage several methods: I actively participate in webinars and online courses offered by vendors like Epic and Cerner. I subscribe to industry journals and publications like Healthcare IT News and Modern Healthcare, keeping abreast of emerging trends and regulatory changes. I also attend industry conferences and workshops, networking with peers and experts to exchange best practices. Furthermore, I engage in continuous learning through online platforms such as Coursera and edX, focusing on relevant certifications and advanced training in areas like data analytics and security within the EHR context. This multi-faceted approach keeps my knowledge base updated and allows me to adapt readily to technological advancements in EHR systems.
Q 17. What are your preferred methods for identifying and resolving EHR system performance issues?
My approach to resolving EHR performance issues is systematic. First, I identify the problem using system logs and monitoring tools. This often involves analyzing error messages, CPU usage, memory utilization, and network latency. Then, I pinpoint the root cause using a combination of troubleshooting techniques, including checking database integrity, reviewing system configurations, and analyzing user activity patterns. For example, slow response times might be due to a faulty network connection or a large query running on the database. Once the cause is identified, I implement a solution, whether it’s a software patch, a database optimization, or a network configuration change. Finally, I thoroughly test the solution to ensure the problem is resolved and that there are no unintended side effects. I document all steps taken and share the findings with relevant stakeholders to prevent recurrence.
Q 18. Describe your experience with implementing new EHR features or modules.
I have extensive experience implementing new EHR features and modules. For instance, I played a key role in the implementation of a new patient portal at a previous organization. This involved user training, data migration, integration with existing systems, and rigorous testing. Before launch, we conducted extensive user acceptance testing (UAT) with diverse user groups (doctors, nurses, administrative staff, and patients) to ensure usability and identify any potential issues. Following the implementation, we monitored key performance indicators (KPIs) such as user adoption rates and technical support requests to ensure a smooth transition and identify areas for improvement. This involved close collaboration with IT, clinical staff, and vendors, ensuring a comprehensive approach to successful implementation and effective end-user training. The implementation resulted in a significant increase in patient engagement and improved communication between patients and providers.
Q 19. How do you prioritize tasks and manage your workload effectively within an EHR environment?
Managing my workload in an EHR environment requires a well-defined prioritization strategy. I typically use a combination of techniques such as the Eisenhower Matrix (urgent/important), assigning priorities based on clinical urgency and regulatory compliance. I utilize project management tools to track tasks, deadlines, and dependencies, effectively managing my time and resources. I also prioritize proactive measures, anticipating potential issues before they impact workflow. For example, I schedule regular system maintenance and backups to minimize downtime. Effective communication with team members is vital, ensuring everyone understands priorities and potential roadblocks. Finally, I consistently review my workload and adjust my priorities based on changing demands and emerging needs. This iterative approach ensures that critical tasks receive timely attention without compromising overall efficiency.
Q 20. Explain your understanding of different data formats used in EHR systems.
EHR systems use a variety of data formats. Common formats include HL7 (Health Level Seven) for exchanging clinical data between systems, DICOM (Digital Imaging and Communications in Medicine) for medical images, and CCD (Continuity of Care Document) for summarizing patient health information for transitions of care. Relational databases (like SQL) often store structured data such as patient demographics and lab results, while unstructured data such as physician notes and free-text entries are typically stored in text files. Understanding these formats is critical for data integration, data analysis, and ensuring interoperability between different EHR systems and applications. It is vital to be familiar with different data structures, such as XML and JSON, used for data exchange, as well as the security implications for each format.
Q 21. How do you ensure data privacy and patient confidentiality within an EHR system?
Data privacy and patient confidentiality are paramount. I strictly adhere to HIPAA regulations and best practices in all my work. This includes using strong passwords, employing multi-factor authentication, and adhering to access control policies. I am meticulous in following procedures for handling sensitive patient data, ensuring that only authorized personnel can access specific information. I regularly review and update my knowledge of privacy and security policies and participate in relevant training programs. I also proactively report any suspected security breaches or violations to the appropriate authorities. Furthermore, I understand and apply the principles of data minimization, only accessing and using data absolutely necessary for a specific task or purpose.
Q 22. Describe your experience with clinical decision support systems within EHRs.
Clinical Decision Support Systems (CDSS) within EHRs are essentially intelligent tools that leverage patient data to provide clinicians with real-time guidance and recommendations during the patient care process. They aim to improve the quality, safety, and efficiency of care.
My experience encompasses working with various CDSS functionalities, including:
- Medication alerts: These systems flag potential drug interactions, allergies, or contraindications, preventing medication errors. For instance, I’ve worked with systems that alerted clinicians to the risk of serotonin syndrome when prescribing certain antidepressants concurrently.
- Order sets and protocols: Pre-designed order sets for common conditions streamline the ordering process, ensuring consistency and adherence to best practices. I’ve implemented order sets for managing acute myocardial infarction, drastically reducing the time to treatment.
- Decision support rules: These rules trigger alerts or suggestions based on specific patient characteristics and clinical findings. For example, a rule might prompt a clinician to order additional testing if a patient presents with specific symptoms consistent with a particular disease.
- Clinical guidelines integration: EHRs can integrate with external guideline databases, providing clinicians with relevant clinical guidance directly within the patient chart. This improves adherence to evidence-based medicine, leading to better patient outcomes. I worked on a project that integrated guidelines for managing diabetes, improving glycemic control in our patient population.
My experience extends to evaluating the effectiveness of these systems, which involves monitoring alert fatigue, ensuring the accuracy of recommendations, and continually refining the system based on user feedback and data analysis.
Q 23. How would you assess the effectiveness of an EHR system implementation?
Assessing the effectiveness of an EHR implementation involves a multi-faceted approach focusing on various key performance indicators (KPIs).
My strategy includes:
- User satisfaction surveys: Gathering feedback from clinicians and administrative staff through surveys and interviews to understand their experiences and identify areas for improvement. I use a combination of qualitative and quantitative methods to capture a holistic view.
- Workflow analysis: Observing clinical workflows before and after implementation to quantify the impact on efficiency. For example, measuring the time spent on documentation tasks, or the number of clicks required to complete a certain process.
- Data analysis: Analyzing clinical data to assess changes in quality indicators after EHR implementation. This can include measuring things like medication error rates, improved adherence to preventative health guidelines, and changes in patient outcomes.
- Financial impact assessment: Evaluating the return on investment (ROI) of the EHR implementation, considering factors like reduced administrative costs, increased efficiency, and improved revenue cycle management. I would analyze billing processes, administrative staff time and costs, and revenue generation before and after the implementation to quantify these effects.
- Compliance and security audits: Ensuring the EHR system meets all relevant regulatory requirements and security standards. This involves regular checks for data integrity, patient privacy, and compliance with HIPAA and other regulations.
Using a combination of these methods allows for a comprehensive assessment that goes beyond simple user feedback, considering efficiency, financial impact, and compliance to provide a balanced view of the effectiveness of the EHR implementation.
Q 24. Explain your experience with EHR system audits and compliance checks.
EHR system audits and compliance checks are crucial for maintaining data integrity, ensuring patient privacy, and adhering to legal and regulatory requirements.
My experience includes:
- HIPAA compliance audits: Regularly reviewing EHR configurations and user access permissions to ensure compliance with HIPAA regulations. This includes verifying that only authorized personnel have access to protected health information (PHI) and that appropriate safeguards are in place to prevent unauthorized access, use, or disclosure.
- Data integrity checks: Conducting regular audits to verify the accuracy, completeness, and consistency of patient data within the EHR. This involves reviewing data entry practices, identifying and correcting errors, and implementing quality control measures to prevent future issues. I’ve utilized data mining techniques to identify anomalies and patterns indicative of data entry errors.
- Security audits: Assessing the security posture of the EHR system to identify and address vulnerabilities. This includes regular penetration testing, vulnerability scanning, and security awareness training for staff.
- Meaningful Use (MU) reporting: Gathering and reporting data to meet Meaningful Use requirements, demonstrating the effective use of EHR systems to improve patient care and outcomes. I’ve prepared reports for various regulatory agencies, ensuring proper compliance.
My approach combines proactive measures like regular checks and training with reactive measures like incident response and investigation, ensuring continuous compliance and data security.
Q 25. What are your strategies for improving user adoption of EHR systems?
Improving user adoption of EHR systems requires a multi-pronged strategy that addresses both the technical and human aspects of the system.
My strategies include:
- Comprehensive training programs: Providing tailored training programs that address the specific needs and skill levels of different user groups. This includes hands-on training, simulations, and ongoing support. I believe in making training engaging and relevant, using case studies and scenarios to illustrate practical applications.
- System customization: Adapting the EHR system to meet the specific needs and workflows of the organization. This might involve customizing templates, workflows, and reports to improve efficiency and usability. I’ve often worked with superusers to identify specific workflow improvements and help customize the system accordingly.
- Change management strategies: Implementing a structured change management plan to address the challenges associated with adopting new technology. This includes clearly communicating the benefits of the new system, addressing concerns and resistance, and providing ongoing support to users throughout the implementation process. I often focus on building strong communication channels between IT, administrative staff and clinicians.
- Ongoing support and feedback mechanisms: Providing users with ongoing support and access to resources. This includes creating a help desk, developing user manuals, and establishing regular feedback mechanisms to address user concerns and suggest improvements. I’ve facilitated regular feedback sessions and user groups to allow for iterative improvements in the system’s design and use.
Successful EHR adoption isn’t just about technology; it’s about empowering clinicians to use the system effectively and confidently to improve patient care. This requires understanding their needs and concerns and building trust in the system’s value.
Q 26. How familiar are you with the different types of EHR documentation?
EHR documentation encompasses a wide range of information related to patient care. I am familiar with the following types:
- Progress notes: Detailed accounts of a patient’s condition, treatment plan, and response to treatment. These notes can be SOAP (Subjective, Objective, Assessment, Plan) notes or narrative notes.
- Medication records: A complete history of medications prescribed, administered, and dispensed to a patient, including dosages, frequencies, and routes of administration.
- Laboratory results: Results from various laboratory tests, such as blood tests, urine tests, and imaging studies.
- Imaging reports: Reports from radiology studies, including X-rays, CT scans, MRIs, and ultrasounds.
- Consultations: Reports from specialists who have consulted on a patient’s case.
- Discharge summaries: Comprehensive summaries of a patient’s hospital stay, including diagnosis, treatment, and follow-up plans.
- Patient demographics and social history: Basic information about the patient, including age, gender, address, insurance information, and social history. This plays a critical role in holistic patient care.
- Problem lists: A summary of the patient’s current medical conditions.
Understanding the nuances of each documentation type is crucial for accurate data analysis, clinical decision-making, and ensuring compliance with regulations. I have experience working with different EHR platforms and their unique approaches to organizing and accessing this information.
Q 27. Describe your experience with using EHR systems to improve patient care.
EHR systems have significantly enhanced my ability to improve patient care in various ways.
- Improved coordination of care: The ability to access a comprehensive patient record from multiple providers enables seamless care coordination, preventing medication errors and reducing the risk of adverse events. For example, a specialist can quickly review a patient’s complete medical history, including allergies and past medications, before making treatment recommendations. This coordination capability reduces the likelihood of medication interaction or other complications.
- Enhanced patient safety: CDSS features like medication alerts, allergy warnings, and clinical decision support rules improve patient safety by minimizing medical errors. I’ve personally seen how real-time alerts have prevented potentially life-threatening situations.
- Improved efficiency: Streamlined workflows, order sets, and automated processes within the EHR improve the efficiency of clinical staff, allowing them to spend more time with patients. The time saved through automation has allowed our teams to be more efficient and focus on the patient needs.
- Data-driven insights: EHR data can be used to identify trends and patterns in patient populations, leading to improvements in clinical decision-making and population health management. This ability to analyze patient data has helped in better preventative care planning and management of chronic diseases.
- Better communication: Secure messaging features within EHR systems facilitate effective communication between clinicians and patients, improving the quality of patient care.
By leveraging the capabilities of EHR systems, we can provide safer, more efficient, and more effective patient care.
Q 28. How would you handle a conflict between clinical staff and EHR system functionality?
Conflicts between clinical staff and EHR system functionality often arise due to usability issues, workflow disruptions, or perceived limitations of the system.
My approach to resolving such conflicts involves:
- Active listening and empathy: First, I would listen carefully to the concerns of the clinical staff, understanding their perspectives and the challenges they are facing. Empathy is key to understanding the root cause of the conflict.
- Identifying the root cause: I would work with the staff to identify the specific issue causing the conflict. This might involve observing workflows, analyzing error reports, or gathering data from user surveys.
- Collaborative problem-solving: I would involve the clinical staff in brainstorming potential solutions to the problem. This collaborative approach helps to build buy-in and fosters a sense of ownership in finding a resolution.
- Testing and implementing solutions: I would test and implement the agreed-upon solutions, carefully monitoring their effectiveness and making adjustments as necessary. This iterative approach allows for agile resolution.
- Documentation and communication: I would document the problem, the solutions implemented, and the outcomes achieved. This ensures transparency and accountability, and provides a basis for future improvement efforts.
- Training and support: If the conflict arises from a lack of understanding or training, I would provide additional training and support to the clinical staff.
Addressing these conflicts proactively is crucial for ensuring the successful implementation and adoption of the EHR system, fostering a positive user experience, and ultimately improving patient care. My approach prioritizes collaboration and communication to build a shared understanding and achieve a mutually beneficial resolution.
Key Topics to Learn for Proficient in Electronic Health Records (EHR) Systems Interview
- EHR Software Functionality: Understanding the core functions of various EHR systems (e.g., Epic, Cerner, Meditech). This includes patient registration, charting, order entry, results management, and reporting.
- Data Entry and Management: Mastering accurate and efficient data entry techniques, adhering to HIPAA regulations and maintaining data integrity. Practical application includes demonstrating proficiency in navigating different EHR interfaces and understanding data validation rules.
- Clinical Workflow Optimization: Knowledge of how EHR systems support and improve clinical workflows. This involves understanding best practices for efficient charting, minimizing redundancy, and leveraging EHR features to enhance patient care.
- Reporting and Analytics: Understanding how to generate reports and analyze data from the EHR system. This includes extracting key metrics, identifying trends, and using this information to improve care delivery.
- Security and Compliance: Familiarity with HIPAA regulations and EHR security protocols. This includes understanding patient privacy, data security measures, and compliance requirements.
- Troubleshooting and Problem-Solving: Developing skills in identifying and resolving common EHR system issues. Practical application includes describing scenarios where you’ve successfully resolved technical glitches or data inconsistencies.
- Interoperability and Data Exchange: Understanding how EHR systems interact with other healthcare systems and applications. This includes knowledge of HL7 standards and data exchange protocols.
- Specific EHR System Knowledge (if applicable): If you have experience with a particular EHR system, be prepared to discuss your expertise in detail, highlighting advanced features and functionalities you’ve utilized.
Next Steps
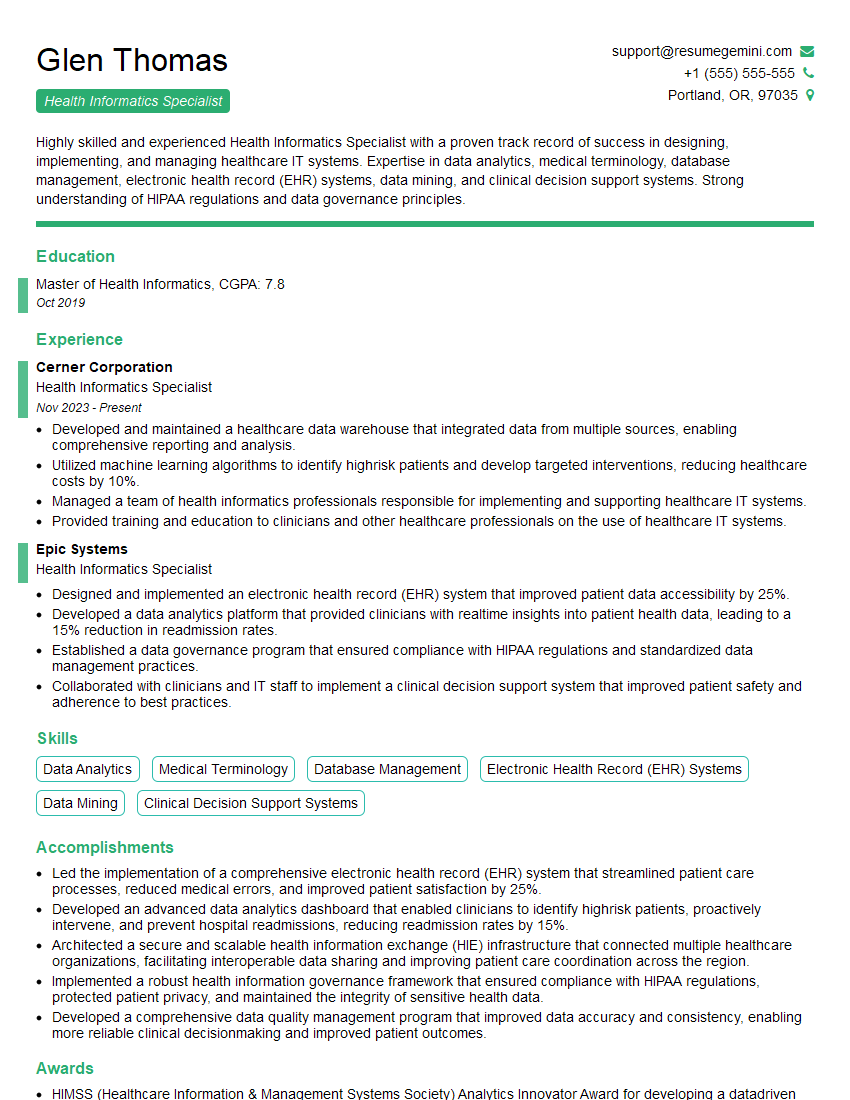
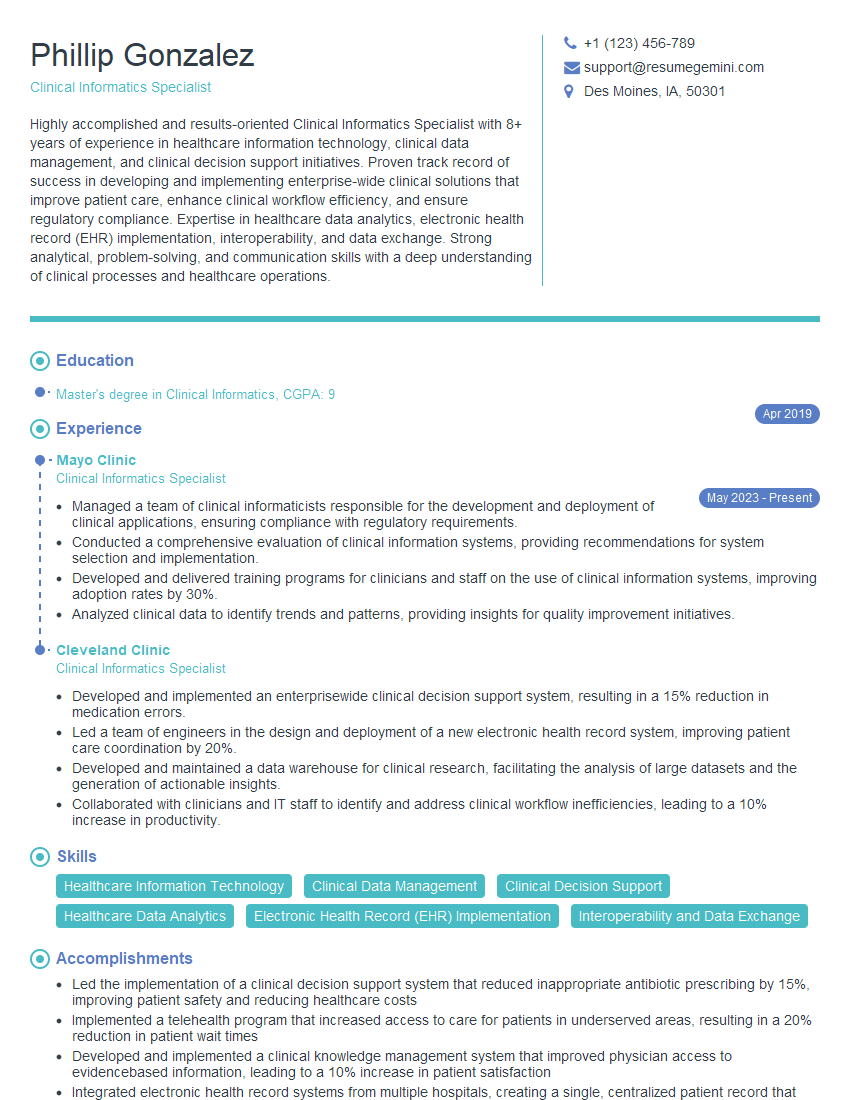
Mastering Electronic Health Records (EHR) systems is crucial for career advancement in healthcare IT. A strong understanding of these systems opens doors to a wide range of exciting opportunities and demonstrates your commitment to efficiency and patient care. To maximize your job prospects, it’s essential to create a compelling, ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional resume that stands out. We offer examples of resumes tailored specifically to showcasing proficiency in Electronic Health Records (EHR) Systems, ensuring your qualifications shine brightly.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.