The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Progress Note Writing interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Progress Note Writing Interview
Q 1. What are the key components of a well-written progress note?
A well-written progress note is the cornerstone of effective patient care and legal protection. It’s a concise yet comprehensive record of a patient’s encounter, detailing their condition, treatment, and response. Key components include:
- Subjective (S): This section captures the patient’s own description of their symptoms, concerns, and feelings. For example, “Patient reports persistent headaches for the past week, rated 7/10 on pain scale.”
- Objective (O): This section contains measurable and verifiable data obtained during the examination. Examples include vital signs (blood pressure, heart rate), physical exam findings (e.g., “Lungs clear to auscultation”), and lab results.
- Assessment (A): This is your interpretation of the subjective and objective data, including your diagnosis or working diagnosis. For example: “Suspected migraine headache based on patient history and physical exam.”
- Plan (P): This outlines your treatment plan, including medications, tests, referrals, and follow-up appointments. For instance: “Prescribed sumatriptan 100mg for headache relief. Scheduled follow-up appointment in one week.”
- Date and Time: Crucial for maintaining a chronological record.
- Provider Signature and Credentials: Ensures accountability and verification.
Think of it like a detective’s case file: you gather information (S & O), analyze it (A), and create a strategy (P) to resolve the case (patient’s health issue).
Q 2. Explain the difference between SOAP and CHEDDAR charting methods.
SOAP and CHEDDAR are both structured charting methods, but they differ in their organization and emphasis. SOAP (Subjective, Objective, Assessment, Plan) focuses on a problem-oriented approach, ideal for episodic visits or addressing specific issues. CHEDDAR (Chief Complaint, History, Examination, Details, Drugs, Assessment, Return visit), on the other hand, provides a more comprehensive narrative, often used for detailed initial evaluations.
SOAP is straightforward and concise, perfect for routine visits where a specific issue is the focus. Imagine a patient with a cough; a SOAP note would focus on the cough, examining relevant aspects like its onset, character, associated symptoms, and the treatment plan.
CHEDDAR, with its inclusion of ‘Details’ and emphasis on comprehensive history, is better suited for more complex cases requiring a detailed overview. For instance, a new patient visit would benefit from CHEDDAR’s structured approach, providing a complete medical history, physical exam, and treatment plan.
In essence, SOAP is like a quick snapshot, while CHEDDAR is a detailed portrait.
Q 3. How do you ensure accuracy and completeness in progress note documentation?
Accuracy and completeness are paramount in progress note documentation. To ensure this, I employ several strategies:
- Diligent Data Collection: I meticulously gather information from the patient, review lab results, imaging reports, and other relevant sources.
- Careful Observation and Examination: Thorough physical examination and assessment are crucial to ensure accurate objective findings.
- Clear and Concise Language: I avoid ambiguity and use precise medical terminology. Using standardized terms minimizes misinterpretations.
- Verification and Double-Checking: I verify all information before documenting, especially medication names and dosages.
- Timely Documentation: I record notes immediately after each patient encounter to minimize memory lapses and ensure accuracy.
- Template Utilization (within reason): Using EHR templates can enhance consistency but must be customized to accurately reflect each individual patient’s unique condition. Over-reliance on templates can lead to inaccurate or generic documentation.
Consider this: a seemingly minor inaccuracy, such as a wrong medication dose, could have serious consequences. A systematic approach ensures the highest standard of accuracy and completeness.
Q 4. Describe your experience with different EHR systems and their impact on progress note writing.
I have extensive experience with various EHR systems, including Epic, Cerner, and Athenahealth. Each system has its strengths and weaknesses in terms of progress note writing.
Epic, for example, is known for its robust functionalities, but its complexity can sometimes be a challenge for less tech-savvy users. Cerner often has a user-friendly interface but might lack certain features. Athenahealth often prioritizes ease of use but might lack the breadth of capabilities present in larger systems.
The impact on progress note writing varies. Some systems offer excellent templates and auto-suggestions, speeding up documentation. However, the dependence on templates can occasionally lead to generic notes that lack the specificity needed for individual patients. Efficient navigation and proficiency in using various functionalities of the system are key to effectively leverage its features and improve the quality of note writing. I adapt my approach to each system to maximize efficiency while ensuring complete and accurate documentation.
Q 5. How do you handle conflicting information from different sources when documenting a patient’s progress?
Handling conflicting information requires a systematic approach. I prioritize evidence-based medicine and documented findings. If information from different sources is contradictory, I would:
- Review all sources carefully: Identify the source of each piece of information, looking for potential biases or errors.
- Gather additional data if needed: Conduct further investigations to resolve the discrepancies, potentially ordering additional tests or consultations.
- Document all findings transparently: Note the conflicting information and how it was resolved (or if resolution was not possible).
- Use professional judgment: Based on my clinical experience and the available evidence, I would make a clinical judgment regarding the most accurate and reliable information.
For example, if a patient reports chest pain but the ECG is normal, I would document both findings, mention the lack of objective correlation, and possibly suggest further investigations like cardiac enzyme testing. Transparency is key to avoid misinterpretations.
Q 6. What are the legal and ethical considerations when writing progress notes?
Legal and ethical considerations are paramount in progress note writing. The notes serve as a legal record and must be accurate, objective, and complete. Key considerations include:
- Accuracy and Completeness: Omitting relevant information or recording inaccurate data can have legal ramifications.
- Objectivity: Personal opinions or biases should be avoided. Focus on factual observations and measurable data.
- Confidentiality: Protecting patient privacy is critical. Notes must comply with HIPAA regulations (in the US) and other relevant laws.
- Legibility: Illegible notes can be misinterpreted or even lost. Using clear, concise language and legible handwriting (or typing) is essential.
- Amendments: If corrections are necessary, they should be made properly by adding a line through the mistake, adding the correction, and signing and dating it. Never erase or obliterate information.
Failure to adhere to these principles can lead to malpractice lawsuits, disciplinary actions, and damage to professional reputation.
Q 7. How do you ensure patient confidentiality while documenting patient progress?
Patient confidentiality is a cornerstone of medical ethics. I ensure confidentiality by following these measures:
- Adhering to HIPAA regulations (or equivalent laws): Strictly following all guidelines related to patient data access, storage, and disclosure.
- Using secure electronic systems: Utilizing password-protected EHR systems, secure messaging, and other technologies to protect patient information.
- Limiting access to records: Ensuring that only authorized personnel have access to patient records.
- Proper disposal of paper records: Shredding or securely destroying any paper records that are no longer needed.
- Using appropriate language: Avoiding informal language or slang in written notes.
- Understanding and complying with the institution’s confidentiality policies: This includes being aware of any specific protocols or procedures related to data security and privacy.
Imagine the devastating consequences of a data breach – loss of trust, potential legal action, and significant emotional distress for the patient. Protecting confidentiality is not just a legal obligation but a moral imperative.
Q 8. Explain your understanding of HIPAA regulations as they relate to progress note writing.
HIPAA (Health Insurance Portability and Accountability Act) regulations are crucial for maintaining patient privacy and security in healthcare. When it comes to progress notes, HIPAA dictates that all protected health information (PHI) must be kept confidential. This includes names, addresses, dates of birth, medical record numbers, and any information that could reasonably identify a patient. My understanding encompasses several key areas:
- Confidentiality: Progress notes are strictly confidential and only accessible to authorized personnel involved in the patient’s care. Access controls, such as passwords and user permissions, are essential. I always ensure I am accessing only the records I need for the specific patient I’m working with.
- Security: Progress notes, whether electronic or paper-based, must be stored securely to prevent unauthorized access or disclosure. This involves following secure electronic health record (EHR) practices, using strong passwords, and properly disposing of paper records.
- Disclosure: PHI can only be disclosed with the patient’s consent or under specific exceptions allowed by HIPAA, such as for treatment, payment, or healthcare operations. For example, I would need authorization before releasing information to an insurance company or a family member who isn’t directly involved in the patient’s care.
- Breach Notification: In the event of a data breach involving PHI, I am aware of the notification procedures required by HIPAA and would immediately report it to the appropriate authorities.
In practice, I always adhere to my organization’s HIPAA compliance policies and undergo regular training to stay updated on any changes to the regulations. Understanding HIPAA is paramount; a single breach can have serious legal and ethical consequences.
Q 9. How do you use medical terminology and abbreviations correctly in progress notes?
Accurate and consistent use of medical terminology and abbreviations is vital for clear and concise progress notes. Using the wrong term can lead to misinterpretations, delays in treatment, and potentially harm the patient. My approach involves:
- Using approved terminology: I always refer to standardized medical dictionaries and terminologies like SNOMED CT and LOINC. These resources ensure the use of consistent and unambiguous terms.
- Avoiding ambiguous abbreviations: I avoid using abbreviations that are not universally understood or could be misinterpreted. For instance, instead of using ‘u’ for units, I would write ‘units’ in full to avoid confusion with ‘µ’ (micro).
- Contextual clarity: Even when using standard abbreviations, I ensure the context makes the meaning crystal clear. If an abbreviation might be unclear, I spell it out the first time it appears in a note.
- Regular updates: Medical terminology and abbreviations evolve, so I stay up-to-date by attending conferences, reading medical journals, and consulting my organization’s guidelines.
For example, instead of writing 'Pt c/o HA', which could be interpreted in several ways, I would write 'Patient complains of headache'. This ensures unambiguous communication.
Q 10. Describe your process for reviewing and correcting errors in progress notes.
Error correction in progress notes requires meticulous attention to detail and strict adherence to institutional guidelines. My process involves:
- Immediate Correction: If I notice an error while documenting, I correct it immediately. In electronic health records, systems often allow for adding an addendum, which shows the correction, the date and time of the correction, and my initials.
- Documentation of Corrections: I never erase or obliterate errors. Any corrections must be clearly documented, ideally with a short explanation as to the reason for the correction. This maintains the integrity and audit trail of the medical record.
- Signature and Date: All corrections must be dated and signed or initialed electronically to show accountability.
- Escalation: If I am unsure how to correct a significant error, I consult with a supervisor or another qualified healthcare professional for guidance.
Think of it like a legal document; accuracy is paramount. A clearly documented correction shows responsible practice and transparency, crucial for protecting the patient and healthcare providers.
Q 11. How do you handle urgent or critical situations that require immediate documentation?
Urgent or critical situations demand immediate documentation to ensure continuity of care and effective communication among the healthcare team. My approach prioritizes speed and accuracy:
- Immediate Entry: I make sure to document the critical information as soon as the situation allows. Even if it’s a brief note, it provides a baseline record.
- Use of Templates: In some EHR systems, emergency or critical care templates are available to expedite documentation, reducing the time spent on typing while focusing on the most critical details.
- Voice Recognition: Some systems offer voice recognition software, allowing me to dictate notes rapidly, especially during emergencies.
- Follow-up Documentation: After the immediate crisis has subsided, I complete a more comprehensive record, expanding on the initial notes and ensuring all information is captured accurately.
For example, during a cardiac arrest, my initial note might simply state, 'Cardiac arrest noted at 14:30. CPR initiated. Emergency team notified.'. Later, a more detailed account of the events and interventions can be added.
Q 12. How do you prioritize your tasks when managing a high volume of progress notes?
Managing a high volume of progress notes requires a structured and efficient approach. My strategies include:
- Prioritization: I prioritize notes based on urgency (e.g., critical care patients first), then by deadlines (e.g., notes required for billing), and finally, by workflow (e.g., completing notes for a specific physician first to streamline their workflow).
- Time Blocking: I allocate specific time blocks during my day dedicated solely to progress note writing. This helps me focus and avoids interruptions.
- Batch Processing: I often group similar notes together (e.g., notes for patients seen in the same clinic) to improve efficiency.
- Use of EHR Tools: Utilizing the EHR’s features, such as templates, auto-completion, and copy-paste functions where appropriate and compliant, can drastically reduce time spent on repetitive tasks.
Imagine a painter; they don’t paint one brush stroke at a time across multiple canvases. They group similar colors or sections, working on each efficiently. The same principles apply to efficient progress note writing.
Q 13. Describe your experience with clinical documentation improvement (CDI) initiatives.
Clinical Documentation Improvement (CDI) initiatives focus on improving the accuracy and completeness of medical records. My experience includes:
- Chart Reviews: I have participated in chart reviews, identifying areas where documentation is incomplete, unclear, or inconsistent with the patient’s medical condition.
- Querying Clinicians: I have experience in querying physicians and other healthcare providers to clarify information and obtain necessary details to enhance the overall quality of documentation.
- Education and Training: I have participated in CDI education and training programs, improving my understanding of documentation standards and best practices.
- Data Analysis: I’ve been involved in analyzing documentation data to identify trends, issues, and areas for improvement within the healthcare organization.
CDI is not about finding fault; it’s about collaborative work to ensure the medical record accurately reflects the patient’s care and supports appropriate reimbursement. It’s about teamwork and improvement.
Q 14. What is your experience with auditing progress notes for compliance?
Auditing progress notes for compliance ensures that documentation meets regulatory requirements and internal standards. My experience in this area involves:
- Reviewing for Completeness: I ensure all essential elements are present, such as patient identifiers, dates, times, diagnoses, procedures, and treatment plans.
- Checking for Accuracy: I verify the information against other medical records and sources to ensure accuracy and consistency.
- Assessing for Clarity: I check if the language is clear, concise, and avoids ambiguities. Unclear documentation can have serious consequences.
- Compliance with Regulations: I assess compliance with HIPAA, coding guidelines, and other relevant regulations. This involves checking for the proper use of medical terminology and adherence to documentation policies.
Think of an auditor checking financial records; the same principles of accuracy, completeness, and compliance apply to auditing medical records. The goal is to ensure the integrity and reliability of the information within those records.
Q 15. How do you ensure the readability and understandability of your progress notes?
Readability and understandability in progress notes are paramount for effective communication and continuity of care. I achieve this through several key strategies:
- Clear and Concise Language: I avoid medical jargon whenever possible, opting for plain language that anyone with a basic understanding of healthcare could comprehend. For instance, instead of ‘tachycardia,’ I might write ‘rapid heart rate.’
- Structured Formatting: I use headings and bullet points to organize information logically. This makes it easy to quickly scan the note and find specific details. For example, using separate sections for ‘Subjective,’ ‘Objective,’ ‘Assessment,’ and ‘Plan’ (SOAP) helps to clarify the information.
- Grammatically Correct Sentences: This might seem obvious, but proper grammar and spelling are essential for professionalism and clear communication. I always proofread my notes before finalizing them.
- Use of Abbreviations (with Caution): While abbreviations can save time, I use them sparingly and only when their meaning is universally understood within the context of the medical record. I avoid using abbreviations that are not standard.
Imagine a nurse reviewing my notes – they need to be able to understand the patient’s condition and care plan quickly and without ambiguity. My goal is to write notes as if I am explaining the patient’s situation to a colleague in a clear, concise and comprehensive manner.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How familiar are you with different types of progress notes (e.g., admission note, discharge summary)?
I am very familiar with various types of progress notes. Each serves a specific purpose and has a slightly different format:
- Admission Note: This comprehensive note documents the reason for admission, presenting illness, patient history, current medications, allergies, physical exam findings, and initial treatment plan. It serves as the foundation for the patient’s entire hospital stay.
- Discharge Summary: A concise summary of the patient’s hospital course, including diagnosis, treatment received, response to treatment, and instructions for post-discharge care. It’s crucial for continuity of care after discharge.
- Operative Note: Details the surgical procedure performed, including the indication, technique, complications, and findings. This note is critical for legal and medical record keeping.
- Progress Notes (daily or as needed): These notes document the patient’s ongoing progress, changes in condition, responses to treatment, and any significant events. They provide a chronological account of the patient’s stay.
- Consultation Notes: These record the findings and recommendations of a specialist who has been consulted on a particular patient.
Understanding these different formats is essential for writing accurate and complete medical documentation tailored to the specific situation.
Q 17. Describe your process for documenting subjective and objective findings.
Documenting subjective and objective findings is a cornerstone of accurate progress note writing. I use the SOAP (Subjective, Objective, Assessment, Plan) method:
- Subjective (S): This section captures information reported by the patient, such as their chief complaint, pain levels, symptoms (e.g., nausea, dizziness), and feelings. I record these using direct quotes whenever possible. Example: “Patient reports severe abdominal pain rated 8/10.”
- Objective (O): This section focuses on measurable and observable data obtained during the physical examination, laboratory tests, and imaging studies. Example: “Temperature 101°F, heart rate 110 bpm, blood pressure 140/90 mmHg. Abdomen tender to palpation in the right lower quadrant.”
Separating subjective and objective information is crucial. Subjective information represents the patient’s perspective, while objective information provides verifiable evidence. The assessment and plan then build upon these foundations.
Q 18. How do you effectively communicate complex medical information in progress notes?
Communicating complex medical information requires clear, structured writing and a focus on the audience. I employ these strategies:
- Layman’s Terms Where Appropriate: I avoid overly technical jargon, and explain complex concepts using simple language and analogies when appropriate. For example, instead of ‘metabolic acidosis,’ I might explain the concept of the body’s acid-base balance being disrupted.
- Use of Tables and Charts: For complex data sets, such as lab results or medication lists, I utilize tables to improve readability and comprehension.
- Step-by-Step Explanation: For procedures or treatments, I provide step-by-step explanations, ensuring the process is easy to follow.
- Logical Flow: I present information in a logical order, starting with the most important details and then proceeding to more specific information.
By focusing on simplicity and clear structure, even the most complex information becomes much more accessible to others who may need to read my notes, including other healthcare professionals.
Q 19. What strategies do you use to improve the efficiency of your progress note writing?
Improving efficiency in progress note writing involves leveraging technology and optimizing my workflow:
- Electronic Health Records (EHR) Software: I utilize EHR software’s features effectively, including templating, copy-and-paste functions (used judiciously to avoid redundancy), and auto-completion to reduce repetitive tasks.
- Voice-to-Text Software: Using voice-to-text tools can significantly speed up the writing process, though I always meticulously review and edit the output for accuracy.
- Structured Data Entry: I use structured data entry fields whenever possible, which allows for efficient data capture and reduces the need for free-text entry.
- Templates: I develop templates for common situations (e.g., post-operative notes) to streamline the writing process. This reduces writing time and minimizes the risk of omission.
Efficient documentation allows me more time to focus on patient care rather than administrative tasks. This balance is key.
Q 20. How do you stay updated on changes in medical terminology, coding, and documentation guidelines?
Staying current in medical terminology, coding, and documentation guidelines is crucial for accurate and compliant progress notes. I utilize various methods:
- Professional Organizations: I actively engage with professional organizations like the American Medical Association (AMA) and subscribe to their publications and updates.
- Continuing Medical Education (CME): Regular CME courses cover updates to coding guidelines, documentation standards, and new medical terminology.
- Online Resources: I regularly consult reputable online resources and medical journals for updates in my field. Keeping abreast of changes to coding practices, particularly, is vital for accurate billing and reimbursement.
- Internal Training Programs: I participate in internal training programs offered by my healthcare facility to stay updated on institutional policies and procedures regarding documentation.
Continuous learning is a vital part of maintaining my professional competency and ensuring the quality of my progress notes.
Q 21. How do you handle situations where a physician’s dictation is unclear or incomplete?
When a physician’s dictation is unclear or incomplete, I take proactive steps to ensure accuracy and completeness:
- Clarification with the Physician: I politely contact the physician to clarify any ambiguities or missing information. This direct communication helps prevent errors and ensures the note reflects the intended content.
- Review of Other Documentation: If clarification is not immediately possible, I review other documentation, such as lab results or imaging reports, to infer the missing information. This must be documented carefully and transparently.
- Documentation of the Ambiguity: If the ambiguity cannot be resolved, I clearly document the unclear parts of the dictation in the progress note, indicating my attempts to clarify the information. This provides a record of the situation and limits potential liability.
- Following Institutional Guidelines: I adhere to the institutional policies and procedures for handling incomplete or unclear dictation.
Accuracy and transparency are paramount. Addressing unclear dictation promptly minimizes the risk of misinterpretations and ensures the integrity of the patient’s medical record.
Q 22. What is your experience with using templates in progress note writing?
Templates are indispensable tools for efficient progress note writing. They provide a structured format, ensuring consistency and completeness. I’ve extensively used templates tailored to different specialties and patient populations. For instance, I use one template for routine follow-ups that includes sections for chief complaint, review of systems, medication reconciliation, and a plan. Another template is designed for new patient visits, which incorporates a more comprehensive history taking section. These templates are not rigid; they allow for customization based on individual patient needs while maintaining a standardized format that improves legibility and reduces the risk of omitting crucial information.
The benefits of using templates include reduced time spent on note creation, improved accuracy due to predefined sections, and enhanced consistency across documentation. Imagine trying to remember all the necessary sections each time you write a note – a template eliminates that cognitive load. It allows me to focus on the clinical details rather than the structural elements of the note.
Q 23. How do you manage your time effectively when writing progress notes for multiple patients?
Managing time effectively when documenting for multiple patients requires a strategic approach. I prioritize tasks using a combination of techniques. Firstly, I batch similar tasks – for instance, I’ll complete all my progress notes for a particular clinic session before moving onto other responsibilities. Secondly, I utilize time-blocking, allocating specific time slots for charting. Thirdly, I leverage technology to my advantage, using voice recognition software (more on this in a later response) to significantly speed up the writing process. Finally, I strive for efficiency in my examination and patient interactions; a well-structured clinical encounter minimizes the time needed for documentation.
For example, if I have appointments scheduled back-to-back, I’ll use a quick note-taking method during the encounter, using abbreviations and key phrases, to efficiently record the patient information. Once the patient has left, I quickly input the detailed notes using my voice recognition software, and the pre-filled template structure ensures that I don’t miss any essential information. This flow ensures I’m not falling behind and maintains an efficient workflow.
Q 24. How do you integrate relevant diagnostic test results and other clinical data into your progress notes?
Integrating diagnostic test results and other clinical data seamlessly into progress notes is crucial for comprehensive patient care. I employ a structured approach. I first ensure the results are readily accessible through the electronic health record (EHR). Then, I systematically review the relevant data, summarizing key findings in a clear and concise manner within the progress note. For example, if a patient has had blood work done, I won’t simply state ‘blood work reviewed.’ Instead, I’ll mention specific values, such as ‘Hemoglobin 10.5 g/dL, indicating anemia,’ and correlate these findings with the patient’s clinical presentation. I avoid simply copying and pasting large chunks of lab data, focusing instead on the clinically relevant information and its interpretation.
This ensures the note remains focused on the patient’s clinical picture, making it easily readable and understandable for others. I often use tables or bulleted lists to organize extensive data efficiently, enhancing clarity and readability. This method ensures that the diagnostic information is not only included but also actively contextualized within the overall assessment and management plan.
Q 25. Describe your experience using a voice recognition system for progress note documentation.
I have extensive experience using voice recognition systems for progress note documentation. It has drastically reduced my charting time and improved efficiency. I find that the accuracy is high, especially after training the system with my specific vocabulary and phrasing patterns. Initially, there was a learning curve in adapting my speech patterns, but it becomes second nature with practice. The system helps to minimize transcription errors and allows for hands-free documentation, especially helpful during busy clinic hours.
However, I am mindful of its limitations. Complex medical terminology or unusual phrasing sometimes needs editing, and I always thoroughly review and edit the generated text before finalizing the note to maintain accuracy. It’s a valuable tool that enhances workflow when coupled with careful post-transcription review. It’s not a complete replacement for manual charting; it’s a powerful tool that streamlines a part of the documentation process.
Q 26. How do you ensure the integration of progress notes with other aspects of the patient’s medical record?
Seamless integration of progress notes with other aspects of the patient’s medical record is paramount for continuity of care. The EHR facilitates this by linking the progress note to other relevant documents such as prior notes, medication lists, imaging reports, and consultation summaries. I always ensure that my progress note clearly references any relevant prior findings and incorporates updates in light of new information. For instance, if a patient’s blood pressure has been consistently high, I would reference previous notes and correlate them with the current findings.
This integrated approach prevents duplication of efforts and ensures that the patient’s entire clinical history is readily accessible to all healthcare providers involved in their care. It creates a comprehensive and coherent narrative of the patient’s medical journey, making it easy for others to understand the patient’s current status and plan of care. It also helps in identifying trends and patterns in the patient’s health over time.
Q 27. What is your understanding of the importance of proper grammar and punctuation in progress notes?
Proper grammar and punctuation are essential in progress notes for clarity, accuracy, and legal defensibility. Poor grammar can lead to misinterpretations that may have serious consequences for patient care. Imagine a note that reads, ‘Patient complaining of chest pains, treated and sent home.’ Without proper punctuation, it’s unclear whether the patient was actually treated and sent home or was simply diagnosed and awaiting further treatment.
Therefore, I prioritize clear and concise writing, adhering to grammatical rules and using correct punctuation to ensure the note’s meaning is unambiguous. I double-check my writing for any errors, and the structure imposed by the templates ensures the information flows logically. Legible and well-structured notes reflect professionalism and minimize the risk of miscommunication or legal issues.
Q 28. Describe your problem-solving approach when encountering challenges during progress note writing.
My problem-solving approach when encountering challenges during progress note writing is systematic and multi-faceted. If I’m struggling to articulate a complex clinical picture, I might break it down into smaller, more manageable components. I might consult clinical guidelines, textbooks, or even colleagues for clarification on diagnostic or treatment approaches. If I’m unsure about the best way to phrase something to ensure clarity, I’ll strive for simplicity and plain language, avoiding jargon wherever possible.
If I’m facing technical issues with the EHR system, I utilize the help desk or troubleshoot the issue using established problem-solving methods. If I’m short on time, I prioritize the most critical information and focus on completing the essential sections of the note, then return to add further details when time permits. My goal is always to produce a complete, accurate, and concise record of the patient encounter, even when facing challenges. Effective problem-solving is a crucial skill for efficient and safe progress note documentation.
Key Topics to Learn for Progress Note Writing Interview
- SOAP Note Structure: Understanding and applying the subjective, objective, assessment, and plan format for clear and concise documentation.
- Legal and Ethical Considerations: Mastering the principles of confidentiality, accuracy, and compliance with HIPAA regulations in progress note writing.
- Medical Terminology and Abbreviations: Demonstrating proficiency in using accurate and standardized medical terminology and abbreviations.
- Progress Note Content and Flow: Creating a logical and chronological narrative that effectively communicates patient progress and treatment plans. This includes understanding what information is relevant and what should be omitted.
- Problem-Solving and Critical Thinking: Applying critical thinking skills to analyze patient data and create accurate and insightful progress notes that support clinical decision-making.
- Different Note Types: Familiarity with various note types (e.g., initial, progress, discharge) and their specific requirements.
- Electronic Health Records (EHR) Systems: Practical experience with common EHR systems and their impact on progress note writing efficiency and accuracy.
- Chart Auditing and Review: Understanding the importance of regular chart audits and their role in maintaining quality documentation and identifying areas for improvement.
Next Steps
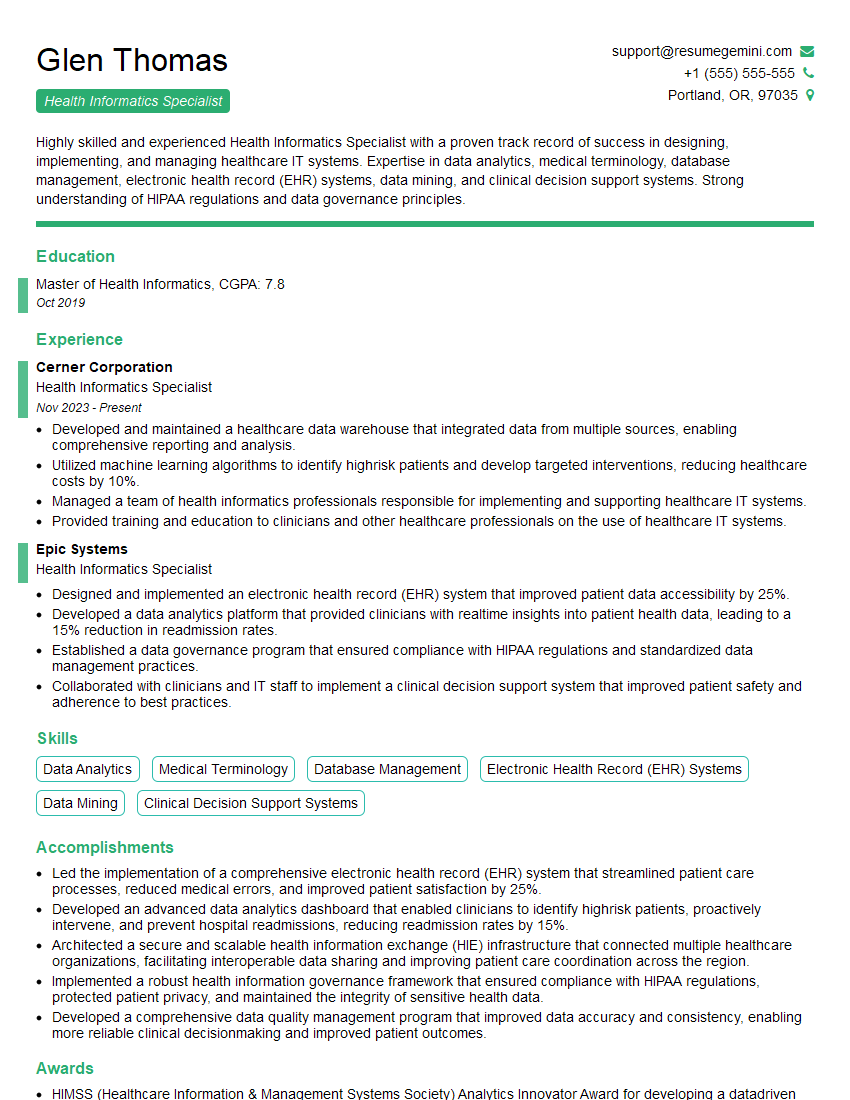
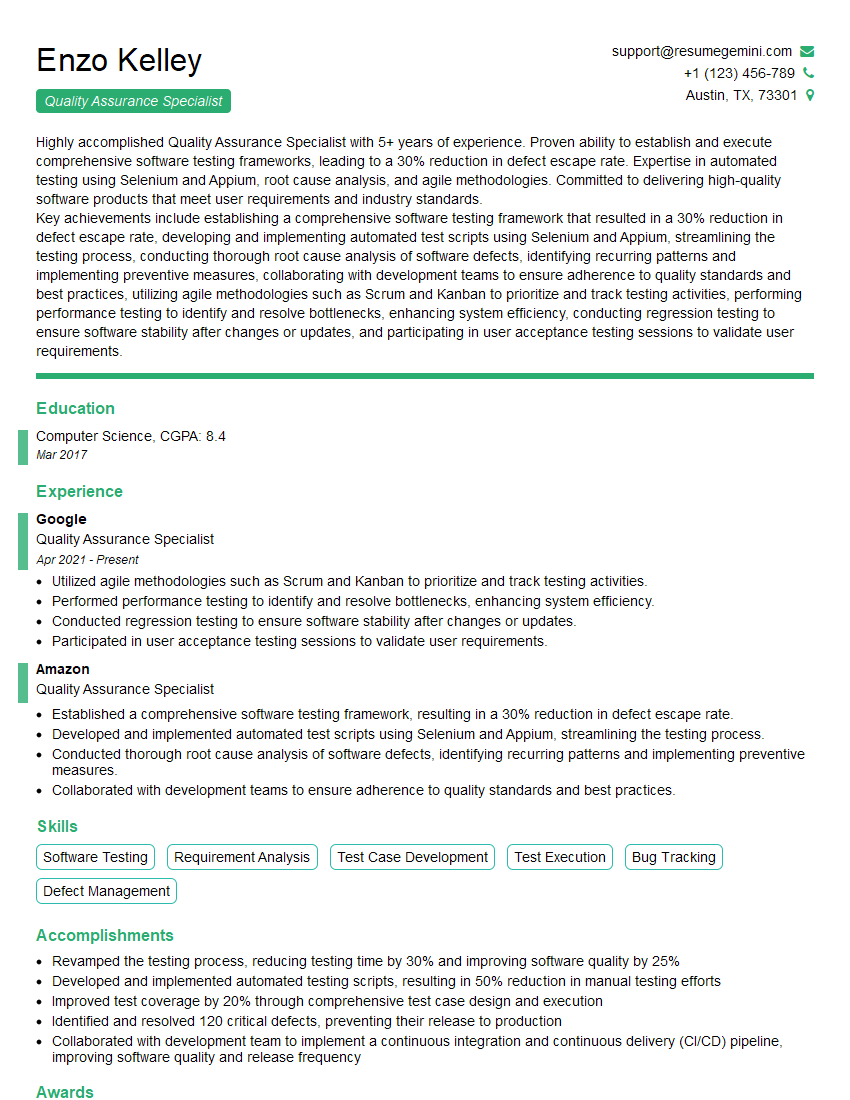
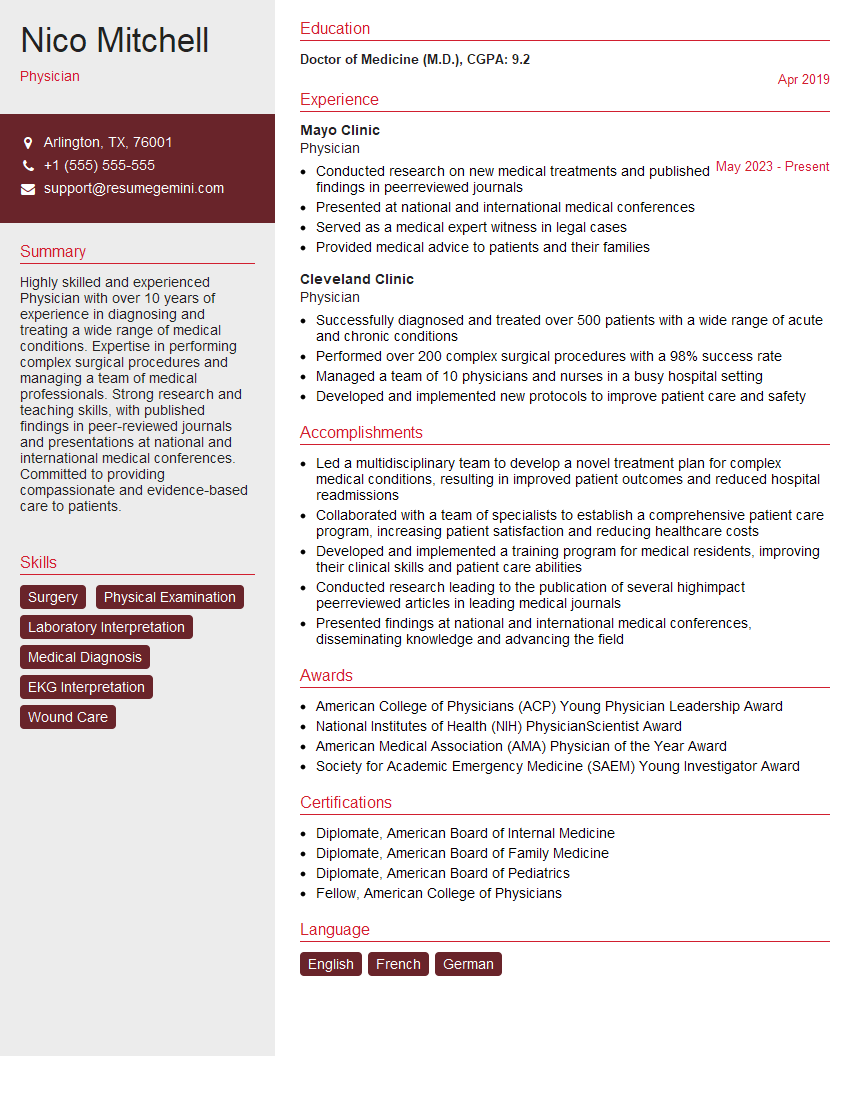
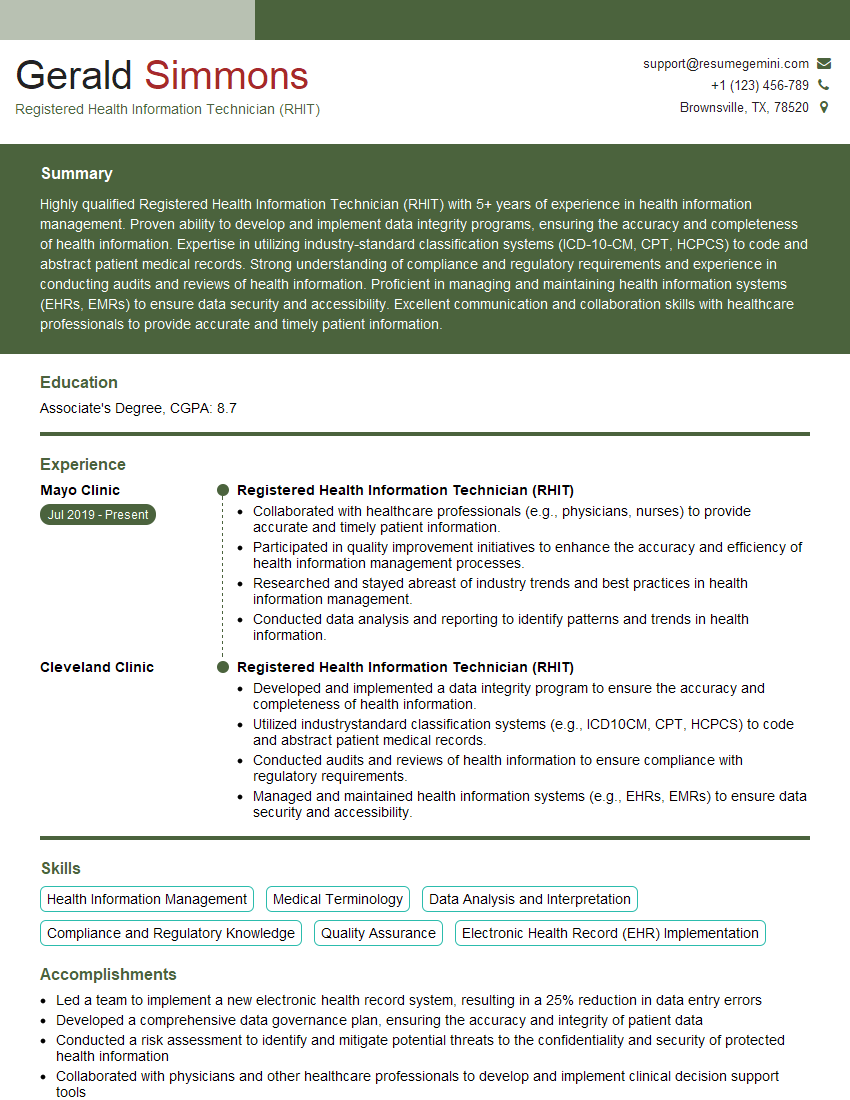
Mastering progress note writing is crucial for career advancement in healthcare, demonstrating your professionalism and clinical skills. A well-crafted resume is your first impression – make it count! Build an ATS-friendly resume to maximize your chances of landing your dream job. ResumeGemini is a trusted resource that can help you create a compelling and effective resume. We provide examples of resumes tailored to Progress Note Writing to give you a head start. Invest time in refining your resume; it’s the key that unlocks your next opportunity.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.