Preparation is the key to success in any interview. In this post, we’ll explore crucial Psoriatic Arthritis Treatment interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Psoriatic Arthritis Treatment Interview
Q 1. Explain the diagnostic criteria for Psoriatic Arthritis.
Diagnosing Psoriatic Arthritis (PsA) can be challenging because its symptoms overlap with other conditions. There isn’t one single definitive test, but rather a combination of clinical findings and exclusion of other diseases. The Classification Criteria for Psoriatic Arthritis (CASPAR) are widely used. These criteria consider several factors, giving points for each:
- History of psoriasis: This includes skin psoriasis, nail changes (pitting, discoloration, onycholysis), or a family history of psoriasis.
- Arthritis affecting specific areas: PsA often involves the distal interphalangeal (DIP) joints of the fingers and toes (the joints closest to the fingertips and toenails), which is less common in other arthritides.
- Asymmetrical joint involvement: Unlike Rheumatoid Arthritis (RA), PsA often affects joints on only one side of the body.
- Dactylitis (sausage digits): Inflammation of the entire finger or toe, giving it a swollen “sausage-like” appearance.
- Radiographic evidence of PsA: X-rays can show characteristic bone erosions and joint damage specific to PsA.
A high score on the CASPAR criteria, along with clinical presentation, helps make a diagnosis. It’s crucial to remember that early diagnosis is key for effective management, so any suspicion warrants thorough investigation.
Q 2. Describe the pathogenesis of Psoriatic Arthritis.
The exact pathogenesis of PsA is complex and still under investigation, but it’s understood to be an autoimmune disease, meaning the body’s immune system mistakenly attacks its own tissues. Genetic predisposition plays a significant role, with specific genes linked to both psoriasis and PsA. An environmental trigger, like an infection, may activate the immune system in genetically susceptible individuals.
The immune response involves the activation of T cells (a type of white blood cell) and cytokines (signaling proteins). These contribute to inflammation in the skin and joints. There is evidence suggesting an interplay between skin and joint inflammation, meaning skin involvement can precede or even influence the development of arthritis. The chronic inflammation leads to cartilage and bone damage over time.
Q 3. What are the common clinical manifestations of Psoriatic Arthritis?
PsA presents diversely, making diagnosis challenging. Symptoms can vary significantly between patients. Common clinical manifestations include:
- Arthritis: Joint pain, swelling, stiffness, and limited range of motion. The affected joints can vary greatly but commonly involve the hands, feet, and spine.
- Psoriasis: This is the hallmark feature, characterized by raised, red, scaly plaques on the skin, commonly on the elbows, knees, scalp, and lower back. Nail changes are common such as pitting, thickening, discoloration, or separation from the nail bed (onycholysis).
- Dactylitis: Inflammation of the entire finger or toe, resulting in sausage-like swelling.
- Enthesitis: Inflammation where tendons and ligaments attach to bone (entheseal points). This can cause pain in the heels, lower back, and other areas.
- Spondylitis: Inflammation of the spine, which can cause back pain, stiffness, and limited spinal mobility.
- Uveitis: Inflammation of the eye, causing redness, pain, and blurred vision.
The combination and severity of these symptoms can vary considerably from person to person.
Q 4. Differentiate between Psoriatic Arthritis and Rheumatoid Arthritis.
While both PsA and RA are autoimmune diseases causing chronic arthritis, there are key differences:
- Presence of Psoriasis: PsA is always associated with psoriasis, either on the skin, nails, or both. RA does not have this association.
- Joint Involvement: PsA often affects the DIP joints of the hands and feet, whereas RA primarily targets the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints. PsA’s joint involvement is often asymmetric (affecting different joints on each side of the body), while RA is usually symmetric.
- Systemic Symptoms: While systemic symptoms are possible in both, RA tends to be more commonly associated with severe fatigue, fever, and overall malaise compared to PsA.
- Specific Imaging Findings: Radiographic findings differ between the two, with PsA showing characteristic erosions and bony changes that differ from those seen in RA.
In practice, a rheumatologist considers these factors, along with blood tests (such as rheumatoid factor and anti-citrullinated peptide antibodies, which are more frequently positive in RA) to differentiate between the two.
Q 5. Outline the initial treatment approach for Psoriatic Arthritis.
The initial treatment approach for PsA focuses on controlling both the arthritis and the psoriasis. This often involves a multi-faceted strategy. It starts with assessing the severity of the disease and the individual’s needs. Early and aggressive treatment is crucial to prevent joint damage and improve long-term outcomes.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These are often used for pain and inflammation relief. They are not disease-modifying; they help manage symptoms but don’t prevent joint damage.
- Corticosteroids: These potent anti-inflammatory medications can provide rapid relief, but long-term use carries significant side effects. Usually, they are used for short periods or localized injection into inflamed joints.
- Disease-Modifying Antirheumatic Drugs (DMARDs): As explained further below, these medications are crucial in slowing the progression of joint damage. The choice depends on factors like comorbid conditions and patient preferences.
- Topical and systemic treatments for psoriasis: Managing the psoriasis is important, and treatment options include topical creams, phototherapy, and systemic medications such as biologics or methotrexate.
A rheumatologist will carefully consider the patient’s individual circumstances and disease severity to create a tailored treatment plan.
Q 6. Discuss the role of NSAIDs in Psoriatic Arthritis management.
NSAIDs play an important role in managing the symptoms of PsA, particularly pain and inflammation. They reduce prostaglandin production, substances that mediate inflammation. Common NSAIDs used include ibuprofen, naproxen, and diclofenac. These can provide significant relief, especially in the early stages or during acute flares.
However, it’s crucial to understand that NSAIDs are not disease-modifying; they only treat the symptoms. They do not prevent the underlying joint damage that occurs with PsA. Long-term use can also lead to gastrointestinal problems, such as ulcers and bleeding, necessitating careful monitoring and potential use of protective medications (like proton pump inhibitors).
NSAIDs are often part of the initial treatment strategy, but they are usually complemented by disease-modifying treatments to prevent long-term joint damage and disability.
Q 7. Explain the use of DMARDs (Disease-Modifying Antirheumatic Drugs) in Psoriatic Arthritis.
DMARDs are cornerstone treatments in PsA because they slow the progression of joint damage, unlike NSAIDs. They are started early in the disease process for the greatest impact. There are several categories of DMARDs used, including:
- Conventional DMARDs (cDMARDs): These include methotrexate, sulfasalazine, and leflunomide. They work by suppressing the immune system, reducing inflammation, and slowing joint destruction. These medications often take several weeks to months to show their full effect.
- Biologic DMARDs: These are targeted therapies that act on specific parts of the immune system involved in the pathogenesis of PsA. Examples include TNF inhibitors (adalimumab, etanercept, infliximab), IL-17 inhibitors (secukinumab, ixekizumab), and IL-23 inhibitors (ustekinumab). Biologics can be very effective, but they are more expensive and can have a higher risk of side effects. Careful monitoring for infections and other adverse events is crucial.
The choice of DMARD depends on various factors including the severity of the disease, the presence of other conditions, previous treatment responses, and individual patient factors. A rheumatologist will carefully weigh the risks and benefits to determine the optimal DMARD regimen for each patient.
Q 8. Describe the mechanism of action of TNF inhibitors in Psoriatic Arthritis.
Tumor Necrosis Factor (TNF) inhibitors are a cornerstone of Psoriatic Arthritis (PsA) treatment. Their mechanism of action centers around blocking TNF-alpha, a pro-inflammatory cytokine that plays a significant role in the inflammation and joint damage characteristic of PsA. Think of TNF-alpha as a key that unlocks inflammation. TNF inhibitors act like a lock-picking device, preventing this key from initiating the inflammatory cascade.
Specifically, these biologics bind to TNF-alpha, preventing it from binding to its receptors on immune cells. This blockage reduces the production of other inflammatory mediators, resulting in decreased inflammation and ultimately, improved symptoms such as pain, swelling, and stiffness. Different TNF inhibitors, such as adalimumab, etanercept, and infliximab, vary slightly in their structure and method of binding, but the fundamental mechanism remains the same.
Q 9. What are the common side effects associated with biologic therapies for Psoriatic Arthritis?
Biologic therapies, while highly effective, can have side effects. These vary depending on the specific medication but commonly include:
- Increased risk of infections: Because biologics suppress the immune system, patients are more susceptible to infections like colds, flu, and more serious bacterial, fungal, or viral infections.
- Injection site reactions: Pain, redness, or swelling at the injection site are common with injectable biologics.
- Infusion reactions: For infusion medications, reactions like fever, chills, or nausea can occur during or after the infusion.
- Increased risk of certain cancers: Some studies have shown a slightly increased risk of certain cancers, particularly lymphoma, although this risk is generally low.
- Heart failure: Some biologics can impact the heart, and a history of heart failure is a factor to be carefully evaluated before initiating therapy.
- Neurological effects: Rarely, demyelinating events (such as multiple sclerosis) have been linked to certain biologics.
It’s crucial to discuss potential side effects with your physician before starting any biologic therapy, and regular monitoring is essential to detect and manage any issues promptly.
Q 10. How do you monitor the response to treatment in Psoriatic Arthritis?
Monitoring response to PsA treatment involves a multi-faceted approach. We use a combination of objective and subjective measures:
- Disease Activity Scores: Standardized scores like the Disease Activity Score 28 (DAS28) or the Clinical Disease Activity Index (CDAI) quantify disease severity based on factors such as tender and swollen joint counts, erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) levels, and patient-reported pain scores. These provide objective data tracking improvement.
- Patient-reported outcomes (PROs): This includes detailed assessment of pain levels, functional abilities using questionnaires, fatigue, and other symptoms related to PsA. Patient feedback is critical in evaluating the effectiveness of treatment.
- Imaging studies: X-rays and ultrasound can assess for joint damage and inflammation over time, providing crucial information about the disease’s impact on joints.
- Laboratory tests: Regular blood tests, such as complete blood count (CBC), inflammatory markers (ESR, CRP), and liver function tests (LFTs), are essential to monitor for potential side effects and assess overall health.
By combining these assessments, we obtain a comprehensive view of the patient’s response to therapy, allowing for timely adjustments as needed.
Q 11. What are the indications for referral to a specialist in Psoriatic Arthritis?
Referral to a rheumatologist, a specialist in inflammatory arthritis, is indicated when:
- Diagnosis is uncertain: PsA can mimic other conditions, and a specialist is best equipped to make an accurate diagnosis.
- Disease is severe or unresponsive to initial treatment: If symptoms are uncontrolled despite initial therapy with NSAIDs or DMARDs, referral for more advanced treatment options is crucial.
- Significant joint damage or disability is present: PsA can cause substantial joint damage, and early specialist intervention can help prevent long-term disability.
- Significant comorbidities exist: Patients with coexisting conditions like diabetes, heart disease, or kidney disease will require multidisciplinary care management.
- Patient preference or complex disease course: Some patients might feel more comfortable navigating the challenges of managing PsA with a specialist.
Early referral can lead to better treatment outcomes and reduce long-term disability.
Q 12. Discuss the importance of patient education in managing Psoriatic Arthritis.
Patient education is absolutely paramount in managing PsA. Empowered patients are better equipped to actively participate in their care, leading to better outcomes and improved quality of life. Effective education should cover:
- Disease understanding: Patients need to understand what PsA is, its progression, and its impact on their body.
- Treatment options: Patients should be fully informed about their treatment plan, including the benefits, risks, and side effects of each medication.
- Lifestyle modifications: The importance of regular exercise, a healthy diet, stress management techniques, and smoking cessation should be emphasized.
- Self-management strategies: Patients should learn how to monitor their symptoms, recognize potential flares, and adjust their activities accordingly.
- Disease monitoring: Patients should learn how to understand and report their Disease Activity Scores to healthcare professionals.
- Support resources: Information about support groups and other resources can help patients connect with others facing similar challenges.
Using clear language, visual aids, and interactive sessions improves patient comprehension and encourages adherence to the treatment plan.
Q 13. How do you address patient concerns regarding the long-term effects of Psoriatic Arthritis medications?
Addressing patient concerns regarding long-term effects is crucial. Many patients worry about the potential side effects of long-term medication use, particularly with biologics. I address these concerns by:
- Openly discussing potential risks: I provide balanced information on both the benefits and risks of medication, emphasizing that the risks are often outweighed by the benefits in preventing disease progression.
- Individualized risk assessment: I discuss the patient’s specific risk factors and personalize the assessment of potential side effects. For example, patients with a history of heart failure will require more careful monitoring.
- Regular monitoring: I emphasize the importance of regular follow-up visits and laboratory tests to detect and manage potential side effects early.
- Patient empowerment: I encourage patients to actively participate in their care, empowering them to voice their concerns and ask questions.
- Alternative treatment strategies: In some cases, we may explore alternative treatment strategies or consider medication tapering or cessation if appropriate.
By fostering a strong doctor-patient relationship built on trust and open communication, I aim to address patient concerns and improve their confidence in their treatment plan.
Q 14. Describe the role of physical therapy in Psoriatic Arthritis management.
Physical therapy plays a vital role in PsA management, focusing on improving function, reducing pain, and preventing joint damage. A tailored program typically includes:
- Range of motion exercises: Gentle exercises help maintain joint flexibility and prevent stiffness.
- Strengthening exercises: Strengthening exercises improve muscle strength and support around affected joints, enhancing stability and reducing pain.
- Low-impact aerobic exercises: Activities like swimming, cycling, or walking can improve cardiovascular health and overall fitness without putting excessive stress on joints.
- Joint protection techniques: Learning techniques to minimize joint stress during daily activities helps reduce pain and prevent further damage.
- Adaptive equipment: Using assistive devices like splints, canes, or adaptive kitchen utensils can make daily tasks easier and safer.
- Education and self-management: Physical therapists educate patients on proper posture, body mechanics, and self-management strategies to improve their independence.
Physical therapy should be integrated into the overall management plan, working in conjunction with medication and other treatments for optimal outcomes.
Q 15. What are the psychosocial implications of Psoriatic Arthritis?
Psoriatic arthritis (PsA) significantly impacts patients’ psychosocial well-being. The chronic pain, inflammation, and joint deformities can lead to significant limitations in daily activities, impacting work, social life, and overall quality of life. Think of someone who used to enjoy gardening; PsA might make simple tasks like bending over extremely painful, leading to isolation and frustration.
- Depression and Anxiety: The constant physical discomfort and limitations can trigger depression and anxiety. Many patients struggle with feelings of hopelessness and helplessness.
- Reduced Social Participation: Pain and fatigue can make it difficult to participate in social events and maintain relationships, leading to social isolation.
- Body Image Issues: Joint deformities and skin lesions associated with psoriasis can negatively affect body image and self-esteem.
- Financial Strain: The costs associated with medical care, medication, and lost work can create significant financial burdens, further adding to stress.
Comprehensive management of PsA should consider these psychosocial factors. Referral to mental health professionals, support groups, and occupational therapy can provide crucial support and coping mechanisms.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage comorbidities associated with Psoriatic Arthritis (e.g., cardiovascular disease)?
PsA often coexists with other health conditions, including cardiovascular disease (CVD). Managing these comorbidities is crucial for improving overall patient outcomes. We treat the whole patient, not just the PsA.
- Cardiovascular Risk Factors: PsA patients often have increased risk factors for CVD, such as hypertension, dyslipidemia (high cholesterol), and obesity. These need aggressive management.
- Medication Considerations: Some medications used to treat PsA, such as corticosteroids, can increase CVD risk. We carefully weigh the benefits and risks of medication choices, often opting for therapies with a more favorable cardiovascular profile.
- Lifestyle Modifications: We strongly encourage lifestyle modifications such as regular exercise (adapted to the patient’s physical limitations), healthy diet, smoking cessation, and weight management to reduce CVD risk. These are fundamental.
- Regular Monitoring: Regular monitoring of blood pressure, cholesterol levels, and other CVD risk factors is essential. Collaborating with cardiologists is often necessary for optimized care.
For example, a patient with both PsA and hypertension might receive medication to manage both conditions, along with dietary advice and regular exercise recommendations tailored to their limitations. This integrated approach is key.
Q 17. Explain the role of imaging (X-rays, ultrasound) in diagnosing and monitoring Psoriatic Arthritis.
Imaging plays a vital role in diagnosing and monitoring PsA. While not always definitive on its own, it provides valuable information to support clinical findings.
- X-rays: X-rays are useful for detecting erosions (bone damage), joint space narrowing (indicating cartilage loss), and other structural changes characteristic of PsA. They help assess disease severity and progression over time. Imagine it like seeing the ‘skeleton’ of the joint damage.
- Ultrasound: Ultrasound provides real-time images of soft tissues, allowing visualization of synovitis (inflammation of the joint lining), tenosynovitis (inflammation of tendon sheaths), and enthesitis (inflammation at the insertion points of tendons and ligaments). It’s like a detailed ‘soft tissue scan’.
In clinical practice, we use imaging to confirm the diagnosis, assess disease activity, and monitor the response to treatment. For example, a patient with suspected PsA might undergo hand X-rays to look for erosions. Serial ultrasounds can then track changes in synovitis following treatment with biologics.
Q 18. Discuss the use of corticosteroids in Psoriatic Arthritis.
Corticosteroids are potent anti-inflammatory drugs that can provide rapid relief of symptoms in PsA. However, they are typically used for short-term symptom control due to potential side effects.
- Systemic Corticosteroids: These are given orally or intravenously and are effective for reducing inflammation quickly. However, long-term use can lead to significant side effects, including osteoporosis, weight gain, diabetes, and increased risk of infections.
- Intra-articular Corticosteroid Injections: These injections directly into the affected joint provide localized relief with fewer systemic side effects. They are useful for managing flares in specific joints. Think of it as a targeted approach.
Corticosteroids are usually not a first-line treatment for PsA, but they can be beneficial in managing acute flares or severe symptoms. Their use should be carefully considered and monitored due to potential side effects. The goal is to use them judiciously for short bursts, as needed.
Q 19. Describe the different types of biologic therapies used to treat Psoriatic Arthritis.
Biologic therapies are powerful medications that target specific components of the immune system involved in the inflammation of PsA. They offer significant benefits for many patients who haven’t responded to other treatments.
- Tumor Necrosis Factor (TNF) inhibitors: These block TNF-alpha, a key inflammatory cytokine. Examples include etanercept, adalimumab, and infliximab.
- Interleukin-17 (IL-17) inhibitors: These block IL-17, another pro-inflammatory cytokine. Examples include secukinumab and ixekizumab.
- Interleukin-12/23 inhibitors: These block both IL-12 and IL-23, cytokines that promote inflammation. Ustekinumab is an example.
- Interleukin-23 inhibitors: These specifically target IL-23. Guselkumab is an example.
- Janus kinase (JAK) inhibitors: These inhibit certain enzymes involved in immune signaling. Examples include tofacitinib and upadacitinib. These are newer options.
The choice of biologic depends on individual patient factors, including disease severity, comorbidities, and prior treatment responses. Each biologic targets a slightly different part of the immune system, so finding the right one is a personalized journey.
Q 20. What are the contraindications for biologic therapy in Psoriatic Arthritis?
Several factors can contraindicate the use of biologic therapies in PsA. Safety is paramount.
- Active Infections: Biologics suppress the immune system, increasing susceptibility to infections. They are generally avoided in patients with active infections.
- Tuberculosis (TB): Patients should be screened for latent TB before starting biologics, as reactivation can occur. Treatment for latent TB is often required before starting biologics.
- Hepatitis B: Biologics can reactivate Hepatitis B; patients with a history of Hepatitis B need careful monitoring.
- Heart Failure: Some biologics may worsen heart failure; careful assessment is needed in patients with this condition.
- Pregnancy and Breastfeeding: Use during pregnancy and breastfeeding should be carefully considered and usually avoided due to a lack of safety data.
- Malignancies: Increased risk of certain malignancies has been associated with some biologics. This needs careful consideration.
A thorough evaluation of the patient’s medical history and current health status is essential before initiating biologic therapy to ensure safety and efficacy. We must carefully weigh the benefits against the potential risks.
Q 21. How do you manage treatment failure in Psoriatic Arthritis?
Treatment failure in PsA can be frustrating, but there are strategies to address it. It’s crucial to understand *why* treatment failed before making changes.
- Assess Adherence: First, we assess if the patient has been taking the medication as prescribed. Poor adherence can significantly impact outcomes.
- Evaluate Disease Activity: A thorough clinical evaluation, including imaging and laboratory tests, is necessary to assess the level of disease activity despite treatment. We need objective data.
- Consider Switching Biologics: If the initial biologic is ineffective, switching to another biologic targeting a different part of the immune system is a common strategy.
- Add on Therapy: In some cases, adding another medication, such as a conventional disease-modifying antirheumatic drug (DMARD), can enhance the effectiveness of the biologic.
- Consider Targeted Synthetic DMARDs (tsDMARDs): If biologics haven’t worked, tsDMARDs such as JAK inhibitors are another option.
- Referral to a Rheumatologist Specialist: Consult with a specialist for complex cases or when treatment failure occurs. They can provide expert guidance on further management options.
For example, if a patient fails to respond to a TNF inhibitor, we might switch to an IL-17 inhibitor or a JAK inhibitor. Each step is a collaborative decision, carefully considering the patient’s preferences and potential risks and benefits.
Q 22. Describe the process of initiating and tapering biologics.
Initiating and tapering biologics in Psoriatic Arthritis (PsA) requires a careful, individualized approach. Initiation usually begins with a loading dose, followed by regularly scheduled maintenance doses. This allows for rapid achievement of therapeutic levels in the bloodstream. The specific loading and maintenance schedules vary considerably depending on the particular biologic agent. For example, some TNF inhibitors might require a loading dose followed by bi-weekly injections, while others are administered monthly. Close monitoring of efficacy and adverse events is crucial during this initial phase.
Tapering, on the other hand, is a gradual reduction in the dose of the biologic, aiming to find the lowest effective dose while maintaining disease control. This process isn’t universally recommended and is often dictated by individual patient response and tolerability. For instance, if a patient achieves remission on a high dose, we might slowly decrease the dosage to see if they can maintain remission with a lower dose, thereby minimizing the long-term risk of side effects. However, abrupt cessation can lead to disease flares, so tapering must be done under careful medical supervision. The specifics depend on the patient’s response, comorbidities, and the half-life of the medication. We might reduce the frequency of injections initially, then decrease the dose itself over several months. Regular monitoring through clinical examination and laboratory tests is essential throughout the tapering process.
Q 23. What are the challenges in managing Psoriatic Arthritis in patients with comorbidities?
Managing PsA in patients with comorbidities presents significant challenges. The interplay between PsA and conditions like cardiovascular disease, diabetes, or chronic kidney disease complicates treatment decisions. For example, some biologics might increase the risk of infections, which could be particularly hazardous for a patient with compromised immunity due to diabetes or kidney disease. Similarly, certain medications used to treat comorbidities may interact negatively with PsA medications. The decision-making process becomes far more complex, necessitating close collaboration with other specialists, thorough risk-benefit assessments, and meticulous monitoring of both PsA and comorbidities.
A patient with PsA and cardiovascular disease, for instance, may require careful selection of a biologic agent that minimizes cardiovascular risks. We might opt for a medication with a known favorable cardiovascular safety profile, or carefully consider the use of additional medication that address the comorbidities and PsA separately. The ultimate goal is to achieve optimal control of both conditions without compromising the patient’s overall health and well-being. Regular monitoring is absolutely vital in such cases.
Q 24. How do you counsel patients on lifestyle modifications to manage Psoriatic Arthritis?
Counseling patients on lifestyle modifications is an integral part of managing PsA. It’s about empowering patients to take an active role in their own health. The key components of such counseling generally include:
- Healthy Diet: Encouraging a balanced diet rich in fruits, vegetables, and omega-3 fatty acids, while reducing processed foods, saturated fats, and sugary drinks, can help manage inflammation.
- Regular Exercise: Low-impact exercises like swimming, cycling, or walking are beneficial for improving joint mobility, strengthening muscles, and promoting cardiovascular health. We always need to ensure exercises are within the patient’s tolerance level to avoid exacerbating joint pain.
- Weight Management: Maintaining a healthy weight reduces stress on joints and can potentially alleviate some PsA symptoms.
- Stress Management: PsA symptoms can be exacerbated by stress, so we discuss strategies such as yoga, meditation, or deep breathing exercises to manage stress levels.
- Sleep Hygiene: Getting adequate, quality sleep is crucial for overall health and can positively impact disease activity. We provide guidance on establishing a consistent sleep schedule and creating a relaxing bedtime routine.
It’s crucial to approach this counseling with empathy and understanding. We acknowledge that lifestyle changes can be challenging and support patients in setting realistic, achievable goals. We work collaboratively with patients to tailor the plan to their individual circumstances and preferences.
Q 25. Describe your experience with specific Psoriatic Arthritis treatment modalities.
My experience encompasses a wide range of PsA treatment modalities, both conventional and biological. I have extensive experience with Disease Modifying Antirheumatic Drugs (DMARDs) such as methotrexate, sulfasalazine, and leflunomide. These are often the first-line treatment for many patients. I’ve also had significant success with various biologic agents, including TNF inhibitors (e.g., etanercept, adalimumab, infliximab), interleukin-17 inhibitors (e.g., secukinumab, ixekizumab), and interleukin-23 inhibitors (e.g., ustekinumab). The choice of treatment depends on several factors such as disease severity, patient comorbidities, prior treatment history, and patient preference.
For example, I’ve treated numerous patients with early PsA using methotrexate, achieving excellent results in many cases. In patients who don’t respond adequately to methotrexate or who have more severe disease, I’ve used biologic agents. I’ve observed that certain biologics are particularly effective in specific subsets of patients. For instance, interleukin-17 inhibitors have shown great efficacy in controlling skin manifestations associated with PsA, while other biologics might be better suited for managing joint inflammation.
Q 26. How would you approach a case of treatment-resistant Psoriatic Arthritis?
Treatment-resistant PsA necessitates a more aggressive and multifaceted approach. It involves a systematic reassessment of the patient’s condition, including a thorough review of their medical history, current medications, and response to prior treatments. This might involve advanced imaging (such as ultrasound or MRI) to better assess the extent of joint involvement. We often consider the following steps:
- Optimize Current Treatment: First, we evaluate whether the current medication is being administered appropriately and whether any potential drug interactions or adherence issues are contributing to treatment failure. We might consider increasing the dose of the current medication or switching to a different formulation.
- Combination Therapy: Combining multiple DMARDs or adding a biologic to a DMARD regimen can enhance efficacy. Careful monitoring of side effects is vital when employing combination therapy.
- Biologic Switching: If a patient is unresponsive to one biologic, a switch to a different class of biologic agent may be necessary. For instance, if a TNF inhibitor fails, we might consider an interleukin-17 or interleukin-23 inhibitor.
- Targeted Synthetic DMARDs (tsDMARDs): These newer medications, like tofacitinib or baricitinib, are another option to consider, especially when biologics are ineffective or contraindicated.
- Referral to a Rheumatologist specializing in PsA: A specialist consultation can provide expert opinion and potentially access to more advanced treatment options.
Treatment-resistant PsA is challenging, but a systematic and collaborative approach can often lead to better disease control and improved patient outcomes. Open communication with the patient and clear expectations are critical throughout the process.
Q 27. Explain the importance of shared decision-making in Psoriatic Arthritis management.
Shared decision-making is paramount in PsA management. It’s about empowering patients to actively participate in the design and execution of their treatment plan. Instead of simply prescribing medication, we engage in a collaborative dialogue, discussing the risks, benefits, and potential side effects of various treatment options in a way that is easily understandable. We consider the patient’s lifestyle, preferences, values, and priorities, ultimately aiming for a treatment plan that aligns with their individual needs and goals. This is not merely a matter of ethics, but is essential to ensure both treatment adherence and patient satisfaction.
For example, if a patient expresses concerns about the potential side effects of a particular biologic, we’ll explore alternative options, carefully weighing the benefits against the risks. We also involve patients in monitoring their progress and adjusting the treatment plan as needed. The patient becomes an active participant in their healthcare journey, improving overall treatment compliance and satisfaction. This shared decision-making approach fosters trust, improves adherence to the treatment plan, and leads to better outcomes.
Q 28. Describe your understanding of the latest research advancements in Psoriatic Arthritis treatment.
Recent research advancements in PsA treatment are very promising. There’s been a significant focus on developing novel biologics targeting specific inflammatory pathways. The development of new targeted synthetic DMARDs has provided alternative treatments for patients who do not respond well to traditional therapies or biologics. There’s also growing interest in understanding the genetic underpinnings of PsA to better identify patients who will benefit from specific treatments.
Furthermore, research is actively exploring biomarkers that could help predict treatment response and identify patients at higher risk of developing severe disease. This could lead to more personalized medicine approaches, tailoring treatment to individual patient characteristics. The advancements in imaging techniques, such as MRI and ultrasound, are also improving our ability to monitor disease activity and assess treatment response. Finally, there’s increasing emphasis on integrating digital health technologies and telehealth platforms to improve access to care and enhance treatment management for patients with PsA.
Key Topics to Learn for Psoriatic Arthritis Treatment Interview
- Disease Pathophysiology: Understanding the complex interplay of genetics, immune system dysfunction, and environmental factors contributing to Psoriatic Arthritis development.
- Clinical Presentation and Diagnosis: Differentiating Psoriatic Arthritis from other inflammatory arthritides, utilizing diagnostic criteria (e.g., CASPAR), and interpreting imaging findings.
- Pharmacological Management: In-depth knowledge of Disease-Modifying Antirheumatic Drugs (DMARDs), biologics (TNF inhibitors, IL-17 inhibitors, etc.), and targeted synthetic DMARDs (tsDMARDs), including their mechanisms of action, efficacy, and adverse effects.
- Non-Pharmacological Management: The role of lifestyle modifications (diet, exercise, weight management), physical therapy, and occupational therapy in managing Psoriatic Arthritis symptoms and improving patient quality of life.
- Treatment Strategies and Algorithm: Developing personalized treatment plans based on patient characteristics, disease severity, and response to therapy. Understanding treatment escalation strategies and the importance of shared decision-making.
- Monitoring and Assessing Treatment Response: Utilizing appropriate clinical and laboratory measures (e.g., joint counts, inflammatory markers, patient-reported outcome measures) to evaluate treatment efficacy and adjust therapeutic approaches.
- Comorbidities and Co-management: Recognizing and managing common comorbidities associated with Psoriatic Arthritis, such as cardiovascular disease, metabolic syndrome, and depression.
- Current Research and Future Directions: Staying updated on the latest research advancements in Psoriatic Arthritis treatment, including novel therapeutic targets and emerging treatment modalities.
- Ethical Considerations: Understanding the ethical implications of treatment decisions, including informed consent, shared decision-making, and access to care.
Next Steps
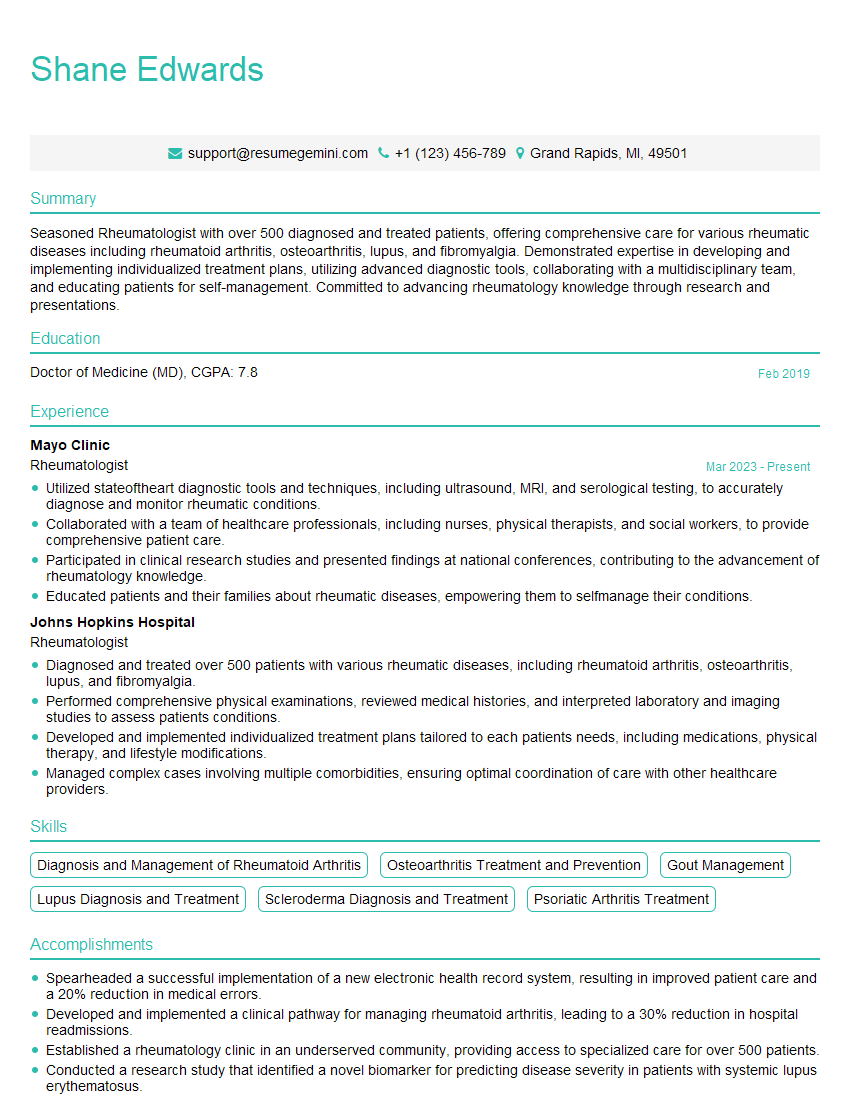
Mastering Psoriatic Arthritis treatment is crucial for career advancement in rheumatology and related fields. A strong understanding of these concepts will significantly enhance your interview performance and demonstrate your expertise. To increase your job prospects, focus on creating an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. Examples of resumes tailored to Psoriatic Arthritis Treatment are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.