Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Public Health and Preventive Medicine interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Public Health and Preventive Medicine Interview
Q 1. Describe the different levels of prevention in public health (primary, secondary, tertiary).
Public health prevention strategies are categorized into three levels: primary, secondary, and tertiary prevention. Think of it like a car accident: preventing the accident altogether is primary, quickly addressing injuries after the accident is secondary, and long-term rehabilitation is tertiary.
- Primary Prevention: This aims to prevent disease or injury before it ever occurs. Examples include vaccinations (preventing measles), promoting healthy lifestyles (reducing heart disease risk through diet and exercise), and advocating for policies that create safer environments (seatbelt laws to reduce traffic fatalities). The focus is on healthy populations.
- Secondary Prevention: This focuses on early detection and prompt treatment of disease to prevent progression and limit long-term consequences. Examples include screenings (mammograms for breast cancer), regular check-ups (identifying hypertension early), and contact tracing (controlling infectious disease outbreaks). The focus is on individuals who may be at risk or show early signs of disease.
- Tertiary Prevention: This focuses on managing long-term health problems and improving the quality of life for individuals already diagnosed with a disease or condition. Examples include rehabilitation programs after a stroke, chronic disease management (diabetes education), and support groups for individuals with mental health conditions. The focus is on minimizing disability and improving quality of life.
Q 2. Explain the concept of epidemiological triad and its application in disease prevention.
The epidemiological triad is a framework that describes the interaction between three key factors in the development of a disease: the agent, the host, and the environment. It’s like a three-legged stool – if one leg is weak, the stool (disease occurrence) is unstable.
- Agent: This is the causative factor of the disease, such as a bacterium (Salmonella), virus (influenza), or chemical toxin (lead).
- Host: This is the individual (or population) susceptible to the disease. Factors like age, genetics, immune status, and nutrition influence susceptibility.
- Environment: This encompasses all external factors that can influence the interaction between the agent and the host, including physical factors (temperature, sanitation), biological factors (vectors, reservoirs), and socio-economic factors (poverty, access to healthcare).
Applying the triad to disease prevention involves interrupting the chain of transmission at any of these three points. For example, to prevent malaria (agent: Plasmodium parasite), we can use mosquito nets (environment modification), antimalarial drugs (host intervention), or insecticide spraying (agent control).
Q 3. What are the key components of a health needs assessment?
A health needs assessment is a systematic process used to identify and quantify the health problems and needs of a specific population. It’s like taking inventory of a community’s health, highlighting areas requiring attention. Key components include:
- Defining the population: Clearly specifying the geographic area and population group to be assessed.
- Gathering data: Collecting data from various sources, including vital statistics (birth and death rates), disease surveillance data, health surveys (community health needs assessments), and qualitative data (focus groups, key informant interviews).
- Analyzing data: Summarizing the collected data to identify patterns and trends in health problems, risk factors, and health disparities.
- Prioritizing needs: Ranking health problems based on severity, prevalence, and potential for intervention.
- Developing recommendations: Formulating actionable recommendations for addressing the identified health needs. This may involve designing and implementing public health programs, advocating for policy changes, or improving access to healthcare services.
- Resource allocation: Determining how resources (financial, human, material) will be allocated to implement the recommendations.
Q 4. How do you measure the effectiveness of a public health intervention?
Measuring the effectiveness of a public health intervention involves comparing outcomes in a group that received the intervention with a group that did not (control group). This can be done using various metrics:
- Quantitative measures: These include changes in disease incidence or prevalence rates, mortality rates, hospitalization rates, or improvements in health behaviors (e.g., increased vaccination coverage).
- Qualitative measures: These capture the perspectives and experiences of those impacted by the intervention. They might involve conducting surveys, interviews, or focus groups to assess changes in knowledge, attitudes, and practices.
- Cost-effectiveness analysis: This assesses the cost of the intervention relative to the health benefits achieved, allowing comparisons between different interventions.
For instance, evaluating a handwashing campaign might involve comparing rates of diarrhea in communities with and without the intervention, as well as assessing changes in handwashing practices through surveys.
Q 5. Describe the different types of epidemiological study designs and their strengths and weaknesses.
Epidemiological study designs are chosen based on the research question and available resources. Some common designs include:
- Cross-sectional studies: Observe a population at a single point in time. Strengths: relatively quick and inexpensive; good for generating hypotheses. Weaknesses: cannot establish causality; susceptible to bias.
- Cohort studies: Follow a group of individuals over time to observe disease development. Strengths: can establish temporal relationships; useful for studying rare exposures. Weaknesses: expensive and time-consuming; prone to loss to follow-up.
- Case-control studies: Compare individuals with a disease (cases) to those without the disease (controls) to identify risk factors. Strengths: efficient for studying rare diseases; less time-consuming than cohort studies. Weaknesses: cannot establish causality; prone to recall bias.
- Randomized controlled trials (RCTs): Randomly assign participants to either an intervention group or a control group. Strengths: the gold standard for evaluating causality; minimizes bias. Weaknesses: expensive and time-consuming; ethical concerns may limit applicability.
Each design has its own strengths and weaknesses, and the choice of design depends on the research question and resources available.
Q 6. Explain the importance of data analysis in public health.
Data analysis is crucial in public health for several reasons:
- Identifying health problems: Analyzing data from surveillance systems, health surveys, and other sources allows us to identify emerging health threats, track disease trends, and understand the distribution of health problems across different populations.
- Evaluating interventions: Data analysis is essential for assessing the effectiveness of public health interventions and programs. We use statistical methods to compare outcomes in intervention and control groups and determine if the intervention had a significant impact.
- Identifying risk factors: Through statistical analysis, we can uncover risk factors associated with various health outcomes, enabling the development of targeted prevention strategies.
- Monitoring health equity: Data analysis helps us identify and monitor health disparities among different population groups, informing interventions to reduce health inequities.
- Informing policy decisions: Evidence-based data analysis provides a strong foundation for informing policy decisions related to public health resource allocation, program development, and health promotion initiatives.
Without robust data analysis, public health decision-making would be based on speculation rather than evidence.
Q 7. What are the social determinants of health and how do they impact health outcomes?
Social determinants of health (SDOH) are the conditions in which people are born, grow, live, work, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. They are the circumstances shaped by the distribution of money, power, and resources at global, national, and local levels.
- Examples of SDOH include: economic stability (poverty, employment), education access and quality, social and community context (social cohesion, discrimination), health care access and quality, and neighborhood and built environment (housing quality, access to healthy food).
- Impact on health outcomes: SDOH significantly impact health outcomes. For example, individuals living in poverty may have limited access to nutritious food, safe housing, and quality healthcare, leading to higher rates of chronic diseases and lower life expectancy. Similarly, lack of education can limit employment opportunities and access to health information, negatively influencing health outcomes. Discrimination based on race, ethnicity, or gender can lead to chronic stress and health disparities.
Addressing SDOH requires multi-sectoral approaches involving collaboration across various sectors (healthcare, education, housing, social services) to create healthier environments and reduce health inequities.
Q 8. How do you address health disparities in a community?
Addressing health disparities requires a multifaceted approach that tackles the root causes of inequities. It’s not enough to simply treat the symptoms; we need to understand and dismantle the systems that create these disparities in the first place.
- Data-Driven Assessment: We begin by meticulously analyzing health data to identify specific disparities. This might involve comparing disease rates, access to care, and health outcomes across different demographic groups within the community. For example, we might find higher rates of diabetes among a specific ethnic group or lower vaccination rates in a low-income neighborhood.
- Community Engagement: Crucially, we need to actively involve the community itself. This means working with community leaders, healthcare providers, and residents to understand their unique needs and perspectives. This participatory approach ensures that interventions are culturally relevant and effectively address the specific challenges faced by the community.
- Multi-sectoral Collaboration: Health disparities are rarely solely healthcare problems. They often stem from social determinants of health such as poverty, lack of education, inadequate housing, and environmental hazards. Addressing these requires collaboration with housing authorities, schools, social service organizations, and other relevant sectors.
- Targeted Interventions: Based on the data and community input, we can then develop targeted interventions. This could range from implementing culturally appropriate health education programs to advocating for policies that improve access to healthy food, affordable housing, and quality education. For instance, we might launch a mobile health clinic to increase access to care in underserved areas or develop a community garden to promote healthy eating habits.
- Evaluation and Adjustment: The process is iterative. We need to continuously monitor the impact of our interventions and adjust our strategies accordingly. Regular evaluation ensures that we’re making progress and are responsive to the evolving needs of the community.
Imagine a community struggling with high rates of cardiovascular disease due to limited access to healthy food and opportunities for physical activity. A successful strategy would involve partnering with local grocery stores to stock fresh produce, creating community walking trails, and launching a heart-health education program tailored to the community’s cultural background.
Q 9. Describe your understanding of the public health ethical principles.
Public health ethics rests on several core principles that guide decision-making and ensure that actions are just, fair, and respect individual rights.
- Beneficence: This principle emphasizes doing good and acting in the best interests of the population. Public health interventions should aim to improve health outcomes and prevent harm.
- Non-maleficence: This involves avoiding harm. Interventions should be carefully assessed to minimize potential risks and unintended consequences. For example, a vaccination campaign, while beneficial overall, must account for potential adverse reactions in a small percentage of individuals.
- Justice: This principle calls for fairness and equity in the distribution of health resources and benefits. Interventions should address health disparities and ensure that all members of the community have equal access to essential health services.
- Respect for autonomy: This principle upholds individual rights and choices. Public health interventions should respect people’s autonomy and provide them with the information they need to make informed decisions about their health. Mandatory vaccination programs, for example, must carefully balance the public good with individual rights and freedoms.
- Transparency and accountability: Public health actions should be transparent and open to public scrutiny. Decision-making processes should be clear and justifiable, and public health officials should be accountable for their actions.
A real-world example is the ethical debate surrounding mandatory mask-wearing during a pandemic. Balancing the principle of beneficence (protecting the community from disease spread) with the principle of autonomy (respecting individual choices) requires careful consideration and transparent communication.
Q 10. Explain the role of health communication in public health.
Health communication is crucial in public health because it bridges the gap between scientific knowledge and public action. Effective communication ensures that people have the information they need to make informed decisions about their health and participate in health-promoting behaviors.
- Risk Communication: This involves informing the public about potential health threats, such as pandemics or natural disasters, and explaining how to mitigate those risks.
- Health Promotion: This focuses on encouraging healthy behaviors, such as physical activity, healthy eating, and vaccination.
- Disease Prevention: This involves educating the public about disease prevention strategies, such as handwashing and safe sex practices.
- Crisis Communication: This involves providing timely and accurate information during public health emergencies, such as outbreaks or natural disasters.
- Community Engagement: Effective health communication goes beyond simply disseminating information. It involves engaging communities in a dialogue, actively listening to their concerns, and tailoring communication strategies to their specific needs and cultural contexts.
Consider an anti-smoking campaign. Effective health communication would go beyond simply displaying scary images of lung cancer. It would involve engaging community leaders, providing cessation support, and addressing the social and environmental factors that contribute to smoking behavior.
Q 11. What are the challenges of implementing health policies?
Implementing health policies presents numerous challenges, often stemming from complex political, economic, and social factors.
- Political Opposition: Policies often face resistance from interest groups that stand to lose from the changes. For example, the tobacco industry has historically lobbied against policies aimed at reducing smoking.
- Economic Constraints: Implementing effective policies requires resources, and budget limitations can hinder their success. Many public health interventions require significant funding for staffing, infrastructure, and program development.
- Implementation Challenges: Even well-intentioned policies can fail if they are not implemented effectively. This requires clear guidelines, adequate training, and strong monitoring systems.
- Public Resistance: Public acceptance is essential for the success of many health policies. Lack of public trust or understanding can lead to resistance, as seen in the controversies surrounding vaccine mandates.
- Data Gaps and Measurement Difficulties: Evaluating the effectiveness of health policies often requires sophisticated data collection and analysis, which can be expensive and time-consuming. Difficulties in measuring the impact of interventions can also make it challenging to demonstrate their effectiveness.
For instance, implementing a policy to increase access to healthy food in low-income areas might face political opposition from businesses that profit from selling unhealthy options, economic constraints due to limited funding, and public resistance from individuals who may prefer cheaper, less healthy alternatives.
Q 12. How do you evaluate the effectiveness of a health communication campaign?
Evaluating the effectiveness of a health communication campaign requires a multi-pronged approach that goes beyond simply measuring reach.
- Reach and Exposure: We assess how many people were exposed to the campaign’s messages. This can be measured through website traffic, social media engagement, and media coverage.
- Knowledge and Attitudes: We measure changes in people’s knowledge and attitudes related to the health issue addressed by the campaign. This might involve pre- and post-campaign surveys.
- Behavior Change: The ultimate goal is to see if the campaign led to changes in behavior. For example, did a campaign promoting handwashing lead to increased handwashing rates? This requires behavior monitoring and data collection in the target population.
- Program Process Evaluation: We also assess the effectiveness of the campaign’s implementation. Did the campaign reach the target audience as intended? Were there any challenges in implementing the campaign?
- Impact Evaluation: This involves assessing the overall impact of the campaign on health outcomes, such as reduced disease rates or improved health behaviors. This often requires longitudinal studies to track changes over time.
For example, in evaluating a campaign to promote physical activity, we would measure changes in self-reported physical activity levels, participation in exercise programs, and, ultimately, changes in relevant health indicators like BMI or cardiovascular risk factors.
Q 13. What is the difference between morbidity and mortality rates?
Morbidity and mortality rates are both important indicators of population health, but they measure different aspects.
- Morbidity Rate: This refers to the rate of disease or illness in a population. It’s often expressed as the number of cases of a specific disease per 1,000 or 100,000 people in a given population over a specified period. A higher morbidity rate indicates a greater prevalence of illness within a community.
- Mortality Rate: This refers to the rate of death in a population. It’s usually expressed as the number of deaths per 1,000 or 100,000 people in a given population over a specified period. A higher mortality rate signals a greater number of deaths within that community.
For example, a community might have a high morbidity rate for influenza (many people getting sick) but a low mortality rate (few deaths due to influenza). Conversely, a community might have a low morbidity rate for a particular cancer but a high mortality rate because the cancer is highly lethal.
Q 14. Explain the concept of herd immunity.
Herd immunity, also known as community immunity, is a form of indirect protection from infectious diseases. It occurs when a large percentage of a population becomes immune to an infection, making the spread of the disease unlikely.
This immunity can be achieved through vaccination or through prior infection. When a sufficient proportion of the population is immune, the disease is less likely to find a susceptible host and thus its transmission is interrupted, protecting even those who aren’t immune. The exact percentage needed for herd immunity varies depending on the disease and its mode of transmission.
Think of it like a forest fire. If most of the trees are fire-resistant (immune), the fire is less likely to spread widely. Similarly, if a large percentage of a population is immune to a disease, the spread of that disease is greatly reduced.
Herd immunity is crucial for protecting vulnerable individuals, such as infants or those with weakened immune systems, who may not be able to receive vaccines or might have a poor response to them. However, it’s essential to note that achieving herd immunity through natural infection can be risky and potentially lead to a large number of deaths and severe illnesses.
Q 15. Describe your experience with health surveillance systems.
My experience with health surveillance systems spans over a decade, encompassing both design and implementation. I’ve worked extensively with various systems, from nationally-integrated disease surveillance platforms to localized community-based initiatives. This includes experience with both passive surveillance, relying on mandatory reporting by healthcare providers, and active surveillance, involving targeted data collection and investigation, such as conducting epidemiological surveys or enhanced monitoring during outbreaks. For example, in my previous role, I was instrumental in improving the efficiency of our region’s influenza surveillance system by implementing a real-time data-entry system which reduced reporting delays significantly and facilitated more timely public health interventions. I’m also familiar with various data sources including electronic health records, laboratory results, mortality data, and syndromic surveillance data from sources like over-the-counter medication sales. My expertise extends to data analysis, using statistical methods to identify trends, patterns, and outbreaks, informing the development of effective public health strategies.
I understand the importance of various elements like data quality, timeliness, completeness, and comparability across various data streams. My experience includes collaborating with public health informaticians to ensure data integrity and interoperability which are critical in making meaningful, impactful interventions.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle data privacy and confidentiality in public health?
Data privacy and confidentiality are paramount in public health. I adhere strictly to all relevant regulations, including HIPAA in the US and GDPR in Europe. This means employing rigorous de-identification techniques, using secure data storage and transmission methods, and implementing strict access control protocols. Only authorized personnel with a legitimate need to access the data for public health purposes are granted access. All data handling procedures are documented and regularly audited to ensure compliance. We use anonymization and aggregation techniques whenever possible to reduce the risk of re-identification. For instance, instead of releasing individual-level data on disease cases, we might present aggregated statistics at a county or regional level. Furthermore, I actively participate in training programs to ensure that all team members are fully aware of and understand their responsibilities concerning data privacy and confidentiality.
Protecting individual privacy is not just a matter of compliance; it’s essential for maintaining public trust, which is critical for the success of any public health initiative. Transparency about data usage and its limitations is an integral part of how we operate.
Q 17. What is your experience with grant writing and securing funding for public health projects?
I have extensive experience in grant writing and securing funding for public health projects. I have successfully secured funding from various sources, including federal agencies (e.g., CDC, NIH), foundations (e.g., Robert Wood Johnson Foundation), and private corporations. My success stems from a deep understanding of funding priorities, coupled with the ability to articulate compelling project narratives that align with the funder’s mission. I’m proficient in developing strong research proposals, budgets, and evaluation plans. For example, I successfully secured a grant from the CDC to implement a community-based intervention to reduce childhood obesity. This involved a meticulous process of researching potential funders, crafting a persuasive grant application outlining project goals, methodology, and impact, and presenting our case during an interview. Developing realistic and achievable budgets and demonstrating a clear pathway for evaluating the impact of the project are equally vital aspects of this process.
Q 18. Explain your knowledge of infectious disease surveillance and control.
My knowledge of infectious disease surveillance and control is comprehensive. I’m proficient in applying epidemiological principles to identify, investigate, and control outbreaks. This includes experience with various infectious agents, including influenza, measles, and emerging infectious diseases. My work involves utilizing various surveillance systems to detect outbreaks, conducting epidemiological investigations to determine the source, mode of transmission, and risk factors, and implementing control measures, such as vaccination campaigns, contact tracing, and isolation. For instance, during a recent outbreak of measles in our community, I led an epidemiological investigation, which included interviewing cases, identifying contacts, and recommending vaccination strategies. I understand the importance of early detection and rapid response in controlling infectious diseases and am adept at using various data analysis techniques and epidemiological models to predict outbreaks and optimize resource allocation. Collaboration with laboratory personnel and clinical providers is key to ensuring swift and effective responses.
Q 19. How do you address health emergencies and crises?
Addressing health emergencies and crises requires a multi-faceted approach. My experience involves developing and implementing emergency response plans, coordinating with various stakeholders, and managing resources effectively during crises. This includes experience with natural disasters (hurricanes, floods), pandemic preparedness (influenza, novel coronaviruses), and bioterrorism events. The first step involves activating emergency response plans, which details pre-determined steps, communication channels, and resource allocation procedures. Rapid assessment of the situation, needs, and available resources is crucial. This is followed by resource allocation, communication with the public, and coordination with various stakeholders, including healthcare providers, emergency services, and government agencies. For example, during a hurricane, we established temporary shelters, coordinated medical services, and ensured access to essential supplies. Maintaining clear, consistent communication throughout a crisis is vital to minimize panic and maintain public trust.
Q 20. Describe your experience working in diverse community settings.
I have a strong track record of working effectively in diverse community settings. My experience includes working with communities of varying socioeconomic backgrounds, ethnicities, and cultures. I understand the importance of cultural sensitivity and community engagement in public health interventions. Effective community engagement involves building trust, actively listening to community concerns, and tailoring interventions to the specific needs and preferences of the community. For instance, during a public health campaign targeting a specific ethnic community, we took special care to understand their cultural beliefs and preferences before designing and delivering the program. This often involved using culturally appropriate languages and methods. Understanding the social determinants of health is crucial, and I tailor public health interventions to address underlying social, economic, and environmental factors that influence health outcomes.
Q 21. Explain your experience working collaboratively with interdisciplinary teams.
I’m highly skilled in collaborative work with interdisciplinary teams. Public health requires collaboration with professionals from various disciplines, including clinicians, epidemiologists, statisticians, public health informaticians, environmental health specialists, and community leaders. My approach emphasizes clear communication, shared goals, and mutual respect. This collaborative approach ensures a comprehensive and effective public health response. For example, during an outbreak investigation, I worked closely with clinicians to identify and characterize cases, with laboratory personnel to conduct testing, and with environmental health specialists to identify potential sources of contamination. I utilize a variety of communication methods, including regular meetings, email, and project management software, to ensure seamless teamwork and efficient workflow. I’m adept at facilitating consensus-building within teams, navigating diverse perspectives, and ensuring that all team members feel heard and valued.
Q 22. How do you stay updated on current public health issues and research?
Staying current in public health requires a multifaceted approach. It’s not just about reading the latest journal articles (though that’s crucial!). I employ a strategy that combines several key methods:
- Peer-reviewed journals and publications: I regularly subscribe to and read journals like the American Journal of Public Health, The Lancet, and JAMA, focusing on areas like epidemiology, disease surveillance, and health policy. I also follow prominent public health organizations like the CDC and WHO for their publications and reports.
- Professional organizations and conferences: Active membership in organizations such as the American Public Health Association (APHA) provides access to webinars, conferences, and newsletters, keeping me abreast of emerging trends and research findings. Attending these conferences allows for networking and direct interaction with leading experts.
- Online resources and databases: I leverage online databases like PubMed and Google Scholar to search for specific research articles and literature reviews. I also follow reputable news sources and public health blogs that provide summaries of important research and policy developments, but always critically assess the source’s reliability and potential bias.
- Social media and professional networks: Platforms like Twitter and LinkedIn connect me with other public health professionals, researchers, and organizations, enabling me to share and learn from others’ insights and perspectives. I carefully curate my network to ensure the information is from credible sources.
This combined approach ensures I stay well-informed about the dynamic landscape of public health and can effectively utilize the most up-to-date evidence in my work.
Q 23. Describe a time you had to make a difficult decision in public health.
During a measles outbreak in a highly underserved community, I faced a difficult decision regarding resource allocation. We had limited vaccine doses and competing needs: vaccinating children in schools versus targeting high-risk individuals in overcrowded shelters. Prioritizing one group over the other felt ethically challenging.
To navigate this, we employed a structured decision-making process. We first analyzed the epidemiological data, identifying areas with the highest prevalence and transmission rates. Then, we considered the potential impact of vaccination on each group, weighing factors like mortality risk, likelihood of spread, and community vulnerability. A crucial part of the process was transparent communication with the community, including leaders, healthcare providers, and residents of the shelters and schools. We explained the data, the rationale behind the prioritization, and the steps we were taking to ensure equitable distribution of future vaccine supplies. This helped to build trust and support for the tough choices we made. Ultimately, we prioritized vaccinating children in schools first, due to their higher risk of both transmission and severe complications, followed immediately by those in overcrowded shelters. We secured additional vaccine resources through collaborations with neighboring health departments to eventually vaccinate everyone. While difficult, this structured approach, emphasizing transparency and community engagement, helped us make the most responsible decision possible under the circumstances.
Q 24. Explain your understanding of health informatics and its applications in public health.
Health informatics is the application of computer and information science to improve healthcare. In public health, it’s transformative. It involves collecting, storing, analyzing, and interpreting health data to support decision-making, surveillance, and interventions.
Its applications are vast:
- Disease surveillance: Real-time data from electronic health records (EHRs) and other sources allows for rapid detection and response to outbreaks. For example, tracking flu cases using data from physician offices, hospitals, and labs can help predict and mitigate outbreaks.
- Population health management: Analyzing large datasets can identify high-risk populations, allowing targeted interventions to improve health outcomes. For instance, identifying individuals with diabetes through claims data allows for targeted education and support programs.
- Public health interventions: Health informatics supports the development and evaluation of public health interventions. For instance, using data analytics to understand which community health campaigns are most effective helps tailor campaigns in the future.
- Health communication: Technology enhances the reach and effectiveness of health communication. Web portals, mobile apps, and social media can provide individuals with access to health information and encourage healthy behaviours.
Essentially, health informatics empowers public health professionals to move from reacting to health crises to proactively improving population health.
Q 25. How do you use technology to improve public health outcomes?
Technology plays a vital role in enhancing public health outcomes. I use technology in several key ways:
- Data analysis and visualization: Statistical software (
R,SAS,Python) helps analyze large datasets to identify trends, risk factors, and disparities. Data visualization tools (e.g., Tableau) make it easier to communicate complex findings to diverse audiences. - Geographic Information Systems (GIS): GIS software helps map disease outbreaks, identify environmental hazards, and target interventions geographically. This visual representation of health data is crucial for effective resource allocation and community-based interventions.
- Electronic health records (EHRs): Access to de-identified EHR data allows for monitoring disease prevalence, tracking chronic conditions, and evaluating the impact of public health interventions.
- Mobile health (mHealth): mHealth applications can deliver health information, promote healthy behaviours, and provide access to telehealth services. For example, using mobile apps for chronic disease management or promoting vaccination uptake.
- Social media and digital communication: Effective communication using social media and targeted websites helps reach diverse communities, share important health information, and promote engagement in public health initiatives.
By leveraging these technologies responsibly and ethically, I aim to improve the efficiency, effectiveness, and reach of public health interventions.
Q 26. Explain your knowledge of health equity and health justice.
Health equity and health justice are intertwined concepts. Health equity refers to achieving health fairness and the absence of avoidable, unfair, or remediable differences among groups of people. It’s about ensuring everyone has a fair opportunity to attain their full health potential, regardless of their social position or other characteristics. Health justice takes it further, acknowledging the social determinants of health and addressing the root causes of health inequities – often stemming from systemic racism, oppression, and discrimination.
For example, disparities in access to healthcare, quality of care, and environmental exposures all contribute to health inequities. Health justice calls for addressing these upstream factors – improving housing, education, and economic opportunities – to create fairer and healthier societies. It’s about understanding that social injustices create health injustices, and rectifying both is crucial for achieving health equity.
My work involves actively identifying and addressing health disparities. This includes understanding the social, economic, and environmental factors impacting health within specific populations and using this knowledge to design interventions that are culturally sensitive, equitable, and effective.
Q 27. Describe your experience with program evaluation and quality improvement.
Program evaluation and quality improvement are integral to ensuring public health initiatives are effective and efficient. Program evaluation is the systematic assessment of an intervention’s impact, while quality improvement is a continuous process of refining existing programs to optimize their effectiveness and efficiency.
My experience includes conducting both formative and summative program evaluations. Formative evaluation involves assessing a program during its development, making adjustments as needed. Summative evaluation assesses the program’s impact after implementation. I use a variety of methods: quantitative data analysis (e.g., statistical tests to compare outcomes), qualitative data collection (e.g., interviews, focus groups to gather community perspectives), and mixed-methods approaches to combine both perspectives.
For quality improvement, I’ve used models such as the Plan-Do-Study-Act (PDSA) cycle, where changes are implemented in small steps, regularly evaluated, and adapted as needed. This iterative process ensures that programs are continuously improved based on real-time data and feedback. This may involve using data dashboards to monitor key indicators and make adjustments in real-time to maximize impact.
Q 28. How do you prioritize competing public health needs?
Prioritizing competing public health needs requires a systematic approach. There is rarely enough funding or resources to address all issues simultaneously. I use a framework that incorporates several steps:
- Needs assessment: A comprehensive assessment identifies the most pressing health issues using epidemiological data, community input, and consideration of burden of disease. This involves quantifying the impact, measuring the prevalence of a disease or health condition, identifying those most at risk and the effectiveness of potential interventions.
- Risk assessment: Evaluating the potential harm and the vulnerability of the affected population, factoring in severity, prevalence and the urgency of the intervention.
- Resource availability: Considering budgetary limitations, staffing capacity, and available infrastructure when making prioritization decisions.
- Stakeholder engagement: Input from community members, healthcare providers, and policymakers is crucial, ensuring that interventions align with community values and priorities.
- Ethical considerations: Prioritization must adhere to ethical principles, ensuring fairness and equitable distribution of resources.
- Data-driven decision-making: Using data to inform prioritization, demonstrating the impact of the chosen interventions and justifying those choices to the stakeholders.
In essence, prioritizing involves a balance of data-driven assessment, ethical considerations, community engagement, and effective resource allocation to maximize public health impact.
Key Topics to Learn for Your Public Health and Preventive Medicine Interview
Acing your interview requires a strong understanding of the field’s core principles and their practical application. Focus your preparation on these key areas:
- Epidemiology: Understanding disease patterns, outbreaks, and the factors influencing them. Consider practical applications like designing epidemiological studies or interpreting surveillance data.
- Biostatistics: Mastering the statistical methods used to analyze health data. Practice interpreting statistical outputs and applying them to real-world public health problems.
- Health Promotion and Disease Prevention: Develop a strong understanding of strategies for promoting healthy behaviors and preventing disease at individual, community, and population levels. Be prepared to discuss specific examples and their effectiveness.
- Health Policy and Management: Familiarize yourself with the policy-making process and how it impacts public health initiatives. Understand the role of public health organizations and the challenges they face.
- Social Determinants of Health: Explore the social, economic, and environmental factors that influence health outcomes. Be prepared to discuss how to address these factors through policy and programs.
- Environmental Health: Understand the impact of environmental factors on health and the strategies for mitigation and prevention. This includes topics such as air and water quality, sanitation, and hazardous waste management.
- Global Health: Familiarize yourself with global health challenges and the role of international collaborations in addressing them. Consider the ethical and logistical complexities involved.
- Health Communication and Advocacy: Understand how to effectively communicate public health information to diverse audiences and advocate for policies that promote health equity.
Next Steps: Launching Your Public Health Career
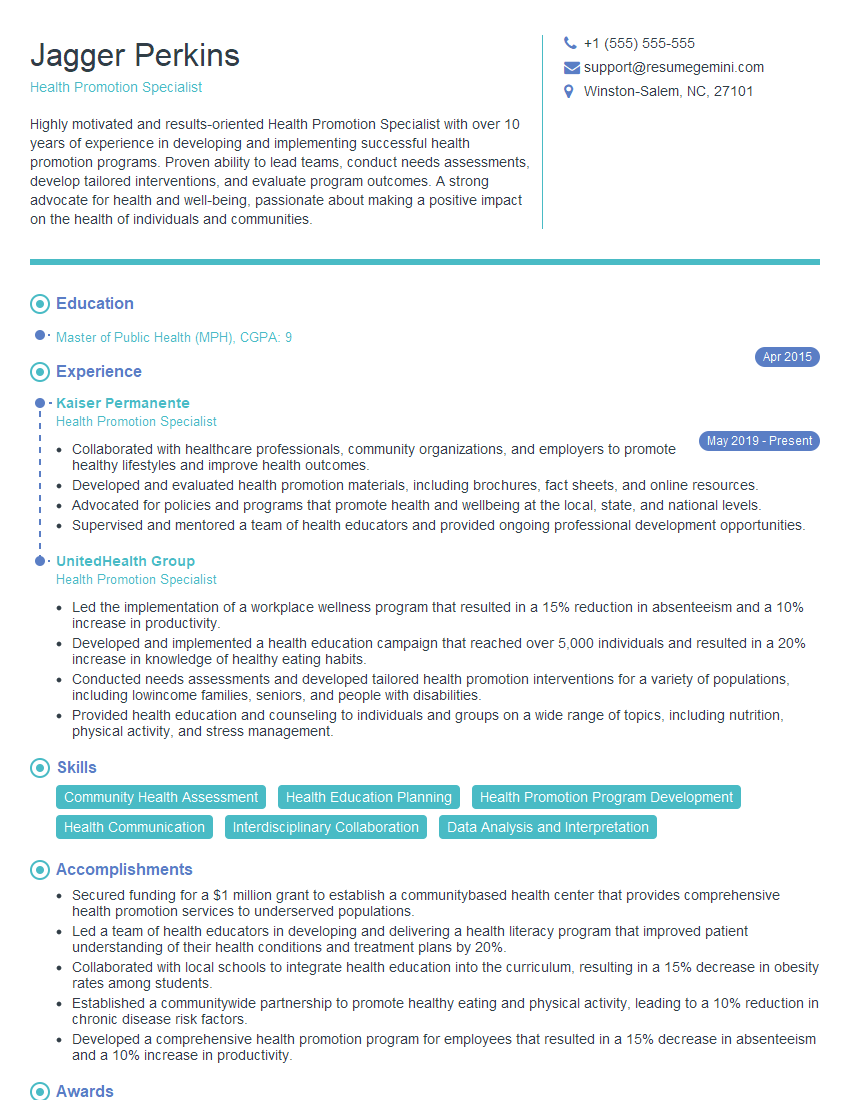
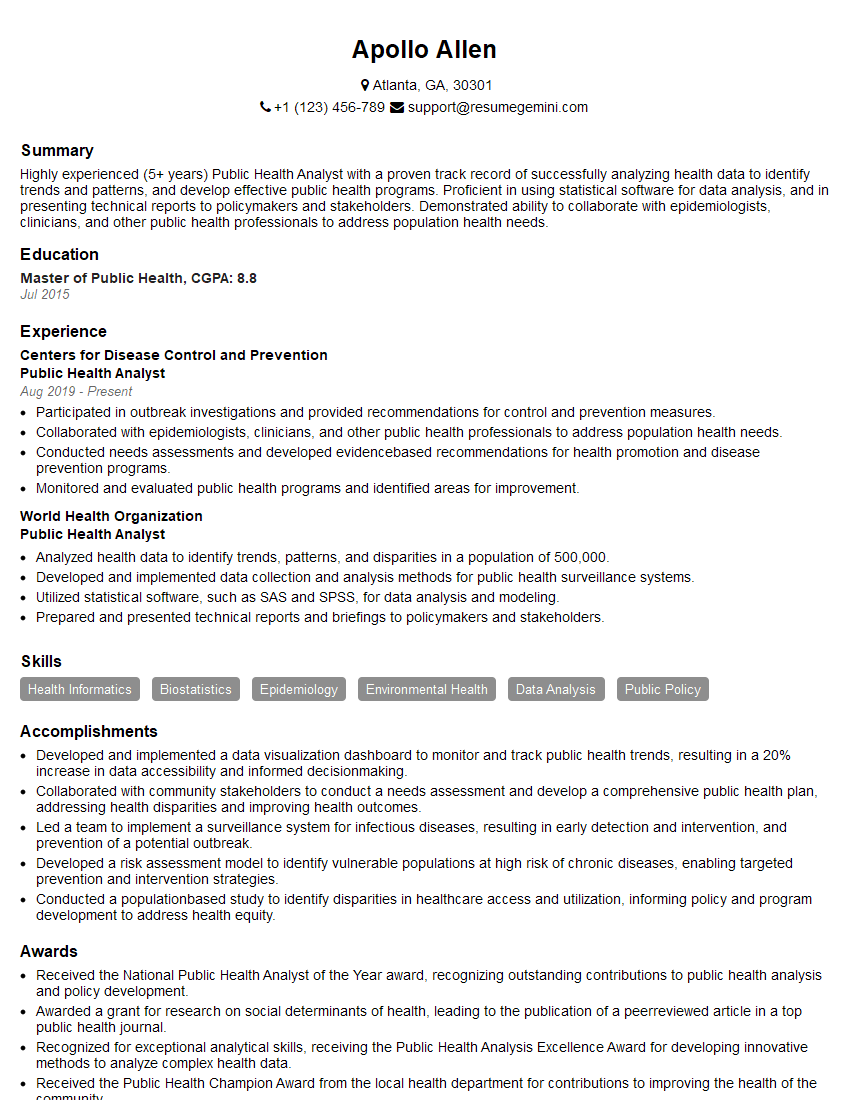
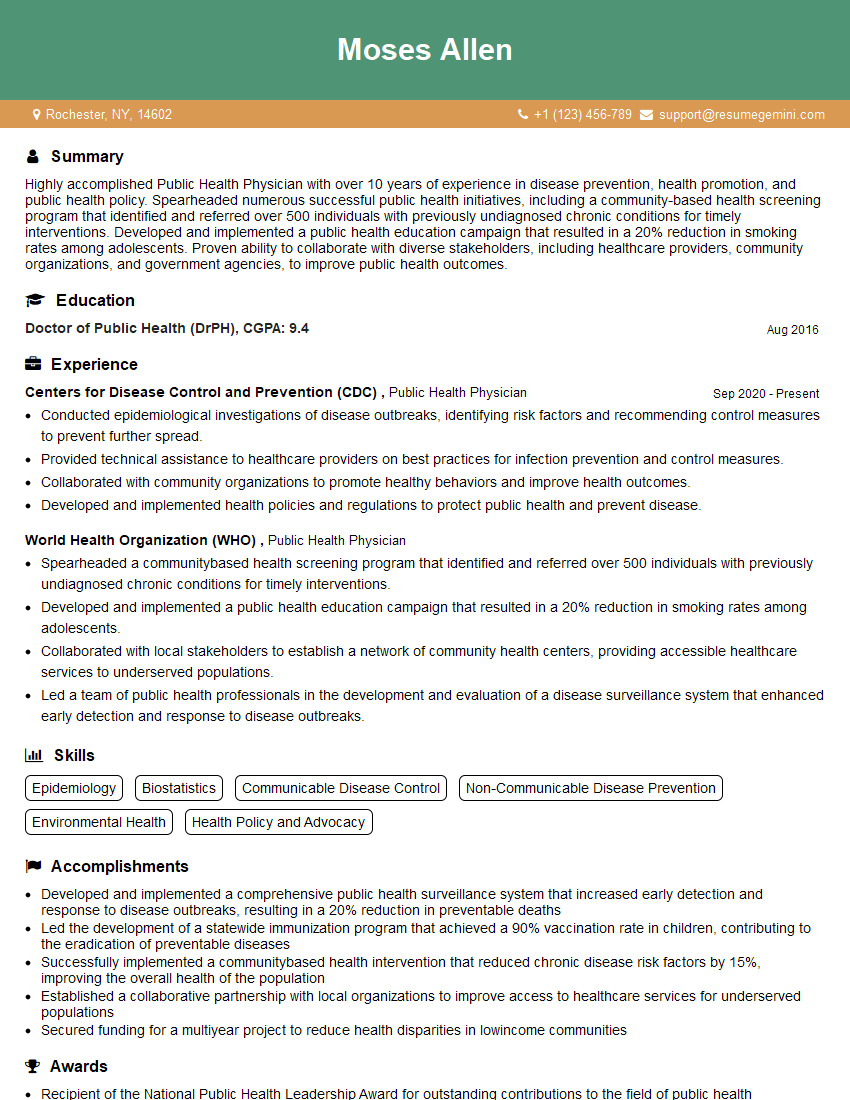
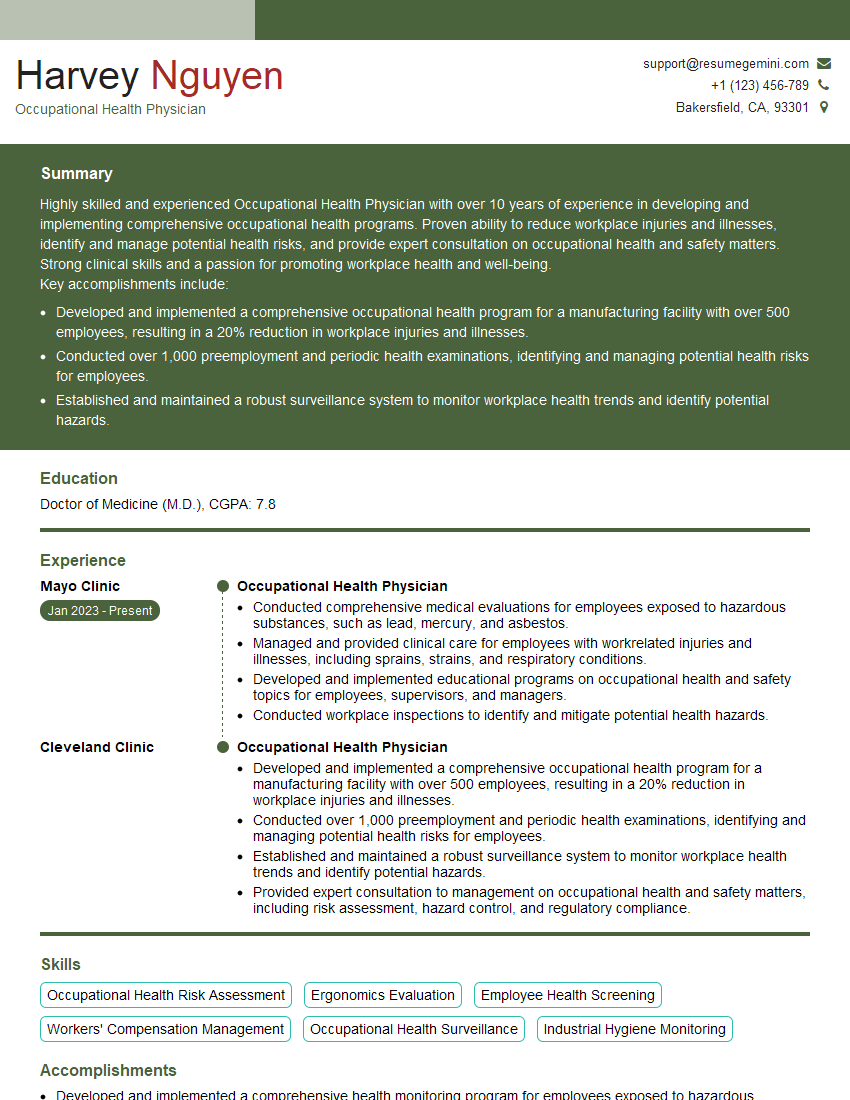
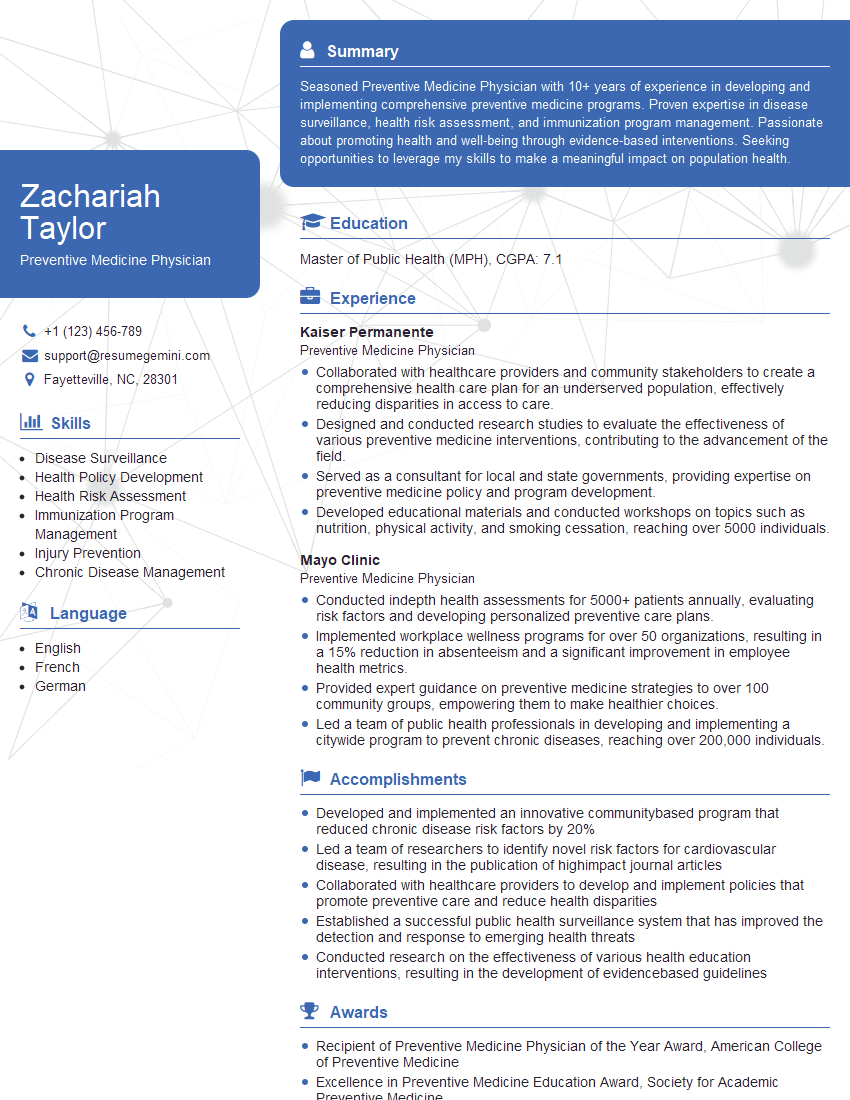
Mastering these concepts will significantly enhance your interview performance and demonstrate your readiness for a successful career in Public Health and Preventive Medicine. To maximize your job prospects, a strong, ATS-friendly resume is crucial. This is where ResumeGemini can help. ResumeGemini provides a trusted platform to build a professional resume that highlights your skills and experience effectively. We offer examples of resumes specifically tailored for Public Health and Preventive Medicine professionals to guide you. Invest time in crafting a compelling resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.