Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Rhinology interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Rhinology Interview
Q 1. Describe the different types of sinusitis and their management.
Sinusitis, or inflammation of the sinuses, is classified by its duration and location. Acute sinusitis lasts less than four weeks, subacute lasts four to twelve weeks, and chronic sinusitis persists for over twelve weeks. The location dictates whether it’s maxillary, frontal, ethmoid, or sphenoid sinusitis, often involving multiple sinuses simultaneously.
Management depends on the severity and duration. Acute sinusitis is often initially managed conservatively with saline nasal irrigation, nasal decongestants (used cautiously and for short periods to avoid rebound congestion), and pain relievers. If symptoms persist or worsen, antibiotics might be necessary, targeting common bacterial culprits. Chronic sinusitis often requires a more multifaceted approach, including long-term nasal corticosteroids (inhaled or oral), mucus-thinning agents, and potentially allergy management. In recalcitrant cases, Functional Endoscopic Sinus Surgery (FESS) becomes a consideration.
- Acute Sinusitis Management Example: A patient presents with facial pain, nasal congestion, and yellow-green discharge for five days. Initial treatment would involve saline nasal irrigation, over-the-counter pain relievers, and close monitoring. If no improvement after 7-10 days, antibiotics would be considered.
- Chronic Sinusitis Management Example: A patient with persistent nasal congestion, post-nasal drip, and reduced sense of smell for three months might require a combination of nasal corticosteroids, saline irrigation, and potentially allergy testing and treatment. If symptoms are not controlled, FESS could be explored.
Q 2. Explain the endoscopic anatomy of the paranasal sinuses.
Endoscopic anatomy reveals the complex network of paranasal sinuses. The endoscope allows visualization of the ostiomeatal complex (OMC), the critical drainage pathway of the sinuses. Key structures include:
- Anterior Ethmoid Air Cells: These cells are located anteriorly within the ethmoid bone and drain into the middle meatus.
- Middle Ethmoid Air Cells: Situated more posteriorly, they also drain into the middle meatus.
- Posterior Ethmoid Air Cells: These are the furthest back ethmoid air cells, often draining into the superior meatus.
- Maxillary Sinus Ostium: The natural opening of the maxillary sinus, typically located high on the medial wall of the sinus. Its location often contributes to poor drainage.
- Frontal Sinus Ostium: The opening of the frontal sinus, which drains into the frontonasal recess, a crucial area within the OMC.
- Sphenoid Sinus Ostium: The opening of the sphenoid sinus, located high and posteriorly, making it more challenging to access.
Understanding this anatomy is crucial for FESS, enabling surgeons to identify and address areas of obstruction and inflammation.
Q 3. What are the indications for functional endoscopic sinus surgery (FESS)?
Functional Endoscopic Sinus Surgery (FESS) is indicated when conservative management fails to alleviate symptoms of chronic sinusitis. Specific indications include:
- Chronic sinusitis refractory to medical therapy: Persistent symptoms despite adequate medical treatment.
- Recurrent acute sinusitis: Frequent episodes of acute sinusitis.
- Nasal polyposis: Presence of significant nasal polyps causing obstruction and symptoms.
- Sinonasal fungal disease: Fungal infections within the sinuses.
- Suspected sinonasal malignancy: Although biopsy is the primary diagnostic tool, FESS can facilitate tissue acquisition for pathological examination.
- CSF Rhinorrhea: Leakage of cerebrospinal fluid into the nose, often requiring surgical repair.
In each case, a thorough evaluation including history, physical examination, and often imaging (CT scan) is necessary to confirm the diagnosis and assess the suitability of FESS.
Q 4. Discuss the complications associated with FESS.
While FESS is generally safe and effective, potential complications exist. These can be broadly classified into intraoperative and postoperative complications:
- Intraoperative Complications: These include bleeding, damage to adjacent structures (e.g., orbit, optic nerve, intracranial structures), and perforation of the dura mater.
- Postoperative Complications: Postoperative complications can include persistent or recurrent sinusitis, epistaxis (nosebleed), orbital complications (e.g., orbital cellulitis, visual disturbances), cerebrospinal fluid leak, and meningitis. Rarely, infections might occur.
Minimizing risks requires meticulous surgical technique, precise anatomical knowledge, and careful patient selection. Postoperative care plays a crucial role in preventing and managing complications.
Q 5. How do you diagnose nasal polyps?
Diagnosis of nasal polyps typically involves a combination of:
- History and Physical Examination: Patients often present with nasal obstruction, hyposmia (reduced sense of smell), and possibly facial pressure or pain. Examination reveals pale, grey, smooth, polypoid masses in the nasal cavity.
- Nasal Endoscopy: This provides direct visualization of the polyps and assessment of their extent.
- Imaging: Computed tomography (CT) scans offer detailed anatomical information, helping to assess the size and location of polyps and rule out other pathology.
- Allergy testing: Often performed to identify potential underlying allergic triggers.
It’s important to differentiate nasal polyps from other nasal masses, such as tumors, which requires careful evaluation.
Q 6. What are the surgical options for nasal polyps?
Surgical options for nasal polyps depend on the severity and extent of disease. Options include:
- Functional Endoscopic Sinus Surgery (FESS): This is the most common surgical approach, aiming to remove polyps and improve sinus ventilation and drainage.
- Medical therapy (alone or pre-operatively): Topical or systemic corticosteroids can shrink polyps, making surgery less extensive or potentially avoiding the need for surgery altogether.
The choice of surgical technique is tailored to the individual patient and their specific clinical presentation. Postoperative management often involves nasal corticosteroids to prevent recurrence.
Q 7. Describe the management of epistaxis.
Epistaxis, or nosebleed, management depends on the severity and location of the bleed. Simple anterior bleeds often resolve with direct pressure applied to the soft portion of the nose, typically for 10-15 minutes. Patients should sit upright, leaning slightly forward to avoid swallowing blood.
More significant bleeds may require additional interventions, including:
- Chemical cautery: Application of silver nitrate or other cauterizing agents to the bleeding site.
- Packing: Insertion of nasal packing material to apply pressure and stop bleeding. This can be anterior packing (placed in the front of the nose) or posterior packing (placed further back, often requiring hospitalization).
- Embolization: A procedure where the bleeding vessel is blocked using specialized techniques. This is typically used for more severe posterior bleeds.
- Surgery: In rare cases, surgery may be necessary to ligate the bleeding vessel.
It’s crucial to identify and address underlying causes, such as hypertension, coagulation disorders, or tumors. If epistaxis is recurrent or severe, further investigation is warranted.
Q 8. Explain the different types of nasal fractures and their treatment.
Nasal fractures are breaks in the bones of the nose. They range from simple, minimally displaced fractures to complex, comminuted (shattered) fractures involving multiple bones. The classification often depends on the location and severity of the fracture.
- Simple fractures: These are usually single breaks with minimal displacement of the nasal bones. Think of it like a clean crack in a piece of wood.
- Comminuted fractures: These involve multiple breaks and fragmentation of the nasal bones. Imagine shattering a glass – many small pieces.
- Depressed fractures: The bone fragments are pushed inward towards the nasal cavity.
- Open fractures: These fractures penetrate the skin, increasing the risk of infection.
Treatment depends on the severity and timing. Simple, minimally displaced fractures often heal well without intervention, requiring only pain management, ice packs, and possibly nasal splinting. However, more complex fractures usually require surgical intervention – a closed reduction, where the bones are repositioned without an external incision, or an open reduction which involves an incision to directly visualize and repair the fracture fragments.
For example, a patient presenting with a severely displaced nasal fracture resulting in significant nasal deformity and obstruction would likely require an open reduction and rhinoplasty to restore the nasal structure and function.
Q 9. How do you evaluate and manage a patient with a deviated nasal septum?
A deviated nasal septum is a condition where the cartilage and/or bone that separates the nostrils (the septum) is crooked or off-center. This can obstruct airflow, leading to nasal congestion, difficulty breathing through the nose, nosebleeds, and sinus infections.
Evaluation involves a thorough history and physical examination. This includes assessing nasal airflow using a rhinomanometry (measuring airflow resistance), inspecting the nasal passages using a nasal speculum and possibly a rhinoscopy (endoscopic examination), and palpation to feel for septal deviations. Imaging, such as a CT scan, may be necessary in cases of complex septal deformities or if there is suspicion for associated injuries.
Management depends on the severity of symptoms. If symptoms are mild, conservative management, such as nasal saline irrigation and decongestants, may suffice. However, if symptoms are significant and affect quality of life, surgical correction (septoplasty) is often recommended. For example, a patient struggling with chronic nasal congestion affecting sleep and daily activities would benefit from a septoplasty.
Q 10. Describe the surgical techniques for septoplasty.
Septoplasty is a surgical procedure to straighten a deviated nasal septum. Several techniques exist, but the fundamental goal is to reshape the septal cartilage and bone to improve airflow without significantly altering the external nasal appearance.
- Endoscopic septoplasty: This minimally invasive technique utilizes an endoscope (a thin, flexible tube with a camera) to visualize the nasal passages and perform the surgery. Smaller incisions are made, resulting in less post-operative swelling and scarring. This is generally the preferred approach for most cases.
- Open septoplasty: This involves an incision in the columella (the skin between the nostrils) to gain direct access to the septum. This provides better visualization and allows for correction of more complex deformities. It’s often chosen for cases with significant septal deviations or those requiring concurrent procedures like rhinoplasty.
Both techniques involve carefully resecting (removing) or repositioning deviated cartilage and bone to create a straighter septum. The surgeon utilizes specialized instruments to achieve this. Post-operatively, nasal packing may be used to control bleeding and support the repositioned septum. Ultimately, the choice of technique depends on the individual’s anatomy and the severity of the deviation.
Q 11. What are the common causes of olfactory dysfunction?
Olfactory dysfunction, or loss of smell (anosmia), can have many causes, broadly categorized into:
- Upper Respiratory Infections (URIs): Viral infections are a common cause of temporary anosmia due to inflammation of the olfactory mucosa.
- Trauma: Head injuries, particularly those affecting the cribriform plate (the bony structure separating the nose from the brain), can sever the olfactory nerves leading to anosmia.
- Neurological disorders: Conditions such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis can affect the olfactory pathways.
- Nasal Polyps: These benign growths in the nasal sinuses can obstruct airflow and impair olfaction.
- Sinusitis: Chronic inflammation of the sinuses can affect olfactory function.
- Medications: Certain medications, such as nasal corticosteroids, can cause a decreased sense of smell.
- Smoking: Chronic exposure to smoke irritates and damages the olfactory receptors.
It’s crucial to consider that olfactory loss can be an early sign of neurological disorders, highlighting the importance of a thorough investigation.
Q 12. How do you diagnose and manage olfactory dysfunction?
Diagnosis of olfactory dysfunction begins with a detailed history including the onset, duration, and character of the smell loss. A Sniffin’ Sticks test is a commonly used tool to assess olfactory function objectively. This involves smelling different odorants and identifying them. Imaging studies, like CT or MRI, might be necessary to rule out structural causes such as tumors or fractures. Further investigations may include neurological examinations if neurological causes are suspected.
Management depends on the underlying cause. If the anosmia is due to a URI, it’s usually temporary and resolves spontaneously. If a structural cause, such as polyps, is identified, surgical intervention may be necessary. In cases of neurological involvement, management focuses on treating the underlying disease. Unfortunately, some causes of anosmia (like damage to the olfactory nerves) may be irreversible. Olfactory training can be attempted in some patients to improve their ability to detect odors.
Q 13. Discuss the various approaches to managing chronic rhinosinusitis.
Chronic rhinosinusitis (CRS) is a long-term inflammation of the nasal lining and sinuses. Management involves a multi-faceted approach:
- Medical Management: This includes nasal saline irrigation, topical and systemic corticosteroids to reduce inflammation, and antibiotics if bacterial infection is present. Mometasone furoate nasal spray is a common corticosteroid used for long-term control of CRS symptoms.
- Surgical Management: This is considered when medical management fails to provide adequate symptom relief. Surgical interventions aim to improve sinus drainage and ventilation. Functional endoscopic sinus surgery (FESS) is a common minimally invasive procedure to remove inflamed tissue and improve sinus drainage. Balloon sinuplasty, discussed below, is another surgical option.
- Allergen Avoidance: Identifying and avoiding allergens, such as pollen, dust mites, and pet dander, can help reduce inflammation and prevent exacerbations.
- Lifestyle Modifications: Maintaining good hydration, stopping smoking, and controlling other risk factors, such as environmental pollutants, can positively impact CRS management.
A tailored approach is necessary, combining medical and surgical strategies depending on the severity of CRS, the patient’s response to treatment, and the presence of complications like nasal polyps.
Q 14. What are the indications for balloon sinuplasty?
Balloon sinuplasty is a minimally invasive procedure used to widen the openings of the sinuses, improving drainage and ventilation. It’s not a replacement for FESS in all cases but has become a valuable tool for specific situations.
Indications for balloon sinuplasty include:
- Chronic rhinosinusitis unresponsive to medical therapy: Patients with CRS who haven’t experienced adequate improvement with medical management are candidates for balloon sinuplasty.
- Patients with limited access to FESS: Balloon sinuplasty can be performed in an office setting, potentially offering a less invasive alternative for patients who may not be candidates for a more complex procedure such as FESS.
- Patients with specific anatomical issues: Balloon sinuplasty may be particularly beneficial in patients with certain anatomical features that make FESS more challenging.
It’s essential to note that balloon sinuplasty may not be appropriate for all patients with CRS. The decision to proceed with balloon sinuplasty or other surgical options is made on a case-by-case basis after a careful assessment of the patient’s condition and other factors.
Q 15. Compare and contrast FESS and balloon sinuplasty.
Functional Endoscopic Sinus Surgery (FESS) and balloon sinuplasty are both minimally invasive procedures used to treat chronic sinusitis, but they differ significantly in their approach.
- FESS: This procedure involves using endoscopes and specialized instruments to remove diseased tissue, polyps, and bone obstructing sinus drainage. It’s a more extensive surgery, requiring precision and expertise to navigate the complex anatomy of the sinuses. Think of it like a thorough cleaning and remodeling of a clogged drainpipe.
- Balloon Sinuplasty: This technique uses a small balloon catheter to dilate the sinus ostia (openings) and improve drainage. It’s less invasive, typically requiring shorter operating time and less post-operative recovery. Imagine using a plumber’s snake to clear a less severe blockage.
Comparison: Both aim to improve sinus drainage, but FESS addresses more complex issues like significant polyposis or bony obstructions, while balloon sinuplasty is better suited for milder cases. FESS has a longer recovery time and potential for complications, though the success rate is high. Balloon sinuplasty is generally faster and safer but may not be effective for all cases of chronic sinusitis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage a patient with recurrent sinusitis?
Managing recurrent sinusitis requires a multi-pronged approach focusing on both medical and surgical options. It’s crucial to first identify the underlying cause of the recurrence.
- Medical Management: This often involves long-term use of nasal corticosteroids (like fluticasone or mometasone) to reduce inflammation and improve drainage. In addition, saline nasal irrigation helps to cleanse the sinuses. Antibiotics might be used for acute exacerbations, but their overuse can contribute to antibiotic resistance, so their use is carefully considered.
- Surgical Management: If medical management fails to provide relief, surgical intervention may be necessary. FESS or balloon sinuplasty could be considered depending on the patient’s specific condition and the severity of the sinus disease. Imaging is essential to determine the suitability for surgery.
- Allergy Management: Identifying and managing any underlying allergies is paramount since allergies often contribute to sinusitis. This involves allergy testing, immunotherapy (allergy shots), and avoidance of allergens.
A patient with recurrent sinusitis will require close follow-up to monitor their progress and adjust treatment as needed. This may involve regular appointments with an otolaryngologist to assess symptoms and imaging findings.
Q 17. Describe the role of imaging in the diagnosis of sinonasal disease.
Imaging plays a crucial role in diagnosing sinonasal diseases, providing valuable insights into the anatomical structures and pathological processes.
- CT scans: These are the gold standard for evaluating the paranasal sinuses. They provide high-resolution images, allowing detailed visualization of sinus anatomy, identifying areas of inflammation, fluid retention, bone erosion, and presence of masses or polyps. This allows for precise surgical planning in cases requiring FESS.
- MRI: While less frequently used than CT for sinus evaluation, MRI offers superior soft-tissue contrast and is helpful in assessing the extent of inflammation and differentiating between different types of tissues. It’s particularly valuable in evaluating tumors and assessing orbital or intracranial involvement.
- X-rays: While less detailed, X-rays can provide a preliminary assessment of sinus opacification (cloudiness) which suggests disease but is not specific.
By combining clinical findings with imaging data, clinicians can accurately diagnose different sinonasal pathologies, guide treatment decisions, and monitor the effectiveness of interventions. For instance, a CT scan showing opacified sinuses, mucosal thickening, and bony erosion might suggest chronic sinusitis that could benefit from FESS.
Q 18. What are the different types of nasal tumors?
Nasal tumors encompass a wide range of benign and malignant lesions. They are classified based on their origin and biological behavior.
- Benign tumors: These include papillomas (wart-like growths), angiofibromas (tumors containing blood vessels), and inverted papillomas (more complex growths that can sometimes become malignant). These often present as nasal obstruction, bleeding, or facial deformity.
- Malignant tumors: These are much more serious and can be life-threatening. Squamous cell carcinoma is the most prevalent malignant nasal tumor. Other types include adenocarcinomas, lymphomas, and sarcomas. These are often accompanied by symptoms like persistent nasal obstruction, epistaxis (nosebleeds), facial pain, and potential spread to other areas of the head and neck.
The exact type of nasal tumor dictates its management, emphasizing the importance of histopathological analysis (microscopic examination of a tissue sample).
Q 19. Discuss the surgical management of nasal tumors.
Surgical management of nasal tumors depends heavily on the tumor’s type, size, location, and extent of spread.
- Benign Tumors: Often managed with endoscopic resection (removal through the nose), often utilizing an endoscope to precisely remove the lesion while preserving surrounding structures.
- Malignant Tumors: These necessitate a more extensive approach, often requiring external approaches to ensure complete resection. This might involve partial or total maxillectomy (removal of part or all of the upper jaw bone), craniofacial resection (removal of bone from the skull and face), or neck dissection (removal of lymph nodes). The extent of surgery is determined by a multidisciplinary team of surgeons, oncologists, and radiation specialists. Post-surgical radiation therapy and chemotherapy are often used to prevent recurrence.
The surgical approach is tailored to each individual case to maximize tumor removal while preserving function and minimizing aesthetic consequences. For instance, a small, early-stage squamous cell carcinoma might be removed endoscopically, whereas a large, invasive tumor may require extensive resection and adjuvant therapy.
Q 20. How do you manage allergic rhinitis?
Managing allergic rhinitis focuses on reducing symptoms and improving quality of life. The approach is multifaceted and personalized.
- Pharmacological Management: This includes intranasal corticosteroids (like fluticasone or mometasone) to reduce inflammation, antihistamines to block histamine release and relieve sneezing, itching, and runny nose, and decongestants (often used short-term to alleviate nasal congestion). Leukotriene inhibitors provide another therapeutic option.
- Allergen Avoidance: Identifying and avoiding allergens is critical. This might involve removing pets from the home, using air purifiers, changing bed linens frequently, and avoiding exposure to known triggers.
- Immunotherapy (Allergy Shots): For patients with severe, persistent allergic rhinitis that doesn’t respond well to medications or allergen avoidance, immunotherapy can be highly effective in building tolerance to allergens over time.
The best management strategy for allergic rhinitis will depend on the individual’s symptoms, the severity of their allergies, and their preferences. For example, a patient with mild symptoms might only need over-the-counter antihistamines and allergen avoidance, while a patient with severe symptoms might require a combination of medications and immunotherapy.
Q 21. Explain the pathogenesis of allergic rhinitis.
Allergic rhinitis is triggered by an IgE-mediated hypersensitivity reaction to environmental allergens like pollen, dust mites, pet dander, and mold spores.
The process begins when allergen-specific IgE antibodies bind to mast cells in the nasal mucosa. Upon subsequent exposure to the same allergen, the allergen crosslinks IgE molecules on the mast cell surface, triggering degranulation. This releases a cascade of inflammatory mediators, including histamine, leukotrienes, and cytokines.
These mediators cause vasodilation (widening of blood vessels), increased vascular permeability (leakiness), edema (swelling) of the nasal mucosa, and stimulation of sensory nerves, leading to the characteristic symptoms of allergic rhinitis: sneezing, runny nose, nasal congestion, itching, and sometimes eye and throat symptoms.
Genetic predisposition plays a role, increasing susceptibility to developing allergic rhinitis. The chronic inflammatory response further contributes to the persistence of symptoms and potential for associated complications, including sinusitis and otitis media.
Q 22. Describe the different types of nasal stents and their applications.
Nasal stents are devices inserted into the nasal cavity to maintain patency (openness) after surgery or trauma, or to treat nasal obstruction. They come in various materials and designs, each with specific applications.
- Merocel stents: These are made of a biodegradable material that gradually dissolves over several days. They are commonly used after nasal polypectomy or septoplasty to prevent synechiae (scarring) and maintain airway patency. They are particularly useful for patients who might find removing traditional stents difficult.
- Silicone stents: These are flexible and reusable, offering longer-term support. They are often preferred for more complex cases requiring prolonged patency, such as after nasal fracture repair or in patients with recurrent nasal collapse.
- Balloon stents: These inflatable stents are deployed via a catheter and then inflated to provide structural support to the nasal passages. They can be particularly useful in treating nasal valve collapse or other complex nasal airway obstructions.
- Acrylic stents: Custom-made acrylic stents offer precise anatomical fitting and are ideal for correcting complex nasal deformities, often used in revision rhinoplasty cases.
The choice of stent depends on the individual patient’s needs, the surgical procedure performed, and the duration of support required. For example, a patient undergoing a simple septoplasty might benefit from a Merocel stent for its ease of use and biodegradability, whereas a patient with severe nasal valve collapse might require a more durable silicone or even a balloon stent for effective airway maintenance.
Q 23. What are the indications for nasal reconstruction?
Nasal reconstruction aims to restore the form and function of the nose after trauma, surgery, or congenital defects. Indications include:
- Trauma: Nasal fractures, lacerations, and other injuries resulting in deformities or functional impairments.
- Congenital anomalies: Birth defects affecting the nasal structure, such as cleft lip and palate.
- Skin cancer resection: Surgical removal of skin cancers from the nose may require reconstruction to cover the defect and restore the nasal contour.
- Rhinoplasty complications: Revision rhinoplasty is often indicated to correct unsatisfactory results from previous procedures.
- Infections: Severe infections that damage nasal tissues may require extensive reconstruction.
The decision to pursue nasal reconstruction hinges on the extent of the damage, the patient’s functional limitations, and their aesthetic concerns. A thorough evaluation, including physical examination, imaging (CT scan), and patient consultation, is crucial to determine the best course of action.
Q 24. Discuss the surgical techniques for nasal reconstruction.
Nasal reconstruction techniques are highly individualized and depend on the specific defect and available tissues. Common techniques include:
- Local flaps: Using nearby tissues, like skin and cartilage from the nose or surrounding areas, to reconstruct the defect. This is often preferred for smaller defects as it minimizes donor site morbidity.
- Free flaps: These involve transferring tissue from a distant location on the body (e.g., forearm, fibula) to the nose. This is used for larger defects or when local tissues are inadequate. Microvascular surgery is required to connect the blood vessels of the flap to the recipient site.
- Cartilage grafts: Autologous (from the patient’s own body, often the ear or rib) or allogeneic (donor) cartilage can be used to provide structural support and reshape the nose. This is frequently used in the correction of nasal deformities.
- Bone grafts: In cases involving significant bone loss, bone grafts can be used to reconstruct the underlying skeletal framework.
The surgical plan considers several factors including the location, size, and depth of the defect, the patient’s overall health, and available tissue resources. Often, a combination of techniques is used to achieve optimal results. For instance, a large defect may be initially repaired with a free flap followed by refinement with cartilage grafts to restore aesthetic contour.
Q 25. How do you manage a patient with CSF rhinorrhea?
CSF rhinorrhea, leakage of cerebrospinal fluid (CSF) from the nose, is a serious condition requiring immediate attention, as it carries a high risk of meningitis. Management involves a multidisciplinary approach:
- Initial assessment: A thorough neurological examination is essential to rule out intracranial injury or other complications. Beta-2 transferrin testing of the nasal drainage confirms CSF leakage.
- Conservative management (initial): This involves bed rest, head elevation (to reduce intracranial pressure), and prophylactic antibiotics to prevent infection. Lumbar drainage may be used in certain cases to reduce intracranial pressure.
- Surgical repair: This is the cornerstone of definitive treatment. The specific surgical technique depends on the location and cause of the leak. It may involve minimally invasive endoscopic approaches or open surgery, often aiming for a watertight seal of the defect using tissue grafts or other techniques.
- Post-operative care: Careful monitoring for recurrence of CSF leak and infection is crucial. Patients may require further imaging to confirm the success of the repair.
Timely diagnosis and appropriate management are vital to minimize the risk of life-threatening complications. A neurosurgical consultation is typically involved in the management of CSF rhinorrhea, ensuring optimal care and close collaboration between rhinology and neurosurgery.
Q 26. Explain the role of antibiotics in the management of sinusitis.
The role of antibiotics in sinusitis management is controversial and evolving. While antibiotics were previously widely prescribed, current guidelines emphasize a more targeted approach. Antibiotics are indicated in cases of:
- Severe or complicated sinusitis: This includes symptoms suggestive of orbital cellulitis (infection behind the eye), intracranial complications (brain abscess), or severe systemic illness.
- Failure to respond to conservative management: If symptoms such as facial pain, nasal congestion, and purulent rhinorrhea persist despite adequate symptom control with decongestants, saline irrigations, and anti-inflammatory medications, antibiotics may be considered.
- Immunocompromised patients: Individuals with weakened immune systems are at increased risk for severe sinusitis and may benefit from prophylactic or therapeutic antibiotics.
The choice of antibiotic is guided by local antibiograms (bacterial resistance patterns) and clinical judgment. Broad-spectrum antibiotics may be initially used, followed by narrower-spectrum antibiotics if the causative organism is identified. Prolonged antibiotic use should be avoided to minimize the risk of antibiotic resistance. The focus should always be on identifying and addressing underlying contributing factors alongside appropriate antimicrobial use.
Q 27. What are the potential long-term complications of sinusitis?
Untreated or recurrent sinusitis can lead to several potential long-term complications:
- Orbital complications: Inflammation may spread to the eye socket, causing orbital cellulitis, potentially leading to vision loss or blindness.
- Intracranial complications: In rare but serious cases, infection can spread to the brain, resulting in meningitis, encephalitis, or brain abscess.
- Osteomyelitis: Infection of the bone surrounding the sinuses.
- Nasal polyposis: Chronic inflammation can lead to the formation of nasal polyps, which can further obstruct nasal breathing and contribute to recurrent infections.
- Chronic sinusitis: Persistent inflammation can lead to irreversible damage to the sinus mucosa, resulting in chronic symptoms and reduced quality of life.
Early diagnosis and appropriate management of sinusitis are crucial to prevent these long-term complications. Regular follow-up and patient education regarding preventive measures are essential aspects of care.
Q 28. Describe your experience with minimally invasive sinus surgery techniques.
Minimally invasive sinus surgery (MIS), also known as functional endoscopic sinus surgery (FESS), has revolutionized the treatment of sinusitis. My experience with MIS encompasses a wide range of cases, from simple to complex sinus disease. The advantages of MIS include smaller incisions, reduced post-operative pain, shorter hospital stays, and faster recovery times compared to traditional open sinus surgery.
I routinely utilize endoscopes and specialized instruments to navigate the nasal passages and sinuses, identifying and addressing areas of inflammation and obstruction. Specific techniques employed include removal of diseased mucosa, widening of sinus ostia (openings), and improving sinus ventilation. I have extensive experience using image-guided navigation systems to enhance precision during complex procedures. In some cases, I utilize balloon sinuplasty, a minimally invasive technique employing a balloon catheter to dilate narrowed sinus openings. This less invasive technique is often well-suited for patients with chronic sinusitis who have not responded to medical therapy.
The outcomes of MIS are generally excellent, with most patients experiencing significant improvement in their symptoms. However, it’s vital to carefully select appropriate candidates for MIS. Careful patient selection, skilled surgical technique, and close post-operative monitoring are crucial for optimal results. I personally emphasize meticulous surgical technique to minimize complications and achieve optimal long-term outcomes for my patients. I believe that the continual advancement in MIS techniques and technology will continue to improve patient care in rhinology.
Key Topics to Learn for Rhinology Interview
- Nasal Anatomy and Physiology: Detailed understanding of the nasal cavity, paranasal sinuses, and their intricate relationships. This includes blood supply, innervation, and lymphatic drainage.
- Diagnostic Techniques: Proficiency in interpreting nasal endoscopy findings, CT scans, and other imaging modalities used in diagnosing rhinologic conditions. Consider practical application of interpreting images and correlating them with patient presentations.
- Common Rhinologic Diseases: Thorough knowledge of the etiology, pathophysiology, diagnosis, and management of rhinitis (allergic, non-allergic), sinusitis (acute, chronic), nasal polyps, and nasal tumors. Be prepared to discuss treatment strategies, including medical and surgical approaches.
- Surgical Techniques: Familiarity with functional endoscopic sinus surgery (FESS), septoplasty, turbinate surgery, and other relevant surgical procedures. Understanding the indications, contraindications, and potential complications of each procedure is crucial.
- Pediatric Rhinology: Understanding the unique challenges and considerations in diagnosing and managing rhinologic conditions in children. This includes congenital nasal anomalies and developmental aspects.
- Medical Management of Rhinologic Conditions: Deep understanding of medical therapies used in the treatment of allergic rhinitis, sinusitis, and other rhinologic conditions. Be ready to discuss medication classes, mechanisms of action, and potential side effects.
- Complications and Management: Knowledge of potential complications associated with rhinologic procedures and their management. This includes post-operative bleeding, infection, and other adverse events.
- Research and Evidence-Based Practice: Ability to critically appraise research studies and apply evidence-based principles to patient care. Prepare to discuss current trends and advancements in Rhinology.
Next Steps
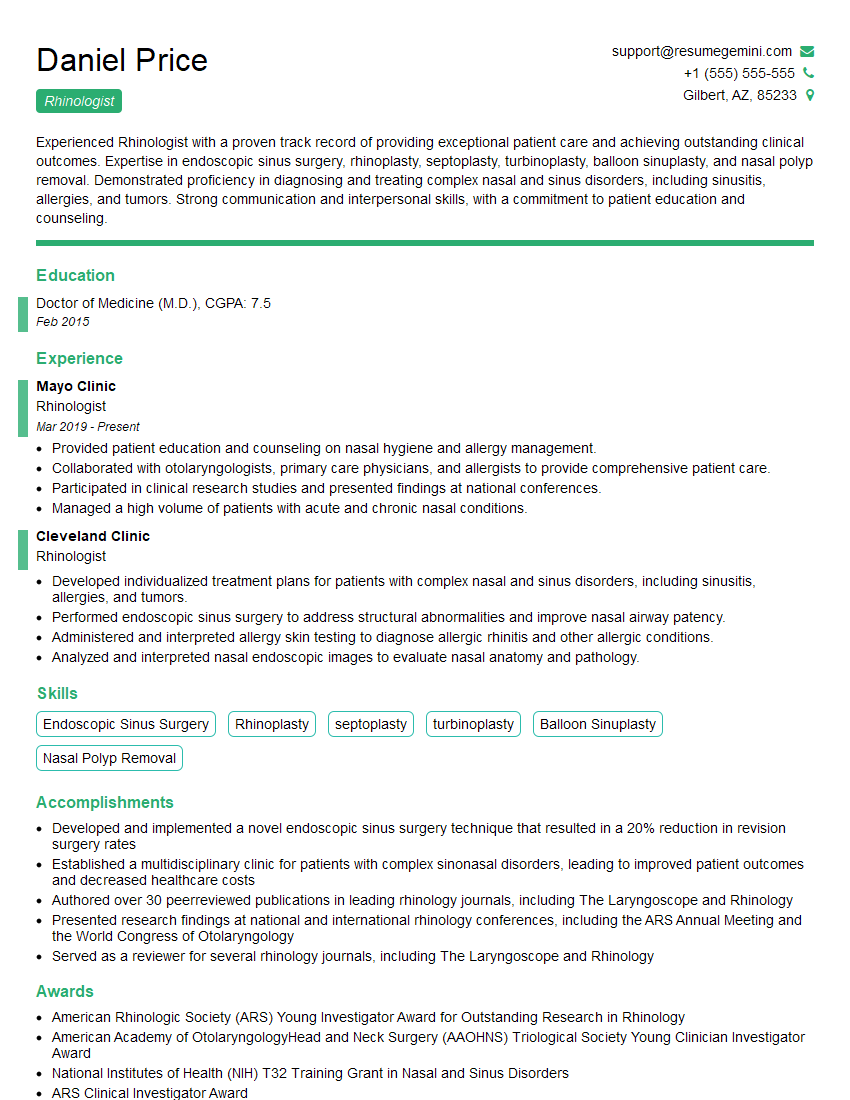
Mastering Rhinology opens doors to a rewarding career with opportunities for specialization and leadership. A strong foundation in this field is highly valued by employers. To maximize your job prospects, invest time in crafting an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource for building professional resumes. Use its tools to create a compelling document that showcases your expertise and helps you stand out from other candidates. Examples of resumes tailored to Rhinology are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.