Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Schizophrenia Treatment interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Schizophrenia Treatment Interview
Q 1. Describe the positive and negative symptoms of schizophrenia.
Schizophrenia is characterized by a range of symptoms, broadly categorized as positive and negative. Positive symptoms represent an excess or distortion of normal functions, while negative symptoms reflect a deficit or diminishment of normal functions.
Positive Symptoms: These are often the most noticeable and distressing. They include:
- Hallucinations: False sensory perceptions, most commonly auditory (hearing voices), but also visual, tactile, olfactory, or gustatory.
- Delusions: Fixed, false beliefs that are not based in reality, such as delusions of grandeur (believing one is famous or powerful), persecution (believing one is being followed or plotted against), or control (believing one’s thoughts or actions are being controlled by external forces).
- Disorganized thinking and speech: Difficulty organizing thoughts and expressing them coherently, leading to loose associations, tangential speech, or word salad (incoherent speech).
- Grossly disorganized or abnormal motor behavior: This can range from childlike silliness to unpredictable agitation, catatonia (immobility or excessive purposeless movement), or bizarre behavior.
Negative Symptoms: These are often more subtle and persistent, and can significantly impact a person’s quality of life. They include:
- Flat affect: Reduced expression of emotions, appearing emotionally unresponsive.
- Alogia: Poverty of speech, reduced fluency and content of speech.
- Avolition: Lack of motivation and initiative, difficulty starting or completing tasks.
- Anhedonia: Inability to experience pleasure or joy.
- Social withdrawal: Reduced interest in social interaction and relationships.
It’s crucial to remember that individuals with schizophrenia may experience a unique combination and severity of these symptoms, making individualized treatment essential.
Q 2. Explain the dopamine hypothesis of schizophrenia.
The dopamine hypothesis of schizophrenia proposes that an excess of dopamine activity in certain brain regions contributes to the development of the disorder. While not a complete explanation, it’s a cornerstone of our understanding of the illness and its treatment. Specifically, it suggests that:
- Increased dopamine synthesis: The brain produces more dopamine than usual.
- Increased dopamine release: More dopamine is released into the synapses (the gaps between nerve cells).
- Increased dopamine receptor sensitivity: Dopamine receptors in the brain are more responsive to dopamine.
- Decreased dopamine reuptake: Less dopamine is reabsorbed from the synapses.
This increased dopamine activity is thought to be particularly implicated in the development of positive symptoms like hallucinations and delusions. However, it’s important to note that the hypothesis has evolved, and we now understand that other neurotransmitters and brain regions are also involved in the complex pathophysiology of schizophrenia.
Research indicates that alterations in other neurotransmitter systems, including glutamate and GABA, also contribute to the disorder’s complex symptom profile.
Q 3. What are the different types of antipsychotic medications and their mechanisms of action?
Antipsychotic medications are the cornerstone of schizophrenia treatment. They’re broadly classified into two main categories: first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs).
First-Generation Antipsychotics (FGAs): These, also known as typical antipsychotics, primarily work by blocking dopamine D2 receptors. Examples include haloperidol and chlorpromazine. Their main mechanism is reducing the excess dopamine activity believed to contribute to positive symptoms.
Second-Generation Antipsychotics (SGAs): Also known as atypical antipsychotics, these medications have a broader mechanism of action, blocking not only dopamine D2 receptors but also other receptors like serotonin 5-HT2A receptors. Examples include risperidone, olanzapine, clozapine, and quetiapine. This broader receptor blockade is believed to be responsible for their often improved efficacy in treating negative symptoms and a reduced risk of certain movement disorders.
The choice between FGAs and SGAs depends on several factors, including symptom profile, patient preferences, side effect profile, and previous treatment response. Clozapine, while highly effective, is reserved for treatment-resistant cases due to its risk of agranulocytosis (a serious blood disorder).
Q 4. Discuss the side effects of antipsychotic medications and their management.
Antipsychotic medications can have a range of side effects, varying in severity and frequency depending on the specific medication and individual patient factors. These can include:
- Extrapyramidal Symptoms (EPS): These are movement disorders caused by dopamine blockade in the basal ganglia. They include akathisia (restlessness), Parkinsonism (rigidity, tremor, slow movement), dystonia (muscle spasms), and tardive dyskinesia (involuntary movements, often of the face and tongue, potentially irreversible).
- Metabolic side effects: Weight gain, increased blood sugar and cholesterol levels, increased risk of type 2 diabetes, and dyslipidemia (abnormal blood fats).
- Anticholinergic effects: Dry mouth, constipation, blurred vision, urinary retention.
- Sedation: Drowsiness and fatigue.
- Prolactin elevation: Can lead to menstrual irregularities in women and gynecomastia (breast enlargement) in men.
- Neuroleptic Malignant Syndrome (NMS): A rare but life-threatening reaction characterized by high fever, muscle rigidity, altered mental status, and autonomic instability. Requires immediate medical attention.
Management of Side Effects: The management of side effects often involves adjusting the dosage, switching medications, or adding medications to counteract specific side effects. For example, anticholinergic medications can help manage EPS, while lifestyle changes and potentially other medications might help with metabolic side effects. Close monitoring and regular communication between the patient and their healthcare provider are crucial for effective side effect management.
Q 5. How would you assess a patient’s response to antipsychotic medication?
Assessing a patient’s response to antipsychotic medication is a multifaceted process, requiring careful monitoring and consideration of several factors. It’s not simply about the reduction of positive symptoms; it’s about the overall improvement in the patient’s functioning and well-being.
Assessment Tools: We utilize a combination of:
- Symptom rating scales: Standardized scales like the Positive and Negative Syndrome Scale (PANSS) help quantify the severity of symptoms and track changes over time.
- Clinical interviews: Regular discussions with the patient and their family/caregivers provide valuable qualitative data on their functioning, mood, and overall well-being.
- Functional assessments: We evaluate the patient’s ability to perform daily tasks, such as personal hygiene, work, and social interactions.
- Monitoring of side effects: Regular checks for weight changes, blood work, and any extrapyramidal symptoms help ensure safety and medication tolerance.
Response Criteria: Significant improvement usually involves a substantial reduction in the severity of positive symptoms (hallucinations, delusions), an improvement in negative symptoms (motivation, social interaction), and enhanced overall functioning in daily life. The specific criteria for response may vary slightly depending on the treatment goals and the patient’s individual circumstances.
Q 6. What are the common challenges in adhering to medication regimens for schizophrenia?
Adherence to medication regimens is a significant challenge in schizophrenia treatment. Many factors contribute to non-adherence:
- Side effects: Unpleasant or debilitating side effects can lead patients to discontinue medication.
- Cognitive impairment: Difficulty remembering to take medication is common in schizophrenia.
- Cost and access: High medication costs or lack of insurance coverage can create barriers to adherence.
- Mental health symptoms: The very symptoms of schizophrenia, such as delusions or lack of insight, can interfere with adherence.
- Social factors: Lack of social support, poverty, or unstable housing can negatively impact adherence.
Strategies to Improve Adherence: Strategies to promote adherence include:
- Patient education: Thoroughly explaining the importance of medication and the potential consequences of non-adherence.
- Medication management support: Using tools such as pill organizers, reminders, or family involvement.
- Addressing side effects: Proactively managing side effects through dose adjustments or adding other medications.
- Motivational interviewing: Helping patients identify and resolve their barriers to adherence.
- Long-acting injectable medications: These medications offer a convenient option for patients struggling with daily pill-taking.
Q 7. Describe different psychosocial interventions used in schizophrenia treatment.
Psychosocial interventions play a vital role in schizophrenia treatment, complementing medication and improving overall outcomes. They address various aspects of the illness, including symptom management, social functioning, and quality of life.
Common psychosocial interventions include:
- Psychoeducation: Educating patients and their families about schizophrenia, its symptoms, treatment options, and strategies for managing the illness.
- Cognitive Behavioral Therapy (CBT): Helps patients identify and change negative thought patterns and beliefs that contribute to their symptoms.
- Social skills training: Teaches patients skills needed for effective communication and social interaction.
- Supported employment: Provides assistance with job searching, job placement, and maintaining employment.
- Vocational rehabilitation: Helps patients develop vocational skills and gain employment.
- Family therapy: Educates families about schizophrenia and helps them develop coping strategies for supporting their loved ones.
- Assertive Community Treatment (ACT): Provides intensive, community-based support to patients who have difficulty engaging with traditional mental health services.
The specific psychosocial interventions used will depend on the patient’s individual needs and circumstances. A collaborative approach, involving psychiatrists, psychologists, social workers, and other professionals, is often essential for providing comprehensive and individualized care.
Q 8. Explain the role of family therapy in managing schizophrenia.
Family therapy plays a crucial role in managing schizophrenia by improving the family’s understanding of the illness and its impact. It equips family members with effective coping strategies and communication skills to reduce stress and improve the patient’s overall well-being. It’s not about blaming the family, but rather empowering them to be part of the solution.
For example, a family might learn how to respond calmly to a patient experiencing hallucinations or delusions, reducing the likelihood of escalating conflict. The therapist guides the family in setting realistic expectations and fostering a supportive environment that promotes adherence to medication and treatment. This collaborative approach significantly reduces the likelihood of relapse and improves the patient’s quality of life.
- Education: Families learn about schizophrenia’s symptoms, causes, and treatment options.
- Communication Skills Training: Family members learn effective communication techniques to avoid arguments and misunderstandings.
- Problem-Solving Skills: Families learn to identify and address challenges related to the patient’s illness.
- Stress Management: Families learn techniques to manage the stress associated with caring for a loved one with schizophrenia.
Q 9. What are the cognitive behavioral therapy (CBT) techniques used in schizophrenia?
Cognitive Behavioral Therapy (CBT) for schizophrenia focuses on identifying and modifying negative thought patterns and maladaptive behaviors that contribute to symptoms. It’s a collaborative process where the therapist and patient work together to understand the relationship between thoughts, feelings, and behaviors.
- Cognitive Restructuring: This involves identifying and challenging delusional beliefs and hallucinations. For instance, if a patient believes they are being monitored by the government, the therapist helps them examine the evidence for and against this belief.
- Behavioral Experiments: These involve testing out beliefs in a safe and controlled environment. If a patient fears social situations due to paranoia, they might gradually engage in increasingly challenging social interactions with the therapist’s support.
- Problem-Solving Skills Training: This equips patients with strategies to manage everyday challenges, improving their independence and self-esteem.
- Relapse Prevention Planning: Patients learn to identify early warning signs of relapse and develop strategies to cope with these signs.
For example, a patient struggling with auditory hallucinations might learn to challenge the voices’ validity by engaging in distracting activities or practicing relaxation techniques.
Q 10. How would you address a patient experiencing a psychotic episode?
Managing a patient experiencing a psychotic episode requires a calm, empathetic, and systematic approach. Safety is paramount. The immediate priorities are ensuring the patient’s safety and the safety of those around them.
- Assess the situation: Determine the level of risk to the patient and others. Is the patient exhibiting aggression or self-harm behaviors?
- Create a safe environment: Reduce external stimuli (e.g., noise, crowds) and ensure the patient feels secure.
- Use a calm and reassuring tone: Avoid arguing or challenging the patient’s delusions directly. Validate their feelings without validating the content of their delusions.
- Administer medication: If the patient is prescribed antipsychotic medication, administer it as prescribed by their doctor.
- Seek professional help: Contact emergency services or the patient’s psychiatrist immediately.
- De-escalation techniques: Use active listening and empathy to help reduce the patient’s anxiety and agitation.
Imagine a patient experiencing visual hallucinations and becoming agitated. A calm, reassuring voice and a quiet, safe space can help de-escalate the situation before medication is required. Active listening and validating their fear, even if the source is not real, can build trust and reduce distress.
Q 11. Discuss the importance of relapse prevention strategies in schizophrenia.
Relapse prevention is crucial in schizophrenia because it significantly improves the patient’s quality of life and reduces the burden on their families and healthcare systems. Relapse refers to the return of psychotic symptoms after a period of remission.
Effective relapse prevention strategies include:
- Medication adherence: Taking prescribed antipsychotic medication regularly is the cornerstone of relapse prevention.
- Psychotherapy: CBT and other therapies help patients manage symptoms, cope with stress, and develop healthy coping mechanisms.
- Social support: Strong social connections and support networks provide a buffer against stress and increase resilience.
- Lifestyle changes: Maintaining a healthy lifestyle that includes regular exercise, a balanced diet, and sufficient sleep can significantly reduce the risk of relapse.
- Stress management techniques: Learning and practicing stress management techniques, such as yoga or meditation, can help manage triggers.
- Early warning sign identification: Patients and their families learn to recognize early warning signs of relapse.
For instance, a patient might notice increased anxiety or difficulty sleeping as early warning signs and immediately implement their relapse prevention plan, such as increasing medication adherence or seeking support from a therapist.
Q 12. What are the warning signs of an impending relapse in schizophrenia?
Recognizing warning signs of an impending relapse in schizophrenia is crucial for timely intervention and preventing a full-blown episode. These signs can vary from person to person, but some common indicators include:
- Increased anxiety or irritability: A noticeable increase in anxiety, irritability, or mood swings.
- Sleep disturbances: Changes in sleep patterns, such as insomnia or excessive sleeping.
- Withdrawal from social activities: Avoiding social interactions or becoming increasingly isolated.
- Changes in appetite or weight: Significant changes in eating habits, weight gain or loss.
- Decreased self-care: Neglecting personal hygiene or daily routines.
- Return of negative symptoms: A worsening of negative symptoms such as apathy, lack of motivation, or flat affect.
- Increased suspiciousness or paranoia: Heightened suspiciousness or paranoia, even if mild.
- Changes in thought patterns: Difficulty concentrating, disorganized thinking, or unusual thought content.
It’s important to note that not all individuals will experience all of these symptoms. A combination of these, or even a single prominent symptom, can signal an increased risk of relapse. Open communication with the patient and their support system is essential in identifying these changes early.
Q 13. How would you manage a patient experiencing treatment-resistant schizophrenia?
Treatment-resistant schizophrenia is a significant challenge, defined as a lack of substantial improvement despite adequate trials of at least two different antipsychotic medications. Managing this requires a multifaceted approach:
- Clozapine: This medication is often considered a last resort for treatment-resistant cases due to its unique mechanism of action and high efficacy, albeit with potential side effects.
- Combination therapy: Combining two or more antipsychotic medications can sometimes improve outcomes.
- Augmentation strategies: Adding other medications, such as antidepressants or mood stabilizers, to enhance the effectiveness of antipsychotics.
- Long-acting injectables: Switching to long-acting injectable antipsychotics can improve medication adherence, a crucial factor in treatment success.
- Psychotherapy: Continuing CBT or other psychotherapies to address psychological symptoms and improve coping skills remains vital.
- Electroconvulsive therapy (ECT): In select cases, ECT might be considered if other treatments fail.
- Regular monitoring: Frequent monitoring of symptoms, side effects, and medication efficacy is essential.
The choice of treatment strategy depends on the individual patient’s characteristics, symptom profile, and response to previous treatments. A collaborative approach involving the psychiatrist, patient, and their family is crucial in making informed decisions.
Q 14. Describe your experience with Assertive Community Treatment (ACT) programs.
Assertive Community Treatment (ACT) programs provide intensive, community-based services to individuals with severe mental illness, including schizophrenia. My experience working with ACT teams has been highly positive. I’ve seen firsthand the significant impact these programs can have on individuals who often struggle to engage with traditional mental health services.
ACT teams typically consist of a multidisciplinary group including psychiatrists, nurses, social workers, and peer support specialists who work collaboratively to provide comprehensive support. This support includes medication management, individual and group therapy, case management, assistance with housing and employment, and crisis intervention. The team’s commitment to working with individuals in their natural environment, rather than solely in a clinical setting, is a cornerstone of ACT’s success.
For example, an ACT team might assist a patient in finding stable housing, accessing vocational training, and connecting with social support networks. This comprehensive approach significantly reduces hospitalizations, improves quality of life, and empowers individuals to lead more fulfilling lives. Witnessing patients regain their independence and achieve meaningful goals within an ACT program is incredibly rewarding.
Q 15. What are the ethical considerations in treating patients with schizophrenia?
Ethical considerations in treating schizophrenia are multifaceted and demand careful consideration at every stage. A core principle is respect for autonomy – ensuring patients understand their diagnosis and treatment options and are actively involved in decision-making. This is especially challenging when psychosis impacts judgment. We must balance the patient’s right to refuse treatment with their safety and the potential harm to themselves or others.
Confidentiality is paramount, but exceptions exist in situations where there’s a clear and imminent risk of harm. Beneficence (acting in the patient’s best interest) and non-maleficence (avoiding harm) guide our choices, carefully weighing the benefits of medication against potential side effects. Finally, justice ensures equitable access to care regardless of socioeconomic status or other factors.
For example, a patient might refuse antipsychotic medication due to distressing side effects. Ethically, we must explore alternative strategies, perhaps focusing on psychosocial interventions, while carefully monitoring the patient’s condition and engaging in ongoing dialogue to build trust and explore treatment options collaboratively. This often involves navigating complex legal and ethical frameworks regarding involuntary commitment, which should only be considered as a last resort and with careful judicial oversight.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you approach patients with schizophrenia who are resistant to treatment?
Treatment resistance in schizophrenia is a significant challenge. It requires a holistic and personalized approach, moving beyond simply increasing medication dosage. First, we need to meticulously assess treatment adherence, exploring potential barriers like side effects, stigma, or lack of understanding about the illness.
We often engage in shared decision-making, involving the patient in choosing treatments and collaboratively setting goals. This might involve switching medications, exploring augmentation strategies (adding another medication to enhance the primary treatment’s effectiveness), or considering novel treatments like clozapine (which is reserved for treatment-resistant cases due to potential side effects).
Psychotherapy, particularly Cognitive Behavioral Therapy (CBT) and family therapy, plays a crucial role. CBT can help manage symptoms like delusions and hallucinations, improve coping mechanisms, and enhance social functioning. Family therapy addresses the emotional burden on families and provides support and education to improve family interactions and engagement in the treatment process.
For instance, a patient might be resistant to taking medication due to weight gain. We’d then explore alternative medication options with a lower risk of weight gain, emphasizing the long-term benefits of stable mental health versus short-term side effects. We’d also implement strategies to address lifestyle factors that contribute to weight gain.
Q 17. How would you differentiate between schizophrenia and other psychotic disorders?
Differentiating schizophrenia from other psychotic disorders requires careful clinical assessment considering various factors including symptom duration, symptom presentation, and the presence of other symptoms. Schizophrenia is characterized by a combination of positive symptoms (hallucinations, delusions, disorganized thinking), negative symptoms (flat affect, avolition, alogia), and cognitive deficits (impaired attention, memory, executive function).
The key differentiator is the duration of symptoms: schizophrenia requires continuous signs of the disturbance for at least six months. Other psychotic disorders, like brief psychotic disorder (symptoms lasting less than a month) or schizophreniform disorder (symptoms lasting 1-6 months), have shorter durations.
Schizoaffective disorder involves both psychotic symptoms and mood episodes (major depressive or manic episodes). Delusional disorder is characterized predominantly by non-bizarre delusions without other significant psychotic symptoms. Careful diagnostic interviews and assessments using standardized scales are crucial to differentiate these conditions. A comprehensive history, including family history of mental illness and substance use, is also important.
Q 18. Discuss the role of early intervention in schizophrenia.
Early intervention in schizophrenia is critical for improving long-term outcomes. Early detection and treatment can significantly reduce the severity and duration of psychotic episodes, minimize the risk of relapse, and improve overall functional outcomes. This typically involves identifying individuals at high risk of developing psychosis (e.g., those with attenuated psychotic symptoms or a family history of schizophrenia) through careful assessment and monitoring.
Early intervention programs usually involve a multidisciplinary team, including psychiatrists, psychologists, and social workers. Treatment often includes antipsychotic medication (typically at lower doses initially), psychosocial interventions such as CBT and family therapy, and social skills training. The goal is to prevent or mitigate the development of chronic symptoms, promote recovery, and support the individual’s ability to live independently and participate in society.
For example, a young person experiencing transient psychotic symptoms and a strong family history of schizophrenia might benefit from early intervention. Careful monitoring, supportive therapy, and education for both the patient and their family can significantly reduce the risk of a full-blown psychotic episode.
Q 19. What are the long-term goals of treatment for schizophrenia?
Long-term treatment goals for schizophrenia focus on achieving and maintaining remission, improving quality of life, and maximizing functional capacity. This is a continuous process that involves regular monitoring and adjustments to the treatment plan as needed.
The primary goal is to minimize the severity and frequency of psychotic symptoms, enabling individuals to lead fulfilling lives. We aim to improve social functioning, cognitive abilities, and independent living skills. Treatment also focuses on reducing hospitalization rates, promoting adherence to medication, and preventing relapse.
Supporting the individual’s integration into society and building a strong support system, including family, friends, and community resources, is a crucial aspect of long-term care. This also incorporates helping individuals develop coping mechanisms for managing stress and challenges, and accessing appropriate social and vocational support.
Q 20. Describe your experience with different assessment tools used in schizophrenia.
Assessment in schizophrenia involves a combination of clinical interviews, standardized rating scales, and neuropsychological testing. Clinical interviews provide a detailed history of symptoms, functioning, and social support.
Standardized rating scales, such as the Positive and Negative Syndrome Scale (PANSS) and the Brief Psychiatric Rating Scale (BPRS), quantify the severity of psychotic symptoms, enabling objective monitoring of treatment response. These provide a structured way to assess symptoms over time, enabling us to track progress and adjust treatment accordingly.
Neuropsychological testing evaluates cognitive abilities such as attention, memory, and executive functions, which are often impaired in schizophrenia. This helps us tailor interventions and support strategies to the individual’s specific cognitive strengths and weaknesses.
For instance, the PANSS allows us to systematically rate the severity of hallucinations, delusions, and negative symptoms, providing a quantitative measure of symptom improvement over the course of treatment. This data helps us make evidence-based decisions about medication changes or augmentation strategies.
Q 21. Explain the importance of patient and family education in schizophrenia management.
Patient and family education are indispensable components of schizophrenia management. Educating patients about their illness, its course, and treatment options empowers them to actively participate in their care and improves adherence to medication. This includes explaining the nature of schizophrenia, addressing misconceptions and stigma, and providing practical strategies for symptom management.
Family education is equally crucial. Families often experience significant emotional distress, requiring support and education to understand the illness, manage their own reactions, and provide effective support to their loved one. Family therapy can significantly improve communication, reduce conflict, and enhance collaboration in the treatment process.
Educating families about medication side effects, recognizing early warning signs of relapse, and developing coping strategies empowers them to support the patient effectively. This collaborative approach significantly improves patient outcomes and reduces the burden on families.
For example, a family might be unaware of the early warning signs of relapse. Educating them about changes in sleep patterns, increased social withdrawal, or worsening symptoms enables early intervention, potentially preventing a full-blown relapse.
Q 22. What are the common comorbid conditions associated with schizophrenia?
Schizophrenia is often accompanied by other mental health and physical conditions, which we call comorbid conditions. These can significantly complicate treatment and worsen the patient’s overall prognosis. Common comorbid conditions include:
- Substance Use Disorders: This is extremely prevalent, with nicotine addiction being particularly common. Alcohol and illicit drug use further complicate symptoms and treatment adherence.
- Anxiety Disorders: Conditions like generalized anxiety disorder, panic disorder, and social anxiety are frequently observed, adding another layer of distress for the individual.
- Depression: Major depressive episodes are common, often preceding the onset of schizophrenia or occurring concurrently. This can worsen the overall negative symptoms.
- Obsessive-Compulsive Disorder (OCD): OCD symptoms can sometimes overlap with certain aspects of schizophrenia, making diagnosis and treatment more challenging.
- Post-Traumatic Stress Disorder (PTSD): Traumatic experiences can trigger or exacerbate schizophrenic symptoms, requiring careful consideration in treatment planning.
- Medical conditions: Individuals with schizophrenia may also experience increased rates of cardiovascular disease, diabetes, and other physical health problems due to factors such as lifestyle, medication side effects, and lack of consistent healthcare.
Understanding these comorbidities is crucial for effective treatment planning, as addressing them simultaneously improves overall outcomes.
Q 23. How would you manage a patient with schizophrenia who is also struggling with substance abuse?
Managing a patient with schizophrenia and substance abuse requires a holistic and integrated approach. It’s not enough to treat one condition in isolation; they must be addressed concurrently. My strategy typically involves:
- Motivational Interviewing: This patient-centered approach helps the individual recognize the impact of substance use on their mental health and motivates them towards change.
- Medication Management: Antipsychotic medication is essential for managing psychotic symptoms. However, careful consideration is needed to select medications that minimize the risk of interaction with substances of abuse.
- Substance Abuse Treatment: This often involves referral to specialized programs, such as detoxification, residential treatment, or outpatient therapy. This might include cognitive behavioral therapy (CBT) adapted to address substance use, or medication-assisted treatment (MAT) for certain substances.
- Dual Diagnosis Treatment Team: Collaboration with psychiatrists, psychologists, social workers, and addiction specialists is critical. A coordinated care plan ensures consistent messaging and supports the patient’s recovery.
- Regular Monitoring: Close monitoring of both mental and physical health is necessary to detect relapses and adjust treatment accordingly. This includes regular blood tests and urinalysis.
For example, a patient struggling with both schizophrenia and alcohol dependence might require a combination of antipsychotics, participation in Alcoholics Anonymous, and regular sessions with a therapist specializing in dual diagnosis. The recovery journey is often challenging and requires patience, persistence, and strong collaboration between the patient and the treatment team.
Q 24. How do you incorporate cultural considerations into your treatment approach for schizophrenia?
Cultural considerations are paramount in schizophrenia treatment. Ignoring cultural factors can significantly hinder treatment adherence and effectiveness. My approach involves:
- Cultural Sensitivity Training: Ongoing education helps me understand different cultural beliefs, values, and communication styles related to mental illness.
- Assessment of Cultural Beliefs: Understanding the patient’s perspectives on mental illness, treatment, and family roles is critical. Some cultures might stigmatize mental illness or prefer alternative healing methods.
- Collaboration with Cultural Experts: Working with interpreters, community leaders, and culturally competent clinicians ensures that treatment is accessible and appropriate for the patient’s background.
- Adaptation of Treatment Approaches: Treatment plans need to be adapted to respect cultural preferences and beliefs while still being effective. This might involve adjusting communication styles, incorporating family involvement as appropriate, or considering culturally relevant therapeutic approaches.
- Addressing Cultural Barriers: Identifying and overcoming barriers such as language difficulties, transportation limitations, or lack of culturally appropriate services is crucial for successful treatment.
For instance, a patient from a culture that highly values family involvement might benefit from family therapy sessions. In contrast, a patient from a culture where open discussion of mental illness is discouraged requires a more sensitive and confidential approach.
Q 25. What is your experience with working in multidisciplinary teams for schizophrenia care?
My experience working in multidisciplinary teams for schizophrenia care has been overwhelmingly positive. I’ve found that a collaborative approach leads to superior patient outcomes. These teams typically include:
- Psychiatrists: Prescribing medication, managing symptoms, and providing ongoing psychiatric care.
- Psychologists: Providing therapy, such as CBT, to address symptoms and improve coping skills.
- Social Workers: Connecting patients with social services, support groups, and vocational rehabilitation programs.
- Nurses: Monitoring medication side effects, educating patients and families, and providing support.
- Occupational Therapists: Helping patients develop daily living skills and participate in meaningful activities.
- Case Managers: Coordinating care and ensuring seamless transitions between different services.
Effective communication and shared decision-making within the team are vital for successful treatment. Regular team meetings, clear documentation, and a unified treatment plan ensure that everyone is on the same page and working towards the same goals. The patient’s active participation in these discussions is encouraged to promote shared responsibility and self-efficacy.
Q 26. Explain your understanding of the recovery model in schizophrenia treatment.
The recovery model emphasizes the patient’s strengths, resilience, and ability to live a meaningful life despite their illness. It moves away from a purely medical model that focuses solely on symptom reduction. Key elements include:
- Person-centered care: Treatment plans are tailored to the individual’s unique needs, goals, and preferences.
- Hope and empowerment: The focus is on promoting hope, self-esteem, and self-management skills.
- Focus on strengths and resilience: Identifying and building upon the patient’s strengths and resources is crucial.
- Shared decision-making: The patient is actively involved in all aspects of their treatment, including goal-setting and decision-making.
- Social inclusion and community participation: Encouraging social connections, meaningful activities, and participation in the community.
- Recovery-oriented services: Accessing support services and programs tailored to promote recovery, such as peer support groups and vocational training.
Think of it like this: instead of just aiming to reduce symptoms, the recovery model aims to help the individual build a fulfilling life, even with the challenges of schizophrenia. This might involve finding employment, building strong relationships, and pursuing personal interests, all while managing their illness effectively.
Q 27. Describe a challenging case involving a patient with schizophrenia and how you addressed it.
One challenging case involved a young adult with schizophrenia who experienced significant medication non-adherence, resulting in frequent hospitalizations. He was also struggling with severe social isolation and expressed a lack of motivation to engage in treatment.
My approach involved:
- Building rapport and trust: I spent time getting to know him, understanding his perspective, and acknowledging his feelings of frustration and hopelessness.
- Motivational interviewing: I helped him explore his reasons for non-adherence and identify his own goals for recovery.
- Collaborative goal setting: We worked together to develop realistic and achievable goals, starting with small steps.
- Medication education: I provided clear, concise information about his medication and addressed his concerns about side effects.
- Referral to supported employment: This provided a structured work environment with ongoing support to help him gain confidence and social interaction.
- Peer support: Connecting him with a peer support group provided a sense of community and understanding.
Over time, his adherence improved, and his symptoms became more manageable. He started showing increased engagement in life and found a sense of purpose through his employment. This demonstrates the power of patient-centered care and a collaborative approach in overcoming challenging situations.
Q 28. What are your professional development goals related to schizophrenia treatment?
My professional development goals focus on enhancing my expertise in schizophrenia treatment through ongoing learning and collaboration. This includes:
- Advanced training in evidence-based therapies: Deepening my understanding and proficiency in therapies such as CBT, Acceptance and Commitment Therapy (ACT), and family-based interventions.
- Staying abreast of current research: Regularly reviewing the latest research findings on schizophrenia treatment and integrating new knowledge into my practice.
- Expanding knowledge of comorbidities: Strengthening my understanding of common comorbid conditions and their effective management.
- Mentorship and supervision: Seeking mentorship from experienced professionals to refine my skills and knowledge.
- Participation in professional conferences and workshops: Networking with colleagues and gaining insights from experts in the field.
I am committed to providing the highest quality of care for individuals with schizophrenia and continually striving to improve my expertise in this complex and challenging area.
Key Topics to Learn for Schizophrenia Treatment Interview
- Positive and Negative Symptoms: Understanding the distinction between positive and negative symptoms and their implications for treatment planning.
- Pharmacological Interventions: Knowledge of antipsychotic medications (first-generation and second-generation), their mechanisms of action, side effects, and monitoring strategies. Practical application: Discussing medication choices based on specific patient profiles and symptom presentation.
- Psychosocial Treatments: Familiarity with evidence-based psychosocial interventions such as Cognitive Behavioral Therapy (CBT), family therapy, and social skills training. Practical application: Explaining how these therapies complement pharmacological approaches.
- Diagnosis and Assessment: Understanding diagnostic criteria (DSM-5 or ICD-11), assessment tools, and the importance of differential diagnosis. Practical application: Describing a comprehensive assessment process for a patient presenting with potential schizophrenia symptoms.
- Relapse Prevention and Management: Strategies for relapse prevention, including medication adherence, early intervention, and coping mechanisms. Practical application: Developing a relapse prevention plan for a patient in remission.
- Ethical Considerations: Awareness of ethical dilemmas in schizophrenia treatment, such as informed consent, patient autonomy, and confidentiality. Practical application: Analyzing ethical challenges presented in a complex clinical scenario.
- Co-occurring Disorders: Recognizing and managing co-occurring disorders, such as substance abuse, depression, and anxiety. Practical application: Developing a treatment plan that addresses both schizophrenia and co-occurring disorders.
- Long-term Treatment and Recovery: Understanding the importance of long-term treatment, recovery-oriented care, and support systems. Practical application: Designing a comprehensive discharge plan that promotes long-term recovery.
Next Steps
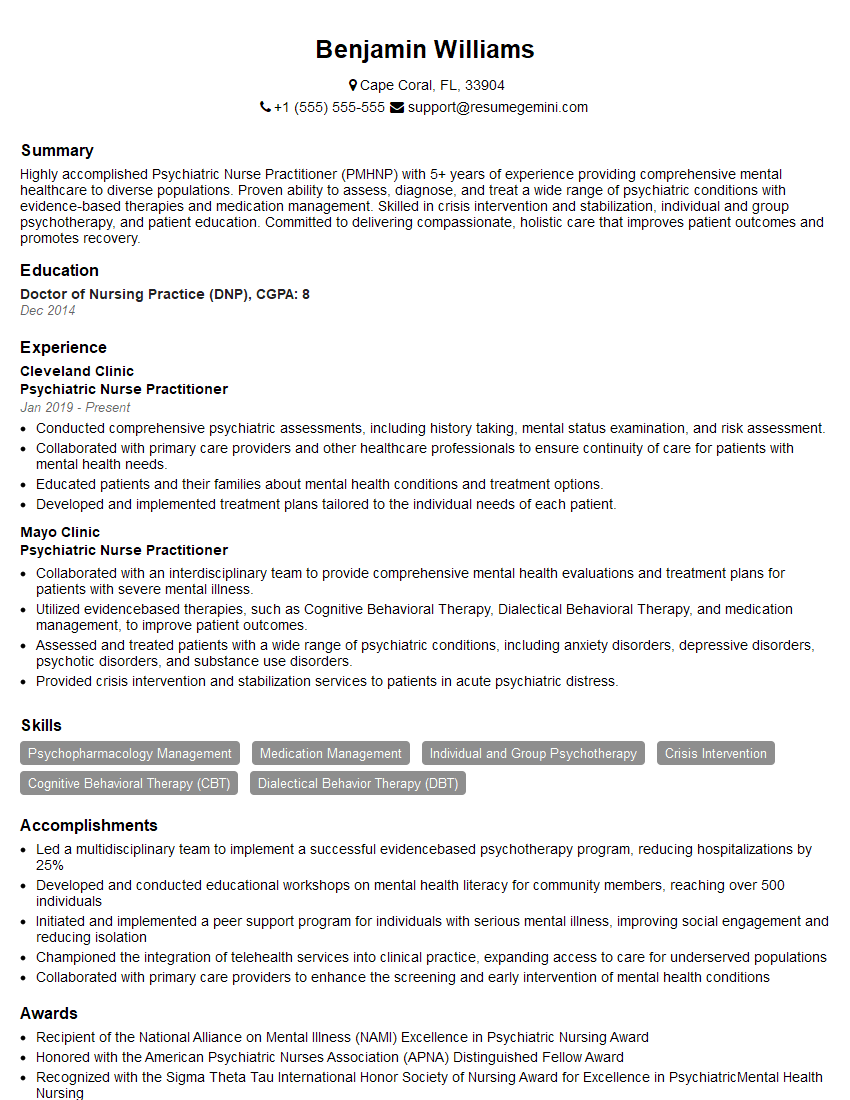
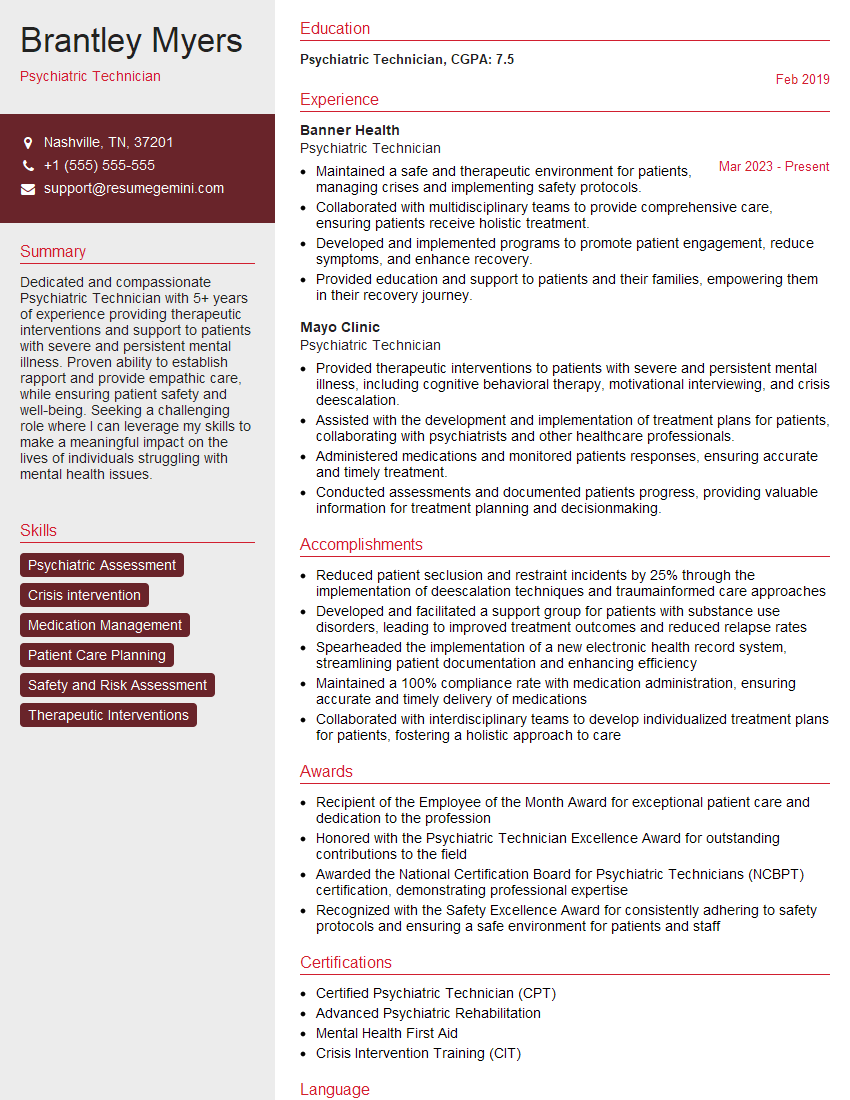
Mastering Schizophrenia Treatment demonstrates a deep understanding of complex mental health issues and positions you as a valuable asset in the field. A strong understanding of these concepts significantly enhances your career prospects, opening doors to diverse and rewarding opportunities. To maximize your chances, creating an ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you craft a compelling and effective resume tailored to highlight your expertise in Schizophrenia Treatment. Examples of resumes tailored specifically to this area are available to provide you with a clear framework for building your own.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.