Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Specimen Handling and Preparation interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Specimen Handling and Preparation Interview
Q 1. Explain the proper procedure for receiving and logging specimens.
Proper specimen reception and logging are crucial for maintaining sample integrity and traceability. It’s the foundation of accurate and reliable results. The process begins the moment a specimen arrives at the lab.
- Verification: The specimen’s identifying information (patient name, medical record number, date, time of collection, specimen type) on the requisition form must meticulously match the information on the specimen container. Any discrepancies must be immediately addressed by contacting the referring physician or clinic.
- Inspection: Visually inspect the specimen for any signs of damage, leakage, or improper labeling. Note any observations in the laboratory information system (LIS).
- Accessioning: Assign a unique laboratory accession number to the specimen. This number serves as a permanent identifier throughout the testing process. This is usually done automatically by the LIS.
- Logging: Enter all relevant information (accession number, patient details, specimen type, collection date and time, referring physician, tests requested) into the LIS. This creates an auditable trail.
- Storage: Immediately store the specimen according to its specific requirements (temperature, light protection). Blood samples, for instance, might require refrigeration, while tissue samples often require specific fixatives and storage conditions.
Imagine a scenario where a blood sample arrives with a mismatched name. Failing to identify this error could lead to incorrect results and potentially harm the patient. Rigorous logging and verification procedures are the safeguards against such mistakes.
Q 2. Describe your experience with different specimen types (e.g., blood, tissue, urine).
My experience encompasses a wide range of specimen types, each demanding specific handling techniques.
- Blood: I’m proficient in handling various blood samples (whole blood, serum, plasma) for a variety of tests, from routine hematology and coagulation studies to complex molecular diagnostics. Understanding anticoagulants and their impact on downstream analyses is essential.
- Tissue: Processing tissue samples for histology is a significant part of my work. This includes proper fixation, embedding, sectioning, and staining of specimens. Experience with different tissue types (e.g., biopsies, surgical specimens) is critical to optimizing processing techniques to maintain tissue architecture and antigenicity.
- Urine: Handling urine samples involves attention to detail regarding proper collection techniques to avoid contamination. I have experience performing routine urinalysis, as well as processing samples for more specialized assays.
- Other Specimens: My experience extends to handling other specimen types, including cerebrospinal fluid (CSF), body fluids (peritoneal, pleural, synovial), and stool samples. Each requires unique handling precautions to prevent contamination and maintain integrity.
For example, in processing a tissue biopsy for cancer diagnosis, careful fixation is paramount to preserve cellular morphology and ensure accurate interpretation by the pathologist. Improper fixation can compromise the diagnostic quality.
Q 3. How do you ensure the chain of custody is maintained for specimens?
Maintaining the chain of custody is paramount for the legal validity of test results, especially in forensic or medico-legal cases. It guarantees the integrity and authenticity of the evidence.
- Documented Transfers: Every transfer of a specimen must be meticulously documented, including the date, time, recipient, and purpose of the transfer. This is often done using barcodes and electronic tracking systems integrated with the LIS.
- Secure Storage: Specimens must be stored in secure locations with restricted access to prevent unauthorized handling or tampering. Temperature and humidity monitoring is also crucial for many specimens.
- Sealed Containers: Specimens are typically transported and stored in tamper-evident containers. Any breach of the seal must be immediately noted and documented.
- Multiple Signatures: In sensitive cases, multiple signatures may be required to document each transfer and verify the integrity of the chain of custody.
- Regular Audits: Regular audits of the chain of custody procedures help identify potential weaknesses and ensure compliance with regulations.
Imagine a criminal investigation relying on DNA evidence. A break in the chain of custody could lead to the dismissal of the evidence and compromise the entire case. The chain of custody is a critical element of ensuring the reliability and admissibility of the results.
Q 4. What are the critical steps in preparing tissue samples for histology?
Preparing tissue samples for histology is a multi-step process requiring precision and attention to detail. The goal is to produce high-quality sections for microscopic examination.
- Fixation: Immediately after removal, tissues are fixed, typically using formalin, to preserve cellular structure and prevent degradation. The choice of fixative depends on the type of tissue and the intended staining.
- Processing: The tissue undergoes a series of dehydration steps using increasing concentrations of alcohol, followed by clearing with xylene, and finally embedding in paraffin wax. This embedding provides structural support for sectioning.
- Sectioning: The embedded tissue block is sectioned using a microtome to create thin slices (usually 4-5 micrometers thick) that are mounted on glass slides.
- Staining: Sections are stained using various techniques (e.g., hematoxylin and eosin, special stains) to highlight specific cellular components and structures. This allows pathologists to make accurate diagnoses.
- Mounting and Coverslipping: Finally, the stained slides are mounted with a coverslip to protect the section and ensure long-term preservation.
For instance, inadequate fixation can result in tissue artifacts, making accurate diagnosis difficult. Conversely, proper fixation ensures that the cellular details are preserved and easily visible under the microscope.
Q 5. Explain the importance of proper labeling and identification of specimens.
Proper labeling and identification are critical for patient safety and the accuracy of laboratory results. It prevents sample mix-ups and ensures that the results are correctly associated with the appropriate patient.
- Unique Identifiers: Each specimen should have a unique identifier (e.g., accession number, barcode) that is consistently applied to all associated documents and containers.
- Patient Information: The specimen label should clearly display the patient’s name, medical record number, date and time of collection, and the type of specimen.
- Legible Labels: Labels should be printed clearly and permanently affixed to the specimen container using waterproof and durable materials.
- Multiple Labels: In some cases, multiple labels might be required (e.g., one on the container and another on the transport bag).
- Label Consistency: It’s essential to maintain consistency in labeling practices to ensure accurate tracking throughout the testing process.
Imagine a situation where two patients with the same name have specimens collected on the same day. Without clear and accurate labeling, a mix-up could have serious consequences. Proper labeling is a fundamental step in ensuring accurate and safe laboratory practices.
Q 6. Describe your experience with different fixation methods.
Fixation is a critical step in preserving the structure and composition of tissue samples. The choice of fixative depends on the type of tissue and the intended analyses.
- Formaldehyde (Formalin): The most commonly used fixative for routine histology. It crosslinks proteins, preserving cellular morphology. However, it’s a known carcinogen, so safe handling practices are essential.
- Bouin’s Solution: Excellent for preserving nuclear and cytoplasmic details. It’s particularly useful for certain types of tissue and staining techniques.
- Alcohol-Based Fixatives: Suitable for cytology specimens and some specialized histochemical procedures. They are effective in preserving cellular components.
- Microwaving Fixation: This method accelerates the fixation process but requires specialized equipment and careful attention to avoid over-fixation or tissue damage.
For example, using formalin for fixation for immunohistochemistry is crucial to preserve antigenicity. Other fixatives may alter the antigenicity, leading to false-negative results. The choice of fixative is not arbitrary; it is tailored to the specific requirements of each test.
Q 7. How do you handle specimens that arrive improperly labeled or damaged?
Improperly labeled or damaged specimens pose significant challenges. My approach involves a systematic process to address these issues and prevent errors.
- Assessment: The first step involves carefully assessing the extent of the damage or labeling error. Note all relevant observations in the LIS.
- Contacting the Referring Physician: Attempt to contact the referring physician or clinic to clarify the information or obtain a replacement specimen. This is crucial to prevent misidentification.
- Documentation: Meticulously document all communication and actions taken regarding the mislabeled or damaged specimen.
- Rejection (if necessary): If the specimen is severely damaged or the identification cannot be reliably established, it may be necessary to reject the specimen. The referring physician will be notified.
- Internal Investigation (if necessary): If the error occurred within the laboratory, an internal investigation might be conducted to determine the cause of the issue and prevent future occurrences.
A scenario might involve a specimen with an illegible label. Simply guessing the patient identity is unacceptable. Contacting the referring physician is crucial to obtain the correct information and prevent a potentially serious medical error.
Q 8. What quality control measures do you employ during specimen handling?
Quality control in specimen handling is paramount to ensure accurate and reliable results. It’s a multi-step process starting from the moment a specimen is received until it’s archived. We employ a robust system encompassing several key measures:
- Proper Identification and Labeling: Each specimen receives a unique identifier, meticulously tracked through every stage. This prevents mix-ups and ensures traceability. For instance, we use barcodes linked to our laboratory information system (LIS).
- Chain of Custody Documentation: A detailed record of every person who handles the specimen, along with the time and date, is maintained. This is vital for audit trails and ensuring accountability. Think of it like a package tracking system for medical samples.
- Temperature Monitoring: Specimens requiring specific temperatures are stored and transported accordingly, with continuous monitoring using data loggers. Improper temperature can degrade samples, yielding unreliable results. Imagine the difference between storing ice cream at room temperature versus in a freezer.
- Regular Equipment Calibration and Maintenance: Our centrifuges, microtomes, and other equipment are regularly calibrated and maintained to ensure accuracy and prevent errors. A poorly calibrated instrument is like using a faulty scale to measure ingredients in a recipe – the result is unpredictable.
- Internal Audits and Proficiency Testing: Regular internal audits assess adherence to protocols, while external proficiency testing ensures our results are comparable to other reputable labs. It’s akin to a chef regularly checking their cooking techniques against established standards.
Q 9. Describe your experience with embedding tissue samples in paraffin.
Paraffin embedding is a crucial step in tissue processing, preparing samples for microtomy. My experience includes embedding a wide range of tissue types, from small biopsies to large surgical specimens. The process typically involves:
- Tissue Cassette Labeling: The tissue sample is placed in a labeled cassette, ensuring accurate identification throughout the process.
- Tissue Processing: The tissue undergoes dehydration through a series of graded alcohols, followed by clearing with xylene or a xylene substitute, and finally infiltration with molten paraffin wax. This removes water and replaces it with a medium that allows for thin sectioning.
- Embedding: The paraffin-infiltrated tissue is carefully oriented in a mold with fresh paraffin, ensuring optimal sectioning. I use various techniques to ensure proper orientation depending on the tissue type and the region of interest.
- Cooling and Hardening: The mold is cooled, allowing the paraffin to solidify and create a tissue block ready for sectioning. Proper cooling prevents the formation of cracks or distortions.
I’ve dealt with numerous challenges, including challenging tissue types like bone or very fatty tissues, which require modified processing times and techniques to achieve optimal results. For example, decalcification might be necessary for bone samples before embedding.
Q 10. How do you ensure the safety and integrity of specimens during storage?
Maintaining the safety and integrity of specimens during storage is critical for preserving their quality and preventing contamination. This involves:
- Appropriate Storage Conditions: Specimens are stored in designated freezers or refrigerators at appropriate temperatures (-80°C for long-term storage, 4°C for short-term storage). Temperature monitoring systems are used to ensure consistency.
- Biohazard Safety Precautions: All specimens are handled following strict biohazard protocols, including the use of personal protective equipment (PPE) such as gloves and lab coats. Proper disposal procedures are followed for biohazardous waste.
- Inventory Management System: A well-organized inventory system allows for easy retrieval of samples while minimizing the risk of cross-contamination or damage. We use a computerized system with barcoded samples for accurate tracking.
- Regular Inspections: Regular inspections of storage areas and equipment help ensure that optimal conditions are maintained and that any issues are identified and resolved promptly.
Imagine the consequences of failing to maintain the cold chain – irreversible damage to the specimen could occur, rendering it unusable for analysis.
Q 11. What are the different types of stains used in histology and their applications?
Histology relies on various stains to visualize different cellular components. Here are some examples:
- Hematoxylin and Eosin (H&E): This is the most common stain, providing general tissue morphology. Hematoxylin stains nuclei blue/purple, while eosin stains cytoplasm pink/red.
- Periodic Acid-Schiff (PAS): Used to stain carbohydrates, including glycogen and mucin. It’s crucial for identifying fungal infections and certain types of tumors.
- Masson’s Trichrome: Distinguishes collagen from other tissue components, often used in fibrosis studies. It provides a clear differentiation between connective tissue and muscle.
- Silver stains: Used to detect microorganisms like bacteria and fungi, as well as nerve fibers.
- Immunohistochemical (IHC) stains: These stains utilize antibodies to identify specific proteins or antigens within the tissue, aiding in diagnosis of diseases and understanding cellular processes. This is a more advanced technique discussed in a later answer.
The choice of stain depends on the specific diagnostic question. For instance, if we suspect a fungal infection, we would use a PAS stain. If we are looking at liver fibrosis, Masson’s Trichrome stain is beneficial.
Q 12. Explain the process of microtomy and sectioning of tissue samples.
Microtomy is the process of cutting extremely thin sections of embedded tissue for microscopic examination. It involves using a microtome, a precision instrument capable of creating sections as thin as a few micrometers (µm).
- Tissue Block Preparation: The paraffin-embedded tissue block is trimmed to create a smooth surface for sectioning.
- Microtome Orientation: The block is carefully oriented in the microtome, ensuring the desired plane of sectioning.
- Sectioning: The microtome’s knife advances, slicing the tissue block into thin sections. The thickness is precisely controlled.
- Section Mounting: Sections are collected using a water bath and transferred onto glass slides.
- Drying and Staining: The sections are dried before undergoing staining procedures.
The skill lies in creating uniform, wrinkle-free sections that are thin enough for light to pass through yet thick enough to retain cellular detail. It requires practice and a keen eye for detail. Imagine trying to slice a very soft cheese thinly and evenly—it takes precision and steady hands.
Q 13. Describe your experience with immunohistochemistry (IHC) techniques.
Immunohistochemistry (IHC) is a powerful technique that allows for the visualization of specific proteins within tissues using antibodies. My experience encompasses various IHC protocols, including:
- Antibody Selection: Choosing the right antibody is crucial, as its specificity determines the accuracy of results. We consider factors such as antigen retrieval method and antibody concentration.
- Antigen Retrieval: Many antigens need to be unmasked to allow antibody binding. This usually involves heat-induced epitope retrieval (HIER) or enzymatic digestion.
- Antibody Incubation: The tissue sections are incubated with primary antibody, which binds to its target antigen. We use optimized incubation times and temperatures based on the antibody’s specifications.
- Detection System: Various detection systems (e.g., chromogenic or fluorescent) are used to visualize the antibody-antigen complexes. Chromogenic systems use enzymes to produce a colored reaction product, while fluorescent methods use fluorophores to create fluorescence.
- Counter Staining: A counterstain is usually applied to visualize the overall tissue morphology. H&E is a common choice.
I have experience in troubleshooting IHC issues, such as weak staining or non-specific background. This often requires optimization of the protocol or selection of a different antibody.
Q 14. What are the common artifacts encountered during specimen processing and how can they be avoided?
Several artifacts can arise during specimen processing, potentially leading to misinterpretation of results. These include:
- Tissue shrinkage and distortion: Caused by improper processing or dehydration. Careful attention to processing times and reagents can minimize this.
- Folding and tears: Occur during sectioning; skilled microtomy techniques and proper handling are necessary to avoid this.
- Precipitation of processing reagents: Can create background staining; using fresh reagents and meticulous cleaning of equipment prevent this.
- Air bubbles: Introduced during embedding or mounting; careful technique minimizes this.
- Fixative artifacts: Fixatives can induce artifacts; using appropriate fixatives and fixation times is key.
Preventing artifacts requires meticulous attention to detail at every stage of the process, from proper fixation and processing to skilled microtomy and staining techniques. Think of it as baking a cake – even small errors in the process can significantly impact the final result.
Q 15. Explain your understanding of different types of centrifuges and their applications.
Centrifuges are essential in specimen handling for separating components of a sample based on density. Different types cater to specific needs.
- Microcentrifuges: Small, low-speed centrifuges ideal for small volumes (e.g., PCR tubes, microtubes). I’ve used these extensively for separating serum from blood samples in clinical chemistry assays.
- Clinical Centrifuges: These are larger, often refrigerated, and can handle larger blood collection tubes. They’re vital for separating blood components like plasma or serum for various tests.
- High-Speed Centrifuges: Used for separating subcellular components like organelles or isolating specific proteins. Their higher speeds generate stronger centrifugal force. In my previous role, we used a high-speed centrifuge to isolate mitochondria for further biochemical analysis.
- Ultracentrifuges: These are the highest-speed centrifuges, capable of separating macromolecules like DNA or viruses. These are typically found in advanced research settings.
The choice of centrifuge depends entirely on the sample volume, desired separation resolution, and the nature of the components being separated. For instance, a microcentrifuge would be unsuitable for processing a large volume of blood required for blood bank testing, while an ultracentrifuge would be overkill for separating blood cells.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with cytological preparations, including smears and cell blocks.
Cytological preparations, such as smears and cell blocks, are crucial for microscopic examination of cells.
- Smears: These are made by spreading a cellular suspension thinly onto a slide. I have extensive experience preparing Pap smears for cervical cancer screening, where proper technique (even spreading, avoidance of artifacts) is critical for accurate diagnosis. The quality of the smear directly influences the clarity of the microscopic image.
- Cell Blocks: These are prepared from centrifuged cellular material, creating a tissue-like structure embedded in paraffin for sectioning. They’re particularly useful when dealing with fluids with low cellularity, allowing for easier handling and sectioning compared to smears. I’ve used this technique for processing body fluids like pleural effusions to identify malignant cells.
Both methods require meticulous attention to detail; proper fixation is essential to preserve cellular morphology and prevent degradation. I’ve always ensured adherence to standardized procedures to guarantee the quality and reliability of the cytological preparations.
Q 17. How do you troubleshoot issues related to poor tissue staining or inadequate sectioning?
Troubleshooting poor tissue staining or inadequate sectioning involves systematic investigation.
- Poor Staining: This can stem from several issues, including inadequate fixation (under-fixed or over-fixed tissue), improper staining technique (incorrect reagent concentrations, timing, or rinsing), or problems with the tissue itself (autolysis). My troubleshooting strategy begins with checking all steps meticulously; reviewing the fixation process, verifying staining protocols, and looking for any deviations from the SOPs.
- Inadequate Sectioning: This often arises from issues with tissue processing, embedding, or the microtome itself. Problems like insufficient paraffin infiltration (resulting in crumbly sections), improper orientation of the tissue block, or a dull blade can significantly impact section quality. I find checking the microtome blade sharpness and inspecting the tissue block for proper infiltration to be the first steps.
A systematic approach, coupled with a good understanding of the process involved, is crucial to identifying the root cause and implementing corrective actions. For example, if repeated poor staining is observed, we would review the reagents’ expiration dates, examine staining controls, and if necessary, repeat the staining procedure with a new batch of reagents.
Q 18. Explain the importance of following standard operating procedures (SOPs) in specimen handling.
Adherence to standard operating procedures (SOPs) in specimen handling is paramount for ensuring accuracy, reliability, and safety.
SOPs dictate every step, from specimen accessioning and labeling to processing, staining, and disposal. Following SOPs minimizes errors, prevents contamination, and maintains data integrity. For example, improper labeling can lead to misdiagnosis, while incorrect fixation can compromise the quality of the sample rendering it unsuitable for analysis. Furthermore, strict adherence to SOPs in handling biohazardous materials is crucial for protecting laboratory personnel from exposure to infectious agents. In my experience, deviations from SOPs are documented and thoroughly investigated to understand the cause and prevent recurrence, enhancing our continuous quality improvement efforts.
Q 19. Describe your experience with automated specimen processing equipment.
My experience includes working with automated tissue processors, embedding centers, and slide stainers.
Automated tissue processors significantly improve efficiency and consistency in tissue processing, reducing hands-on time and minimizing human error. I’m proficient in operating and maintaining these systems, troubleshooting technical issues such as reagent levels, system malfunctions, and ensuring optimal performance. Automated embedding centers greatly improve the speed and quality of paraffin embedding; while automated slide stainers help to standardize the staining process and optimize stain quality. They help maintain consistency and throughput, which are crucial for high-volume laboratories. I also have experience validating and optimizing automated equipment parameters to ensure optimal performance and quality.
Q 20. How do you manage the disposal of biohazardous waste generated during specimen handling?
Managing biohazardous waste is a critical aspect of specimen handling, requiring strict adherence to safety regulations.
All biohazardous waste generated during specimen handling, including contaminated sharps, tissues, fluids, and slides, is segregated according to local and national regulations. We use appropriate color-coded containers for different waste types and ensure proper labeling with biohazard symbols. I’ve been trained in proper waste handling protocols including double-bagging of contaminated items and the use of appropriate personal protective equipment (PPE). Disposal is coordinated with a licensed medical waste disposal company. All processes are documented according to regulatory requirements, ensuring compliance and minimizing risk to personnel and the environment.
Q 21. What is your experience with using different types of microscopy equipment?
My experience encompasses various microscopy techniques and equipment.
- Brightfield microscopy: This is the most commonly used technique for routine histopathological examination. I regularly use brightfield microscopes for assessing tissue architecture, cellular morphology, and staining quality.
- Fluorescence microscopy: I have experience using fluorescence microscopes for immunofluorescence studies, identifying specific proteins or cellular components using fluorescently labeled antibodies. This is crucial for more specialized diagnostic procedures.
- Polarizing microscopy: This is vital for identifying birefringent materials such as crystals or certain types of fibers. This is particularly useful in forensic pathology or for identifying specific types of crystals in biological samples.
Proficiency in using these different microscopy techniques and interpreting the generated images is crucial for accurate diagnosis and research. My experience includes troubleshooting issues associated with each type of microscopy, including optimization of illumination, image capture, and image analysis software.
Q 22. Explain the principles of quality assurance and quality control in a laboratory setting.
Quality assurance (QA) and quality control (QC) are crucial for ensuring the reliability and accuracy of laboratory results. QA focuses on the overall processes and systems to prevent errors, while QC focuses on the individual tests and procedures to detect and correct errors. Think of QA as building a sturdy house (the process), and QC as regularly inspecting the foundation and walls (the individual steps) to make sure it remains stable and sound.
- QA in a lab setting involves establishing standardized operating procedures (SOPs), regular equipment calibration and maintenance, proficiency testing (comparing results with other labs), and auditing processes to ensure compliance with regulations and best practices. For example, we might implement a system for tracking reagent lot numbers and expiration dates to ensure we’re always using appropriate materials.
- QC in a lab setting involves running control samples alongside patient samples. These controls are materials with known values, and their results should fall within an acceptable range. If the controls are outside the range, it indicates a potential problem with the test or the equipment, alerting us to investigate further and potentially correct any issues before processing patient samples. A QC chart helps us visually track these results over time and spot trends.
Both QA and QC are essential for maintaining the credibility of the laboratory and ensuring patient safety. They work together to create a system of checks and balances.
Q 23. How do you maintain a clean and organized work environment in the laboratory?
Maintaining a clean and organized lab environment is paramount for accuracy, safety, and efficiency. It minimizes the risk of contamination and accidents, and improves workflow. Imagine a cluttered kitchen – you’d struggle to find ingredients and increase the risk of spills and accidents. A lab is similar.
- Regular Cleaning: Daily cleaning involves wiping down benches, equipment, and centrifuges with appropriate disinfectants. Weekly cleaning might include more thorough cleaning of floors and less frequently used areas.
- Organized Storage: Reagents, supplies, and equipment should be stored systematically, labeled clearly, and dated for easy access and tracking. We use a color-coded system in our lab to quickly identify different types of reagents and their locations.
- Waste Disposal: Proper waste disposal protocols must be strictly followed. This includes segregating different types of waste (e.g., sharps, chemical waste, biohazardous waste) and using appropriate containers.
- 5S Methodology: Implementing the 5S methodology (Sort, Set in Order, Shine, Standardize, Sustain) can create a more structured and efficient work environment. This framework helps establish consistent practices for maintaining cleanliness and organization.
The emphasis is always on preventing contamination and ensuring a safe working space for everyone.
Q 24. Describe your experience with inventory management of reagents and supplies.
Effective inventory management of reagents and supplies is critical for avoiding shortages, reducing waste, and ensuring timely testing. I’ve extensive experience using a combination of manual and computerized systems. Think of it as managing a well-stocked pantry – you need the right ingredients in the right amounts at the right time.
- Inventory Tracking: I’m proficient in using inventory management software to track reagent lot numbers, expiry dates, quantities on hand, and usage rates. This data helps us to predict and schedule orders to avoid running out of essential supplies.
- Stock Rotation: We follow a ‘first-in, first-out’ (FIFO) system to ensure that older reagents are used before newer ones, minimizing the risk of expiry.
- Ordering and Procurement: I’m experienced in collaborating with procurement departments to place timely orders, negotiate favorable pricing, and maintain adequate stock levels.
- Waste Reduction: We actively monitor reagent usage and identify areas where we can optimize processes to reduce waste and improve cost-effectiveness.
Through meticulous tracking and proactive management, we ensure that our laboratory is always well-equipped to provide accurate and timely results.
Q 25. How do you handle emergency situations involving specimen spills or contamination?
Emergency situations, such as specimen spills or contamination, require immediate and decisive action to minimize risk and prevent further problems. My training emphasizes safety protocols and rapid response. We treat every spill as a potential biohazard.
- Specimen Spills: In the event of a specimen spill, the immediate priority is to contain the spill using absorbent materials. Then, we use appropriate disinfectants to decontaminate the area according to established safety protocols. All personnel involved must follow appropriate personal protective equipment (PPE) guidelines.
- Contamination Incidents: If contamination is suspected, we immediately isolate the affected area and notify the appropriate personnel, such as the laboratory supervisor and infection control officer. We’ll conduct a thorough investigation to determine the source of contamination and implement corrective actions to prevent recurrence.
- Documentation: All incidents, including the steps taken to address them, are thoroughly documented in an incident report. This report serves as a record for review and future improvement.
Following established protocols is crucial in managing emergency situations and ensuring the safety of personnel and the integrity of the laboratory environment.
Q 26. What are your skills in using laboratory information systems (LIS)?
I possess extensive experience using Laboratory Information Systems (LIS). These systems are the backbone of modern laboratories, streamlining workflows and improving data management. Think of an LIS as a sophisticated organizational tool for all laboratory data.
- Data Entry and Management: I’m proficient in entering patient demographics, test requests, and results accurately and efficiently into the LIS. I’m also skilled in retrieving and interpreting data from the system for various purposes, including quality control analysis and reporting.
- Specimen Tracking: LIS helps us effectively track specimens throughout the testing process, from accessioning to reporting. This minimizes the risk of errors and delays.
- Reporting and Analysis: I utilize LIS features to generate reports on various metrics, including turnaround time, test volumes, and quality control data. This aids in performance monitoring and identification of areas for improvement.
- System Troubleshooting: I’m capable of troubleshooting common LIS issues and seeking assistance when necessary. Understanding the system’s limitations and seeking help when needed is crucial.
My expertise in LIS ensures that the laboratory operates efficiently and produces reliable, timely results.
Q 27. Explain your experience with documenting procedures and results accurately.
Accurate documentation is essential for maintaining the integrity and credibility of laboratory results. It’s the foundation of traceability and accountability within the lab. Imagine trying to reconstruct a recipe without clear instructions – it’s crucial to have detailed and accurate steps recorded.
- SOP Adherence: I strictly follow standardized operating procedures (SOPs) when documenting procedures and results. This ensures consistency and accuracy.
- Detailed Record Keeping: My documentation includes all relevant information, such as patient identifiers, test requests, reagents used, results, and any observations or deviations from the SOPs. All entries are meticulously dated and time-stamped.
- Legible Handwriting/Typing: Whether handwritten or computerized, my documentation is always legible and easily understandable. Clear documentation minimizes the risk of misinterpretations or errors.
- Error Correction: If an error occurs, I correct it appropriately, ensuring that the correction is clearly marked and the original entry remains visible. We never erase or obliterate original entries.
Precise and complete documentation is critical to avoid ambiguity, and it protects both the laboratory and the patients.
Q 28. Describe a situation where you had to solve a problem related to specimen handling.
In one instance, we experienced a significant delay in receiving test results for a critical patient sample due to a malfunctioning centrifuge. This posed a challenge as the timely results were crucial for the patient’s treatment.
- Problem Identification: We immediately identified the malfunctioning centrifuge as the source of the delay. After initial troubleshooting, we confirmed it required professional repair.
- Solution Implementation: We implemented a two-pronged approach: First, we immediately sent the samples to a backup centrifuge at a nearby reference laboratory for processing, ensuring results were obtained in a timely manner. Second, we initiated the repair of the faulty centrifuge by contacting a qualified technician, ensuring its availability as quickly as possible.
- Lessons Learned: This incident highlighted the importance of having a robust contingency plan in place to handle equipment malfunctions. We subsequently implemented regular preventative maintenance checks for all our centrifuges to minimize the risk of future incidents.
This experience taught me the importance of quick thinking, resourcefulness, and thorough preventative maintenance to minimize disruptions and ensure patients receive prompt, accurate results.
Key Topics to Learn for Specimen Handling and Preparation Interview
- Specimen Integrity and Chain of Custody: Understanding and maintaining the integrity of specimens from collection to analysis, including proper labeling, storage, and transportation. This includes knowing legal and regulatory requirements for maintaining chain of custody.
- Specimen Accessioning and Processing: Practical application of accessioning procedures, including data entry, verification, and sample preparation techniques. This involves understanding the importance of accurate data recording and minimizing pre-analytical errors.
- Aseptic Techniques and Safety Protocols: Understanding and applying aseptic techniques to prevent contamination and ensure safety. This includes proper handling of biohazardous materials and adherence to relevant safety regulations and guidelines.
- Common Specimen Types and Handling Requirements: Knowledge of different specimen types (blood, urine, tissue, etc.) and their specific handling requirements, including appropriate collection containers, processing methods, and storage conditions.
- Quality Control and Quality Assurance: Understanding the importance of quality control measures in ensuring accurate and reliable results. This includes proficiency in using quality control materials and interpreting quality control data.
- Troubleshooting and Problem-Solving: Developing the ability to identify and address common problems encountered during specimen handling and preparation, such as hemolysis, inadequate sample volume, or contamination. This may involve understanding root cause analysis and implementing corrective actions.
- Instrumentation and Technology: Familiarity with common laboratory equipment used in specimen handling and preparation, including centrifuges, automated analyzers, and other relevant technologies. This also involves understanding basic troubleshooting for common instrument malfunctions.
Next Steps
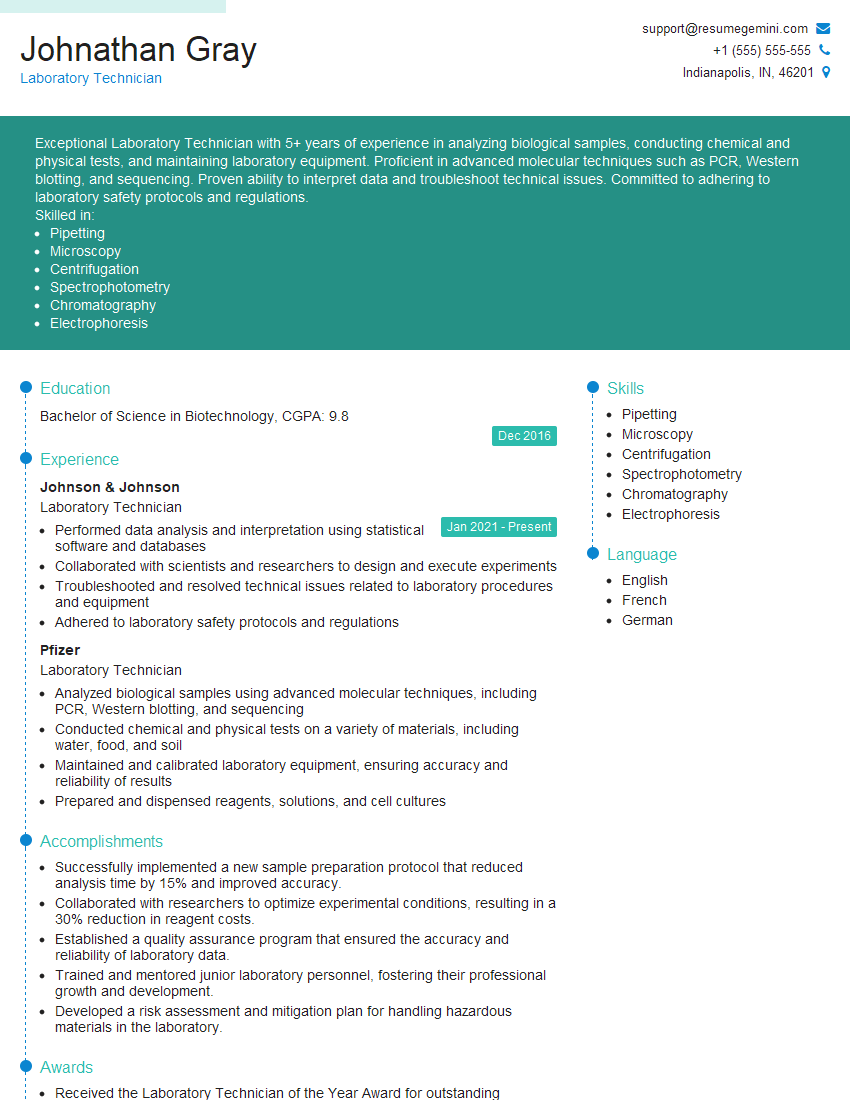
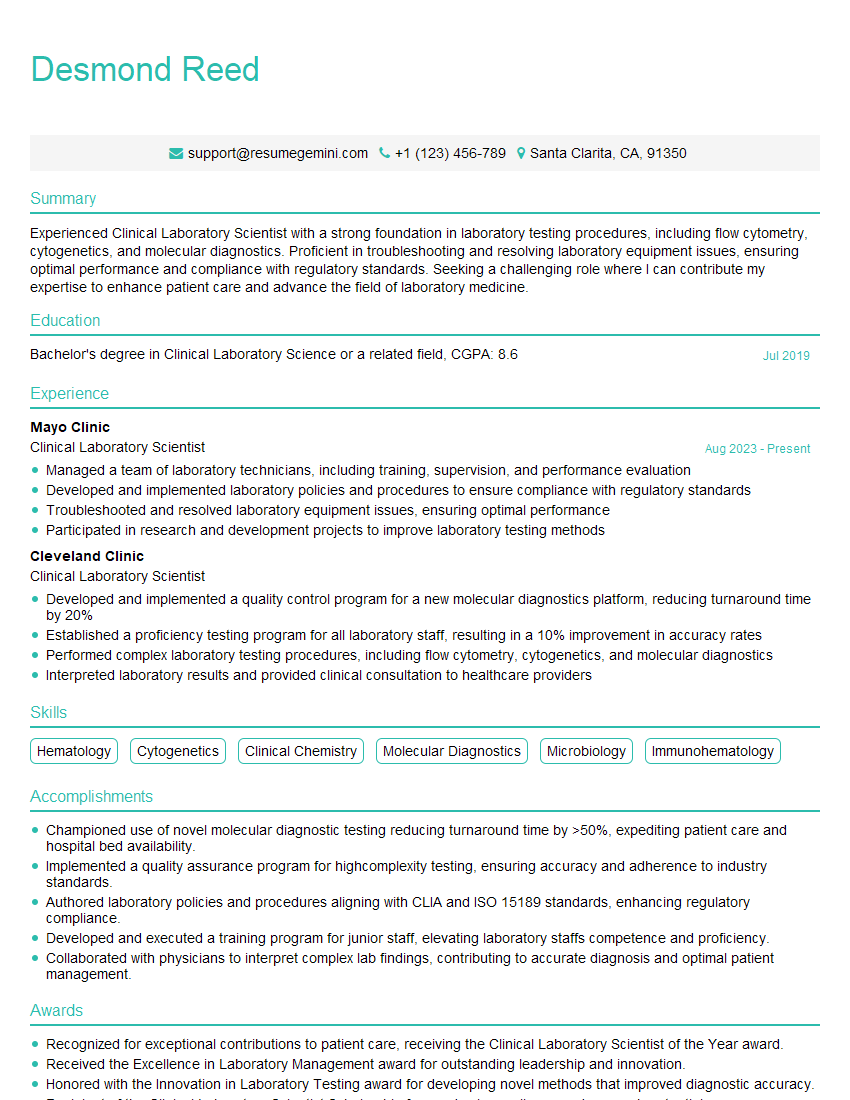
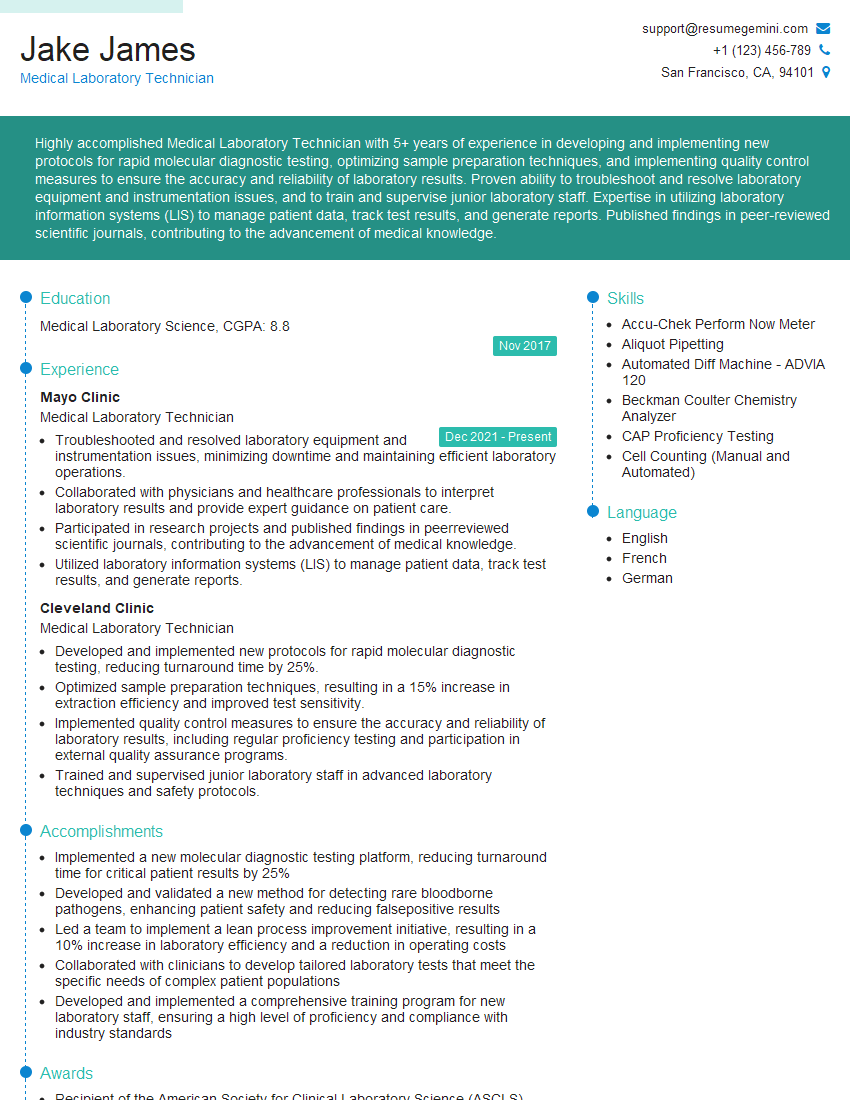
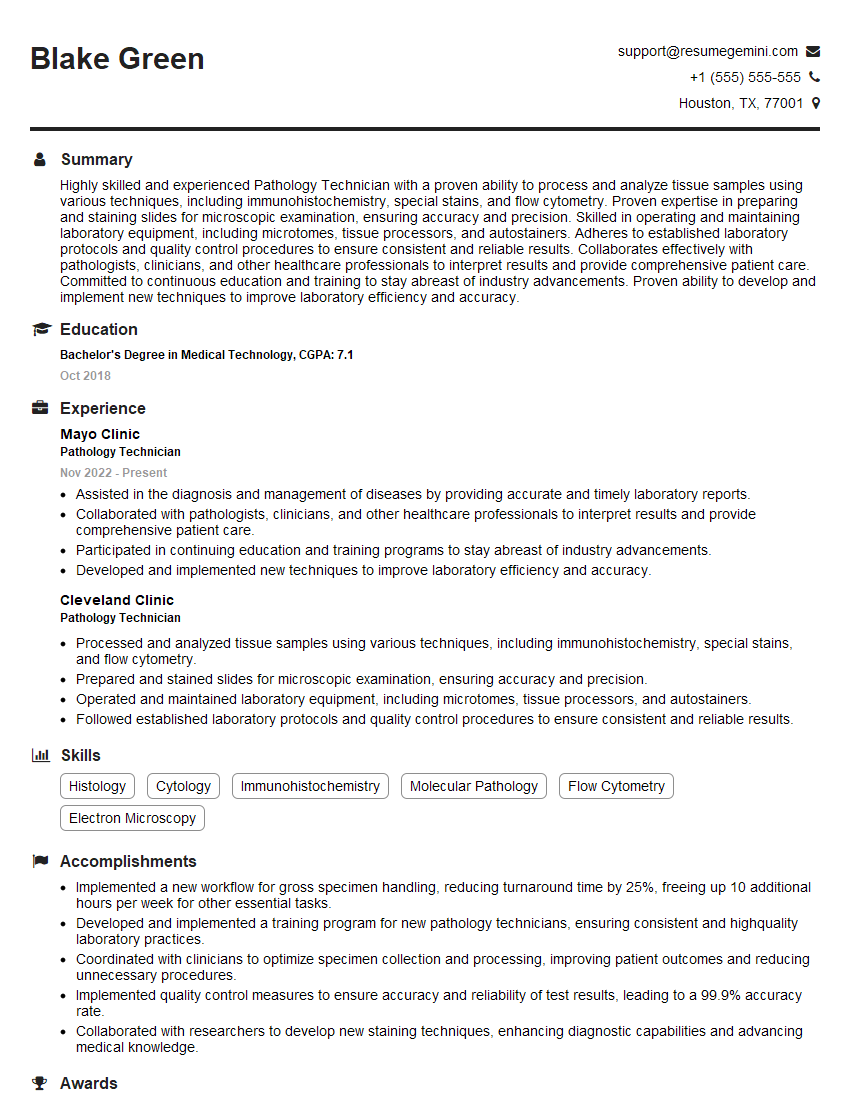
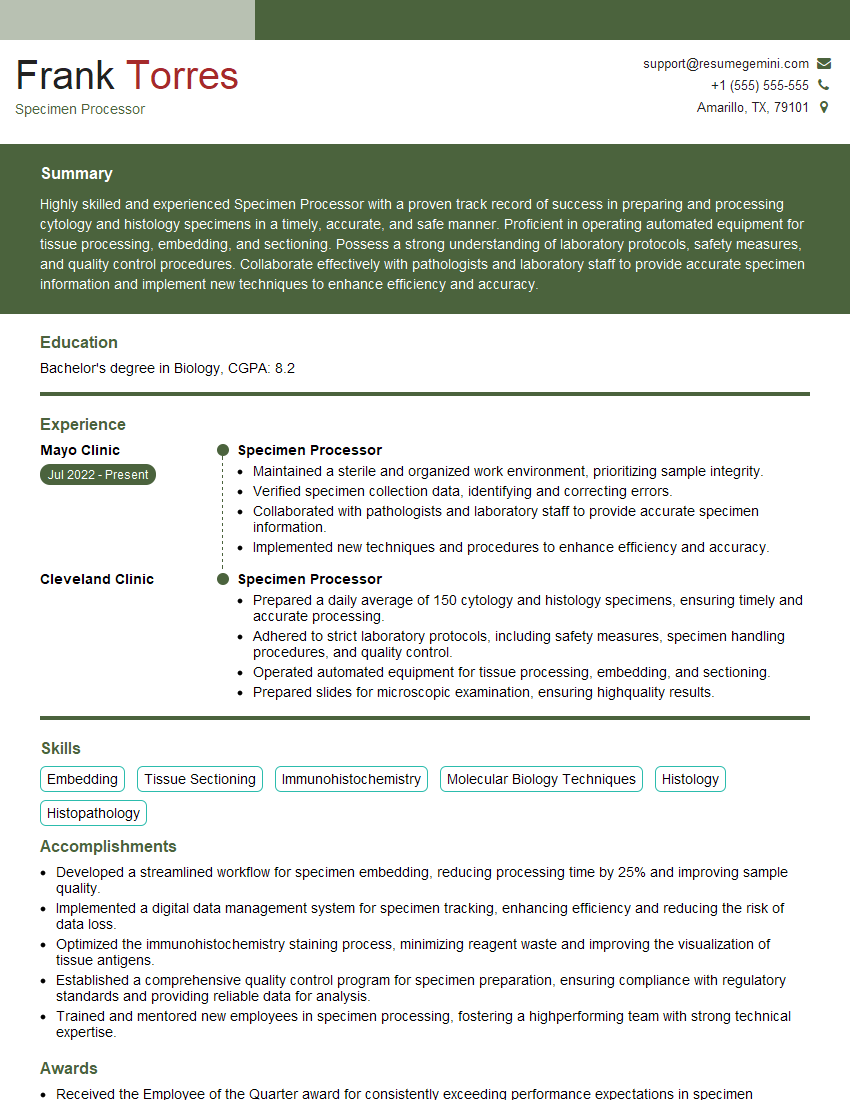
Mastering Specimen Handling and Preparation is crucial for career advancement in the medical laboratory field. A strong foundation in these techniques demonstrates your commitment to accuracy, patient safety, and reliable results. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume that stands out to recruiters. Examples of resumes tailored to Specimen Handling and Preparation are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.