Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Spine Imaging interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Spine Imaging Interview
Q 1. Describe the differences between T1-weighted and T2-weighted MRI images of the spine.
T1-weighted and T2-weighted MRI images provide different contrasts of the spine, highlighting different tissue properties. Think of it like taking two different photographs of the same scene, using different lighting and filters to emphasise specific details.
T1-weighted images show good anatomical detail. Fat appears bright (high signal intensity), while water and cerebrospinal fluid (CSF) appear dark (low signal intensity). Bone marrow is also bright. This makes them excellent for visualizing the anatomy of the spine, including vertebrae, discs, and spinal cord.
T2-weighted images are more sensitive to water content. Water and CSF appear bright, while fat appears dark. This makes them ideal for detecting edema (swelling), inflammation, and lesions involving fluid accumulation, such as tumors or disc herniations.
Example: In a case of a disc herniation, T2-weighted images would better show the herniated disc material as bright against the darker background of the spinal canal, whereas a T1-weighted image might show the disc as slightly less bright or isointense, making the herniation less conspicuous.
Q 2. Explain the imaging findings characteristic of degenerative disc disease.
Degenerative disc disease (DDD) is a common age-related condition affecting the intervertebral discs. Imaging findings reflect the progressive breakdown of the disc’s structure and function.
- Disc Dehydration: On MRI, this shows as a decrease in disc height and a reduction in signal intensity on T2-weighted images, indicating loss of water content. The disc appears flatter and less hydrated than normal.
- Disc Bulging or Protrusion: The disc material may bulge beyond the normal confines of the vertebral bodies. This is visible on both T1 and T2-weighted images, often associated with low back pain.
- Disc Herniation: This is a more significant displacement of disc material beyond the confines of the vertebral body, potentially compressing nerve roots or the spinal cord. This is clearly seen on MRI as a fragment of the disc pushed out, causing further pain and potentially nerve damage.
- Osteophyte Formation: Bone spurs (osteophytes) may form along the edges of the vertebral bodies, a common compensatory response to disc degeneration. These appear as bony projections on both MRI and X-rays.
- Endplate Changes: Modic changes, for instance, are bone marrow changes within the vertebral endplates (the bony surfaces of the vertebrae adjacent to the disc), visible on T1-weighted MRI, suggesting inflammation and bone remodeling.
In Summary: DDD imaging features often include a combination of reduced disc height, signal intensity changes, bulging or herniation, osteophytes, and endplate changes. The specific findings help determine the severity and location of the degeneration.
Q 3. Differentiate between spondylolysis and spondylolisthesis on imaging.
Spondylolysis and spondylolisthesis are related conditions affecting the vertebrae, most commonly in the lumbar spine.
Spondylolysis refers to a defect or fracture in the pars interarticularis, a small segment of bone connecting the superior and inferior articular processes of a vertebra. Imagine it as a crack or break in this specific area. On imaging (usually X-ray or CT), this appears as a lucency (dark area) across the pars interarticularis, often described as a ‘Scottie dog’ defect on an oblique X-ray view.
Spondylolisthesis is the forward slippage of one vertebra over the vertebra below it. This often (but not always) follows spondylolysis, where the fracture allows for the slippage. On imaging, it shows as anterior displacement of the affected vertebra compared to the vertebra immediately below it. The degree of slippage is graded depending on the extent of anterior displacement.
In Summary: Spondylolysis is a fracture in the pars interarticularis; spondylolisthesis is the forward slippage of a vertebra, often a consequence of spondylolysis, but can occur due to other causes.
Q 4. How would you interpret imaging findings suggestive of spinal stenosis?
Spinal stenosis is a narrowing of the spinal canal, reducing space for the spinal cord and nerve roots. Imaging findings depend on the location (central canal, lateral recess, foraminal) and the cause of the stenosis.
- Narrowing of the Spinal Canal: On MRI or CT, the anteroposterior (AP) diameter of the spinal canal is reduced. Measurements are often compared to normative values.
- Foraminal Stenosis: Narrowing of the neural foramina (openings where nerve roots exit) compresses the nerve roots. This is commonly seen in the lateral recess.
- Disc Bulging or Herniation: These can directly compress the spinal cord or nerve roots, contributing to stenosis.
- Osteophyte Formation: Bone spurs from DDD can further reduce the space within the spinal canal.
- Ligamentum Flavum Thickening: The ligamentum flavum (a ligament supporting the spine) may thicken and bulge into the spinal canal.
- Facet Joint Hypertrophy: Enlargement of the facet joints (where vertebrae articulate) can encroach upon the spinal canal.
Interpretation: The combination of these findings on imaging guides diagnosis. The severity of stenosis is assessed by the degree of narrowing and its impact on the spinal cord and nerve roots. Coronal and sagittal reformats on MRI are particularly useful in evaluating the extent and location of the stenosis.
Q 5. What are the imaging features of a spinal fracture?
Imaging findings of spinal fractures vary widely depending on the type and severity of the fracture.
- Fracture Line: A visible line of discontinuity in the bone, seen clearly on X-rays and CT scans.
- Bone Fragmentation: The bone may be fragmented into multiple pieces, evident on CT scans.
- Displacement: The fractured bone segments may be displaced from their normal position, often associated with greater instability and pain.
- Vertebral Compression: The vertebral body may be compressed, losing height, as seen in compression fractures.
- Subluxation: Partial dislocation of one vertebra relative to another, indicating potential instability.
- Edema: MRI can demonstrate bone marrow edema (swelling) around the fracture site, indicating inflammation and bone healing.
- Paraspinal Hematoma: A collection of blood outside the vertebra can be seen on CT or MRI.
Important Note: MRI provides better soft tissue detail, showing edema and hematomas, while CT is superior for assessing the bone itself. X-rays are often the initial imaging modality for evaluating spinal trauma but may miss subtle fractures.
Q 6. Describe the imaging techniques used to evaluate spinal cord compression.
Evaluating spinal cord compression involves a multi-modal approach, leveraging the strengths of different imaging techniques.
- MRI: This is the primary imaging modality for evaluating spinal cord compression. It provides excellent soft tissue contrast, clearly visualizing the spinal cord, its surrounding tissues, and any compression from bone, disc herniations, tumors, or hematomas. Both T1 and T2-weighted images, along with specialized sequences such as STIR (Short Tau Inversion Recovery) and FLAIR (Fluid Attenuated Inversion Recovery) provide valuable information on the nature and extent of compression.
- CT Myelography: This technique is used when MRI is contraindicated (e.g., presence of metallic implants) or when additional information beyond MRI is required. It involves injecting contrast material into the spinal canal, followed by CT imaging, resulting in detailed visualization of the spinal cord and nerve roots. It can better delineate the extent and location of compression in certain situations.
- CT Scan: CT excels at visualizing bone, making it useful to assess the bony anatomy in cases of fractures, stenosis, or other bone abnormalities contributing to cord compression. CT myelography can be helpful in clarifying spinal cord compression.
In Practice: The choice of imaging technique depends on the clinical suspicion, patient factors, and the availability of equipment. Often, MRI is the first line of investigation for suspected spinal cord compression, but CT myelography can play a valuable supplementary role.
Q 7. Explain the role of CT myelography in spine imaging.
CT myelography combines the advantages of CT’s excellent bone detail with the ability to visualize the spinal cord and nerve roots using contrast material. Think of it as a powerful combination that allows for the most detailed visualization of the spinal canal contents.
Procedure: A small amount of iodinated contrast material is injected into the subarachnoid space (the space surrounding the spinal cord). CT scanning then creates images demonstrating the distribution of contrast within the spinal canal and its relationship to surrounding structures. This offers superior visualization compared to conventional CT in evaluating certain conditions.
Clinical Applications: CT myelography is especially useful in situations where MRI might be limited or inconclusive such as:
- Patients with metallic implants: Metallic implants can cause significant artifacts on MRI, obscuring the view of the spinal cord.
- Evaluating subtle or complex pathologies: CT myelography can provide more detailed visualization of subtle compression of the spinal cord or nerve roots.
- Cases of suspected spinal cord or nerve root injury: This technique can be helpful in visualizing injury patterns which are not clearly visible on other imaging modalities.
- Post-operative assessment: It can aid in assessing the surgical outcome and identifying any complications.
Limitations: It’s an invasive procedure with potential risks associated with the injection of contrast material. MRI remains the preferred modality in most cases due to its non-invasive nature and superior soft tissue contrast.
Q 8. What are the indications for MRI of the cervical spine?
Magnetic Resonance Imaging (MRI) of the cervical spine is indicated for a wide range of conditions affecting the neck and upper spine. Essentially, whenever we need detailed visualization of the soft tissues – including the spinal cord, intervertebral discs, ligaments, and muscles – MRI is a powerful tool.
- Neck pain and radiculopathy: MRI helps identify the source of pain, such as a herniated disc compressing a nerve root, causing pain radiating down the arm (radiculopathy).
- Trauma: After a neck injury, MRI assesses for fractures, ligamentous injuries (whiplash), spinal cord contusions, or hematomas.
- Spinal cord compression: MRI is crucial in detecting tumors, inflammation, or degenerative changes that might be compressing the spinal cord, potentially leading to neurological deficits.
- Inflammatory conditions: Conditions like multiple sclerosis or cervical spondylitis (inflammation of the spine) are well visualized on MRI.
- Degenerative changes: Osteoarthritis, spondylosis (degenerative changes of the vertebrae), and spinal stenosis (narrowing of the spinal canal) can be assessed effectively using MRI.
- Pre-surgical planning: MRI provides detailed anatomical information essential for planning surgical procedures, such as spinal fusion or discectomy.
For example, a patient presenting with persistent neck pain and weakness in their right arm might undergo a cervical spine MRI to rule out a cervical disc herniation affecting the nerve root at C6-C7. The high resolution of MRI allows for precise localization of the herniation and assessment of its impact on the neural structures.
Q 9. Discuss the use of discography in diagnosing spine pathologies.
Discography is a specialized imaging technique used to assess the internal structure and integrity of intervertebral discs. It involves injecting contrast material directly into the disc under fluoroscopic guidance. While less frequently used now due to the advancement of MRI, it holds a niche role in diagnosing certain conditions.
Indications: Discography is primarily used when MRI findings are inconclusive or when there’s a suspicion of discogenic pain (pain originating from the disc itself) that isn’t well-explained by other imaging modalities. It’s often used to evaluate patients with chronic low back pain that hasn’t responded to conservative treatment.
Mechanism: The injected contrast highlights the internal structure of the disc, revealing internal tears, fissures, or annular disruptions. The procedure also assesses the patient’s pain response to the injection. If injecting into a damaged disc reproduces the patient’s pain, it supports the diagnosis of discogenic pain.
Limitations: Discography is an invasive procedure with potential risks including infection and bleeding. It’s also subjective as pain response can vary between individuals. MRI is generally preferred as the first-line imaging modality due to its non-invasive nature and ability to comprehensively visualize the entire spine and surrounding structures.
Imagine a patient with persistent low back pain despite negative MRI findings. Discography could be considered to definitively determine if a specific disc is the source of their pain. However, the decision to perform discography should be made carefully, weighing the potential benefits against the risks involved.
Q 10. How would you differentiate between an infection and tumor in the spine on imaging?
Differentiating between spinal infections and tumors on imaging can be challenging, requiring careful analysis of various imaging characteristics. Both can present with similar features like bone destruction, soft tissue masses, and spinal cord compression.
- Location: Infections often involve the vertebral bodies (the main part of the vertebra), while tumors can be located in the vertebral body, the pedicles (the bony bridges connecting the body to the posterior elements), the neural arches, or even extradural (outside the spinal canal) spaces.
- Appearance: Infections often show irregular bone destruction with a characteristic “moth-eaten” appearance, possibly with associated abscess formation (a collection of pus). Tumors might show more well-defined or aggressive bone destruction, with varying degrees of expansion and soft tissue involvement. MRI is crucial to assess soft tissue involvement.
- Signal characteristics on MRI: Infections typically demonstrate increased signal intensity (brighter appearance) on T2-weighted MRI images due to fluid and edema. The signal intensity on MRI varies depending on the type of tumor, but they may exhibit different enhancement patterns with contrast.
- Contrast enhancement: Both infections and tumors typically show contrast enhancement after administering intravenous contrast, but the pattern of enhancement may differ. Infections often exhibit ring-like or rim enhancement, while tumors may demonstrate heterogeneous (irregular) or homogenous (uniform) enhancement.
Advanced imaging techniques like PET-CT scans can be helpful in distinguishing between infection and tumor, as they can assess metabolic activity. Infections will generally show increased metabolic activity, while the metabolic activity of tumors is variable.
For example, a patient with fever and back pain might have imaging showing bone destruction in the vertebral body. The presence of an associated abscess on MRI, along with the patient’s clinical presentation, would strongly suggest a spinal infection. Conversely, a patient with a slowly growing mass causing spinal cord compression without associated inflammatory signs would likely raise suspicion for a spinal tumor.
Q 11. What are the limitations of plain radiography in evaluating spinal pathology?
Plain radiography, while a readily available and cost-effective initial imaging modality, has significant limitations in evaluating spinal pathology. Its primary drawback is its limited ability to visualize soft tissues.
- Poor soft tissue visualization: Plain radiographs primarily show bone and cannot effectively visualize intervertebral discs, spinal cord, ligaments, or muscles. This limits its ability to detect soft tissue injuries like herniated discs, ligamentous tears, or spinal cord compression.
- Limited sensitivity for early changes: Early stages of degenerative changes, fractures, or infections may not be readily apparent on plain radiographs as significant bone destruction or structural changes are often required before they become visible.
- Overlapping structures: Overlapping bony structures can obscure subtle findings, making it difficult to interpret images accurately.
- Radiation exposure: While the radiation dose is relatively low, repeated radiographs expose patients to cumulative radiation, which carries some risk.
For instance, a patient with a herniated disc might have a normal plain radiograph even if they have significant back pain and neurological deficits because the herniated disc itself isn’t directly visualized on a radiograph. Plain radiographs are better at identifying fractures, advanced degenerative changes and bony alignment abnormalities.
Q 12. Describe the advantages and disadvantages of different spine imaging modalities.
Several imaging modalities are used to assess spinal pathology, each with its own advantages and disadvantages:
- Plain radiography:
- Advantages: Readily available, inexpensive, low radiation dose.
- Disadvantages: Poor soft tissue visualization, limited sensitivity for early changes.
- Computed Tomography (CT):
- Advantages: Excellent bone detail, can detect subtle fractures, good for assessing bony alignment.
- Disadvantages: Lower soft tissue contrast compared to MRI, higher radiation dose than radiography.
- Magnetic Resonance Imaging (MRI):
- Advantages: Excellent soft tissue contrast, superior visualization of discs, spinal cord, and other soft tissues. No ionizing radiation.
- Disadvantages: More expensive than radiography and CT, longer scan times, contraindicated in patients with some metallic implants or claustrophobia.
- Myelography: (Contrast injection into the spinal canal)
- Advantages: Can be helpful in visualizing the spinal cord and nerve roots, particularly in cases of severe spinal stenosis or where MRI is contraindicated.
- Disadvantages: Invasive procedure with potential risks of complications, not routinely used due to the availability of MRI.
The choice of imaging modality depends on the clinical question, the patient’s medical history, and the availability of resources. For example, initial evaluation of acute trauma might start with plain radiographs followed by CT if fractures are suspected. For suspected herniated discs or spinal cord compression, MRI is usually preferred.
Q 13. How would you interpret imaging findings consistent with a herniated disc?
Imaging findings consistent with a herniated disc vary depending on the location and severity of the herniation. MRI is the best modality for visualizing herniated discs.
- Disc bulge: A disc bulge refers to a uniform, circumferential displacement of the disc beyond the borders of the vertebral body. On MRI, this appears as a gentle widening of the disc space with no focal protrusion.
- Disc protrusion: A disc protrusion is a localized outward displacement of the disc material beyond the borders of the vertebral body, but still attached to the disc. On MRI, it appears as a focal outward extension of the disc material, maintaining some connection to the parent disc.
- Disc extrusion: In disc extrusion, the disc material extends beyond the borders of the vertebral body, but the outer annulus fibrosus remains intact. On MRI, this shows a focal displacement of disc material that is not directly attached to the main disc.
- Disc sequestration: This represents a complete separation of the disc material from the parent disc. It appears as a fragment of disc material completely separated and free in the spinal canal on MRI.
In addition to the disc itself, MRI also assesses for nerve root compression. Compression is indicated by the displacement or flattening of the nerve root, which may be seen on MRI axial or sagittal images.
For example, an MRI might show a large disc extrusion at L4-L5, compressing the exiting L5 nerve root, consistent with the patient’s complaints of low back pain radiating down the leg. The size, location, and degree of nerve root compression guide clinical management.
Q 14. What is the role of advanced imaging techniques like diffusion-weighted imaging (DWI) in spinal pathologies?
Advanced imaging techniques, such as diffusion-weighted imaging (DWI), play a crucial role in evaluating spinal pathologies, particularly in the context of acute injury and infection.
DWI: DWI measures the movement of water molecules in tissues. In areas of inflammation or cell death (necrosis), the movement of water molecules is restricted, resulting in a bright signal on DWI images. This increased signal intensity allows for early detection of changes before they become morphologically apparent on conventional MRI sequences.
- Spinal cord injury: DWI is sensitive to the extent and location of acute spinal cord injury, identifying areas of ischemia (reduced blood flow) or contusion. Early detection allows for timely intervention.
- Spinal infections: DWI effectively detects inflammatory changes associated with spinal infections, showing increased signal intensity in the involved areas, even before significant bone changes occur on other sequences. This helps in early diagnosis and appropriate treatment.
- Tumors: While DWI is not routinely used for tumor characterization in the spine, the restricted diffusion in certain tumor types can contribute to diagnostic certainty.
For example, a patient who sustains a spinal cord injury might undergo an MRI with DWI sequences to determine the extent and location of the injury. A bright signal on DWI indicates areas of damaged tissue, allowing for better prognostication and treatment planning. Similarly, DWI could help differentiate early-stage spinal infection from other conditions with similar imaging findings.
Q 15. Explain the significance of signal changes on MRI in spinal cord injury.
Signal changes on MRI in spinal cord injury are crucial for assessing the extent and severity of the damage. Different signal intensities on T1-weighted and T2-weighted images reflect various stages of injury and tissue changes.
- Immediately after injury: You might see edema (swelling), appearing as high signal intensity (bright) on T2-weighted images and potentially low signal (dark) on T1-weighted images, reflecting the presence of water. This indicates acute injury and tissue disruption.
- Subacute phase: As the injury evolves, there might be a transition to a more heterogeneous signal pattern with areas of hemorrhage (bleeding) that may show high signal intensity on both T1 and T2 weighted images. This is followed by the development of gliosis and cystic changes that can appear as areas of increased signal on T2-weighted images.
- Chronic phase: In the long term, you might observe atrophy (shrinkage) of the spinal cord, appearing as a decrease in cord size and potentially focal areas of low signal intensity on T1-weighted images. This reflects permanent damage.
Imagine it like this: T2-weighted images are like a wet sponge – they highlight the fluid, and swelling or bleeding shows up brightly. T1-weighted images are like a dry sponge – they show the tissues more directly, and bleeding may be visible as bright signals in chronic cases.
Precise signal characteristics help guide treatment decisions. For example, the presence of significant edema might indicate a need for early surgical decompression to reduce pressure on the spinal cord.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the imaging features of spinal metastases.
Spinal metastases, or cancer spread to the spine, typically present with characteristic imaging features on MRI and CT scans. These features can help differentiate metastases from other spinal pathologies.
- Lytic lesions: These are bone-destructive lesions which appear as areas of decreased density on CT scans and show low signal intensity on T1-weighted MRI and high signal intensity on T2-weighted MRI. They essentially ‘eat away’ at the bone.
- Blastic lesions: These lesions are associated with increased bone density, appearing as areas of increased density on CT and possibly low signal intensity on both T1 and T2 weighted MRI scans. They are characterized by increased bone formation.
- Mixed lesions: Many spinal metastases show a combination of lytic and blastic features.
- Soft tissue involvement: Metastases often extend into the surrounding soft tissues, such as the spinal cord, epidural space, or paraspinal muscles. This soft tissue involvement appears as abnormal masses or areas of increased signal on T2-weighted MRI.
- Cord compression: Spinal cord compression is a significant complication of spinal metastases. This manifests as a narrowing of the spinal canal and direct compression of the cord, which can result in neurological deficits.
For example, a patient presenting with back pain and neurological symptoms may undergo an MRI revealing a lytic lesion in the vertebral body with accompanying soft tissue mass causing spinal cord compression. This imaging finding would be highly suggestive of spinal metastasis requiring immediate evaluation by an oncologist and potentially radiation therapy or surgery.
Q 17. How would you evaluate the stability of a spinal fracture on imaging?
Assessing the stability of a spinal fracture on imaging requires careful evaluation of multiple factors to determine whether the fracture is likely to lead to further displacement or neurological compromise.
- Fracture Disruption: Look for the presence of complete or incomplete vertebral body fracture, the degree of comminution (fragmentation), and posterior element involvement (pedicles, laminae, spinous processes). Significant disruption of the posterior elements suggests instability.
- Ligamentous Injury: Assess the integrity of the anterior and posterior longitudinal ligaments, interspinous and supraspinous ligaments. MRI is superior to CT for visualizing ligamentous injuries. Tears or disruptions suggest instability.
- Displacement: Measure the amount of vertebral body displacement, angulation, and translation. Significant displacement (e.g., >50% of vertebral body height) often indicates instability.
- Spinal Canal Compromise: Determine if the fracture fragments compromise the spinal canal, which can indicate instability and risk of neurological injury. Observe for impingement on the spinal cord or nerve roots.
Imagine the spine as a building. A stable fracture is like a crack in a strong wall – it might be annoying, but the structure is generally intact. An unstable fracture is like a major collapse of a wall – it requires immediate support to prevent further damage. We assess the integrity of the ‘supporting structures’ (ligaments) and the degree of ‘collapse’ (displacement) to determine the stability.
The combination of these findings helps in classifying the fracture (e.g., using the Denis classification for thoracolumbar fractures) and determining the need for surgical stabilization.
Q 18. What are the different types of spinal instrumentation and how are they visualized on imaging?
Various spinal instrumentation techniques are used to stabilize the spine after fractures, deformity correction, or other surgical procedures. These are visualized on imaging to assess placement, efficacy, and potential complications.
- Pedicle screws: These screws are inserted into the pedicles (posterior bony projections) of the vertebra. On imaging, they appear as radiopaque (bright) metallic densities within the pedicles on both CT and radiographs.
- Transfacet screws: These screws are placed through the facet joints, connecting the superior and inferior articulating processes of adjacent vertebrae. They are typically visualized on lateral radiographs and CT.
- Lateral mass screws: These screws are placed into the lateral masses of the cervical vertebrae. They are also clearly visualized on lateral radiographs and CT scans.
- Rods and plates: These metal constructs connect the screws and provide structural support. They appear as radiopaque structures connecting the screws on imaging.
- Cage implants: These are often used in anterior approaches for spinal fusion and appear as radiopaque materials filling the intervertebral disc space.
Think of it like scaffolding for a building: The screws are the anchors, and the rods and plates are the beams providing support. Imaging confirms their placement and stability, checking for any issues such as screw loosening or breakage, which could indicate a need for revision surgery.
Q 19. Discuss the use of contrast agents in spine imaging and their potential complications.
Contrast agents, primarily gadolinium-based chelates, are used in spine MRI to enhance visualization of specific tissues and structures, particularly in cases of infection, inflammation, or tumor.
- Improved visualization: Gadolinium enhances the signal intensity of tissues with a disrupted blood-brain barrier (such as in inflammation or tumor), making them more easily distinguishable from surrounding tissues.
- Applications: Contrast-enhanced MRI is useful in evaluating epidural abscesses, disc herniations with inflammation, neoplastic lesions (tumors), and infection.
- Potential complications: Although rare, gadolinium-based contrast agents can cause nephrogenic systemic fibrosis (NSF) in patients with severe kidney impairment. Allergic reactions, although uncommon, are another potential complication.
It’s like highlighting important parts of a document. The contrast agent highlights areas of inflammation or tumor, making it easier to identify and diagnose the problem. However, like any medication, it has potential side effects, which are carefully considered before administration.
Q 20. Explain the importance of image quality in evaluating spinal pathology.
High-quality spine imaging is essential for accurate diagnosis and treatment planning. Factors influencing image quality significantly impact the interpretation.
- Spatial Resolution: High spatial resolution allows for clear visualization of small anatomical details, essential for detecting subtle fractures, small tumors, or ligamentous injuries. Poor resolution can mask pathology.
- Contrast Resolution: Good contrast resolution allows for differentiation between tissues with similar signal intensities. This is crucial for distinguishing between different types of soft tissues (e.g., inflammation vs. tumor) and bone marrow abnormalities.
- Noise: Excessive image noise reduces the clarity and detail making it difficult to interpret findings. Proper optimization of imaging parameters helps minimize noise.
- Artifacts: Motion artifacts, susceptibility artifacts (from metal implants) and other artifacts obscure the underlying anatomy and can mislead the interpreter.
Imagine trying to read a blurry photograph. If the image is of poor quality, it’s difficult to determine the details and make an accurate assessment. High-quality imaging is the foundation of a precise diagnosis.
Q 21. Describe the role of post-processing techniques in enhancing spine image interpretation.
Post-processing techniques play a crucial role in enhancing image interpretation and improving diagnostic accuracy. They allow for a more thorough analysis of the imaging data.
- Multiplanar reconstruction (MPR): MPR allows for visualization of the anatomy in various planes (axial, sagittal, coronal) which helps to better assess the relationship between different structures, such as the relationship of a lesion to the spinal cord.
- Maximum intensity projection (MIP): MIP enhances the visibility of bone and metal implants, by displaying only the highest intensity signals across the image, therefore making it helpful to asses the integrity of instrumentation.
- Three-dimensional (3D) reconstructions: 3D renderings allow for improved visualization of complex anatomy or fractures. This can help to better understand three-dimensional relationship of bones, especially important in planning surgery.
- Image fusion: Combining images from different modalities (e.g., CT and MRI) allows for correlation of findings and a more comprehensive assessment. This is especially useful in evaluating complex spinal pathology.
Think of it like using different tools to improve your understanding of a complex assembly. These post-processing techniques enhance the visualization of the anatomy and help in generating the most accurate interpretation.
Q 22. What are the ethical considerations regarding patient confidentiality and image management?
Patient confidentiality and image management are paramount in spine imaging. We adhere to strict HIPAA regulations and institutional policies to protect patient privacy. This involves secure storage of digital images using anonymized identifiers, controlled access to PACS (Picture Archiving and Communication System) systems with role-based permissions, and secure transmission of images. For example, only authorized personnel with a legitimate need to access the images (e.g., radiologists, orthopedic surgeons, treating physicians) are granted access. Any breaches or potential breaches are immediately reported according to established protocols. Furthermore, we are acutely aware of the ethical implications of using patient images for teaching or research purposes; we always obtain informed consent before utilizing any identifiable patient data.
- Secure Storage: Images are stored on encrypted servers with restricted access.
- Access Control: PACS systems utilize robust authentication and authorization mechanisms.
- Data Anonymization: Patient identifiers are removed or replaced with unique codes when images are used for educational or research purposes.
- Incident Reporting: Any security incidents are reported promptly to the relevant authorities.
Q 23. How do you ensure accurate and timely reporting of spine imaging studies?
Accurate and timely reporting is crucial for effective patient care. My process begins with a thorough review of all available imaging data, including all imaging planes (axial, sagittal, coronal) and any relevant clinical information. This is followed by a structured reporting process, ensuring all key findings—including the presence, location, size, and characteristics of any abnormalities—are meticulously documented. We utilize standardized reporting templates to ensure consistency and completeness. Timely reporting involves prioritizing urgent cases and communicating findings to the referring physician promptly, often within 24-48 hours, depending on the urgency. I understand that delays can impact patient treatment and therefore prioritize efficiency while maintaining the highest standards of accuracy. For complex cases, a formal discussion with a senior radiologist or specialist may be necessary to ensure the most accurate interpretation.
For example, in a case of suspected spinal fracture, the report is prioritized and communicated immediately to the emergency department physician, enabling swift intervention.
Q 24. Explain your experience working with different imaging systems and software.
Throughout my career, I’ve gained extensive experience with a variety of imaging systems and software. This includes working with different modalities such as CT, MRI, and conventional X-ray systems from various manufacturers (e.g., GE, Siemens, Philips). I am proficient in utilizing various PACS (Picture Archiving and Communication Systems) and image post-processing software packages (e.g., OsiriX, 3D Slicer) to enhance image visualization and analysis. My skills extend to utilizing advanced reconstruction techniques and 3D rendering to better assess complex spinal anatomy and pathology. I am also adept at using specialized software for measuring bone density and spinal curvature.
For instance, in one case, utilizing advanced 3D reconstruction software from a CT scan helped in visualizing a complex fracture pattern not easily appreciated on standard planar images, ultimately guiding surgical planning.
Q 25. Describe your proficiency in interpreting various imaging planes (axial, sagittal, coronal).
Interpreting images in axial, sagittal, and coronal planes is fundamental to spine imaging. Each plane provides unique information. The axial plane offers a cross-sectional view, excellent for evaluating the vertebral bodies, pedicles, and neural foramina. The sagittal plane provides a side view, crucial for assessing spinal alignment, curvature, and the relationships between vertebrae. The coronal plane shows a front-to-back view, particularly useful for visualizing the paraspinal muscles and ligaments. I seamlessly integrate information from all three planes to form a comprehensive understanding of the spinal anatomy and any pathology present. This integrated approach is critical to detecting subtle abnormalities or complex pathologies that might be missed when examining just one plane.
Think of it like building a three-dimensional puzzle: each plane provides a different piece, but only by combining all three can you get the complete picture.
Q 26. How do you handle challenging cases or images with poor quality?
Handling challenging cases or images with poor quality requires a systematic approach. First, I assess the image quality, identifying the limitations (e.g., motion artifacts, poor contrast, insufficient spatial resolution). Then, I utilize image enhancement techniques available in the post-processing software to optimize visualization. This might involve adjusting windowing and leveling, applying noise reduction filters, or employing advanced reconstruction methods. If image quality remains insufficient, I may consult with colleagues or refer the patient for additional imaging studies (e.g., a repeat MRI with better technique). In cases with ambiguous findings, I strive to be conservative in my interpretation, highlighting the limitations of the image quality and suggesting further investigation if clinically indicated. Prioritizing patient safety and avoiding premature or inaccurate conclusions is always my primary concern.
For example, with a motion-blurred MRI, I might focus on identifying areas where the image is clearer, and cross-reference with other imaging modalities or clinical findings to reach a diagnosis.
Q 27. Describe your experience collaborating with other healthcare professionals (e.g., radiologists, surgeons).
Collaboration is essential in spine imaging. I regularly work with radiologists, orthopedic surgeons, neurosurgeons, and other healthcare professionals. This involves discussing findings, coordinating imaging studies, and contributing to shared decision-making regarding patient care. Clear and effective communication is paramount, ensuring that my interpretations are readily understood by the clinical team and incorporated into the overall treatment plan. I often participate in multidisciplinary team meetings to discuss complex cases and formulate the most effective management strategies. This collaborative approach is crucial for providing high-quality patient care.
For example, I might work with a neurosurgeon to plan the optimal surgical approach for a patient with spinal stenosis, providing detailed measurements and anatomical information based on the imaging findings.
Q 28. How do you stay up-to-date with the latest advancements in spine imaging technology and techniques?
Staying current with the latest advancements in spine imaging is a continuous process. I regularly attend professional conferences (e.g., RSNA, ECR), participate in continuing medical education (CME) courses, and read peer-reviewed journals and professional publications (e.g., Radiology, American Journal of Neuroradiology). I also actively participate in professional organizations (e.g., American College of Radiology) to keep abreast of new technologies and guidelines. Online resources and educational platforms are also valuable tools for staying informed about the latest research and developments. This ensures that I am equipped with the most up-to-date knowledge and skills to provide the highest quality care to my patients.
For example, I recently completed a CME course on advanced MRI techniques for spinal cord injury, enabling me to provide more accurate and detailed assessments in this challenging area.
Key Topics to Learn for Spine Imaging Interview
- Anatomy and Physiology of the Spine: Thorough understanding of spinal structures, including vertebrae, discs, ligaments, and nerves. This forms the foundation for interpreting imaging studies.
- Imaging Modalities: Expertise in interpreting X-rays, CT scans, MRI scans, and myelograms. Focus on identifying normal anatomy and recognizing common pathologies.
- Pathologies of the Spine: Knowledge of degenerative disc disease, spinal stenosis, fractures, infections, tumors, and congenital anomalies. Understanding the characteristic imaging features of each condition is crucial.
- Practical Application: Analyzing imaging studies to identify the location, extent, and severity of spinal pathology. Ability to correlate imaging findings with clinical presentation for accurate diagnosis.
- Image Analysis Techniques: Proficiency in measuring spinal canal dimensions, assessing disc height and morphology, and identifying subtle signs of pathology. This includes understanding the limitations of each imaging modality.
- Problem-solving Approach: Developing a systematic approach to image interpretation, considering differential diagnoses, and integrating imaging findings with patient history and clinical examination.
- Advanced Techniques (Optional): Depending on the seniority of the role, familiarity with advanced imaging techniques like dynamic MRI or advanced post-processing techniques might be beneficial.
Next Steps
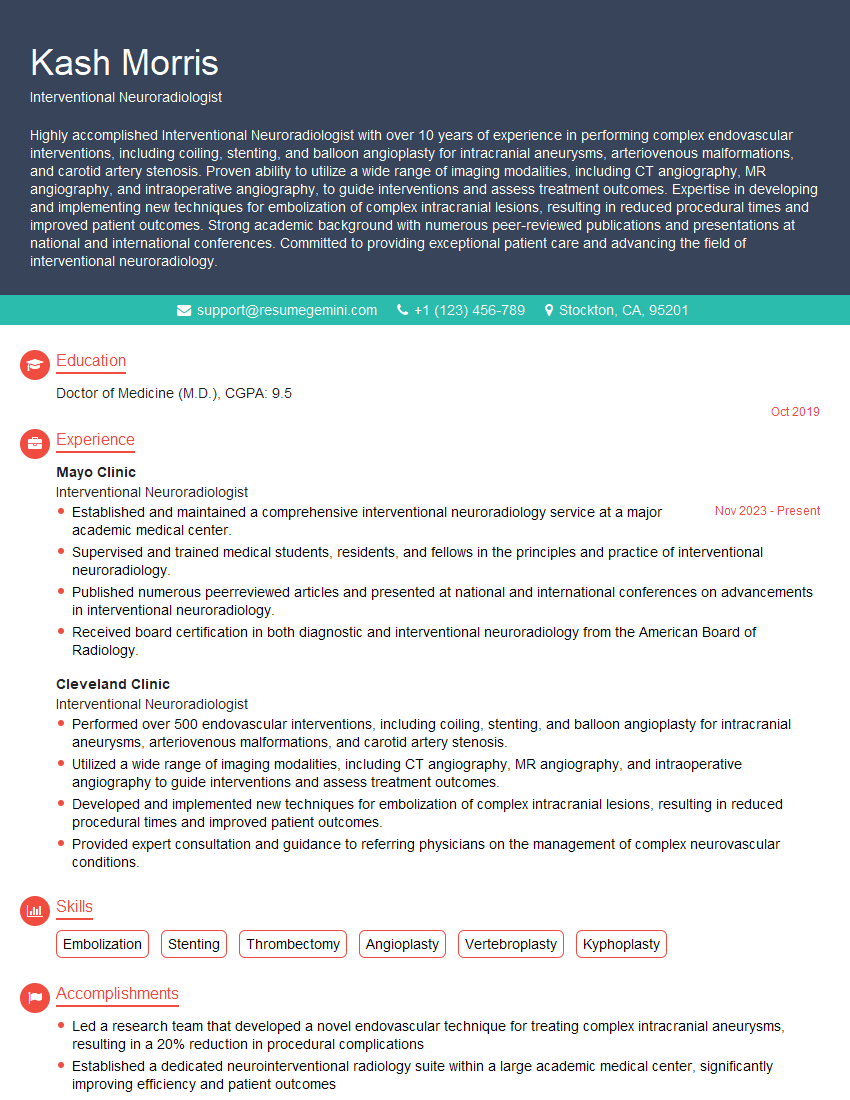
Mastering Spine Imaging opens doors to exciting career opportunities in a rapidly growing field. A strong understanding of this area is highly sought after in diagnostic radiology, orthopedic surgery, neurosurgery, and pain management. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a compelling and effective resume tailored to the specific requirements of Spine Imaging roles. Examples of resumes tailored to this field are available within ResumeGemini to guide you in building a professional application that showcases your skills and experience.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.