Cracking a skill-specific interview, like one for Surgical Correction of Crooked Toes (Hammertoes), requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Surgical Correction of Crooked Toes (Hammertoes) Interview
Q 1. Describe the different surgical techniques used for hammertoe correction.
Hammertoe correction surgery involves several techniques, each tailored to the severity and specific characteristics of the deformity. The goal is always to restore the toe’s normal alignment and function. Common surgical techniques include:
Arthroplasty: This procedure involves removing a portion of the joint to improve the toe’s range of motion and straighten the joint. It’s like smoothing out a rough joint to allow for easier movement. This is often suitable for milder hammertoe deformities.
Osteotomy: An osteotomy involves cutting and reshaping the bone to correct the angle of the joint. Imagine it like carefully adjusting a bent piece of metal to regain its straightness. This is usually reserved for more significant deformities.
Tenotomy: This focuses on the tendons that control toe movement. A tenotomy involves partially or completely severing the tight tendons that are contributing to the bent toe, allowing the toe to straighten. Think of it as releasing a tight rubber band that’s pulling the toe into a bent position.
Capsulotomy: This involves releasing the joint capsule, the tough tissue surrounding the joint. This is often used in conjunction with other procedures to improve joint mobility and allow for better correction.
Soft tissue procedures (e.g., excision of the flexor tendon, release of tight ligaments): These aim to address soft tissue imbalances contributing to the deformity. Often done in conjunction with bony procedures.
Fusion (Arthrodesis): In severe cases or when other procedures have failed, fusion might be necessary. This involves permanently joining the bones of the affected joint. Think of it as rigidly fixing the crooked joint in the correct position. This sacrifices some movement but achieves better long-term stability.
The choice of technique depends on factors like the patient’s age, activity level, the severity of the deformity, and the presence of any associated conditions.
Q 2. What are the indications and contraindications for surgical intervention in hammertoe deformity?
Surgical intervention for hammertoe is indicated when conservative treatments like padding, splinting, or orthotics have failed to provide adequate relief from pain, and the deformity is significantly impacting the patient’s quality of life. The toe may be severely crooked causing discomfort in shoes, calluses, corns, or even ulcerations.
Indications:
- Persistent pain despite conservative management
- Significant cosmetic deformity
- Impaired gait or function
- Recurring ulcerations or corns
- Severe contracture of the toe joint
Contraindications:
- Poor vascular supply to the toe (compromising healing)
- Severe peripheral neuropathy (affecting sensation and healing)
- Severe underlying medical conditions that increase surgical risk
- Patient unwillingness or inability to comply with post-operative care instructions
- Active infection
It’s important to carefully weigh the risks and benefits of surgery in each case.
Q 3. Explain the preoperative assessment and planning process for a patient with a hammertoe.
Preoperative assessment is crucial for successful hammertoe surgery. It begins with a thorough history and physical examination. This includes assessing the patient’s medical history, current medications, allergies, smoking status and any other relevant factors influencing surgical risk. The deformity itself is carefully examined, documenting the severity, location and any associated issues. This often includes:
- Detailed clinical examination: Assessing range of motion, tenderness, presence of calluses or corns, and any neurological deficits.
- Radiographic evaluation (X-rays): Determining the degree of bony deformity and the presence of any arthritis.
- Physical therapy assessment (if applicable): To assess strength, range of motion, and identify areas needing rehabilitation.
- Vascular assessment (if necessary): To ensure adequate blood supply to the toe, especially if the patient has underlying vascular disease.
- Discussion of surgical options and expectations: Thoroughly explaining the procedure, risks, benefits, and recovery expectations to ensure informed consent.
Based on this assessment, the surgeon determines the appropriate surgical technique and creates a detailed surgical plan.
Q 4. What are the common complications associated with hammertoe surgery, and how are they managed?
Hammertoe surgery, while generally safe and effective, carries potential complications. These can include:
- Infection: This is a serious concern and is addressed with appropriate antibiotic prophylaxis and meticulous surgical technique.
- Nerve damage: Potential for numbness or altered sensation in the toe, which usually improves over time.
- Joint stiffness: This is managed with physical therapy and regular exercises.
- Recurrence of deformity: Less common if appropriate surgical technique is chosen and post-op care is followed.
- Nonunion (failure of bone to heal): May require additional surgery.
- Malunion (bone healing in an incorrect position): May require corrective osteotomy.
- Pain: Persistent pain is infrequent but requires additional evaluation and management. Pain management strategies include medication, physical therapy, and sometimes injection therapies.
The management of these complications depends on the specific problem and can range from conservative measures like medication and physiotherapy to further surgery. Regular post-operative follow-up appointments are critical in identifying and addressing any issues promptly.
Q 5. Discuss the post-operative care instructions given to patients after hammertoe surgery.
Post-operative care is crucial for a successful outcome. Instructions usually include:
- Pain management: Patients are prescribed medication to manage post-operative pain and swelling.
- Elevation: Keeping the foot elevated to minimize swelling.
- Wound care: Regularly cleaning and dressing the incision.
- Range of motion exercises: Starting gentle exercises soon after surgery to prevent stiffness.
- Weight-bearing restrictions: Following specific weight-bearing instructions provided by the surgeon. This might involve crutches or a walking boot.
- Regular follow-up appointments: Attending scheduled appointments for monitoring wound healing and progress.
- Physical therapy: Undergoing prescribed physical therapy for strengthening and improving mobility.
- Protective footwear: Wearing appropriate shoes post-operatively to protect the healing toe.
Providing clear and detailed instructions, combined with close follow-up, greatly improves the chances of a successful recovery.
Q 6. How do you select the appropriate surgical approach (e.g., arthroplasty, tenotomy, osteotomy) for different types of hammertoe deformities?
Selecting the appropriate surgical approach for hammertoe is crucial. The choice depends on several factors, including the severity and type of deformity, the patient’s age and activity level, and the presence of any associated conditions.
Mild hammertoe: A tenotomy, or possibly a soft tissue procedure, may suffice. This addresses the imbalance in the tendons and ligaments causing the deformity.
Moderate hammertoe: An arthroplasty, osteotomy, or a combination of these procedures might be necessary. Arthroplasty addresses the joint itself, while an osteotomy corrects bony deformities.
Severe hammertoe with significant joint involvement: Arthrodesis (fusion) may be the most appropriate option for stability and pain relief, although this sacrifices motion.
A thorough clinical examination, radiological assessment (X-rays), and a comprehensive understanding of the patient’s needs and expectations are crucial for making informed surgical decisions. It’s a collaborative process between the surgeon and the patient.
Q 7. What are the advantages and disadvantages of minimally invasive techniques for hammertoe correction?
Minimally invasive techniques for hammertoe correction aim to reduce tissue trauma and improve recovery times. These often involve smaller incisions and less extensive surgical manipulation. Percutaneous techniques are gaining popularity.
Advantages:
- Smaller incisions leading to less scarring.
- Reduced pain and swelling post-operatively.
- Faster recovery and rehabilitation.
- Shorter hospital stay (often outpatient procedures).
Disadvantages:
- Less precise correction compared to open surgery (requiring higher surgeon skill and experience).
- Limited applicability; not suitable for all types of hammertoe deformities.
- Higher risk of recurrence in some cases.
- Potential for complications like tendon rupture or nerve damage though less frequent.
The decision to use minimally invasive techniques is made on a case-by-case basis, carefully considering the patient’s specific needs and the surgeon’s expertise.
Q 8. Describe your experience with different types of implants used in hammertoe surgery.
The choice of implant in hammertoe surgery depends heavily on the specific deformity and the surgeon’s preference. While some procedures are entirely soft tissue based, many utilize implants to enhance correction and stability. Common implants include Kirschner wires (K-wires), which are small metal pins used for temporary fixation, aiding in bone healing and maintaining the corrected position. These are often removed after several weeks. Another option is absorbable pins, which dissolve over time, eliminating the need for a second procedure to remove them. Finally, for more severe deformities or cases requiring more robust stabilization, small plates and screws might be employed to provide more rigid fixation, especially in cases involving osteotomy (bone cutting).
For example, in a flexible hammertoe (where the joint can be passively straightened), a simple soft tissue procedure may suffice. However, a rigid hammertoe (where the joint is fixed in a flexed position) often requires an osteotomy with internal fixation using either K-wires, absorbable pins, or plates and screws for optimal correction and prevention of recurrence.
Q 9. How do you manage patients with comorbid conditions (e.g., diabetes, peripheral neuropathy) undergoing hammertoe surgery?
Managing patients with comorbid conditions like diabetes and peripheral neuropathy requires a meticulous and multidisciplinary approach. These conditions significantly increase the risk of complications, such as wound healing problems, infection, and nerve damage. Pre-operative assessment is crucial, including thorough vascular assessment to evaluate blood flow to the foot. We carefully review the patient’s medical history, HbA1c levels (for diabetes control), and assess their neurological function. Patients with poor glycemic control will usually require optimization of their diabetic management before surgery. The surgical technique itself might be modified to minimize trauma and promote better blood supply to the surgical site. Post-operative care is intensified, including vigilant monitoring for signs of infection and meticulous wound care. We might employ specialized dressings and frequently assess for signs of neuropathy, ensuring appropriate pain management, while closely monitoring the wound healing progress. Regular follow-up appointments are essential to address any emerging issues promptly.
Q 10. How do you counsel patients regarding realistic expectations and potential outcomes after hammertoe surgery?
Counseling patients about realistic expectations is paramount. I explain that while hammertoe surgery aims to improve appearance and function, it’s not a perfect solution. I detail the potential benefits, such as pain reduction and improved foot mechanics, while clearly outlining the potential risks and limitations. For instance, some residual deformity might remain, or there might be some stiffness. I present realistic visual examples of postoperative outcomes – both successful and less-than-perfect – to manage expectations effectively. The conversation also includes the possibility of needing further procedures, such as revision surgery, although that’s rare if proper technique is used. Finally, we discuss the post-operative recovery process, emphasizing the importance of compliance with the prescribed exercises and physical therapy to achieve optimal results. I want the patient to feel fully informed and comfortable with their decision.
For example, I show a patient a before-and-after photo series illustrating varied success levels. This helps to ground the discussion in tangible realities.
Q 11. What are the key elements of informed consent for hammertoe surgery?
Informed consent for hammertoe surgery is a crucial step ensuring ethical and legal compliance. It involves a detailed discussion covering several key elements. First, a thorough explanation of the diagnosis, including the nature and extent of the hammertoe deformity. Second, a comprehensive description of the proposed surgical procedure, including the techniques to be used and the rationale for choosing a particular approach. Third, a frank discussion of the potential benefits of surgery, such as pain relief, improved function and cosmetic appearance. Fourth, a detailed explanation of the potential risks and complications associated with the procedure, which might include infection, nerve damage, persistent pain, stiffness, nonunion (bone not healing properly), and unsatisfactory cosmetic results. Finally, the discussion involves addressing alternative treatment options, such as conservative measures like orthotics or physical therapy. The patient must clearly understand that they are free to decline surgery at any time.
The consent process is documented in writing, and the patient is encouraged to ask questions to ensure complete understanding before signing the consent form.
Q 12. How do you assess the success of hammertoe surgery?
Assessing the success of hammertoe surgery involves multiple criteria. The primary measure is pain reduction. A successful outcome typically results in significant pain relief. Second, we evaluate the correction of the deformity itself. This involves assessing the alignment of the toe and the improvement in joint function. Range of motion is also carefully evaluated, striving for optimal flexibility without compromising stability. Finally, we consider the cosmetic outcome, focusing on the overall appearance of the foot and the aesthetic integration of the corrected toe. Post-operative X-rays play an important role in determining the bony alignment and stability. Patient satisfaction is also a critical factor considered. A combined assessment of these factors determines whether the surgery has achieved a successful outcome.
Q 13. What are the common causes of recurrence after hammertoe surgery?
Recurrence after hammertoe surgery is relatively infrequent when proper surgical technique is utilized, but can occur. Several factors contribute to this. Inadequate correction of the underlying deformity during the initial surgery, for example, failure to address a contributing structural issue like contracture of a tendon, is a major cause. Inadequate post-operative care and noncompliance with instructions regarding physical therapy or shoe wear can also increase the risk of recurrence. In some cases, the underlying biomechanics of the foot might lead to a re-development of the deformity, irrespective of surgical technique. Finally, certain patient-specific factors, such as age, overall health, and the presence of comorbid conditions, can also affect the long-term outcome and increase the risk of recurrence.
Q 14. Explain your approach to managing post-operative pain and swelling in hammertoe patients.
Post-operative pain and swelling are expected after hammertoe surgery, but we manage these aggressively to promote comfort and facilitate healing. The approach is multi-pronged. First, elevation of the foot to reduce swelling and improve venous return is crucial. Second, we prescribe medications, including analgesics (pain relievers), to control post-operative pain and anti-inflammatory drugs such as NSAIDs to reduce swelling. Third, regular ice packs are recommended to further reduce swelling and pain. Fourth, early mobilization and controlled range of motion exercises, as prescribed by the physical therapist, are essential to prevent stiffness and promote flexibility. Finally, appropriate wound care is vital to prevent infection. The patients are carefully monitored for any signs of worsening pain, excessive swelling, or infection, which would warrant prompt intervention.
Q 15. Describe your experience with different types of anesthesia used in hammertoe surgery.
The choice of anesthesia for hammertoe surgery depends on several factors, including the patient’s overall health, the number of toes needing correction, and the complexity of the procedure. We typically offer several options.
- Local anesthesia with sedation: This is a common choice for simpler cases involving one or two toes. The patient remains awake but is relaxed and comfortable due to the sedation medication. This allows for good patient interaction and immediate post-op assessment of sensory function.
- Regional anesthesia (ankle block): This numbs the entire foot and lower leg, offering a higher level of pain control. It’s suitable for multiple toe corrections or more extensive procedures. Recovery is generally faster compared to general anesthesia, while still offering a good level of pain management.
- General anesthesia: This is reserved for patients with significant medical conditions, those requiring multiple procedures simultaneously (such as bunionectomy combined with hammertoe correction), or those who experience severe anxiety related to medical procedures. While offering the most pain relief, it has a longer recovery period and carries the associated risks of general anesthesia.
The decision regarding the type of anesthesia is always made in consultation with the patient and anesthesiologist, taking into account their specific needs and preferences. We carefully weigh the benefits and risks of each option to provide the safest and most effective approach.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you address patient concerns and anxieties about hammertoe surgery?
Addressing patient anxieties about hammertoe surgery is crucial for a positive outcome. I begin by actively listening to their concerns, validating their feelings, and providing thorough education.
- Detailed explanation of the procedure: I use clear and simple language, avoiding medical jargon whenever possible. I explain the steps involved, the expected recovery time, and potential complications. I also show them before and after photos of past successful surgeries.
- Addressing specific concerns: I address their anxieties directly, offering reassurance and evidence-based information. For instance, if a patient is worried about pain, I discuss our pain management strategies, including both anesthetic options and post-operative pain medication. If they are anxious about the outcome, I discuss the realistic expectations and the potential for improvement.
- Building rapport and trust: I create a comfortable environment where patients feel comfortable asking questions. I take time to answer their questions thoroughly and patiently, addressing all their concerns until they feel at ease.
Many patients find that speaking to previous patients who have undergone the procedure can significantly alleviate their anxieties. We often facilitate such connections when appropriate.
Q 17. What are the latest advancements in surgical techniques and technologies for hammertoe correction?
The field of hammertoe correction is constantly evolving. Several recent advancements have improved surgical outcomes and patient experience.
- Minimally invasive techniques: These techniques involve smaller incisions, leading to less scarring, reduced pain, and faster recovery times. Percutaneous techniques, for instance, use small incisions and specialized instruments to correct the deformity.
- Improved implant designs: Advances in biocompatible materials and surgical implant design have led to more effective and durable fixation methods. These newer implants often require less hardware, resulting in less risk of implant failure and faster healing.
- Arthroscopic techniques: In select cases, arthroscopy can be used to access and correct the underlying joint pathology causing the hammertoe deformity. This minimally invasive technique offers several advantages, including reduced trauma and faster recovery.
- Computer-assisted surgery (CAS): CAS technologies, while still relatively new to hammertoe correction, offer precise surgical planning and execution. This can improve accuracy and potentially reduce complications.
These advancements are constantly being refined and improved upon, leading to better patient outcomes and reduced recovery times.
Q 18. How do you stay up-to-date with the current literature and advancements in foot and ankle surgery?
Staying current with the latest literature and advancements in foot and ankle surgery is crucial for providing the best possible care to my patients. I employ several strategies:
- Membership in professional organizations: I am an active member of the American Orthopaedic Foot & Ankle Society (AOFAS) and other relevant professional societies. These organizations offer access to journals, conferences, and continuing medical education (CME) courses.
- Regular review of peer-reviewed journals: I regularly read leading journals in the field, such as the Foot & Ankle International and the Journal of Bone and Joint Surgery. I focus on articles related to surgical techniques, new technologies, and advancements in treatment protocols.
- Attendance at conferences and workshops: I regularly attend national and international conferences and workshops to learn about the latest research and surgical techniques from leading experts in the field.
- Participation in continuing medical education (CME) activities: I actively participate in CME courses and online educational resources to maintain my knowledge and skills.
This ongoing commitment to learning ensures that I can offer my patients the most effective and up-to-date treatments.
Q 19. Describe a challenging case involving hammertoe surgery that you encountered and how you managed it.
One particularly challenging case involved a patient with severe rheumatoid arthritis who presented with multiple, rigidly contracted hammertoes and significant joint destruction. The usual surgical techniques were unsuitable due to the advanced joint damage and the patient’s underlying condition.
The management of this case required a multi-faceted approach:
- Detailed pre-operative planning: Extensive imaging studies (X-rays, CT scans) were performed to assess the extent of the joint damage. This informed our surgical strategy, which focused on soft tissue release and arthrodesis (fusion) of the affected joints.
- Careful surgical technique: The surgery was performed meticulously to avoid further damaging the already compromised joint structures. We used a combination of open and minimally invasive techniques to optimize the surgical approach.
- Post-operative management: Post-operative care was crucial, focusing on pain management, wound care, and close monitoring for complications. Physical therapy played a vital role in maximizing functional recovery.
Despite the challenges, the surgery was successful, and the patient achieved significant improvement in their foot function and pain levels. This case highlighted the importance of careful pre-operative planning, a tailored surgical approach, and meticulous post-operative care in managing complex hammertoe cases.
Q 20. How do you collaborate with other healthcare professionals in the management of patients with hammertoe deformities?
Effective collaboration is vital in managing patients with hammertoe deformities. I work closely with several healthcare professionals:
- Primary care physicians: They provide information about the patient’s overall health and any relevant medical conditions that could affect the surgery or recovery.
- Anesthesiologists: They play a crucial role in selecting the appropriate anesthesia type and ensuring the patient’s safety during the procedure.
- Physical therapists: They provide essential post-operative rehabilitation, helping patients regain strength, range of motion, and function in their foot and ankle.
- Podiatrists: For patients with associated conditions affecting their feet, I often collaborate with podiatrists who may focus on conservative management or other aspects of foot care.
Regular communication and a coordinated care plan ensure that each patient receives comprehensive and optimized care, maximizing their chances of a successful outcome.
Q 21. What is your experience with different types of surgical fixation methods used in hammertoe surgery?
The choice of surgical fixation method depends on various factors, including the severity of the deformity, the patient’s age and overall health, and the surgeon’s preference. I use several techniques:
- K-wires (Kirschner wires): These thin metal wires are commonly used for simple hammertoe corrections. They are inserted through small incisions and provide temporary stabilization of the joint.
- Screws: These offer more robust fixation than K-wires and are often preferred for more severe deformities or when more stability is needed. They can be either bioabsorbable (dissolve over time) or metallic (require removal).
- Plates and screws: In cases with significant bone loss or instability, plates and screws offer the strongest fixation. They are less commonly used in hammertoe correction than K-wires or screws alone, unless there is substantial associated bone damage.
- Implant-less techniques: In select cases, particularly with less severe deformities, it may be possible to correct the deformity without using any implants. This relies primarily on soft tissue releases and judicious joint manipulation.
The selection of the appropriate fixation method is crucial for optimizing surgical outcomes and ensuring a successful recovery. The choice is made on a case-by-case basis and is tailored to the patient’s specific needs.
Q 22. Describe your experience with managing infection after hammertoe surgery.
Infection is a serious concern after any surgery, and hammertoe correction is no exception. My approach focuses on meticulous surgical technique to minimize the risk from the outset. This includes using sterile instruments and drapes, careful tissue handling, and diligent hemostasis (stopping bleeding) to prevent hematoma (blood clots) formation, a breeding ground for infection. Post-operatively, patients receive detailed instructions on wound care, including regular cleaning with antiseptic solutions and monitoring for signs of infection like redness, swelling, increased pain, or pus. Early detection is key. I often prescribe prophylactic antibiotics before surgery for high-risk patients. If infection does occur, it is immediately addressed with aggressive antibiotic therapy, sometimes requiring surgical debridement (removal of infected tissue) to ensure complete eradication.
For example, I recall a patient who developed a minor cellulitis (skin infection) post-operatively. We quickly initiated a course of oral antibiotics, and with diligent wound care, the infection resolved completely within a week. However, in more severe cases, intravenous antibiotics and even surgical intervention may be necessary. Open communication with the patient and a proactive approach are vital in managing post-operative infection.
Q 23. How do you assess and manage potential nerve injury during and after hammertoe surgery?
Nerve injury is a potential complication in hammertoe surgery because the nerves supplying sensation to the toes are located close to the surgical site. My assessment begins with a thorough pre-operative examination, carefully evaluating the patient’s neurological function in the affected toe(s). During surgery, I utilize meticulous surgical dissection techniques, employing magnification and specialized instruments whenever needed, to identify and protect the nerves. Intraoperative nerve monitoring, while not routinely used in all cases, can be employed for complex cases or when there’s a higher risk of nerve injury. Post-operatively, I meticulously monitor the patient for signs of nerve damage, including numbness, tingling, or pain that differs from the expected post-surgical discomfort. Physical therapy can help address any residual nerve-related symptoms.
Imagine the nerves as delicate wires running alongside the structures we operate on. The goal is to carefully navigate around them, avoiding any direct contact or damage. In cases of suspected nerve injury, we might use electrodiagnostic studies (nerve conduction studies) to confirm the diagnosis and guide management.
Q 24. What is your experience with revising previous hammertoe surgeries?
Revision hammertoe surgery presents unique challenges because scar tissue and potential adhesions can complicate the procedure. It often requires more extensive surgery than the initial procedure. Prior to the revision, I thoroughly review the patient’s medical history and imaging studies (X-rays) to understand the details of the previous surgery and the current deformity. The goal is to correct the residual deformity while minimizing further complications. This often involves removing scar tissue, repositioning tendons, and sometimes utilizing different surgical techniques than initially employed.
For instance, I recently revised a case where a previous attempt at hammertoe correction had resulted in a recurrence of the deformity. Through meticulous dissection and careful tendon transfers, we were able to achieve a satisfactory correction and avoid further complications. Open communication with the patient is vital throughout this process, managing expectations regarding the complexity and potential challenges of revision surgery.
Q 25. How do you address the cosmetic concerns of patients regarding hammertoe surgery?
Addressing cosmetic concerns is an essential part of my practice. Hammertoes not only cause pain and functional limitations, but also significantly affect a patient’s self-esteem. I carefully explain the surgical options, discussing the potential benefits and limitations of each approach, and always strive to achieve the best possible cosmetic outcome. In some cases, smaller incisions, strategically placed to minimize scarring, are preferred. Post-operative care also includes measures to reduce scarring, such as silicone gel sheeting.
I always share before-and-after photos with potential patients to show the realistic cosmetic results achievable with surgery. Open communication and realistic expectations contribute to patient satisfaction.
Q 26. What are the long-term functional outcomes expected after hammertoe surgery?
The long-term functional outcomes after successful hammertoe surgery typically involve pain relief, improved range of motion in the affected toe(s), and enhanced ability to wear shoes comfortably. Patients often report improved gait and reduced discomfort during walking and other activities. However, the success is dependent on several factors including the severity of the deformity, the surgical technique, and the patient’s adherence to post-operative instructions. Long-term follow-up appointments are crucial to monitor the healing process and address any potential complications.
It’s important to manage expectations; while the surgery aims for significant improvement, full restoration to pre-deformity functionality isn’t always possible, especially in severe or longstanding cases. The goal is to achieve the best possible functional result considering the individual circumstances.
Q 27. What are the potential risks and benefits of different surgical approaches for hammertoe correction?
Several surgical approaches exist for hammertoe correction, each with its own benefits and risks. These include procedures involving tendon transfers, arthrodesis (joint fusion), and osteotomy (bone resection). Tendon transfers aim to restore the balance of forces around the toe joint, while arthrodesis stabilizes the joint by fusing it. Osteotomy involves reshaping the bone to correct the deformity.
For example, tendon transfers are often preferred for milder cases, as they preserve joint mobility. However, they carry a slightly higher risk of recurrence. Arthrodesis provides excellent long-term stability but sacrifices joint mobility. Osteotomy offers a balance between correction and joint preservation but involves a higher risk of complications like nonunion (failure of the bone to heal) or malunion (healing in an incorrect position). The choice of surgical approach depends on the individual patient’s anatomy, the severity of the deformity, and their functional goals and expectations. A thorough discussion with the patient is essential to select the optimal approach.
Q 28. Describe your experience with using imaging techniques (X-rays, CT scans) in the evaluation and treatment of hammertoe deformities.
Imaging techniques, particularly X-rays, play a crucial role in the evaluation and treatment of hammertoe deformities. Pre-operative X-rays help determine the severity of the deformity, assess the degree of joint involvement, and plan the surgical approach. They allow for precise measurement of bone angles and identification of any associated bone spurs or arthritis. While CT scans are less frequently used for routine hammertoe evaluations, they may be valuable in complex cases or when evaluating the presence of arthritis or other associated conditions.
Post-operative X-rays are essential to confirm the accuracy of the surgical correction and monitor bone healing, especially after procedures like osteotomy or arthrodesis. They allow for early identification of potential complications, such as nonunion or malunion, allowing for timely intervention.
Key Topics to Learn for Surgical Correction of Crooked Toes (Hammertoes) Interview
- Patient Assessment and Diagnosis: Understanding the various types of hammertoes, assessing severity using clinical examination and imaging techniques (X-rays), and differentiating between hammertoe and other foot deformities.
- Surgical Techniques: Mastering the knowledge of different surgical approaches (e.g., arthroplasty, osteotomy, tenotomy), their indications, and potential complications. Understanding pre-operative planning and intra-operative considerations is crucial.
- Post-Operative Care and Management: Familiarize yourself with post-operative pain management, wound care, rehabilitation protocols (physical therapy), and potential complications such as infection, nerve injury, or stiffness. Knowing how to manage patient expectations is key.
- Anesthesia and Perioperative Management: Understanding the anesthesia options and their implications for the procedure. Being aware of potential risks and complications associated with the anesthesia and the surgery itself.
- Biomechanics and Functional Anatomy of the Foot: A solid understanding of the underlying biomechanical factors contributing to hammertoe development and how surgical correction restores normal foot function is essential.
- Complications and their Management: Be prepared to discuss potential complications such as recurrence, malunion, infection, and nerve damage. Knowing how to identify, prevent, and manage these complications demonstrates expertise.
- Latest Advances and Research: Staying up-to-date on the latest surgical techniques, minimally invasive approaches, and emerging research in hammertoe correction is highly beneficial.
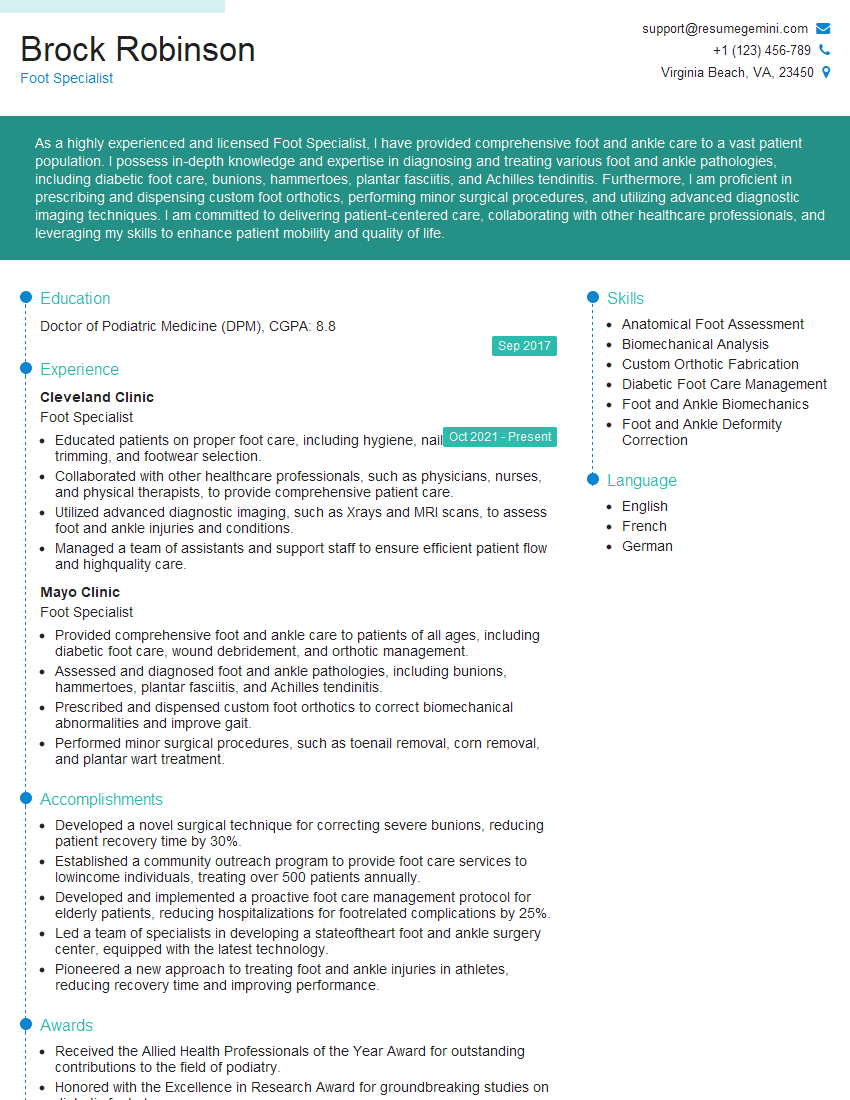
Next Steps
Mastering Surgical Correction of Crooked Toes (Hammertoes) demonstrates a specialized skill set highly valued in the field, significantly enhancing your career prospects. To maximize your job search success, creating an ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a compelling and effective resume tailored to highlight your expertise in this area. Examples of resumes specifically designed for candidates specializing in Surgical Correction of Crooked Toes (Hammertoes) are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.