The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Tendon Transfers interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Tendon Transfers Interview
Q 1. Describe the surgical technique for a flexor tendon transfer.
Flexor tendon transfers involve surgically moving a healthy tendon from one location to another to restore lost function. Think of it like rerouting a cable to power a device that’s lost its original connection. The procedure is complex and requires meticulous surgical technique. It typically involves several steps:
- Incision and Exposure: A carefully planned incision is made to access both the donor tendon and the recipient muscle. The surgeon must carefully dissect through layers of tissue to avoid damaging nerves and blood vessels.
- Harvesting the Donor Tendon: The selected donor tendon is carefully dissected free from its original attachment, ensuring adequate length and preserving its blood supply. This step requires precise surgical skill and a deep understanding of hand anatomy.
- Preparation of the Recipient Site: The recipient muscle’s insertion point is prepared to receive the transferred tendon. This might involve cleaning the insertion site or even creating a new insertion point.
- Tendon Transfer and Fixation: The donor tendon is then routed to its new location and securely fixed to the recipient muscle using sutures or other fixation techniques. The tension of the transfer is carefully adjusted to optimize function and avoid excessive tension or laxity. This is crucial for a successful outcome.
- Closure: The incision is meticulously closed in layers, with careful attention to hemostasis (stopping bleeding) and minimizing scarring.
The specific technique may vary depending on the specific transfer being performed, the patient’s anatomy, and the surgeon’s preference. For example, a transfer of the palmaris longus tendon to restore thumb function would utilize different surgical approaches compared to a transfer of the flexor carpi ulnaris tendon.
Q 2. Explain the indications for a tendon transfer in the hand.
Tendon transfers are indicated when a hand muscle or tendon is damaged or non-functional, leading to loss of movement or strength. They’re a powerful tool to restore hand function, but not a universal solution. Some common indications include:
- High radial nerve palsy: Where the wrist extensors are paralyzed, transfers can help restore wrist extension.
- Loss of thumb opposition: Several transfers, such as the opponensplasty, can restore the ability to oppose the thumb to the fingers.
- Severely injured flexor tendons: When direct repair is impossible or impractical, transfers can provide alternative pathways to restore finger flexion.
- Congenital hand deformities: Transfers can be used to correct certain birth defects impacting hand movement.
- Cerebral palsy: In some cases, transfers can improve hand function in patients with cerebral palsy.
Essentially, a tendon transfer is considered when other less invasive treatments have failed or are unsuitable and the patient’s overall health and condition allow for a major surgical procedure.
Q 3. What are the contraindications for a tendon transfer?
Contraindications to tendon transfer are situations where the procedure is unlikely to be successful or carries unacceptable risks. These include:
- Poor patient health: Significant medical conditions (heart disease, diabetes, etc.) that increase surgical risk.
- Inadequate tendon quality: If the donor tendon is too weak or poorly vascularized, it may not survive the transfer.
- Severe joint contractures: Stiff joints can limit the effectiveness of the transferred tendon.
- Uncontrolled infection: Any infection in the hand significantly increases the risk of complications post-surgery.
- Lack of patient compliance: Successful tendon transfer requires dedicated and intensive rehabilitation. Patients who are unwilling or unable to commit to this will have significantly decreased chances of success.
- Advanced peripheral neuropathy: Severe nerve damage that limits the ability to re-educate the muscles and achieve functional results
Careful assessment of the patient’s condition is crucial before proceeding with a tendon transfer. It’s a major operation, and it’s essential to weigh the benefits against the potential risks and limitations.
Q 4. Discuss the common complications associated with tendon transfers.
Like any surgical procedure, tendon transfers carry potential complications. Some of the most common include:
- Rupture of the transferred tendon: This can be due to insufficient fixation, excessive tension, or trauma.
- Non-union or delayed union: The tendon may not heal properly to the bone, leading to poor function.
- Infection: Infection at the surgical site can cause significant problems, possibly requiring further surgery.
- Tendon adhesions: Scar tissue can form around the transferred tendon, restricting movement.
- Nerve damage: Although rare, there is a risk of damage to nerves during surgery.
- Poor functional outcome: Sometimes, even with successful surgery, the desired functional improvement may not be achieved.
The risk of complications can be minimized through careful surgical planning, meticulous surgical technique, and diligent postoperative care. Regular follow-up with the surgeon is essential to monitor healing and address any potential problems.
Q 5. How do you choose the appropriate donor tendon for a transfer?
Choosing the appropriate donor tendon is a critical aspect of tendon transfer surgery. The selection process involves considering several factors:
- Tendon length and strength: The donor tendon must be long enough to reach the recipient site and strong enough to provide sufficient power.
- Tendon excursion: The donor tendon must have sufficient gliding range of motion to accommodate the new function.
- Vascularity: The donor tendon should have a good blood supply to ensure adequate healing.
- Functional sacrifice: The loss of function at the donor site should be minimal and acceptable.
- Anatomical location: The donor site should be accessible and allow for easy surgical approach.
For example, the palmaris longus tendon is a frequently used donor because it’s relatively long, strong, and its absence usually doesn’t cause significant functional loss. However, not all individuals have a palmaris longus tendon, so other suitable alternatives must be identified. The decision about the best donor tendon is highly individualized and often requires a comprehensive assessment of the patient’s specific needs and anatomy.
Q 6. What are the key principles of tendon-to-bone fixation?
Tendon-to-bone fixation is crucial for a successful tendon transfer. The key principles are:
- Secure Fixation: The tendon must be firmly attached to the bone to ensure that the transfer does not pull out or fail.
- Minimal Tension: The tendon should be fixed with just enough tension to provide the desired functional effect without placing excessive stress on the repair.
- Stable Fixation: The fixation technique must be robust enough to withstand the forces generated during rehabilitation and normal hand use.
- Blood Supply Preservation: The fixation technique should not compromise the blood supply to the tendon, which is vital for healing.
- Appropriate Fixation Method: The chosen method should be suited to the specific tendon and bone involved, and the surgeon’s experience.
Various fixation techniques exist, including using sutures, buttons, screws, or other specialized devices. The choice of fixation method depends on factors such as the size and strength of the tendon and bone, the location of the transfer, and the surgeon’s preference.
Q 7. Describe the rehabilitation protocol following a tendon transfer.
Rehabilitation after a tendon transfer is crucial for achieving a successful outcome. It’s a lengthy process requiring dedication and patience, usually lasting several months. A typical protocol includes:
- Early Protection: The hand is initially immobilized in a splint or cast to protect the repair during the early healing phase.
- Gradual Mobilization: As healing progresses, the patient begins to perform range of motion exercises under the guidance of a therapist.
- Strengthening Exercises: Once sufficient healing occurs, strengthening exercises are introduced to improve the power and function of the transferred tendon.
- Functional Activities: The patient progressively engages in more functional activities like pinching, grasping, and other hand movements.
- Occupational Therapy: Occupational therapy plays a crucial role in helping the patient adapt to the changes in hand function and perform daily tasks.
The specific rehabilitation protocol is tailored to the individual patient and the type of transfer performed. Close monitoring by the surgeon and therapist is necessary to ensure proper healing and prevent complications.
It’s important to remember that tendon transfers often require considerable time and effort before full function is regained. Patient compliance and adherence to the rehabilitation protocol are critical for a successful outcome. The rehabilitation is a collaborative effort involving the patient, the surgeon, and the therapist.
Q 8. How do you manage a failed tendon transfer?
Managing a failed tendon transfer is a complex process requiring a thorough reevaluation of the patient and the initial surgery. Failure can manifest in various ways, including insufficient strength, persistent pain, or recurrent deformity. The first step is a comprehensive clinical examination, focusing on range of motion, strength, and the presence of any residual contractures or adhesions. Imaging, such as ultrasound and MRI, is crucial to assess the tendon’s integrity, the presence of any rerupture, or the development of adhesions.
Depending on the cause of failure, treatment options range from non-surgical approaches like intensive physiotherapy and splinting to re-operative surgery. If the tendon has reruptured, a revision surgery might be necessary, possibly involving a different tendon graft or a modified surgical technique. If adhesions are the primary cause, surgical lysis (breaking up adhesions) combined with careful postoperative rehabilitation is essential. Sometimes, a secondary tendon transfer using an alternative tendon might be needed. In cases of severe failure or lack of response to treatment, a more extensive reconstructive procedure might become necessary, such as a joint fusion or arthrodesis. Throughout the process, open communication with the patient regarding expectations and realistic outcomes is paramount.
Q 9. What imaging modalities are used to assess tendon injuries and guide surgical planning?
Imaging plays a critical role in assessing tendon injuries and guiding surgical planning for tendon transfers. Several modalities are employed, each with its strengths and limitations.
- Ultrasound: This is often the first-line imaging technique. It’s readily available, relatively inexpensive, and allows for real-time assessment of tendon morphology, including thickness, echogenicity (brightness on the image), and the presence of tears or abnormalities. Doppler ultrasound can also assess blood flow within the tendon, crucial for assessing viability.
- Magnetic Resonance Imaging (MRI): MRI provides superior soft tissue contrast, allowing detailed visualization of tendon structure, surrounding tissues, and any associated injuries like muscle tears or nerve damage. It’s particularly useful in identifying subtle tears or assessing the extent of adhesions. Different sequences (T1-weighted, T2-weighted) can provide different information.
- Computed Tomography (CT) scans: While less commonly used for isolated tendon injuries, CT scans can be helpful in complex cases, especially when assessing bony abnormalities or fractures that might be contributing to the tendon issue. CT arthrography (injecting contrast into the joint) can improve visualization of joint structures and tendon insertions.
The choice of imaging modality depends on the clinical suspicion, availability of resources, and the specific information needed for surgical planning. For example, a straightforward tendon rupture might only require ultrasound, while a complex case with suspected nerve involvement might warrant an MRI.
Q 10. Explain the concept of tenodesis.
Tenodesis refers to a surgical procedure where a tendon is surgically attached to a bone. Unlike a tendon transfer, which reroutes a tendon to a new insertion site to restore a lost function, tenodesis aims to stabilize a joint. This is achieved by using the passive tension in the tendon to restrict or limit the joint’s movement. It’s often used to correct instability or improve joint mechanics. A classic example is the tenodesis effect in the wrist, where flexing the wrist passively extends the fingers and vice-versa. This is due to the passive tension of the wrist flexors and extensors on the finger tendons.
In surgical practice, tenodesis is often employed to augment or reinforce existing tendons or to provide stability in situations where primary tendon repair is not feasible or desirable. For example, tenodesis could be used to improve grip strength in a patient with weakened finger extensors. The technique requires precise surgical placement of the tendon to the bone to achieve the desired effect, and rehabilitation plays a critical role in optimizing the functional outcome.
Q 11. Discuss different types of tendon grafts used in tendon transfers.
The choice of tendon graft in a tendon transfer depends on several factors, including the size of the defect, the recipient tendon’s strength requirements, and the availability of suitable donor tendons. Several types of grafts are commonly used:
- Autografts: These are harvested from the patient’s own body, minimizing the risk of rejection and disease transmission. Common autograft sources include the palmaris longus tendon, the plantaris tendon, or portions of other less-critical tendons. The choice depends on the recipient tendon’s size and functional requirements.
- Allografts: These are harvested from a deceased donor. They eliminate the need for a second surgical site for graft harvesting but carry a slightly higher risk of disease transmission, although rigorous screening processes significantly mitigate this risk. Allografts are often processed to reduce immunogenicity.
- Synthetic grafts: Synthetic materials are sometimes used as tendon grafts, offering advantages in terms of ready availability and consistent properties. However, they may not always integrate as well with the recipient tissue, potentially leading to a higher risk of rupture or inflammation. The long-term durability of synthetic grafts may also be a consideration.
The decision regarding the type of graft is made on a case-by-case basis after a thorough evaluation of the patient’s specific needs and the available resources. The surgeon carefully considers the advantages and disadvantages of each graft type to optimize the chances of a successful outcome.
Q 12. How do you address adhesion formation after tendon transfer?
Adhesion formation is a significant complication after tendon transfer surgery. Adhesions are bands of scar tissue that bind the tendon to the surrounding tissues, restricting its movement and causing stiffness and pain. Prevention and management of adhesions are critical for a successful outcome.
Prevention strategies include meticulous surgical technique to minimize trauma to surrounding tissues, use of appropriate surgical lubricants, and the careful placement of drains to reduce post-operative swelling. Post-operative rehabilitation is crucial and involves carefully planned exercises to promote gliding of the tendon within its sheath and prevent adhesion formation. Early, controlled mobilization is generally preferred to minimize the risk of adhesions.
If adhesions develop despite preventative measures, various treatments are available. These might include physiotherapy focusing on mobilization techniques, and sometimes, surgical intervention may be necessary to lyse (break up) the adhesions. This procedure is often done arthroscopically, a minimally invasive technique that reduces scarring and recovery time. Following adhesion lysis, intensive rehabilitation is crucial to prevent recurrence.
Q 13. What are the potential long-term consequences of a tendon transfer?
Long-term consequences of tendon transfers can vary significantly depending on factors such as the type of surgery, patient compliance with rehabilitation, and the overall health of the patient. Some potential long-term consequences include:
- Tendon rupture: Though less common with proper surgical technique and rehabilitation, rupture can occur, especially with high-demand activities.
- Chronic pain: Persistent pain is a possibility, potentially due to adhesions, nerve irritation, or other complications.
- Limited range of motion: Despite rehabilitation, some limitation in joint movement can persist.
- Weakness: The transferred tendon may not fully restore pre-injury strength.
- Donor site morbidity: If an autograft was used, some weakness or discomfort might persist at the donor site.
Regular follow-up appointments are essential to monitor the patient’s progress and address any complications that might arise. Open communication between the surgeon and the patient regarding expectations and potential long-term outcomes is critical.
Q 14. How do you assess the functional outcome of a tendon transfer?
Assessing the functional outcome of a tendon transfer requires a multi-faceted approach involving subjective and objective measurements.
Subjective measures typically include patient-reported outcome measures (PROMs), such as questionnaires assessing pain levels, range of motion, functional ability, and overall satisfaction. These questionnaires are valuable in capturing the patient’s experience and perspective.
Objective measures involve clinical assessments of range of motion using goniometry (measuring angles), strength testing using dynamometry (measuring force), and functional assessments using standardized tests specific to the affected limb (e.g., grip strength, pinch strength, dexterity tests). In addition, imaging techniques such as ultrasound can be used to assess tendon excursion and rule out complications such as rerupture or adhesions.
Combining subjective and objective measures provides a comprehensive picture of the functional outcome. This information is crucial for evaluating the success of the surgery, guiding further rehabilitation, and informing future surgical strategies. Longitudinal follow-up is essential to assess the durability of the outcome over time.
Q 15. Describe your experience with different surgical approaches to tendon transfer.
Surgical approaches to tendon transfer are tailored to the specific needs of each patient and the location of the tendon transfer. The fundamental goal is to obtain a robust, tension-free transfer with optimal biomechanical alignment. Common approaches include open techniques and minimally invasive techniques.
- Open Techniques: These offer excellent visualization of the anatomy, allowing precise dissection and suture placement. This is often necessary for complex transfers involving multiple tendons or significant scarring. For example, a classic wrist extensor transfer for radial nerve palsy may require a relatively extensive open approach to identify and prepare the donor and recipient tendons.
- Minimally Invasive Techniques: These utilize smaller incisions and often employ specialized instruments, aiming to reduce trauma and improve cosmetic outcomes. Arthroscopy can play a role in some transfers, especially those involving intra-articular structures. However, limited visualization can make these techniques challenging for complex cases. A good example is the use of smaller incisions in performing an FCU transfer for wrist flexion weakness.
The choice between open and minimally invasive techniques depends on factors such as the complexity of the case, the surgeon’s expertise, and the patient’s individual circumstances.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Compare and contrast different types of tendon fixation devices.
Tendon fixation devices play a critical role in the success of a tendon transfer. The choice depends on several factors, including the tendon’s size, the recipient site, and the surgeon’s preference.
- Suture Techniques: These remain the gold standard, with various techniques like Kessler, Bunnell, and modified Krackow sutures used depending on the tendon size and strength required. The simplicity and versatility of sutures makes them very commonly used.
- Bioabsorbable anchors: These are small anchors made of materials like polylactic acid (PLA) or polyglycolic acid (PGA) that are gradually absorbed by the body. They’re particularly useful in small tendons or where bone tunnels are difficult to create.
- Metallic anchors: These offer superior initial strength but require a separate procedure for removal in some cases. They’re often preferred in larger tendons or situations requiring significant initial fixation strength.
- Buttons and staples: These are used primarily for larger tendons and offer a good balance of strength and ease of use. However, the potential for irritation or prominence in the skin can be a consideration.
The ideal device provides secure fixation with minimal risk of complications such as tendon rupture, implant failure, or irritation.
Q 17. What are the advantages and disadvantages of using different types of suture materials for tendon repair?
Suture material selection significantly impacts the healing process and overall outcome of a tendon transfer.
- Absorbable sutures: These dissolve over time, eliminating the need for suture removal. However, they can lose strength before sufficient tendon healing occurs, and the absorption rate can vary significantly depending on the material (e.g., Vicryl, PDS).
- Non-absorbable sutures: These provide long-term strength, but require removal, adding another step to the procedure. Common choices include nylon or polypropylene. These can offer better long-term strength than absorbable alternatives.
Choosing the right suture material involves a trade-off between strength, absorption rate, and the risk of infection or reaction. The surgeon typically considers the size of the tendon, the patient’s overall health, and the expected healing time.
For instance, a larger tendon requiring significant initial strength might be repaired with strong non-absorbable sutures, while smaller tendons could potentially utilize absorbable materials. The decision always considers the balance of risks and benefits in the individual patient.
Q 18. Explain your understanding of the biomechanics of tendon healing.
Tendon healing is a complex process involving multiple stages. Initially, a blood clot forms at the repair site (hematoma phase). This is followed by an inflammatory phase, characterized by the migration of inflammatory cells to the area. Fibroblasts then proliferate, producing collagen, which provides the initial structural support (proliferative phase). Finally, the collagen matures and remodels, increasing the strength and organization of the tendon (remodeling phase).
Biomechanically, the initial stages are characterized by low tensile strength, gradually increasing as collagen matures. Early motion is crucial to guide the remodeling process and prevent adhesion formation, but it must be carefully balanced against the risk of disrupting the healing tendon. Understanding the biomechanics is critical in designing appropriate rehabilitation protocols.
For example, early passive range of motion may be incorporated after transfer to optimize the direction of collagen fiber alignment and prevent contractures, but aggressive active range of motion will be delayed to protect the repair site until adequate strength develops.
Q 19. How do you address patient expectations and manage potential complications during the pre-operative consultation?
Pre-operative consultations are crucial for setting realistic expectations and addressing potential complications. I begin by thoroughly explaining the procedure, including its benefits, risks, and limitations, using clear and simple language. I present realistic timelines for recovery, including potential setbacks.
I discuss potential complications, such as infection, tendon rupture, adhesion formation, and nerve injury, explaining their likelihood and management strategies. I also emphasize the importance of patient adherence to the post-operative rehabilitation protocol, as this significantly impacts the outcome. Visual aids, such as anatomical diagrams and previous patient outcome photos, can also help improve understanding.
For example, if a patient has unrealistic expectations of a complete return to pre-injury activity level, I’ll adjust their expectations by explaining that functional recovery may take longer than they anticipated. The detailed explanation also helps to manage patient anxiety around possible complications. Open and honest communication builds trust and facilitates a successful surgical outcome.
Q 20. What are some alternative treatments to tendon transfer?
Alternatives to tendon transfer exist, and the choice depends on the specific condition and the patient’s overall health and functional goals.
- Conservative Management: This may involve physical therapy, splinting, or medication to manage pain and inflammation. It’s often the first approach in less severe cases or when surgical risk is significant.
- Tenolysis: This involves surgically releasing adhesions around the existing tendon to restore movement. It is appropriate if there are adhesions and the tendon still retains some function.
- Tendon Grafting: This involves replacing a damaged section of tendon with a graft, often using autologous tissue (from the patient’s own body) or allograft (donor tissue). This is often considered when the tendon itself is severely damaged and cannot be repaired directly.
- Orthoses and assistive devices: In some cases, functional improvement can be achieved without surgery through the use of braces or assistive devices which will help compensate for limited tendon function.
The decision to pursue surgery versus a non-surgical approach should be made on a case-by-case basis, taking into consideration all potential risks and benefits.
Q 21. Discuss the role of advanced imaging techniques in preoperative planning for tendon transfers.
Advanced imaging techniques play a vital role in pre-operative planning for tendon transfers. These help to precisely assess the condition of the tendons, muscles, nerves, and bones involved.
- High-resolution ultrasound: This is a non-invasive method used to visualize tendon structure, identify tears, assess muscle bulk, and measure tendon length. It helps assess the quality of donor and recipient tendons prior to the procedure.
- Magnetic resonance imaging (MRI): MRI provides more detailed images of soft tissues, including tendons, muscles, and nerves. It is particularly useful in identifying subtle lesions or determining the extent of muscle atrophy.
- Computed tomography (CT) scans: Although less frequently used for tendon assessment itself, CT scans can be helpful for visualizing bone anatomy in complex cases, particularly when bone tunnels are required to secure the transferred tendon.
These imaging techniques facilitate precise surgical planning, enabling the surgeon to select appropriate donor tendons, optimize the transfer technique, and predict the potential outcome. For example, MRI can identify the presence of significant fatty infiltration within the target muscle, informing the decision of the potential for a successful transfer. This detailed information improves the precision and success of the surgery.
Q 22. How do you manage patients with complex combined tendon and nerve injuries?
Managing patients with complex combined tendon and nerve injuries requires a multidisciplinary approach and a meticulous surgical strategy. The key is to prioritize nerve repair before addressing tendon issues. Nerve repair is often more time-sensitive, and its success significantly impacts the functional outcome of the tendon transfer. We carefully assess the extent of both nerve and tendon damage, using electrodiagnostic studies (EMG/NCS) and high-resolution ultrasound or MRI. This detailed assessment guides the surgical plan.
The surgical approach is staged. We typically begin with nerve repair using microsurgical techniques whenever possible, ensuring optimal alignment and tension. This might involve nerve grafting for significant nerve defects. After a period of nerve regeneration (often several months), we proceed with tendon transfer. The choice of donor tendon, the recipient site, and the surgical technique are carefully selected based on the patient’s specific anatomy and functional goals. Post-operative rehabilitation is crucial, emphasizing both nerve recovery and tendon gliding. Regular follow-up appointments, including clinical evaluations and imaging studies, allow us to monitor progress and address any complications.
For instance, in a patient with a combined median nerve laceration and flexor tendon injury in the forearm, we would first perform microsurgical repair of the median nerve. After a period of recovery, we might perform a tendon transfer using the palmaris longus tendon to restore flexion of the thumb. The timing of these interventions is critical for optimal outcomes.
Q 23. Describe your experience with minimally invasive techniques for tendon transfer.
Minimally invasive techniques for tendon transfer offer several advantages, including reduced surgical trauma, smaller incisions, less post-operative pain, and faster recovery. I’ve extensively utilized endoscopic techniques and smaller-incision open approaches. Endoscopic tendon transfers allow for precise tendon mobilization and routing through small incisions, minimizing damage to surrounding tissues. This is particularly beneficial in cases where preserving the vascular supply of the donor tendon is crucial.
However, minimally invasive techniques aren’t always suitable. Their application depends on the complexity of the injury, the location of the tendons, and the patient’s specific anatomy. For instance, in cases of complex tendon injuries requiring extensive repair or in patients with significant scarring, a more traditional open approach might be necessary. The choice of minimally invasive versus open surgery is always individualized, taking into account the specific advantages and limitations of each approach. I regularly utilize ultrasound guidance during minimally invasive procedures to aid in precise tendon identification and placement.
Q 24. How do you adapt surgical techniques for pediatric patients requiring tendon transfers?
Surgical techniques for pediatric patients requiring tendon transfers differ significantly from those used in adults. Children have smaller tendons, more pliable tissues, and ongoing growth, all factors requiring careful consideration. Smaller incisions are used to minimize scarring and potential growth plate disruption. We utilize fine sutures and microsurgical instruments to handle delicate tissues. The use of absorbable sutures helps to avoid the need for subsequent suture removal. Furthermore, we meticulously plan for the ongoing growth of the child, ensuring that the tendon transfer will remain functional as the child grows. This often requires specific tendon lengthening procedures in some instances.
For example, in a child with congenital absence of a thumb muscle, the surgical plan involves careful consideration of the child’s age and growth potential. We might choose a tendon transfer that allows for growth accommodation, thereby avoiding future revisions. The postoperative rehabilitation program also emphasizes growth monitoring and potential adjustments to maintain functional movement throughout development.
Q 25. Discuss the challenges in managing tendon transfers in patients with comorbidities such as diabetes or rheumatoid arthritis.
Patients with comorbidities such as diabetes or rheumatoid arthritis present significant challenges in tendon transfer surgery. Diabetes impairs wound healing, increases the risk of infection, and reduces tendon strength. Preoperative optimization of blood glucose control is crucial to minimize these risks. We often consult with endocrinology to ensure optimal metabolic management pre and post-op. In rheumatoid arthritis, inflammation and joint destruction can significantly impair tendon function and healing. We may need to address underlying joint pathology before undertaking the tendon transfer.
Surgical techniques might need to be modified. For instance, we might use advanced closure techniques to promote wound healing in diabetic patients and utilize antibiotic prophylaxis to reduce infection risk. In patients with rheumatoid arthritis, we might employ joint-preserving techniques alongside the tendon transfer to address the underlying inflammatory process. Post-operative rehabilitation will focus on optimizing tendon gliding, preventing stiffness, and managing inflammation. The collaboration with rheumatology and diabetes specialists is crucial for the success of these complex cases.
Q 26. How do you evaluate and manage postoperative pain in tendon transfer patients?
Post-operative pain management in tendon transfer patients is critical for successful rehabilitation. A multimodal approach is essential, combining pharmacological and non-pharmacological methods. This typically involves a combination of regional anesthesia (such as nerve blocks), opioids for acute pain relief, and non-steroidal anti-inflammatory drugs (NSAIDs) to manage inflammation. We emphasize the importance of minimizing opioid use to avoid potential side effects.
Beyond pharmacological interventions, we incorporate physical therapy and occupational therapy early in the recovery process, focusing on gentle range of motion exercises to prevent stiffness and promote tendon gliding. Pain management education and patient empowerment are integral parts of our approach. We regularly assess pain levels and adjust the treatment plan accordingly. Using validated pain scales helps in objective monitoring and personalized management of postoperative pain. We also address psychological aspects of pain, offering coping strategies and emotional support when needed.
Q 27. What are the ethical considerations surrounding tendon transfer procedures?
Ethical considerations in tendon transfer procedures revolve around patient autonomy, informed consent, and the balance of risks and benefits. Patients must fully understand the procedure, its potential benefits and risks, and alternative treatment options. Detailed discussions about potential complications, rehabilitation needs, and the likelihood of achieving functional goals are essential components of the informed consent process. We must ensure the patient’s decision is voluntary and not coerced.
Surgeons also have a responsibility to select the most appropriate procedure and technique. In some cases, resource allocation might create ethical dilemmas, especially when faced with limited resources or complex cases with low chances of success. In these instances, open communication with the patient and their family is paramount. Transparent discussion about realistic expectations and alternative treatment options is crucial in making ethically sound decisions. We must strive to avoid unnecessary procedures or those that could potentially cause more harm than benefit.
Q 28. Describe a challenging case you encountered involving a tendon transfer and how you addressed it.
One particularly challenging case involved a young musician who sustained a severe brachial plexus injury resulting in complete paralysis of the right arm. Traditional tendon transfers wouldn’t restore meaningful function. The patient’s primary goal was to regain the ability to play the violin. After extensive discussion, we explored a complex multi-stage approach that included free functional muscle transfer from the contralateral leg (using the gracilis muscle), combined with nerve transfers and carefully planned tendon transfers.
The procedure was technically demanding and required significant microsurgical expertise. Post-operatively, the patient underwent an intensive rehabilitation program tailored to restoring fine motor control needed for violin playing. While full recovery wasn’t achieved, the patient successfully regained enough function to play simple melodies, fulfilling their primary functional goal. The case highlighted the need for innovative surgical strategies, meticulous planning, patient-centered goals, and long-term commitment to rehabilitation in addressing challenging cases of peripheral nerve and tendon injuries.
Key Topics to Learn for Tendon Transfers Interview
- Anatomy and Biomechanics: Understand the structure and function of tendons, muscles, and surrounding tissues involved in tendon transfer procedures. Explore the biomechanical principles governing tendon gliding and force transmission.
- Surgical Techniques: Familiarize yourself with different tendon transfer techniques, including harvesting, preparation, and implantation methods. Consider the advantages and disadvantages of various approaches.
- Indications and Contraindications: Master the criteria for selecting appropriate candidates for tendon transfer surgery. Understand the situations where this procedure is not suitable.
- Post-operative Management: Learn about the rehabilitation protocols, including physical therapy and occupational therapy, necessary for successful tendon healing and functional recovery. Understand potential complications and their management.
- Clinical Assessment: Develop proficiency in evaluating patients pre- and post-operatively, including range of motion assessments, strength testing, and functional evaluations. Understand how to interpret clinical findings.
- Problem-Solving: Practice diagnosing potential complications and developing solutions. Consider scenarios where unexpected issues arise during surgery or rehabilitation.
- Current Research and Trends: Stay updated on the latest advancements in tendon transfer techniques, materials, and rehabilitation strategies. Understanding emerging research demonstrates your commitment to the field.
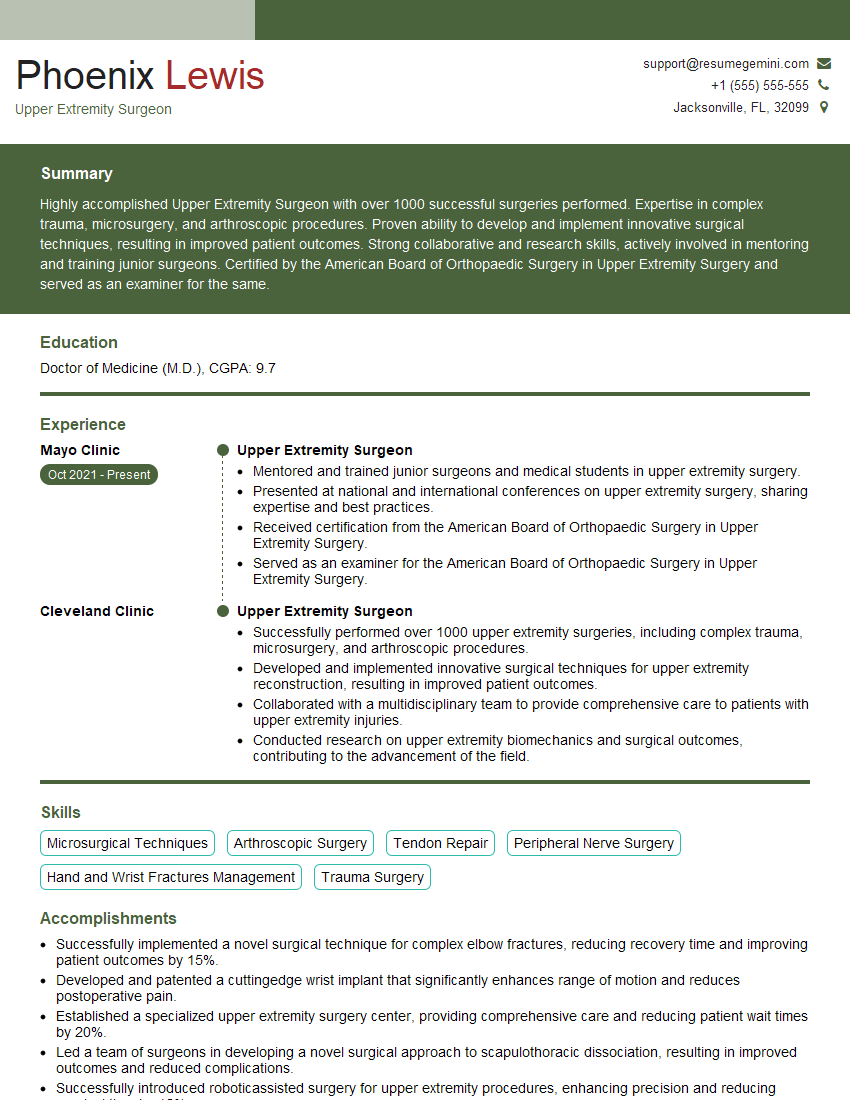
Next Steps
Mastering the intricacies of tendon transfers significantly enhances your career prospects in orthopedics and hand surgery. A strong understanding of these techniques is highly valued by employers and demonstrates a commitment to patient care and advanced surgical skills. To maximize your chances of securing your dream role, it’s crucial to present your qualifications effectively. Building an ATS-friendly resume is essential in navigating the modern job market. We strongly encourage you to leverage ResumeGemini, a trusted resource for creating professional and impactful resumes. Examples of resumes tailored to highlight experience and expertise in Tendon Transfers are available below to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.