Preparation is the key to success in any interview. In this post, we’ll explore crucial Thoracostomy interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Thoracostomy Interview
Q 1. Describe the indications for performing a thoracostomy.
Thoracostomy, or chest tube insertion, is a life-saving procedure indicated when there’s a buildup of air or fluid in the pleural space (the area between the lung and the chest wall). This buildup, known as a pneumothorax (air) or hemothorax (blood), or even a pleural effusion (fluid), can compromise lung function and even lead to respiratory failure. Specific indications include:
- Tension pneumothorax: A life-threatening condition where air enters the pleural space but cannot escape, causing a collapse of the lung and compression of the heart and major vessels.
- Hemothorax: Significant bleeding into the pleural space, often following trauma such as a rib fracture or penetrating injury. The amount of blood loss dictates the urgency of intervention.
- Pneumothorax (simple or spontaneous): A collapsed lung due to air in the pleural space. While some small pneumothoraces can be managed conservatively, larger ones requiring drainage necessitate a thoracostomy.
- Pleural effusion: An accumulation of fluid in the pleural space, often due to infections, heart failure, cancer, or other medical conditions. If the fluid is large enough to compromise lung function, a thoracostomy may be necessary.
- Empyema: A collection of pus in the pleural space, typically requiring drainage via a chest tube.
- Post-operative drainage: Following thoracic surgery, a chest tube is routinely placed to drain fluid, blood, or air from the surgical site to prevent complications.
In essence, thoracostomy is performed to restore negative pressure in the pleural space, allowing the lung to re-expand and improve respiratory function. The decision to perform a thoracostomy is based on clinical assessment, chest X-ray findings, and the patient’s overall condition.
Q 2. Explain the different types of thoracostomy tubes and their applications.
Several types of chest tubes exist, each designed for specific applications:
- Single-lumen chest tubes: These are the most common type, used for draining air or fluid. They have one opening at the end for drainage.
- Double-lumen chest tubes: These tubes have two separate lumens, one for draining fluid and another for venting air. This design is particularly useful in managing a pneumothorax with an associated pleural effusion.
- Triple-lumen chest tubes: Less frequently used, these tubes have three lumens, allowing for simultaneous drainage of fluid and air, as well as irrigation of the pleural space. This is sometimes necessary in complex situations such as empyema.
The choice of tube depends on the specific clinical scenario. For example, a single-lumen tube is sufficient for a simple pneumothorax, while a double-lumen tube is often preferred for a pneumothorax with a hemothorax. The surgeon will select the appropriate type based on the patient’s needs and the anticipated drainage requirements.
Q 3. Detail the steps involved in inserting a chest tube.
Chest tube insertion is a sterile procedure, typically performed under local anesthesia or sedation, sometimes general anesthesia for complex cases. The steps broadly include:
- Preparation: The patient’s skin is prepared and draped sterily. The insertion site (usually the 5th intercostal space in the mid-axillary line) is identified using anatomical landmarks.
- Incision: A small incision is made through the skin and subcutaneous tissue.
- Blunt dissection: Using blunt instruments, a path is created through the intercostal muscles to reach the pleural space.
- Tube insertion: The chest tube is inserted into the pleural space and advanced to the desired location, guided by fluoroscopy or ultrasound in many cases.
- Attachment and stabilization: The chest tube is connected to underwater drainage system and secured to the chest wall with sutures or clips to prevent displacement.
- Dressing: An airtight dressing is applied to seal the insertion site and prevent air leaks.
- Confirmation: A chest x-ray is obtained to confirm proper tube placement and expansion of the lung.
Throughout the procedure, strict sterile technique is crucial to minimize the risk of infection. The process is highly dependent on the specific situation and may vary based on the surgeon’s preference and the patient’s condition.
Q 4. How do you select the appropriate size and location for a chest tube insertion?
The selection of tube size and location is crucial for effective drainage and to minimize complications.
Tube Size: This is determined by the anticipated drainage volume and the viscosity of the fluid. Larger tubes (e.g., 28-36 French) are used for significant bleeding or large amounts of fluid, while smaller tubes (e.g., 12-20 French) are suitable for air drainage or smaller effusions. The surgeon carefully weighs the risk of bleeding vs. adequate drainage.
Tube Location: The insertion site is selected based on the location of the fluid or air collection. For example, a pneumothorax high in the lung may require a higher insertion site. The 5th intercostal space in the mid-axillary line is a common location because it is generally accessible and provides sufficient drainage access. However, this may need to change depending on the clinical scenario. Use of imaging guides tube placement to minimize risk of complications.
Ultimately, the appropriate size and location are determined by the surgeon’s clinical judgment, guided by imaging techniques like chest X-rays or ultrasound, ensuring optimal drainage and minimal trauma to the patient.
Q 5. What are the potential complications of a thoracostomy procedure?
Thoracostomy, while a life-saving procedure, carries potential complications, including:
- Bleeding: Bleeding at the insertion site or into the pleural space is a significant concern, especially in patients with coagulopathies.
- Infection: Infection at the insertion site or in the pleural space (empyema) is a risk, particularly with prolonged drainage.
- Lung injury: Accidental puncture of the lung during insertion can cause a pneumothorax or hemothorax.
- Air leaks: Air can leak around the chest tube, delaying lung re-expansion and requiring additional management.
- Subcutaneous emphysema: Air can leak into the subcutaneous tissues, causing swelling and crepitus.
- Re-expansion pulmonary edema: Rapid re-expansion of the lung can cause fluid to leak into the alveoli, leading to pulmonary edema.
- Cardiac injury: Accidental injury to the heart or major vessels is a rare but serious complication.
Careful technique, meticulous attention to sterile practices, and appropriate patient selection can significantly reduce these risks. Post-operative monitoring of the patient is essential for early detection and management of any potential complication.
Q 6. How do you manage air leaks after thoracostomy?
Air leaks after thoracostomy are common and often resolve spontaneously. Management strategies include:
- Observation: Small, resolving air leaks may only require close observation and monitoring of the drainage system.
- Chest tube clamping: Temporary clamping of the chest tube can help assess whether the air leak is resolving or persistent. However, this is not a long-term solution and should only be done under medical supervision.
- Tube repositioning: If the air leak is substantial or persistent, the chest tube may need to be repositioned to ensure it is effectively sealing the leak.
- Surgical intervention: In some cases, particularly with persistent large air leaks, surgical intervention such as video-assisted thoracoscopic surgery (VATS) may be required to identify and address the source of the leak.
- Positive pressure ventilation: During mechanical ventilation, appropriate pressure settings can enhance lung re-expansion and reduce air leaks.
The specific management strategy will depend on the size of the leak, the patient’s overall condition, and the underlying cause. Continuous monitoring of the drainage system, including the amount and character of drainage, and careful assessment of the patient’s respiratory status are crucial for effective management.
Q 7. Describe the management of a bleeding thoracostomy tube.
Bleeding from a thoracostomy tube is a serious complication that requires immediate attention. Management depends on the severity of the bleeding:
- Mild bleeding: This may manifest as a small amount of blood in the drainage system. Monitoring the drainage volume and character is essential; if the bleeding is worsening, intervention may be needed.
- Significant bleeding: A large amount of blood in the drainage system indicates the need for immediate intervention. This can range from replacing the chest tube to more aggressive measures such as surgical exploration and control of the bleeding source.
- Massive bleeding: This is a life-threatening emergency requiring immediate resuscitation, including fluid resuscitation and blood transfusion, and prompt surgical intervention to control the bleeding source. This may involve going back into the chest cavity to locate and cauterize the bleeding site.
The management of bleeding should be tailored to the patient’s hemodynamic status and the overall clinical picture. Close monitoring, prompt intervention, and potentially surgical exploration to control the source of bleeding are crucial in managing this potentially fatal complication.
Q 8. Explain the process of removing a chest tube.
Removing a chest tube is a crucial procedure requiring meticulous attention to detail and aseptic technique. It’s typically performed when the lung has re-expanded, drainage is minimal, and the patient is clinically stable. The process involves:
- Assessment: Thorough assessment of the patient, including respiratory status, vital signs, and drainage characteristics.
- Preparation: Gathering necessary supplies, including sterile gloves, forceps, an occlusive dressing, and a sterile petroleum gauze.
- Patient Education: Explaining the procedure to the patient, addressing any concerns or anxieties.
- Procedure: The tube is quickly removed while the patient performs a Valsalva maneuver (holding breath and bearing down) to prevent air entry into the pleural space. This maneuver helps to maintain negative intrapleural pressure. Immediately after removal, a sterile occlusive dressing is applied firmly to the site.
- Post-removal Monitoring: Close monitoring of the patient’s respiratory status, including auscultation of lung sounds and monitoring of oxygen saturation, is essential to detect any complications such as pneumothorax or re-accumulation of fluid.
Think of it like slowly pulling out a plug from a bathtub – you want to minimize the disturbance to the water (air) level.
Q 9. What are the post-operative nursing considerations for a patient with a thoracostomy tube?
Post-operative nursing care for a patient with a thoracostomy tube is vital for preventing complications and promoting healing. Key considerations include:
- Respiratory Assessment: Frequent monitoring of respiratory rate, rhythm, depth, breath sounds, and oxygen saturation. Look for signs of respiratory distress like increased work of breathing, cyanosis or use of accessory muscles.
- Drainage Monitoring: Regularly monitoring the amount, color, and character of the drainage. A sudden increase or change in drainage can indicate a problem.
- Tube Management: Maintaining the integrity of the drainage system, ensuring that connections are secure and the drainage system is functioning correctly. Never clamp the tube unless specifically ordered by the physician.
- Pain Management: Assessing and managing pain using appropriate analgesics and non-pharmacological methods. Pain can impede deep breathing and coughing, increasing the risk of complications.
- Patient Education: Educating the patient and family about the purpose of the tube, potential complications, and what to watch for. Include instructions on deep breathing, coughing, and incentive spirometry.
- Wound Care: Monitoring the insertion site for signs of infection, such as redness, swelling, drainage, or increased tenderness.
Imagine it as being a dedicated guardian, constantly vigilantly checking on the patient’s vital signs and the integrity of the system, akin to a life support system.
Q 10. How do you monitor for complications after a thoracostomy?
Monitoring for complications after a thoracostomy is critical for early intervention and improved patient outcomes. Potential complications include:
- Pneumothorax: A collapsed lung, indicated by decreased breath sounds, respiratory distress, and possibly a tension pneumothorax requiring immediate needle decompression.
- Hemothorax: Blood in the pleural space, indicated by bloody drainage, decreased hematocrit, and signs of hypovolemia.
- Infection: Signs of infection at the insertion site, such as redness, swelling, purulent drainage, or fever.
- Air Leaks: Persistent air bubbling in the water-seal chamber indicates an ongoing air leak. Continuous bubbling may suggest a significant leak requiring attention.
- Tube Obstruction: Decreased or absent drainage can signify an obstruction that may need to be addressed.
Imagine the chest tube as a crucial drainage system; any malfunction warrants immediate action to avoid catastrophic events.
Q 11. What are the radiological findings indicative of a successful thoracostomy?
Radiological findings indicative of a successful thoracostomy include:
- Complete Lung Expansion: Chest X-ray demonstrating full lung expansion, without evidence of pneumothorax or significant pleural fluid.
- Absence of Pleural Effusion: No visible accumulation of fluid in the pleural space.
- Appropriate Tube Placement: The chest tube should be correctly positioned within the pleural space, avoiding injury to adjacent structures.
The chest X-ray acts as a visual confirmation that the procedure was effective in restoring normal lung function.
Q 12. Explain the difference between a closed and open thoracostomy.
The difference lies primarily in the surgical approach:
- Closed Thoracostomy: A less invasive procedure where the chest tube is inserted using a trocar or needle, creating a small incision. This approach is typically used for drainage of pleural fluid or small pneumothoraces.
- Open Thoracostomy: A more invasive procedure requiring a larger incision to allow for direct visualization of the pleural space. This is often necessary for larger collections of fluid or air, or in situations requiring more extensive surgical exploration.
Imagine the difference between a small puncture for a blood draw (closed) versus a surgical incision for a major operation (open).
Q 13. Describe the role of suction in managing a thoracostomy.
Suction plays a vital role in managing a thoracostomy by removing air and fluid from the pleural space, promoting lung re-expansion. The level of suction is carefully controlled by the physician, usually using a water-seal system. This system prevents air from re-entering the pleural space while facilitating drainage. The water seal chamber fluctuates with respirations due to the negative pressure within the pleural space, indicating proper lung function and tube patency.
Think of suction as a vacuum cleaner, efficiently removing unwanted substances from the pleural cavity.
Q 14. How do you troubleshoot a malfunctioning thoracostomy drainage system?
Troubleshooting a malfunctioning thoracostomy drainage system requires a systematic approach:
- Assess the Drainage: Check the amount, color, and character of the drainage. Decreased or absent drainage could indicate an obstruction.
- Inspect the Tubing: Examine the tubing for kinks, clots, or disconnections. Gently unkink any kinks, but avoid milking the tube.
- Check the Suction: Verify that the suction is functioning correctly. Fluctuations in the water-seal chamber during respiration indicate patency.
- Assess the Insertion Site: Examine the insertion site for signs of bleeding, infection, or displacement of the tube.
- Consider Air Leaks: Continuous bubbling in the water-seal chamber suggests an air leak. This may indicate a larger problem that requires attention.
- Notify the Physician: If the problem cannot be resolved, or if there are signs of significant complications, immediately notify the physician.
Troubleshooting requires meticulous attention to detail, systematically checking each component of the system to identify the source of malfunction.
Q 15. What are the signs and symptoms of a tension pneumothorax?
Tension pneumothorax is a life-threatening condition where air accumulates in the pleural space, creating a pressure gradient that collapses the lung and compromises venous return to the heart. The symptoms are often dramatic and rapidly progressive.
- Severe respiratory distress: This is the hallmark symptom, characterized by rapid, shallow breathing (tachypnea), shortness of breath (dyspnea), and use of accessory muscles for breathing.
- Hypotension: Due to decreased venous return, the patient will experience a drop in blood pressure.
- Tachycardia: The heart races to compensate for the decreased blood pressure and oxygen levels.
- Tracheal deviation: The trachea (windpipe) may shift away from the affected side due to the pressure exerted by the trapped air.
- Distended neck veins (JVD): Increased pressure in the chest impedes venous return to the heart, leading to distended jugular veins.
- Absent breath sounds on the affected side: As the lung collapses, air entry is diminished or absent.
- Subcutaneous emphysema: Air may leak into the subcutaneous tissues, causing a crackling sensation under the skin (crepitus), particularly around the clavicle and neck.
Imagine a balloon inflating inside a sealed container – the pressure builds, affecting everything around it. That’s similar to what happens in a tension pneumothorax.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you manage a tension pneumothorax?
Management of a tension pneumothorax is a true emergency. Immediate needle decompression is crucial, followed by definitive chest tube placement.
- Needle decompression: This is the immediate life-saving intervention. A large-bore (14-16 gauge) needle is inserted into the second intercostal space, mid-clavicular line, on the affected side. The needle is advanced into the pleural space, releasing the trapped air. This provides immediate relief of pressure.
- Chest tube insertion: Once the patient is stabilized, a chest tube is inserted through a more formal surgical approach, usually in the fifth intercostal space, mid-axillary line, to ensure proper drainage of air and fluid. The tube is connected to an underwater seal drainage system.
- Supplemental oxygen: Oxygen therapy is essential to improve oxygenation.
- Fluid resuscitation: IV fluids are administered to treat hypotension.
- Monitoring: Close monitoring of vital signs, breath sounds, and chest tube drainage is essential.
Think of it as a two-step process: a quick fix with the needle to buy time, followed by a more comprehensive solution with the chest tube.
Q 17. Explain the concept of water-seal drainage.
Water-seal drainage is a method of draining air and fluid from the pleural space using a closed system that prevents air from re-entering the chest cavity. It utilizes a one-way valve system.
The system typically consists of a chest tube connected to a collection chamber. The chamber is partially submerged in water, creating a water seal. Air can exit the pleural space through the tube and bubble up through the water, but cannot re-enter due to the water seal’s pressure. Fluctuation of the water column with respirations is a normal finding, indicating patency of the system.
Think of it like a one-way valve in a plumbing system: fluid can drain out, but nothing can flow back in.
Q 18. How do you assess the effectiveness of thoracostomy drainage?
Assessing the effectiveness of thoracostomy drainage involves several steps:
- Monitor drainage: Measure the amount and character of the drainage (blood, serosanguinous fluid, air) at regular intervals. Decreasing drainage volume is a positive sign.
- Assess respiratory status: Monitor respiratory rate, oxygen saturation, breath sounds, and the patient’s overall respiratory comfort. Improved respiratory function indicates effective drainage.
- Observe chest tube function: Ensure the water seal is functioning correctly (tidaling or fluctuation of the water column during respiration), and there are no air leaks in the system.
- Check for clinical improvement: Look for improvement in vital signs (heart rate, blood pressure), reduced respiratory distress, and the resolution of symptoms such as chest pain and dyspnea.
- Chest X-ray: A chest X-ray is crucial to confirm lung re-expansion and to check for any residual pneumothorax or other complications.
The goal is to see improvement in the patient’s clinical status and evidence of lung re-expansion on imaging.
Q 19. Discuss the role of ultrasound in guiding thoracostomy insertion.
Ultrasound guidance during thoracostomy insertion significantly improves the safety and efficacy of the procedure. It allows real-time visualization of the lung, pleural space, and surrounding structures, minimizing the risk of complications such as lung injury and intercostal vessel damage.
The ultrasound probe is used to identify the pleural space, confirm the placement of the needle or chest tube, and guide the insertion of the tube into the appropriate location. This technique reduces the number of blind attempts and increases the success rate of the procedure on the first attempt.
Think of it like having a roadmap for the procedure, avoiding unintended detours.
Q 20. What are the contraindications for performing a thoracostomy?
Contraindications for thoracostomy are relatively rare but include:
- Severe coagulopathy: Patients with severe bleeding disorders may be at increased risk of bleeding complications.
- Extensive emphysema: Severe subcutaneous emphysema can make it difficult to place the chest tube safely.
- Presence of a large pleural mass or adhesion: These can obstruct the drainage of air or fluid.
- Patient refusal: Informed consent is essential.
Careful assessment of the patient’s condition is paramount to determine suitability for the procedure.
Q 21. How do you handle accidental removal of a thoracostomy tube?
Accidental removal of a thoracostomy tube is an emergency requiring immediate action. The primary goal is to prevent the re-entry of air into the pleural space.
- Cover the insertion site: Immediately cover the insertion site with an occlusive dressing (e.g., petroleum gauze) to prevent air entry. This is the immediate life saving step.
- Assess the patient’s respiratory status: Monitor respiratory rate, oxygen saturation, and for signs of respiratory distress.
- Notify the surgical team: Contact the surgical team immediately for tube replacement.
- Supplemental oxygen: Provide supplemental oxygen.
- Prepare for potential re-insertion: The patient should be prepared for urgent re-insertion of the chest tube in the operating room.
Quick action is critical to prevent the recurrence of a pneumothorax.
Q 22. Describe the use of fibrinolytic agents in managing clots in the thoracostomy tube.
Fibrinolytic agents, such as tissue plasminogen activator (tPA), are sometimes used to break down clots obstructing thoracostomy tubes. This is typically reserved for situations where a clot is significantly impeding drainage and causing respiratory compromise. It’s crucial to understand that this isn’t a routine practice and carries risks. The decision to use fibrinolytic agents must be carefully weighed against the potential for bleeding complications.
For example, if a patient is experiencing a significant increase in respiratory distress despite aggressive suctioning of the thoracostomy tube and we suspect a large clot is the cause, we might consider using a fibrinolytic agent under strict monitoring. The procedure involves careful administration of the agent directly into the tube, followed by close observation for signs of bleeding or re-accumulation of fluid. It’s important to note that alternative methods, such as manual clot removal via irrigation, are often attempted first.
The use of fibrinolytic agents in this context is a highly specialized intervention and requires careful patient selection, close monitoring, and a thorough understanding of the potential benefits and risks.
Q 23. What are the differences in thoracostomy insertion techniques for adults versus children?
Thoracostomy insertion techniques differ between adults and children primarily due to anatomical differences. In adults, the procedure is typically performed under fluoroscopic guidance using a larger-caliber chest tube. The insertion site is often chosen based on the location of the pleural effusion or pneumothorax. The procedure is more straightforward due to the larger size and more easily palpable landmarks.
In children, however, the procedure requires more delicate technique due to their smaller size and more fragile anatomy. Smaller-caliber chest tubes are used, and the procedure may be performed under ultrasound or fluoroscopic guidance. The insertion site is chosen carefully to avoid vital structures. The procedure requires greater precision and attention to detail to minimize trauma to the surrounding tissues. The use of specific sized tubes tailored to the child’s body surface area is crucial.
Think of it like this: inserting a chest tube in an adult is like using a larger screwdriver on a larger screw, while performing the same procedure in a child is like using a smaller, more precise tool on a miniature screw.
Q 24. Explain the significance of measuring the drainage output from a thoracostomy tube.
Measuring thoracostomy tube drainage output is critical for monitoring the patient’s respiratory status and overall clinical progress. The amount and character of drainage—whether it’s serous (clear), sanguineous (bloody), or chylous (milky)—provide valuable information about the ongoing healing process and the potential for complications.
For instance, a large initial drainage volume might indicate a significant hemothorax or pneumothorax. A gradual decrease in drainage typically signals improvement, while a sudden increase could suggest bleeding or re-accumulation of fluid. The character of the fluid also informs us about underlying causes. Persistent bloody drainage might signify ongoing bleeding requiring intervention. Chylous drainage indicates a leak from the lymphatic system and requires specialized management.
Regular and meticulous documentation of drainage output—including volume and character—is essential for guiding clinical decision-making and ensuring optimal patient management. We use standardized charts to record this and use this information to adjust the treatment plan.
Q 25. Discuss the role of patient education in post-thoracotomy care.
Patient education is paramount in post-thoracotomy care. It significantly improves patient outcomes and reduces complications. Education should cover multiple aspects of the recovery process, including pain management, deep breathing exercises, cough techniques, activity limitations, wound care, and signs and symptoms of potential complications.
For instance, patients should be educated on the importance of regular deep breathing and coughing exercises to help prevent atelectasis (lung collapse). They should also understand how to manage their pain using prescribed medications and other methods, such as positioning and relaxation techniques. We often provide written materials and demonstrate the correct techniques. We also educate them on recognizing signs of infection, such as fever, increased pain, or purulent drainage from the incision site or chest tube.
Empowering patients with knowledge allows them to be actively involved in their recovery, leading to better adherence to treatment plans and improved outcomes.
Q 26. How do you address patient anxiety related to the thoracostomy procedure?
Addressing patient anxiety related to thoracostomy is crucial. Many patients experience significant distress about the procedure and its potential complications. We address this through a multi-pronged approach.
Before the procedure, we provide a thorough explanation of the procedure, its purpose, and the potential risks and benefits. We use clear and simple language and encourage the patient to ask questions. We also address their concerns and fears directly and honestly. After the procedure, we provide reassurance, explaining what to expect during recovery and addressing any pain or discomfort. We maintain a calm and supportive demeanor and encourage the patient to express their concerns. We also offer resources such as social work or psychological support if needed.
For example, using anatomical models and diagrams to visually explain the procedure can greatly reduce anxiety. Pain management strategies are vital in mitigating both physical and emotional distress.
Q 27. What are the ethical considerations related to thoracostomy decision-making?
Ethical considerations in thoracostomy decision-making are multifaceted. The primary ethical considerations revolve around patient autonomy, beneficence, and non-maleficence. Informed consent is paramount, ensuring the patient fully understands the procedure, its risks and benefits, and available alternatives.
For example, in cases where a patient lacks decision-making capacity, we must consider the best interests of the patient, often involving discussions with family members or legal guardians. We always strive to balance the potential benefits of the procedure against the potential risks, considering factors such as patient age, overall health, and prognosis. Resource allocation is another important consideration, especially in situations where thoracostomy might be part of a broader treatment plan with limited resources.
Maintaining open communication and a collaborative approach involving the patient, family, and healthcare team is critical to navigating ethical dilemmas.
Q 28. Describe a challenging thoracostomy case you have managed and how you resolved it.
One challenging case involved a patient with a massive hemothorax resulting from a traumatic injury. The initial chest tube placement failed to adequately drain the blood, leading to persistent hypotension and respiratory distress. Conventional techniques were ineffective due to clot formation within the pleural space and around the initial tube.
To resolve this, we performed a surgical exploration under general anesthesia. This allowed for thorough evacuation of the clots, direct visualization of the bleeding source (a lacerated intercostal artery), and placement of additional chest tubes in optimal locations. The surgical approach provided much better access than the initial blind placement. Post-operatively, the patient received blood transfusions and intensive respiratory support. Following the surgical intervention, drainage improved significantly, leading to stabilization of the patient’s hemodynamic and respiratory status.
This case highlighted the importance of adapting our approach when initial attempts fail and the need for timely surgical intervention in certain cases of massive hemothorax to prevent life-threatening complications.
Key Topics to Learn for Thoracostomy Interview
- Anatomy and Physiology of the Thoracic Cavity: Thorough understanding of pleural spaces, lungs, and surrounding structures is crucial. Prepare to discuss their interrelationships and implications for thoracostomy procedures.
- Indications and Contraindications for Thoracostomy: Master the criteria for choosing thoracostomy as a treatment option, and equally important, when it’s not appropriate. Consider various clinical scenarios and their impact on decision-making.
- Types of Thoracostomy Tubes and Insertion Techniques: Familiarize yourself with different tube sizes, materials, and placement methods. Be ready to discuss the rationale behind choosing a specific technique based on patient anatomy and clinical presentation.
- Post-Procedure Care and Complications: This includes monitoring for air leaks, bleeding, infection, and other potential complications. Understanding preventative measures and management strategies is essential.
- Troubleshooting Common Problems: Be prepared to discuss problem-solving approaches for issues such as tube displacement, clotting, or persistent air leaks. Practice explaining your decision-making process clearly and logically.
- Radiographic Interpretation: Thoracic imaging (chest X-rays, CT scans) is vital for assessing tube placement and identifying complications. Review image interpretation skills and be prepared to discuss findings.
- Patient Assessment and Monitoring: Explain how you would monitor a patient undergoing thoracostomy, including vital signs, respiratory status, and pain management.
Next Steps
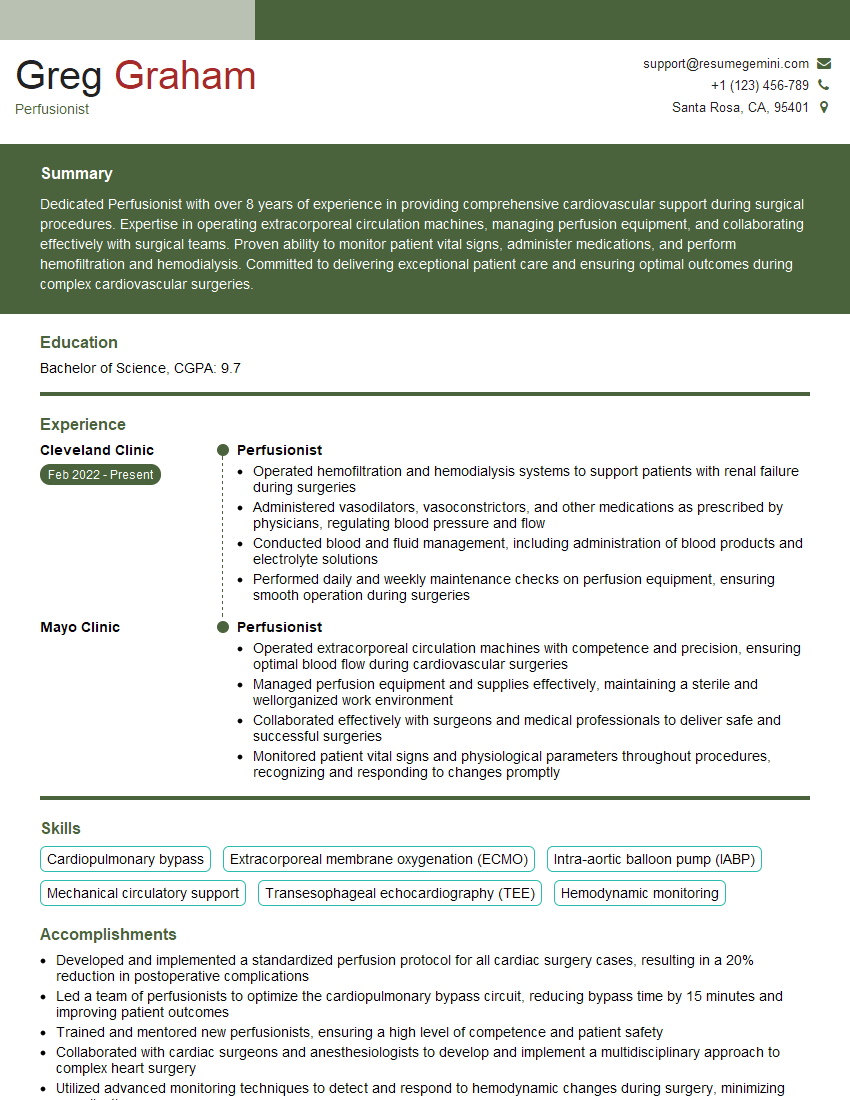
Mastering Thoracostomy demonstrates a high level of surgical skill and critical thinking, significantly enhancing your career prospects in respiratory care, surgical nursing, or related fields. A strong resume is key to showcasing your expertise. To maximize your chances of landing your dream job, create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource to help you build a professional and effective resume. They provide examples of resumes tailored to Thoracostomy, enabling you to present yourself in the best possible light to potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.