The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Total Ankle Replacement Surgery interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Total Ankle Replacement Surgery Interview
Q 1. Describe the surgical technique for a total ankle replacement.
Total ankle replacement (TAR) surgery involves replacing the damaged articular surfaces of the ankle joint with prosthetic components. The procedure typically begins with an incision on the front of the ankle, allowing access to the joint. The damaged cartilage and bone from the tibia (shinbone), talus (ankle bone), and sometimes the fibula (outer leg bone) are carefully removed using specialized instruments. Precise measurements are taken to ensure a perfect fit for the implants. Then, the metal components of the prosthesis are meticulously cemented or press-fit into place. The procedure concludes with meticulous closure of the incision, often using layered sutures and potentially drains to manage any excess fluid.
Think of it like rebuilding a worn-out hinge. We remove the damaged parts of the hinge and replace them with new, artificial components to restore smooth, pain-free movement.
Q 2. What are the indications and contraindications for total ankle replacement?
Indications for TAR include severe osteoarthritis, rheumatoid arthritis, post-traumatic arthritis, and failed ankle fusion where conservative treatments (like physical therapy, medication, and injections) have failed to provide adequate pain relief and functional improvement. The patient should also have realistic expectations about recovery and be willing to comply with the rehabilitation program.
Contraindications include significant infection in the ankle or leg, peripheral vascular disease significantly compromising blood supply to the ankle, severe bone loss or deformity, significant ligamentous instability, uncontrolled diabetes, active rheumatoid arthritis with significant inflammatory changes, and patient factors such as poor compliance and unrealistic expectations.
For example, a patient with a severe infection wouldn’t be a suitable candidate because the infection could compromise the implant and lead to failure. Similarly, a patient with poor circulation wouldn’t heal well, jeopardizing the success of the surgery.
Q 3. Explain the different types of total ankle replacement implants.
Several types of TAR implants exist, differing in their design and materials. They generally consist of a tibial component (placed on the tibia), a talar component (placed on the talus), and sometimes a fibula component (for cases with significant fibular involvement). Some implants are cemented into place, while others are press-fit (designed to integrate with the bone over time). Materials commonly used include cobalt-chromium alloys, titanium alloys, and high-density polyethylene for the bearing surfaces. Different designs also exist, including constrained (more restrictive movement) and unconstrained (allowing more natural motion) implants, each suited to particular patient needs and the specifics of their bone anatomy.
The choice of implant depends on factors like the extent of bone damage, the patient’s activity level, and the surgeon’s preference. It’s a highly individualized decision.
Q 4. How do you assess a patient’s suitability for total ankle replacement?
Assessing a patient’s suitability involves a thorough evaluation of their medical history, physical examination, and imaging studies (X-rays, CT scans, and potentially MRI). We meticulously assess the extent of joint damage, the overall health of the bone, the integrity of surrounding ligaments, and the patient’s overall health status. We also perform a comprehensive functional assessment to gauge the patient’s activity level and their ability to undergo rehabilitation. Furthermore, realistic expectations and patient compliance with post-operative instructions are crucial. Pre-operative counseling is paramount to ensure the patient fully understands the risks, benefits, and limitations of the procedure.
For instance, we’d examine the patient’s range of motion, assess their pain levels, and review their medical records to rule out any contraindications. A thorough discussion of expected outcomes and the rigorous rehabilitation process is also integral to this phase.
Q 5. What are the common complications associated with total ankle replacement?
Common complications include infection (a serious concern requiring potential revision surgery), implant loosening or failure, stiffness, persistent pain, nerve or vascular injury, deep vein thrombosis (DVT), and wound healing complications. The risk of these complications varies depending on various factors, including patient-specific health issues, surgical technique, implant design, and post-operative care.
For example, infection might require antibiotic treatment or even removal and replacement of the implant. Implant loosening can lead to pain and reduced function, potentially requiring revision surgery.
Q 6. How do you manage post-operative pain and swelling after total ankle replacement?
Post-operative pain and swelling management involves a multi-modal approach. This includes medication, such as pain relievers (including opioids in the initial phase, gradually transitioning to non-opioids), and anti-inflammatory drugs. Regular ice application helps reduce swelling and pain. Elevation of the leg is also recommended. Physical therapy plays a crucial role, focusing on range-of-motion exercises and strengthening exercises. Pain management strategies also encompass nerve blocks, if needed, to further control pain in the initial postoperative phase.
We emphasize a proactive approach, aiming to keep the patient comfortable and facilitating early mobilization and participation in the rehabilitation program.
Q 7. Describe your approach to pre-operative planning for a total ankle replacement.
Pre-operative planning is crucial for a successful TAR. It involves a thorough assessment of the patient’s condition, including detailed imaging studies and functional assessments. We use specialized software to plan the surgical approach, ensuring accurate implant sizing and placement. This often involves the use of 3D-printed models which allow the surgeon to practice the procedure, refine the surgical approach, and assess the fit of the implants before the surgery. This meticulous planning minimizes intraoperative complications and improves the accuracy of implant positioning, leading to better long-term outcomes.
This meticulous approach ensures that we have a clear understanding of the patient’s anatomy and needs before the procedure even begins, maximizing the chance of a positive result.
Q 8. What imaging modalities do you utilize in evaluating a patient for total ankle replacement?
Pre-operative imaging is crucial for successful total ankle replacement (TAR). We use a combination of modalities to thoroughly assess the ankle joint and surrounding structures. This allows us to accurately plan the surgery and identify any potential complications.
- Weight-bearing anteroposterior (AP) and lateral radiographs: These are essential for evaluating the degree of osteoarthritis, assessing bone stock, and identifying any deformities like valgus or varus malalignment. We look for joint space narrowing, osteophyte formation, and subchondral sclerosis.
- Mortise view radiograph: This view helps to assess the alignment of the talus within the mortise and to detect any subtle fractures or deformities.
- Computed Tomography (CT) scans: CT scans provide detailed three-dimensional images of the bone, allowing for precise assessment of bone quality and the extent of articular cartilage loss. This is particularly helpful in planning the surgical approach and implant sizing.
- Magnetic Resonance Imaging (MRI): While less frequently used for routine pre-operative assessment, MRI is invaluable in evaluating the condition of the soft tissues, including ligaments, tendons, and cartilage. It helps identify any underlying inflammatory conditions or significant soft tissue damage that might contraindicate TAR.
By combining these imaging techniques, we build a comprehensive picture of the patient’s ankle anatomy and pathology, leading to better surgical planning and improved outcomes.
Q 9. Discuss the role of physiotherapy in the rehabilitation of a patient after total ankle replacement.
Physiotherapy plays a vital role in the recovery process after TAR. A structured rehabilitation program is crucial for restoring range of motion, strength, and ultimately, function. It’s not just about physical recovery, but also about managing pain and improving the patient’s quality of life.
- Early mobilization: We encourage early weight-bearing as tolerated, starting with assisted ambulation and gradually progressing to independent walking. This helps to prevent stiffness and promotes healing.
- Range of motion exercises: These exercises are designed to restore full ankle dorsiflexion, plantarflexion, and inversion/eversion. We use techniques like passive range of motion initially, then progress to active and active-assisted exercises as the patient tolerates.
- Strengthening exercises: We focus on strengthening the muscles surrounding the ankle joint, including the calf muscles, tibialis anterior, and peroneal muscles. This improves stability and reduces the risk of re-injury.
- Proprioceptive exercises: These exercises aim to improve balance and coordination, which is crucial for safe and confident ambulation. Examples include balance board exercises and weight-shifting activities.
- Functional exercises: As the patient progresses, we introduce functional exercises that simulate daily activities, such as stair climbing, walking on uneven surfaces, and performing activities of daily living.
The intensity and duration of physiotherapy vary depending on the patient’s individual needs and progress. Regular follow-up appointments with the physiotherapist are crucial for monitoring progress and adjusting the rehabilitation plan as needed. Patient compliance and active participation are key to successful rehabilitation.
Q 10. How do you address infection following total ankle replacement?
Infection following TAR is a serious complication, requiring prompt and aggressive management. The approach depends on the severity and timing of the infection.
- Early infection (within 3 months): This is typically treated with intravenous antibiotics, guided by culture and sensitivity results. Surgical debridement (removal of infected tissue) may be necessary, often followed by implant retention if the infection is localized and successfully treated with antibiotics.
- Late infection (after 3 months): Late-onset infections are often more challenging to manage and usually require two-stage revision surgery. In the first stage, the infected implant is removed, and the joint is thoroughly debrided and irrigated. The wound is then left open to heal by secondary intention. Once the infection is resolved (typically confirmed by negative cultures), a second stage revision surgery is performed to replace the implant.
In cases of chronic or recurrent infections, it may be necessary to consider an arthrodesis (fusion) of the ankle joint. The specific treatment approach is always individualized based on the patient’s overall health, the type and severity of the infection, and the results of laboratory tests.
Q 11. How do you manage a patient with an implant loosening after a total ankle replacement?
Implant loosening after TAR can be a significant challenge. The management strategy depends on the extent of loosening and the patient’s symptoms.
- Asymptomatic loosening: If the loosening is detected on imaging but the patient is asymptomatic (not experiencing pain or functional limitations), we may adopt a conservative approach with close monitoring and regular imaging follow-ups.
- Symptomatic loosening: If the patient is experiencing pain, instability, or limited function, surgical intervention is typically required. This could involve a revision TAR, where the loose implant is removed and replaced with a new implant, or arthrodesis if the bone stock is compromised or the infection is present.
The decision of whether to proceed with revision surgery is made on a case-by-case basis considering patient age, activity level, overall health, and the extent of implant loosening and bone loss. Sometimes, alternative non surgical management like activity modification is chosen.
Q 12. Describe your experience with revision total ankle replacement surgery.
Revision TAR is a complex procedure requiring specialized expertise. My experience encompasses a wide range of revision cases, including those involving infection, aseptic loosening, implant failure, and malunion. The complexity increases significantly compared to primary TAR, as there is often significant bone loss or deformity that needs to be addressed. This frequently requires augmentation techniques such as bone grafting or the use of custom implants.
I frequently utilize advanced imaging techniques such as CT scans and 3D-printed models to meticulously plan revision surgeries. The surgical technique is adapted to the individual situation, focusing on thorough debridement, proper soft tissue balancing, and the selection of the appropriate implant to restore joint stability and function. Post-operative rehabilitation is similarly tailored to the individual case.
Successful revision TAR relies on careful pre-operative planning, meticulous surgical technique, and a robust rehabilitation program. The outcomes can be excellent, but the procedure is more demanding and has a higher risk of complications than primary TAR.
Q 13. What are the long-term outcomes of total ankle replacement?
Long-term outcomes of TAR are generally favorable for appropriately selected patients. While the longevity of the implant is not indefinite, many patients can experience significant pain relief and improved function for many years.
- Pain relief: A major benefit of TAR is significant pain reduction, leading to improved quality of life.
- Improved function: Most patients experience improvement in their ability to walk, climb stairs, and participate in recreational activities.
- Implant survival: The long-term survival rate of TAR implants varies depending on factors such as patient age, activity level, and surgical technique. Studies report varying survival rates over 10-15 years, with many patients experiencing satisfactory outcomes for 15 years or longer.
- Potential complications: Even with favorable outcomes, there’s a risk of long-term complications, such as implant loosening, infection, and osteolysis (bone loss).
Regular follow-up appointments are crucial to monitor for potential complications and ensure the long-term success of the procedure. Careful patient selection and a meticulous surgical technique significantly contribute to favorable long-term outcomes.
Q 14. What are the advantages and disadvantages of different surgical approaches to total ankle replacement?
Several surgical approaches exist for TAR, each with advantages and disadvantages. The choice of approach depends on factors such as the surgeon’s experience, the specific anatomical characteristics of the patient’s ankle, and the presence of any associated deformities.
- Anterior approach: This approach offers excellent exposure of the ankle joint, minimizing damage to the surrounding soft tissues. It is considered minimally invasive compared to posterior approaches and leads to less post-operative pain. However, limited exposure can sometimes necessitate compromise in implant selection.
- Posterior approach: This approach provides excellent exposure to the posterior aspect of the ankle joint. It is advantageous in cases of significant posterior impingement or posterior malleolar fractures. However, it can potentially result in Achilles tendon injury.
- Medial approach: This approach is less commonly used and is typically reserved for specific situations, such as treating medial impingement. Potential complications can include damage to the medial structures of the ankle.
The optimal surgical approach is a topic of ongoing discussion amongst surgeons. The choice ultimately aims to provide the most favorable balance between adequate exposure, preservation of soft tissue structures, and minimal risk of complications, leading to optimal functional results.
Q 15. How do you counsel patients about the risks and benefits of total ankle replacement?
Counseling patients about total ankle replacement (TAR) involves a thorough discussion of the procedure’s potential benefits and risks. We start by explaining that TAR aims to alleviate severe ankle pain and improve function in patients with end-stage osteoarthritis or other debilitating ankle conditions unresponsive to conservative treatments. The benefits include pain reduction, improved range of motion, and increased ability to participate in daily activities and hobbies.
However, it’s crucial to outline the potential risks, which include:
- Infection: A serious complication requiring further surgery and antibiotics.
- Implant loosening: The implant may become loose over time, requiring revision surgery.
- Nerve damage: Potential for injury to surrounding nerves leading to numbness or tingling.
- Deep vein thrombosis (DVT): Blood clot formation in the leg, potentially leading to pulmonary embolism.
- Fractures: Periprosthetic fractures can occur, particularly in the bones around the implant.
- Limited range of motion: While aiming for improvement, the final range of motion might be limited compared to a healthy ankle.
I use plain language, visual aids like anatomical models and X-rays, and patient-specific examples to ensure they fully grasp the trade-offs. I also emphasize the importance of realistic expectations and the need for diligent post-operative rehabilitation to maximize the chances of a successful outcome. For instance, I’ll share the success stories of previous patients while also honestly addressing potential challenges. This balanced approach facilitates informed decision-making.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with minimally invasive total ankle replacement techniques.
My experience with minimally invasive TAR techniques is extensive. I’ve found that these approaches offer several advantages over traditional open surgery, including smaller incisions, reduced soft tissue trauma, less post-operative pain, faster rehabilitation, and improved cosmetic outcomes. These smaller incisions minimize damage to muscles, tendons, and ligaments, leading to quicker recovery. For example, in a minimally invasive approach, we use specialized instruments and techniques to implant the prosthesis through smaller incisions, often preserving the important stabilizing ligaments. I employ both anterior and lateral approaches depending on the patient’s anatomy and the specific condition. Careful surgical planning, including pre-operative imaging and intra-operative navigation, is crucial to ensuring accuracy and success in these procedures.
I’ve noticed that patients undergoing minimally invasive TAR consistently report less post-operative pain and swelling and experience a significantly shorter hospital stay compared to those undergoing open procedures. Careful patient selection is crucial, however, as certain anatomical variations or severe bone deformities might require a more open approach.
Q 17. How do you select the appropriate implant size and design for a total ankle replacement?
Selecting the appropriate implant size and design is critical for the long-term success of a TAR. This involves a meticulous process encompassing pre-operative planning, intra-operative assessment, and consideration of patient-specific factors. Pre-operatively, detailed imaging studies (X-rays, CT scans) are analyzed to assess the bone’s morphology, articular cartilage damage, and the presence of any deformities. This helps determine the ideal implant size and type.
During surgery, we use a combination of digital templating and trial implants to ensure a precise fit. The surgeon carefully assesses the bone’s anatomy and stability before making the final implant selection. We carefully consider factors such as the patient’s age, activity level, bone quality, and overall health to ensure the best implant choice. The implant design should offer stability, while considering the patient’s biomechanics and alignment requirements to mimic the natural ankle joint’s functionality. For instance, some patients may benefit from implants with enhanced rotational stability, while others might benefit from designs that offer increased articular surface area.
Q 18. What are the latest advancements in total ankle replacement technology?
Recent advancements in TAR technology focus on improved implant designs, surgical techniques, and rehabilitation protocols. Newer implants often incorporate materials with enhanced wear resistance and biocompatibility. Some designs incorporate porous coatings to encourage bone ingrowth, potentially leading to increased implant longevity and stability. The development of patient-specific implants, created using 3D printing based on individual patient anatomy, allows for customized fit and improved precision.
Minimally invasive surgical techniques, as discussed previously, continue to evolve. The use of computer-assisted navigation systems and robotics enhances surgical accuracy and potentially reduces complications. There is also ongoing research into novel materials, such as those with enhanced osseointegration properties. Improvements in post-operative rehabilitation programs, including the use of advanced therapies like platelet-rich plasma (PRP), aim to optimize patient outcomes and functional recovery. These advances, while continuously evolving, are contributing towards better patient outcomes and improved long-term implant survivorship.
Q 19. How do you manage periprosthetic fractures after total ankle replacement?
Periprosthetic fractures following TAR are a significant concern, usually requiring prompt intervention. Management depends on the fracture’s location, severity, and the patient’s overall health. The initial approach involves thorough clinical examination, imaging (X-rays, CT scans), and assessment of patient stability. Treatment options range from conservative management (e.g., immobilization and pain control) for minor fractures to surgical intervention for more significant injuries.
Surgical management typically involves open reduction and internal fixation (ORIF), using plates, screws, or other fixation devices to stabilize the fracture. In some cases, revision TAR may be necessary if the fracture compromises the implant’s stability. The decision depends on several factors, including fracture pattern, bone quality, implant condition, and the patient’s overall health and functional goals. Post-operative rehabilitation is critical for restoring function and preventing further complications. The specific rehabilitation protocol is tailored to the fracture’s severity and the patient’s needs.
Q 20. How do you handle patients with allergies or sensitivities to implant materials?
Patients with allergies or sensitivities to implant materials require careful consideration during the pre-operative planning phase. A detailed allergy history is essential, specifically addressing sensitivities to metals like cobalt, chromium, nickel, and titanium – common components in TAR implants. Alternatives might include implants made of different materials, such as ceramic components. However, it’s essential to discuss the trade-offs, as different materials may have varying longevity and wear characteristics.
Pre-operative allergy testing can be helpful in certain cases, but it’s crucial to remember that even negative test results don’t guarantee a complete absence of a reaction. If a patient has a history of severe metal allergies, the team will carefully weigh the benefits and risks of TAR against other treatment options. Close monitoring post-operatively is essential, and patients are educated about signs of an allergic reaction. This careful planning and monitoring mitigate the risks associated with implant allergies and help ensure patient safety.
Q 21. How do you assess and manage nerve damage following total ankle replacement?
Nerve damage following TAR is a potential complication that requires careful assessment and management. The most commonly affected nerves are the superficial peroneal and sural nerves. Post-operatively, patients are closely monitored for any signs of nerve injury, including numbness, tingling, paresthesia, or weakness in the foot or ankle. A detailed neurological examination, including sensory and motor testing, helps identify the extent of any nerve involvement. Electrodiagnostic studies, such as nerve conduction studies and electromyography, may be employed to confirm the diagnosis.
Treatment approaches vary depending on the severity and type of nerve injury. In some cases, conservative management involving pain management, physiotherapy, and time may suffice. However, for significant nerve injuries, surgical exploration and repair or decompression may be necessary. Regular follow-up visits are crucial to monitor nerve recovery and address any persistent symptoms. Physical therapy plays a crucial role in regaining function after nerve injury, with targeted exercises aimed at improving muscle strength and sensory recovery.
Q 22. Discuss your approach to managing patients with comorbidities such as diabetes or osteoporosis undergoing total ankle replacement.
Managing comorbidities like diabetes and osteoporosis in total ankle replacement (TAR) patients requires a multidisciplinary approach focused on optimizing patient health before, during, and after surgery. Diabetes increases the risk of infection and delayed healing, while osteoporosis elevates the risk of fracture.
- Pre-operative optimization: For diabetic patients, we meticulously control blood glucose levels aiming for HbA1c below 7% to minimize infection risk. We also collaborate with endocrinology to manage any existing diabetic complications. For osteoporosis patients, we assess bone density using DEXA scans and may initiate or adjust osteoporosis medications to improve bone strength. We might consider using bone grafting techniques during the procedure to enhance implant stability.
- Intra-operative considerations: Meticulous surgical technique is paramount to minimize trauma and reduce the risk of infection. We use minimally invasive techniques whenever feasible. We carefully select implants considering bone quality, ensuring a secure fixation. For patients with severe osteoporosis, we might choose a different implant design or augmentation techniques.
- Post-operative management: Post-operatively, strict glycemic control continues for diabetic patients. We closely monitor for signs of infection, including elevated inflammatory markers and local signs at the surgical site. Physiotherapy is crucial for both patient groups, tailored to their specific needs and limitations, emphasizing careful weight-bearing to avoid implant loosening or fractures.
For example, a recent patient with severe osteoporosis required us to use a longer stem implant and augment the bone with a graft to ensure stability. This resulted in a successful outcome with minimal complications.
Q 23. Describe your experience with different types of anesthesia for total ankle replacement.
Anesthesia selection for TAR depends on individual patient factors like age, overall health, and the presence of comorbidities. We typically offer a choice between spinal, epidural, or general anesthesia.
- Spinal anesthesia: Provides excellent analgesia and muscle relaxation for the lower extremities, often allowing for a faster recovery and reduced post-operative nausea and vomiting. It is ideal for patients with fewer comorbidities.
- Epidural anesthesia: Offers similar benefits to spinal anesthesia but allows for prolonged pain management via continuous infusion of local anesthetic and opioids. It’s a good option for patients needing longer-lasting pain control.
- General anesthesia: This is used if spinal or epidural are contraindicated, for example, in patients with spinal deformities or coagulation disorders. Recovery can be slower and associated with more post-operative side effects.
The decision regarding the best anesthesia type involves a detailed preoperative discussion with the patient and anesthesiologist, weighing potential risks and benefits for each individual case.
Q 24. What are your protocols for post-operative infection prophylaxis?
Preventing post-operative infection is a top priority in TAR. Our protocol incorporates several layers of defense:
- Preoperative antibiotics: A single dose of prophylactic antibiotics (typically a cephalosporin) is administered intravenously 30-60 minutes before the incision.
- Meticulous surgical technique: Maintaining a sterile field during surgery minimizes the risk of bacterial contamination. We use a tourniquet to control bleeding and facilitate a clean surgical site.
- Wound care: A sterile dressing is applied postoperatively. We might also use prophylactic antibiotic-impregnated cement during the surgery.
- Postoperative surveillance: Patients are closely monitored for signs of infection, including fever, wound drainage, and elevated white blood cell count. Any suspicion of infection prompts immediate investigation and treatment with appropriate antibiotics based on culture results.
Our protocol reduces the rate of post-operative infections to a minimum. For high-risk patients (e.g., those with diabetes), we might consider extending the duration of antibiotic prophylaxis or implementing additional measures like antimicrobial-impregnated bone cement.
Q 25. How do you differentiate between a failed total ankle replacement and other causes of ankle pain?
Differentiating between a failed TAR and other causes of ankle pain requires a thorough clinical evaluation and imaging studies.
- Clinical evaluation: We assess the patient’s pain location, character, and duration, examining the range of motion and stability of the ankle joint. We look for signs of infection or instability, and assess the patient’s activity levels.
- Imaging: Plain radiographs are initially obtained to evaluate implant position, bone alignment, signs of loosening, or osteolysis (bone loss around the implant). If plain radiographs are inconclusive, we would use CT scans for better bone detail, or MRI scans to evaluate soft tissues and cartilage for inflammatory changes or other pathologies such as ligament tears.
- Other causes of ankle pain: These include arthritis in adjacent joints, tendinitis, nerve entrapment, stress fractures, or even referred pain. A detailed history and physical examination are essential to rule out alternative diagnoses.
For example, a patient presenting with persistent ankle pain after TAR might show radiographic evidence of implant loosening or osteolysis, indicating a failed implant. In contrast, another patient with similar symptoms might have an MRI revealing a peroneal tendon tear, a completely separate issue.
Q 26. How do you use advanced imaging (e.g., CT, MRI) to guide your decision-making in total ankle replacement?
Advanced imaging plays a crucial role in decision-making for TAR, both pre- and post-operatively.
- Preoperative imaging (CT, MRI): CT scans provide detailed bony anatomy, allowing us to assess bone stock, identify any pre-existing deformities, and plan the surgical approach. MRI scans are helpful in assessing the condition of cartilage and soft tissues, guiding us in selecting appropriate implants and anticipating potential surgical challenges. They can also identify hidden fractures or other anatomical problems.
- Postoperative imaging (CT, radiographs): Post-operatively, radiographs and CT scans are used to evaluate implant position, bone integration, signs of loosening or osteolysis, and to identify any complications like fractures or infections. We use CT scans for detailed pre-operative planning in complex cases, for example, in patients with severe bone deformities, or severe arthritis with significant bone loss.
The use of advanced imaging helps us to personalize the surgical approach, select the most appropriate implant, and optimize outcomes. For instance, preoperative CT scans help us plan the optimal bone cuts and implant positioning, minimizing the risk of complications.
Q 27. Describe your experience with robotic-assisted total ankle replacement.
My experience with robotic-assisted TAR has been positive, offering several potential advantages.
- Improved accuracy and precision: The robot allows for more precise bone cuts and implant positioning, potentially leading to better implant fit and alignment, resulting in improved function and reduced complications.
- Minimally invasive approach: Robotic-assisted TAR can often be performed using smaller incisions, reducing tissue trauma, blood loss, and post-operative pain. This leads to faster recovery times.
- Enhanced visualization: The robotic system provides excellent visualization of the surgical field, making the procedure easier and more efficient.
However, it’s crucial to note that robotic-assisted TAR is not a replacement for a surgeon’s skill and judgment. The robot is a tool that enhances the surgeon’s capabilities, not a replacement for expertise and experience. The learning curve for robotic TAR surgery is steep and requires significant investment in training and equipment. We are continuously evaluating the outcomes of robotic vs. conventional TAR to determine which approach is best for individual patients.
Q 28. What is your approach to managing patients’ expectations regarding recovery after total ankle replacement?
Managing patient expectations is critical for a successful TAR outcome.
- Realistic goals: We emphasize that TAR aims to alleviate pain, improve function, and restore mobility, but it is not a magic bullet. There are limitations, and a full return to pre-disease function may not always be achieved.
- Personalized recovery timelines: Recovery times vary depending on individual factors like age, overall health, and the extent of pre-existing damage. We provide individualized estimations and encourage patients to be patient and persistent with their rehabilitation.
- Open communication: We maintain open and honest communication throughout the process, addressing any questions or concerns. We share realistic expectations about potential complications, and involve the patient and their family in decision-making.
- Realistic post-surgical lifestyle: We counsel patients about the long-term expectations, emphasizing the importance of continued physiotherapy, adherence to weight-bearing restrictions and activity modification as needed, and the possibility of needing revision surgery in the future.
By setting realistic expectations, fostering open communication, and empowering patients to take an active role in their recovery, we improve patient satisfaction and overall outcomes following TAR.
Key Topics to Learn for Total Ankle Replacement Surgery Interview
- Pre-operative Assessment: Understanding patient history, physical examination techniques, imaging interpretation (X-rays, CT scans), and determining candidacy for total ankle replacement.
- Surgical Technique: Mastering various surgical approaches (anterior, posterior, lateral), implant selection criteria, bone preparation techniques, and soft tissue management.
- Intraoperative Complications & Management: Recognizing and addressing potential complications such as infection, malposition, nerve injury, and vascular injury during the procedure.
- Post-operative Care & Rehabilitation: Developing a comprehensive post-operative plan, including pain management, weight-bearing protocols, physical therapy strategies, and monitoring for complications.
- Implant Selection & Design: Understanding the biomechanics of different implant designs, their strengths and limitations, and factors influencing implant choice for specific patient needs.
- Revision Ankle Replacement: Familiarization with indications for revision surgery, challenges associated with revision procedures, and different surgical techniques used in revision cases.
- Patient Selection & Expectations: Understanding the criteria for selecting suitable candidates, managing patient expectations, and addressing potential limitations of the procedure.
- Current Research & Trends: Staying updated on the latest advancements in surgical techniques, implant designs, and rehabilitation protocols in the field of total ankle replacement.
- Ethical Considerations: Understanding the ethical implications related to patient autonomy, informed consent, and resource allocation in total ankle replacement surgery.
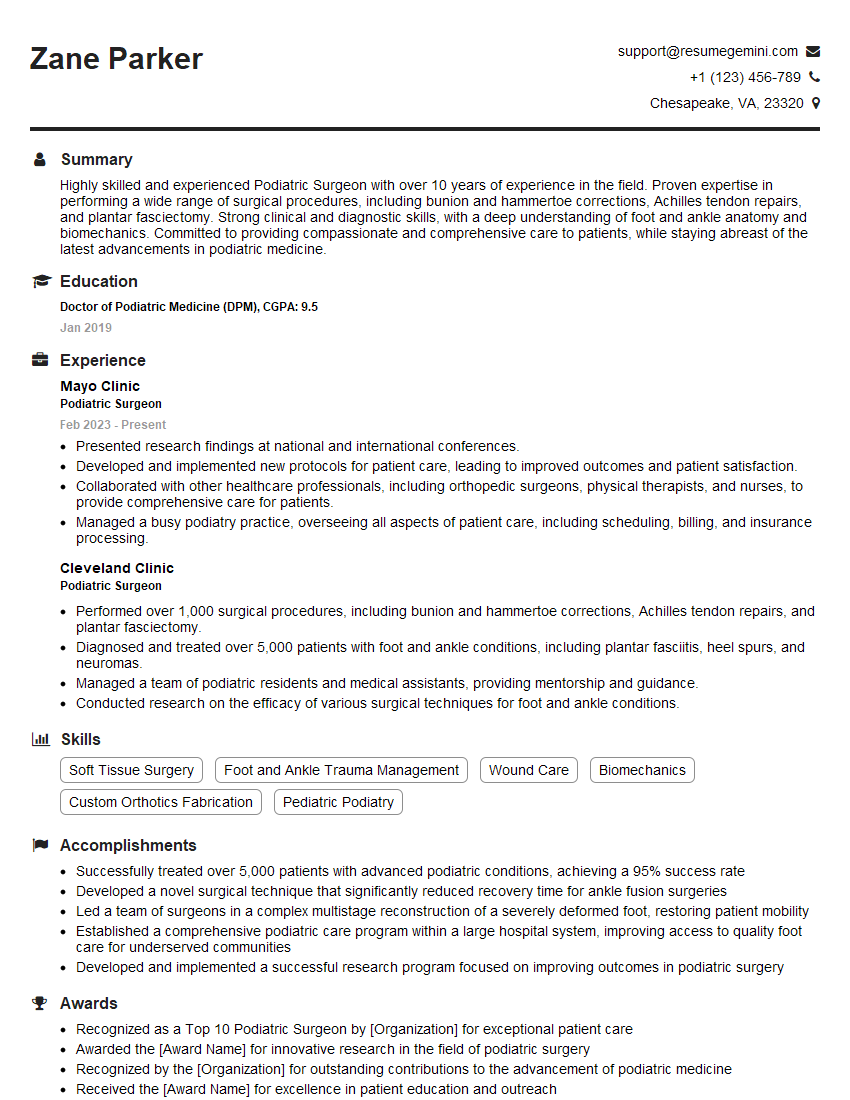
Next Steps
Mastering Total Ankle Replacement Surgery is crucial for career advancement in orthopedic surgery, opening doors to specialized fellowships, leadership roles, and research opportunities. To maximize your job prospects, it’s vital to create an ATS-friendly resume that effectively highlights your skills and experience. We strongly recommend using ResumeGemini to build a professional and impactful resume tailored to your expertise. ResumeGemini offers a user-friendly platform and provides examples of resumes specifically designed for candidates in Total Ankle Replacement Surgery, helping you stand out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.