Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Transanal Endoscopic Microsurgery (TEMS) interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Transanal Endoscopic Microsurgery (TEMS) Interview
Q 1. Describe the indications for TEMS.
Transanal Endoscopic Microsurgery (TEMS) is indicated for the minimally invasive treatment of various benign and malignant rectal lesions. Think of it as a sophisticated keyhole surgery for the rectum. The specific indications include:
- Benign lesions: Rectoceles (bulging of the rectal wall), rectal polyps (small growths), and anal fistulas (abnormal connections between the rectum and skin).
- Early-stage rectal cancers: TEMS can be used for the complete resection of small, early-stage rectal cancers, particularly those confined to the mucosa or submucosa. This is a critical advantage as it allows for less extensive surgery and a faster recovery compared to traditional approaches.
- Selected cases of rectal endometriosis: This debilitating condition affecting the rectum can be addressed using TEMS, depending on the extent and nature of the involvement.
The decision to use TEMS depends heavily on the size, location, and nature of the lesion, as well as the patient’s overall health and suitability for minimally invasive surgery. For instance, a large, deeply invasive rectal cancer would not be suitable for TEMS.
Q 2. What are the contraindications for TEMS?
Several contraindications exist for TEMS, making it unsuitable for all patients. These include:
- Extensive local disease: If the rectal lesion is large, deeply invasive, or has spread to nearby organs, TEMS is usually not feasible. A more extensive surgical approach is often necessary.
- Advanced cancer: Patients with advanced rectal cancer with lymph node involvement or distant metastasis are not candidates for TEMS.
- Severe comorbidities: Patients with significant underlying health conditions, such as severe heart or lung disease, might not tolerate the procedure.
- Previous pelvic radiation therapy: This can cause significant scarring and inflammation, making the procedure technically challenging and increasing the risk of complications.
- Significant inflammation or infection: Active rectal inflammation or infection can increase the risk of complications during and after surgery.
- Inability to tolerate bowel preparation: Adequate bowel preparation is crucial for TEMS. Patients unable to tolerate bowel preparation should not undergo the procedure.
Careful evaluation by a surgeon experienced in TEMS is critical to determine if a patient is a suitable candidate. The potential benefits must be carefully weighed against the risks and limitations of the technique.
Q 3. Explain the advantages of TEMS compared to traditional surgery.
TEMS offers several significant advantages over traditional open rectal surgery:
- Minimally invasive: It involves smaller incisions, leading to less trauma to the surrounding tissues.
- Shorter hospital stay: Patients typically have a shorter hospital stay compared to open surgery, accelerating their recovery.
- Less pain and discomfort: Reduced tissue trauma translates to less post-operative pain and discomfort.
- Faster recovery: Patients usually recover more quickly and return to their normal activities sooner.
- Better cosmetic results: The smaller incisions result in less visible scarring.
- Reduced risk of complications: Although complications can still occur, the overall risk is generally lower compared to open surgery, particularly complications like infections and bowel obstructions.
Imagine the difference between a major abdominal surgery and a small incision. That’s the essence of TEMS’ advantages. The recovery is much smoother and quicker, enabling patients to return to their daily lives more efficiently.
Q 4. Outline the steps involved in a typical TEMS procedure.
A typical TEMS procedure involves several key steps:
- Bowel preparation: Thorough bowel cleansing is essential to provide a clear surgical field.
- Anesthesia: General anesthesia is typically used.
- Transanal insertion of the endoscope: A specialized endoscope with a high-definition camera and integrated instruments is inserted through the anus.
- Dissection and resection: Under direct visualization, the surgeon carefully dissects and removes the lesion.
- Closure of the defect: The defect created by the resection is meticulously closed using surgical clips or sutures.
- Removal of the endoscope: The endoscope is carefully withdrawn.
- Postoperative care: This includes pain management, monitoring of bowel function, and assessment for any potential complications.
The entire procedure is guided by real-time high-definition visualization, allowing for precision and minimizing trauma to surrounding healthy tissues. Each step requires meticulous attention to detail and experience.
Q 5. Describe the instruments used in TEMS.
TEMS utilizes specialized instruments designed for minimally invasive rectal surgery. These instruments include:
- High-definition endoscope: Provides excellent visualization of the surgical field.
- Microsurgical instruments: Small, precise instruments such as scissors, forceps, and graspers designed for delicate work in a confined space.
- Energy devices: These can include monopolar or bipolar electrocautery for hemostasis (controlling bleeding) and tissue dissection. Argon plasma coagulation can be used for coagulation and hemostasis.
- Sutures and clips: For closure of the surgical defect.
- Irrigation system: Provides continuous irrigation of the surgical field to maintain visibility and remove debris.
The instruments are designed to be manipulated through the endoscope’s working channels, allowing for precise manipulation within the rectum. Think of them as tiny, specialized tools designed for delicate work within a small, complex area.
Q 6. How do you manage bleeding during a TEMS procedure?
Bleeding control is crucial during TEMS. Several strategies are employed:
- Electrocautery: Monopolar or bipolar electrocautery is routinely used to coagulate (seal) small bleeding vessels.
- Argon plasma coagulation (APC): APC is an excellent technique to coagulate bleeding vessels without causing thermal injury to surrounding tissue.
- Surgical clips: Hemoclips can be used to occlude (block) larger bleeding vessels.
- Direct pressure: Direct pressure with surgical instruments can temporarily control bleeding.
- Surgical sutures: In cases of significant bleeding, sutures may be required to ligate (tie off) bleeding vessels.
Careful dissection and meticulous attention to hemostasis throughout the procedure are paramount to minimize the risk of bleeding. Experienced surgeons are adept at using these techniques to effectively manage bleeding during TEMS.
Q 7. What are the potential complications of TEMS?
While TEMS is generally safe, potential complications can occur, including:
- Bleeding: Although actively managed, significant bleeding can occur.
- Infection: Postoperative infections are a possibility, though the risk is lower compared to open surgery.
- Perforation: Accidental perforation (hole) of the rectal wall is a rare but serious complication.
- Incontinence: Injury to the anal sphincter can potentially lead to fecal incontinence, though this is infrequent with experienced surgeons.
- Stenosis: Narrowing of the rectum can occur due to scarring.
- Recurrence: If the lesion is not completely removed, recurrence is possible.
Preoperative evaluation, meticulous surgical technique, and careful postoperative monitoring significantly reduce the risk of these complications. It’s crucial for patients to discuss potential risks with their surgeon before undergoing TEMS.
Q 8. How do you diagnose and manage postoperative complications of TEMS?
Postoperative complications after TEMS are thankfully rare but require vigilant monitoring and prompt management. Diagnosis relies heavily on a combination of clinical assessment, laboratory tests, and imaging. Common complications include bleeding, infection, perforation, and stenosis. Let’s look at how we manage them:
- Bleeding: This is usually managed conservatively with close monitoring of vital signs and potentially blood transfusions. In severe cases, endoscopic hemostasis or even laparotomy might be necessary.
- Infection: This is addressed with intravenous antibiotics targeted at the suspected pathogen, guided by culture and sensitivity testing. Close monitoring for signs of sepsis is crucial.
- Perforation: This is a serious complication. Management depends on the location and severity, ranging from conservative management with bowel rest and intravenous fluids to surgical repair.
- Stenosis: This can occur later, and we usually monitor patients with regular endoscopic examinations. Balloon dilation or even re-intervention might be required.
For example, I once had a patient develop a small rectal bleed post-TEMS. Through careful observation and conservative management with intravenous fluids, the bleeding resolved without further intervention. However, a different patient required emergency surgery for a perforation that was diagnosed via CT scan.
Q 9. What are the different types of sutures used in TEMS?
The choice of suture in TEMS is crucial for achieving secure anastomosis and minimizing complications. We utilize absorbable sutures primarily, chosen based on their strength, handling characteristics, and degradation profile. Here are some common examples:
- Polyglactin 910 (Vicryl): This is a widely used absorbable suture offering good knot security and tissue handling. It’s commonly used for mucosal closure.
- Polydioxanone (PDS): This suture offers a longer absorption time compared to Vicryl, suitable for deeper layers where longer-term support is desired.
- Polyglycolic acid (Dexon): Another absorbable suture option, known for its strength and predictable absorption rate. Selection is based on the specific needs of the surgical procedure.
The choice often depends on the location and the tension required at the suture site. For instance, in the mucosal layer where precise placement is crucial and rapid absorption is desired, Vicryl would likely be our preferred choice.
Q 10. How do you select the appropriate TEMS approach for a particular patient?
Selecting the appropriate TEMS approach depends on a thorough evaluation of the patient’s anatomy, pathology, and overall health. Factors considered include lesion location, size, and extent; patient’s body habitus; the presence of comorbidities; and surgeon’s experience.
A transanal approach is typically preferred for lesions that are accessible through the anus. However, if the lesion is too high, then a transabdominal approach might be necessary, potentially involving laparoscopic assistance. Preoperative imaging studies, such as colonoscopy and MRI, are vital in guiding this decision. For instance, a small rectal polyp would be a perfect candidate for a straightforward transanal TEMS, while a large, complex rectal tumor might require a more extensive approach, possibly hybrid or even open surgery.
Q 11. Describe your experience with different TEMS platforms.
My experience encompasses several TEMS platforms, each with its strengths and weaknesses. I’ve worked extensively with both rigid and flexible endoscopes, as well as different types of energy sources for dissection and coagulation.
Rigid endoscopes offer a more stable platform for precise dissection, but access can be limited. Flexible endoscopes provide better access to challenging anatomies, however, the image quality and maneuverability can be slightly compromised. Choosing the platform is a very nuanced decision, often depending on the patient and the specifics of the procedure.
Experience with various energy sources, such as monopolar and bipolar electrocautery, ultrasonic shears, and laser, has allowed me to adapt my technique to different tissue types and clinical situations. For example, ultrasonic shears offer superior hemostasis for larger vessels while bipolar cautery is excellent for delicate dissection.
Q 12. Explain your approach to patient selection for TEMS.
Patient selection for TEMS is crucial for ensuring optimal outcomes. I meticulously evaluate each patient considering factors like:
- Tumor location and size: TEMS is best suited for lesions that are accessible through the anus and are not excessively large or invasive.
- Tumor characteristics: The nature of the tumor (benign vs. malignant), its histology, and its local invasion all play important roles.
- Patient’s general health: Patients should have sufficient cardiac, pulmonary, and renal reserve to tolerate the procedure.
- Anatomic considerations: Factors like anal stenosis, rectal tortuosity, and previous rectal surgeries are considered.
For example, a patient with a large, locally advanced rectal cancer would not be an ideal candidate for TEMS. Conversely, a patient with a small, benign rectal polyp would be an excellent candidate.
Q 13. How do you counsel patients about the risks and benefits of TEMS?
Counseling patients about TEMS involves a detailed discussion of both the potential benefits and risks. I explain the procedure in layman’s terms, emphasizing the minimally invasive nature and potential for faster recovery times compared to open surgery.
I also discuss potential complications, such as bleeding, infection, perforation, and stenosis. I emphasize that while these are rare, they are possibilities. I always answer questions openly and honestly, ensuring the patient understands the implications of the decision. I provide them with written materials and encourage them to bring a support person to the consultation to ensure a thorough understanding.
I believe in informed consent and empowering patients to make the best decision for themselves, based on a complete understanding of their options.
Q 14. What is your experience with intraoperative imaging during TEMS?
Intraoperative imaging during TEMS significantly enhances precision and safety. We routinely use high-definition endoscopes that provide excellent visualization of the surgical field. In cases where additional detail is needed, we may utilize intraoperative ultrasound or even fluoroscopy, although this is less common than the high-resolution endoscopy.
For example, intraoperative ultrasound can help to delineate the tumor margins more accurately, ensuring complete resection. Fluoroscopy may be used in complex cases to guide the placement of clips or sutures. The choice of imaging modality depends on the specific clinical scenario and the information needed to guide the surgical approach.
Q 15. Describe your experience with TEMS in managing specific pathologies (e.g., rectal cancer, polyps).
My experience with Transanal Endoscopic Microsurgery (TEMS) spans a wide range of rectal pathologies. I’ve extensively used TEMS for the resection of benign and malignant lesions, including rectal cancers and polyps. For rectal cancer, TEMS offers a minimally invasive approach, particularly advantageous for early-stage tumors located in the lower rectum. This allows for complete tumor resection while minimizing the trauma associated with open surgery or traditional laparoscopic approaches. The precise visualization provided by TEMS, coupled with its ability to manipulate instruments within the narrow confines of the rectum, enables me to achieve excellent oncological outcomes, such as R0 resection (complete removal of the tumor with clear margins).
In cases of polyps, TEMS allows for the complete removal of even large polyps, reducing the risk of recurrence and the need for more extensive procedures. I regularly employ TEMS for polypectomy in patients with adenomas (precancerous polyps), achieving excellent hemostasis (control of bleeding) and minimizing the risk of perforation. The ability to perform en-bloc resection (removing the polyp in one piece) is crucial for accurate histopathological analysis (examination of tissue under a microscope), aiding in determining the true nature of the lesion and informing further treatment.
The choice between TEMS and other approaches, such as laparoscopic surgery or open surgery, is tailored to the individual patient and tumor characteristics. Factors considered include tumor size and location, patient comorbidities (other health conditions), and surgeon expertise.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage difficult anatomy during a TEMS procedure?
Managing difficult anatomy during TEMS requires a combination of technical skill, meticulous planning, and adaptability. Challenges often arise from anatomical variations such as a narrow anal canal, tortuous rectum (a rectum with many curves), or presence of scar tissue. Pre-operative imaging, such as MRI or CT scans, is essential for assessing the anatomy and identifying potential difficulties. This helps me develop a detailed surgical plan.
Intraoperatively, I utilize specialized instruments designed for TEMS, including flexible endoscopes with high-definition cameras and miniature surgical instruments. These tools allow for precise maneuvering even in challenging anatomical spaces. In cases of significant anatomical distortion, I might employ techniques like careful mobilization of surrounding tissues or the use of a transanal retractor system to improve visualization and access. Sometimes, conversion to a different surgical approach might be necessary if the anatomy is truly unapproachable with TEMS.
Furthermore, experience and proficiency are critical. The more TEMS procedures I perform, the better I become at identifying and managing difficult anatomy. This builds intuitive problem-solving skills that are crucial for success in this complex field.
Q 17. What is your approach to postoperative pain management in TEMS patients?
Postoperative pain management in TEMS patients is a priority. Because TEMS is minimally invasive, the postoperative pain is usually less severe than with open surgery. However, discomfort is expected. My approach is multi-modal, incorporating several strategies: Firstly, I utilize a combination of local anesthetics during the procedure to minimize initial pain. Then, I prescribe a balanced analgesic regimen, often including non-steroidal anti-inflammatory drugs (NSAIDs) for inflammation and pain relief, as well as opioids for breakthrough pain as needed. The opioid use is tightly managed to prevent adverse effects.
Regular monitoring of the patient’s pain levels is vital. This is accomplished through regular assessments using validated pain scales, facilitating prompt adjustments to the analgesic plan. I also emphasize patient education about pain management strategies, including breathing exercises and positioning techniques, to promote comfort. If pain is persistent or severe, further investigation for potential complications is undertaken.
Q 18. What are the key elements of postoperative follow-up in TEMS patients?
Postoperative follow-up in TEMS patients is crucial for ensuring optimal recovery and detecting any complications. The initial follow-up appointment typically occurs within a week post-procedure. This appointment involves assessing the patient’s pain level, wound healing, and bowel function. A digital rectal exam (DRE) is performed to check for any signs of inflammation or infection.
Further follow-up appointments are scheduled, depending on the nature of the procedure and the patient’s condition. These appointments might include repeat DREs, colonoscopies (to visually examine the colon), and imaging studies (if necessary) to monitor for recurrence or complications. It’s also an opportunity for ongoing patient education and address any concerns.
Pathology reports, showing the results of the tissue analysis, are reviewed carefully and the patient is informed about their implications for future care, such as the need for chemotherapy or radiation therapy.
Q 19. Describe your experience with minimally invasive surgical techniques.
My experience with minimally invasive surgical techniques is extensive, extending beyond TEMS. I’m proficient in laparoscopic and robotic surgery for various colorectal procedures. The principles of minimally invasive surgery – smaller incisions, less trauma, reduced pain, faster recovery times – are central to my surgical practice. I believe that patient-centered care necessitates the utilization of the least invasive technique appropriate for achieving optimal treatment outcomes.
My expertise in different minimally invasive approaches allows me to choose the most appropriate technique for each patient based on individual factors, such as tumor location, size, and overall health. This tailored approach minimizes potential complications and optimizes patient outcomes. The combination of experience across diverse minimally invasive techniques allows a holistic approach to the management of colorectal disease.
Q 20. How do you ensure patient safety during a TEMS procedure?
Patient safety is my paramount concern during TEMS procedures. Several strategies are implemented to ensure safety: Firstly, a thorough preoperative evaluation assesses the patient’s overall health, including identifying any contraindications to the procedure. Informed consent is obtained, ensuring the patient understands the risks and benefits of the procedure. A meticulous approach is followed during the procedure, avoiding excessive force and maintaining careful control of bleeding.
Careful attention is paid to maintaining sterility, reducing the risk of infection. The use of advanced imaging technology allows for precise localization and resection of lesions. Postoperatively, strict monitoring of vital signs, pain levels, and bowel function helps identify and manage any potential complications promptly. The use of a team approach, with nurses and other healthcare professionals collaboratively involved, further ensures patient safety. Regular audits of outcomes and adherence to best practices enhance patient safety standards.
Q 21. Explain your understanding of anatomical structures relevant to TEMS.
A deep understanding of the anatomical structures relevant to TEMS is fundamental to performing safe and effective procedures. This includes detailed knowledge of the rectum, anus, surrounding pelvic structures, and their vascular and nervous supply. The rectum’s anatomy is complex, characterized by its three layers (mucosa, submucosa, muscularis propria) and its relationship to adjacent organs such as the prostate (in men), uterus (in women), and bladder. Precise understanding of the surgical planes (tissue layers that are separated during surgery) is crucial for avoiding injury to these adjacent structures.
Knowledge of the vascular supply of the rectum is important to anticipate and control bleeding during the procedure. Similarly, understanding the innervation of the rectum is critical for minimizing functional impairment. I employ various techniques to minimize injury during surgery, including the use of harmonic scalpel and bipolar electrocautery for precise dissection and hemostasis (blood clot formation). Regular participation in anatomical dissection courses and continuous learning maintain my understanding of these vital anatomical structures.
Q 22. Describe your experience with surgical robots and their use in TEMS.
While TEMS is traditionally a minimally invasive procedure performed with standard laparoscopic instruments, the integration of robotic surgical systems is an exciting area of ongoing exploration. Currently, the use of robots in TEMS is limited, and there isn’t widespread clinical adoption. However, the potential benefits are significant. Imagine the advantages of enhanced dexterity, precision, and tremor filtration offered by robotic arms in this complex, confined surgical space. My experience is primarily with observing and researching the feasibility studies conducted using robotic platforms adapted for transanal access. These studies primarily focus on the challenges related to instrument miniaturization, workspace limitations within the rectum, and the development of appropriate haptic feedback systems for surgeons to maintain precise control. One specific challenge we’ve investigated is the adaptation of robotic grasping and suturing tools for delicate tissue handling within the rectum. The next few years will likely witness more breakthroughs in this field as technology advances and overcomes these hurdles.
Q 23. How do you utilize advanced imaging techniques for TEMS?
Advanced imaging plays a crucial role in successful TEMS procedures. We routinely utilize high-definition endoscopes with integrated cameras providing magnified views of the surgical field. This helps us to visualize fine anatomical details and perform precise dissections. Beyond endoscopy, we frequently employ intraoperative ultrasound (IOUS) and sometimes even fluoroscopy. IOUS allows real-time visualization of tissue layers and helps to guide our instruments precisely. This is especially important during resection of tumors close to critical structures. Fluoroscopy, though less commonly used, can be invaluable when dealing with complex pelvic anatomy or when precise placement of clips is essential. Integrating these imaging modalities provides a comprehensive picture, ensuring better surgical precision and minimizing the risk of complications. Imagine trying to navigate a complex maze without a map; the advanced imaging systems are our ‘maps,’ guiding us towards successful and safe surgical outcomes.
Q 24. What are the current research trends in TEMS?
Current research in TEMS focuses on several key areas. One prominent trend is the development of less invasive approaches, including the exploration of natural orifice transluminal endoscopic surgery (NOTES) techniques. The aim is to further minimize the need for external incisions. Another area of active research is the development of novel energy sources, including more refined laser systems and ultrasonic energy, to enhance precision during tissue dissection and hemostasis. Furthermore, there is increasing interest in using advanced imaging techniques, such as three-dimensional (3D) endoscopy and intraoperative optical coherence tomography (OCT), to improve visualization and aid in real-time assessment of tissue margins during tumor resection. Finally, research continues to explore the integration of robotic systems and artificial intelligence (AI) into TEMS to enhance surgical precision and efficiency. The goal is to improve surgical outcomes, reduce complications, and ultimately provide patients with a safer and less invasive treatment experience.
Q 25. Describe your experience with advanced suturing techniques in TEMS.
Advanced suturing techniques are absolutely critical in TEMS. We utilize various approaches, including endoscopic linear staplers, endo-GIA staplers, and specialized transanal suturing devices. The choice depends on the specific surgical situation and the anatomical location. For example, linear staplers are often used for resection of larger lesions or to create anastomoses, while endo-GIA staplers are better suited for smaller, more intricate closures. We often use absorbable sutures to minimize the need for further procedures to remove them. Proficiency in these techniques allows for a meticulous, controlled closure of the surgical site, reducing the risk of postoperative complications like leaks or fistulas. Mastering these techniques, like mastering any fine art, requires extensive practice and experience. I regularly engage in surgical simulation exercises and participate in surgical training programs to hone my skills and stay current with the latest advancements in suturing techniques.
Q 26. What is your experience with different types of energy sources used in TEMS?
A variety of energy sources are used in TEMS, each with its advantages and disadvantages. We commonly utilize monopolar electrocautery for hemostasis and tissue dissection. However, monopolar energy can cause thermal injury to surrounding tissues. Therefore, bipolar electrocautery is frequently preferred, as it delivers more precise energy application. We also utilize ultrasonic energy devices, which offer excellent hemostasis and precise dissection with less thermal spread than monopolar energy. Finally, laser systems, particularly those employing Nd:YAG or CO2 lasers, offer specific advantages in treating particular tissues. The selection of the appropriate energy source depends on various factors, including the type of tissue being dissected or resected, the proximity to critical structures, and the desired level of hemostasis. The decision-making process is akin to selecting the right tool for a particular job in a toolbox, carefully considering the properties of each and the overall surgical goal.
Q 27. How do you manage unexpected complications during a TEMS procedure?
Managing unexpected complications during TEMS requires a calm and systematic approach. The first step is to quickly assess the situation and identify the nature of the complication. This is often done with a combination of intraoperative imaging and careful examination. If bleeding occurs, we employ appropriate hemostasis techniques, such as bipolar cautery, clips, or the use of specialized hemostatic agents. If a perforation occurs, we try to assess the size and location. Small perforations might be managed conservatively, whereas larger ones may require repair with sutures or staplers. In cases of significant bleeding or a complex perforation, it might be necessary to convert to an open surgical approach to better control the situation. We always follow a standardized protocol for managing intraoperative complications, ensuring that we thoroughly document the event and take all necessary steps to prevent recurrence. Each case presents unique challenges, necessitating quick thinking and precise execution.
Q 28. Explain your understanding of the role of the surgical team in successful TEMS procedures.
A successful TEMS procedure relies heavily on a well-coordinated and highly skilled surgical team. The surgeon leads the procedure, making critical decisions and executing the technical aspects of the surgery. However, the scrub nurse plays a crucial role in maintaining a sterile field and preparing instruments. The circulating nurse coordinates the operating room environment, managing equipment, supplies, and patient monitoring. The anesthesiologist closely monitors the patient’s vital signs, adjusting medication as needed to maintain physiological stability. Experienced surgical assistants are essential for efficient retraction of tissue and assistance with intricate maneuvers. Effective communication and teamwork among the entire surgical team are paramount to a smooth and successful procedure. Each team member has a specific role, and the seamless integration of these roles ensures patient safety and optimal surgical outcome. It’s like a finely tuned orchestra – every member plays their part to create a harmonious and successful performance.
Key Topics to Learn for Transanal Endoscopic Microsurgery (TEMS) Interview
- Surgical Technique & Instrumentation: Mastering the nuances of TEMS surgical technique, including instrument handling, camera manipulation, and tissue dissection. Understanding the advantages and limitations of different instruments is crucial.
- Patient Selection & Preoperative Assessment: Develop a strong understanding of appropriate patient selection criteria, including evaluating anatomical suitability and assessing potential risks and complications. Familiarize yourself with relevant preoperative investigations and planning.
- Intraoperative Management & Complications: Thoroughly review potential intraoperative complications, such as bleeding, perforation, and injury to surrounding structures. Prepare to discuss strategies for managing these challenges and ensuring patient safety.
- Postoperative Care & Recovery: Gain expertise in postoperative management, including pain control, bowel management, and monitoring for potential complications. Understand the typical recovery trajectory for patients undergoing TEMS.
- Anatomical Knowledge: Demonstrate a deep understanding of the relevant anatomy, including the rectum, anus, and surrounding pelvic structures. This knowledge is fundamental to successful TEMS procedures.
- Comparison with Alternative Techniques: Be prepared to discuss the advantages and disadvantages of TEMS compared to other surgical approaches for similar conditions, such as traditional transabdominal surgery.
- Emerging Technologies & Advancements: Stay updated on recent advancements and emerging technologies in TEMS, showcasing your commitment to continuous professional development.
Next Steps
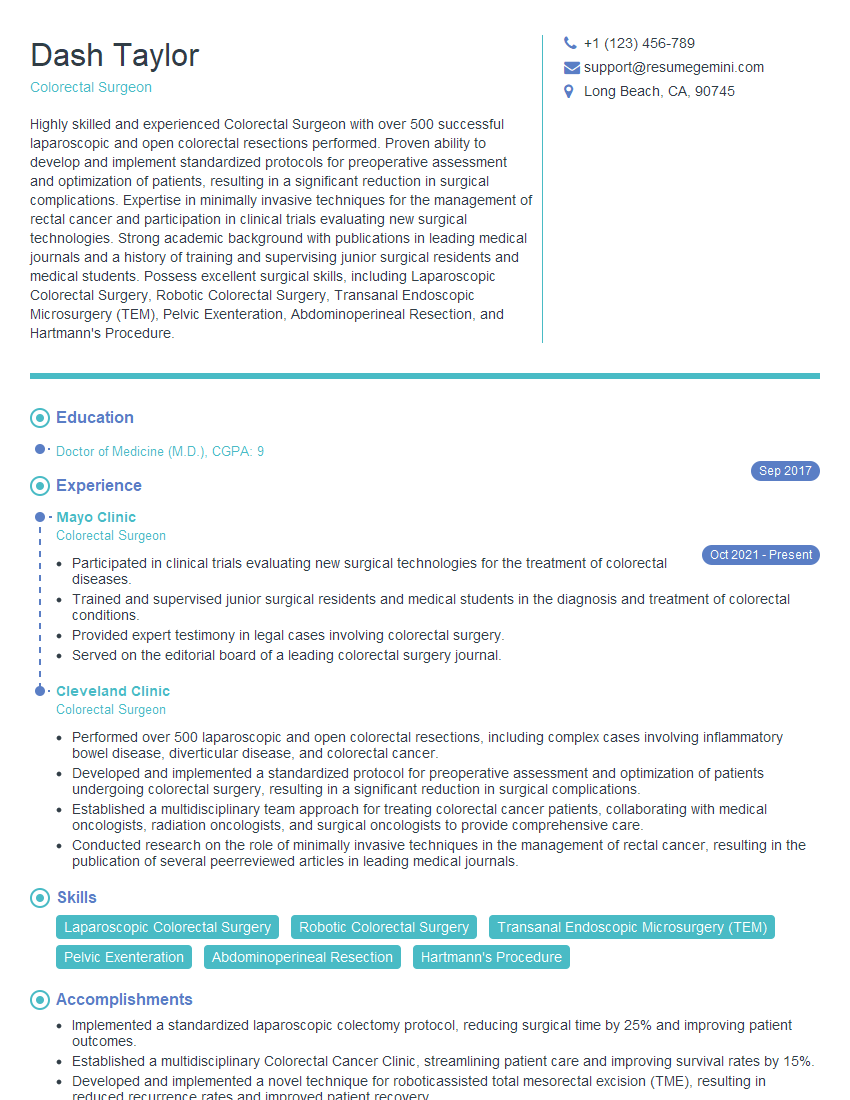
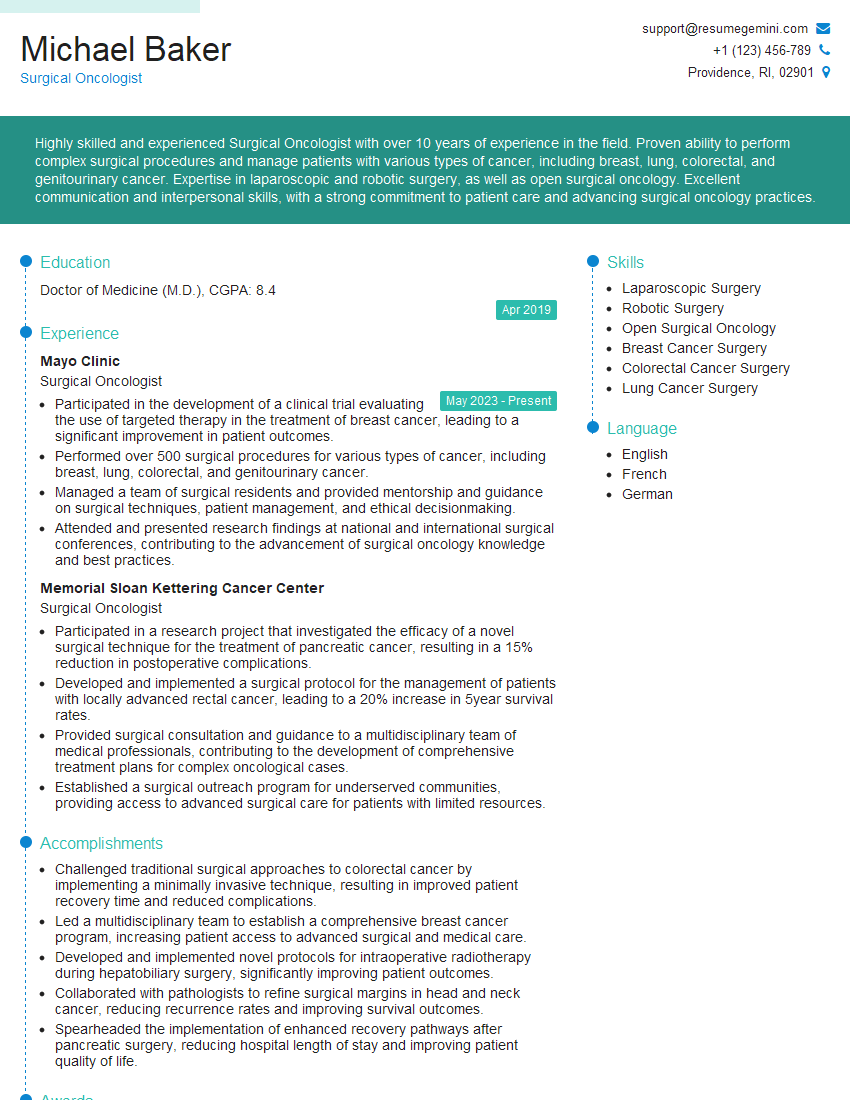
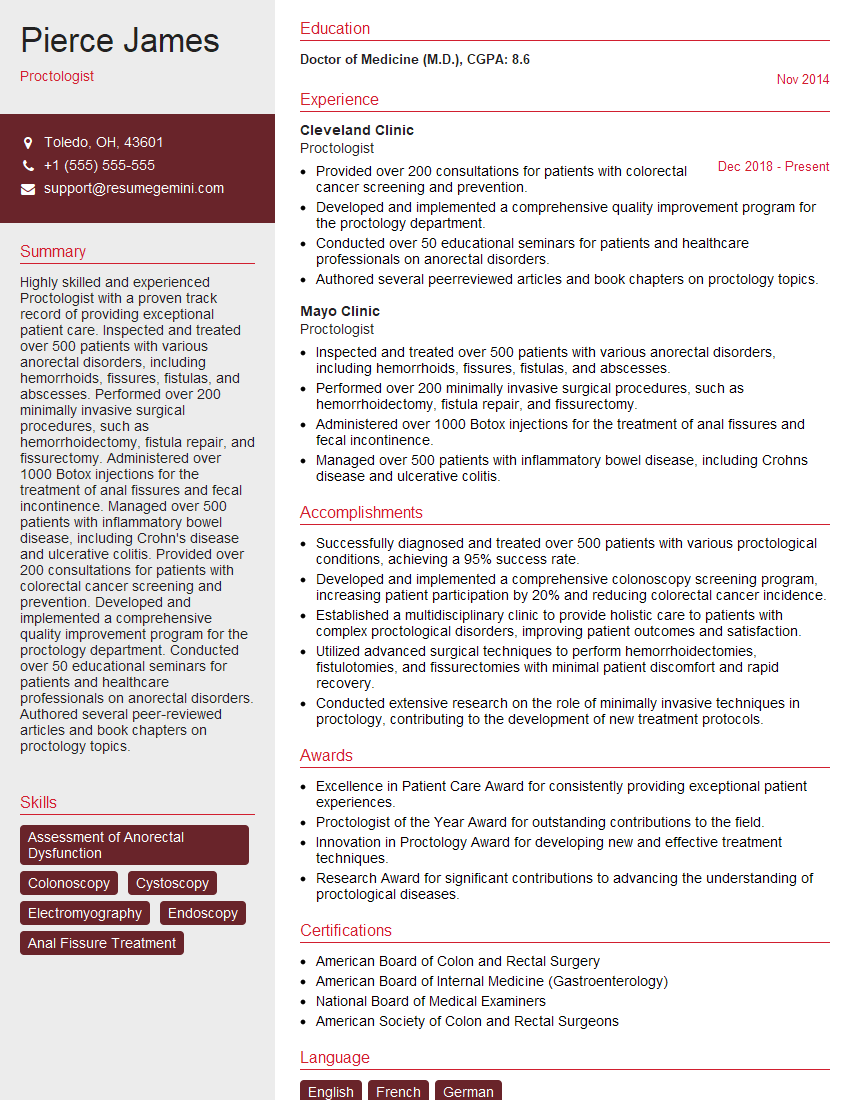
Mastering Transanal Endoscopic Microsurgery (TEMS) opens doors to exciting career opportunities and allows you to contribute significantly to minimally invasive colorectal surgery. A strong resume is key to showcasing your skills and experience to potential employers. Creating an ATS-friendly resume is crucial for maximizing your job prospects. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the demands of the TEMS field. Examples of resumes tailored specifically to Transanal Endoscopic Microsurgery (TEMS) positions are available through ResumeGemini, giving you a head start in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.