The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Transbronchial Lung Biopsy interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Transbronchial Lung Biopsy Interview
Q 1. Describe the indications for performing a transbronchial lung biopsy (TBLB).
Transbronchial lung biopsy (TBLB) is a minimally invasive procedure used to obtain tissue samples from the lungs for diagnostic purposes. Its primary indications revolve around investigating lung lesions or abnormalities detected through imaging (like CT scans or X-rays) or presenting with symptoms suggestive of lung disease.
- Suspicious pulmonary nodules or masses: When imaging reveals a lung nodule or mass of uncertain origin, a TBLB can help determine if it’s benign or malignant.
- Interstitial lung diseases (ILDs): TBLB aids in diagnosing various ILDs, such as sarcoidosis, hypersensitivity pneumonitis, and idiopathic pulmonary fibrosis, by providing tissue for pathological examination.
- Infections: In cases of suspected lung infections that are difficult to diagnose with other methods, TBLB can provide tissue for microbiological analysis (culture and staining).
- Evaluation of diffuse lung disease: When a patient presents with widespread lung involvement (e.g., shortness of breath, cough, and abnormal lung function tests), TBLB can help pinpoint the underlying cause.
- Staging of lung cancer: While not the primary method, TBLB can sometimes be used to help stage lung cancer, especially in cases where a less invasive approach is needed.
Essentially, whenever there’s a need to definitively diagnose a lung abnormality or disease through histological examination, and less invasive techniques prove inadequate, TBLB is considered.
Q 2. What are the contraindications for a TBLB?
TBLB, while minimally invasive, carries certain contraindications that must be carefully considered before the procedure. These contraindications can be broadly classified into:
- Severe respiratory compromise: Patients with severe respiratory distress or compromised respiratory function, such as those with severe COPD or acute respiratory failure, are at increased risk of respiratory complications.
- Uncontrolled bleeding disorders: Patients with uncontrolled bleeding disorders, or those on anticoagulants that cannot be safely held, are at a high risk of bleeding during and after the biopsy.
- Significant cardiovascular disease: Patients with severe cardiovascular disease, especially those with unstable angina or recent myocardial infarction, are at higher risk of cardiac complications.
- Severe obesity or significant pulmonary hypertension: These conditions can pose challenges during bronchoscopy and increase the risk of complications.
- Inability to cooperate: A patient’s inability to cooperate during the procedure can compromise the safety and efficacy of TBLB.
- Recent significant respiratory infection: An active respiratory infection increases the risk of infection spreading during the procedure.
A thorough assessment of the patient’s overall health is crucial to determine whether the benefits of TBLB outweigh the risks associated with the procedure. These contraindications often involve considering the risk/benefit ratio with a multidisciplinary team.
Q 3. Explain the procedure for performing a TBLB, including patient preparation and positioning.
The TBLB procedure typically involves several steps, beginning with patient preparation and positioning:
- Patient Preparation: Informed consent is obtained. Vital signs are monitored. An intravenous line is established. Prophylactic antibiotics are often given, and sometimes prophylactic corticosteroids.
- Positioning: The patient is usually positioned in a semi-sitting or lateral position, providing optimal access to the airways. Sedation or general anesthesia is administered to ensure patient comfort and cooperation.
- Bronchoscopy: A flexible bronchoscope is carefully advanced into the airways, guided by fluoroscopy (x-ray) in many cases. The bronchoscopist visualizes the target lesion or area of interest.
- Biopsy: Once the lesion is located, specialized forceps are introduced through the bronchoscope’s working channel to obtain tissue samples. Multiple biopsies might be taken from different areas to increase the diagnostic yield.
- Specimen Handling: The obtained tissue samples are carefully handled and processed for pathological examination, often involving multiple stains and potentially immunohistochemistry.
- Post-procedure Monitoring: Vital signs are monitored closely after the procedure to detect any potential complications, such as bleeding or pneumothorax (collapsed lung).
The entire procedure is monitored closely by a team, including the pulmonologist, respiratory therapist, and nurse anesthetist (depending on anesthesia type). The process is dynamic, adapting to the patient’s response and the specific characteristics of the lesion.
Q 4. What are the different types of forceps used in TBLB and when would you choose each?
Several types of forceps are used for TBLB, each with unique characteristics making them suitable for specific situations:
- Standard Biopsy Forceps: These are the most commonly used forceps with jaws that grasp tissue. They are suitable for obtaining tissue from relatively accessible areas.
- Small Biopsy Forceps: These are used when obtaining samples from smaller or more delicate lesions where a less aggressive approach is desired.
- Suction Biopsy Forceps: These forceps have a suction mechanism which allows removal of small tissue samples and sometimes fluid from the lung, often from areas of consolidation.
- Radial-End Biopsy Forceps: These forceps have a larger jaw opening, enabling larger samples to be obtained. These might be used to sample larger nodules or masses.
- Ultrasonic Biopsy Forceps: These specialized forceps employ ultrasonic energy to disrupt tissue and enhance sample acquisition, useful for harder tissues.
The choice of forceps depends on factors such as the size, location, and consistency of the lesion, as well as the experience of the bronchoscopist. For instance, small biopsy forceps might be preferred for a small, fragile lesion in a peripheral airway, whereas radial-end forceps might be chosen for a larger, more central lesion.
Q 5. Describe the complications associated with TBLB and how they are managed.
TBLB, despite being minimally invasive, is associated with potential complications. These are generally uncommon but require careful monitoring and management:
- Bleeding: Hemoptysis (coughing up blood) is the most frequent complication. This can range from minimal to life-threatening. Management includes close monitoring, supportive care (oxygen, blood transfusion if needed), and potentially bronchoscopic intervention to control the bleeding.
- Pneumothorax (collapsed lung): Air leakage into the pleural space can cause a pneumothorax, requiring chest tube placement in some cases. It requires close monitoring and appropriate treatment based on the severity of the collapse.
- Infection: Infection at the biopsy site or pneumonia is a possibility, usually managed with antibiotics.
- Bronchospasm: Constriction of the airways can occur, managed with bronchodilators.
- Hypoxemia (low blood oxygen): This is common and usually managed with oxygen supplementation. Severe cases may require mechanical ventilation.
- Cardiac arrhythmias: Rare but possible; monitored carefully. Treatment varies based on the type of arrhythmia.
Careful patient selection, adherence to proper technique, and vigilant post-procedure monitoring are crucial to minimize the risk and effectively manage these complications.
Q 6. How do you interpret the biopsy results obtained from a TBLB?
Interpreting TBLB results involves a collaborative effort between the pulmonologist, pathologist, and other specialists as needed. The pathologist examines the tissue samples microscopically to identify cellular features, architectural patterns, and any infectious organisms.
- Histopathological examination: The pathologist assesses the tissue architecture to determine the type of cells present and identify any abnormalities such as inflammation, fibrosis, or malignancy.
- Immunohistochemistry (IHC): This technique uses antibodies to identify specific proteins within the cells, which can be crucial in diagnosing certain diseases, particularly cancers.
- Microbiological analysis: If an infection is suspected, the tissue sample will be cultured to identify the causative organism and determine its sensitivity to antibiotics.
- Correlation with clinical findings: The pathologist’s findings are integrated with the patient’s clinical history, imaging results, and other laboratory data to reach a definitive diagnosis.
The report will provide a detailed description of the microscopic findings, including the diagnosis and any additional relevant information. This information is fundamental for guiding the appropriate treatment strategy for the patient.
Q 7. What are the advantages and disadvantages of TBLB compared to other diagnostic methods?
TBLB, while valuable, needs to be weighed against other diagnostic methods. Let’s explore its advantages and disadvantages:
Advantages:
- Minimally invasive: Compared to open lung surgery, TBLB is less invasive, with a shorter recovery period and fewer risks.
- Relatively safe: With proper selection and technique, the procedure is generally safe, and serious complications are rare.
- Direct tissue sampling: Provides definitive diagnosis via direct visualization and tissue sampling, unlike imaging alone.
- Cost-effective in selected cases: In many cases, it can avoid the need for more extensive and costly procedures.
Disadvantages:
- Limited diagnostic yield: TBLB may not yield sufficient tissue in all cases, particularly with peripheral lesions or very small nodules.
- Potential complications: While uncommon, bleeding, pneumothorax, and infection are possible complications.
- Not suitable for all lesions: It is not suitable for all lung lesions, especially deep-seated or inaccessible ones.
- Patient factors: The procedure relies on patient cooperation, which may limit its use in some individuals.
The decision of whether or not to perform a TBLB is made on a case-by-case basis, taking into account the patient’s clinical presentation, imaging findings, and the potential risks and benefits of the procedure. Other methods like video-assisted thoracoscopic surgery (VATS) or surgical lung biopsy might be considered if TBLB is deemed unsuitable or yields insufficient diagnostic information.
Q 8. How do you manage a pneumothorax following a TBLB?
Managing a pneumothorax after a transbronchial lung biopsy (TBLB) is a critical aspect of the procedure. A pneumothorax, or collapsed lung, occurs when air leaks into the pleural space, the area between the lung and the chest wall. Its severity ranges from minor to life-threatening, necessitating prompt and appropriate management.
Initial Assessment: The first step involves a thorough clinical assessment, including physical examination (auscultation for diminished breath sounds) and chest X-ray to confirm the diagnosis and determine the size of the pneumothorax. Small pneumothoraces (less than 15% of the hemithorax) may be managed conservatively with close monitoring of respiratory status and oxygen saturation. Larger pneumothoraces, or those causing respiratory distress, require intervention.
Management Strategies:
- Supplemental Oxygen: Providing supplemental oxygen helps improve oxygenation and minimizes the risk of hypoxia.
- Chest Tube Insertion: For larger or symptomatic pneumothoraces, a chest tube is typically inserted to evacuate the air from the pleural space and re-expand the lung. This is often done under image guidance (fluoroscopy) to ensure accurate placement.
- Observation and Serial Chest X-Rays: Close monitoring with serial chest X-rays is essential to track the resolution of the pneumothorax. The chest tube is typically removed once the lung is fully re-expanded and there is no evidence of ongoing air leak.
Example: I recently managed a patient who developed a moderate-sized pneumothorax after a TBLB. Due to the patient’s respiratory distress, a chest tube was promptly inserted. The pneumothorax resolved within 48 hours, and the chest tube was successfully removed. Post-procedure, the patient was monitored closely and made a full recovery.
Q 9. What are the different approaches to performing a TBLB (e.g., flexible vs. rigid bronchoscopy)?
TBLB can be performed using either flexible or rigid bronchoscopy, each with its own advantages and disadvantages.
Flexible Bronchoscopy: This approach uses a thin, flexible bronchoscope that can navigate through smaller airways and is generally better tolerated by patients. It’s less invasive and can reach more peripheral lung lesions. However, it can be more challenging to obtain a sufficient tissue sample compared to rigid bronchoscopy. Navigation to a specific area is heavily reliant on prior imaging (CT or EBUS).
Rigid Bronchoscopy: This technique employs a thicker, rigid bronchoscope which provides better visualization and allows for more forceful sampling techniques, potentially increasing the diagnostic yield. It’s usually preferred for lesions that are easily accessible. The procedure is however more invasive and requires greater patient sedation and cooperation.
Choosing the Right Approach: The choice between flexible and rigid bronchoscopy depends on various factors, including the location and size of the lesion, the patient’s clinical condition, and the operator’s experience. For example, a deeply seated lesion may be better accessed with flexible bronchoscopy guided by EBUS or CT. Conversely, a large, easily accessible lesion may be easily sampled with rigid bronchoscopy.
Q 10. Explain your experience with various TBLB techniques (e.g., cryobiopsy, forceps biopsy).
My experience encompasses a range of TBLB techniques, each with specific applications and limitations.
Forceps Biopsy: This is a commonly used technique where biopsy forceps are advanced through the bronchoscope to obtain tissue samples. It is relatively straightforward, but the sample size and quality can be variable depending on the lesion’s consistency and the operator’s skill. It is suitable for lesions with a relatively soft texture.
Cryobiopsy: Cryobiopsy uses a cryoprobe to freeze and then extract a tissue sample. Freezing the tissue creates a sharper demarcation between the sample and surrounding tissue, minimizing bleeding and potentially increasing sample size and diagnostic yield. It’s particularly useful for firmer or harder lung lesions. However, it does require specialized equipment and expertise.
In Practice: The choice of technique depends on the lesion’s characteristics. For instance, if a lesion is superficial and readily accessible, forceps biopsy might suffice. For deeper or firmer lesions, cryobiopsy might be preferable. I carefully assess each patient’s individual case to select the most appropriate method to optimize the diagnostic yield while minimizing risks.
Q 11. Describe your experience with using image guidance (e.g., EBUS, CT) during TBLB.
Image guidance plays a vital role in enhancing the precision and safety of TBLB. Both EBUS (endobronchial ultrasound) and CT guidance can significantly improve the targeting of the lesion and reduce the number of blind passes needed to obtain an adequate sample.
EBUS-guided TBLB: EBUS uses ultrasound to visualize the airways and surrounding lung tissue. It allows for precise targeting of suspicious lesions, even those located peripherally. This approach minimizes the risk of pneumothorax by ensuring accurate placement of the biopsy forceps.
CT-guided TBLB: CT guidance utilizes real-time CT imaging to pinpoint the lesion’s location. This technique is particularly useful when the lesion is difficult to reach bronchoscopically. It might be coupled with navigation software to assist with precise bronchoscopic advancement.
Real-World Application: I frequently use EBUS guidance for TBLB, especially when dealing with peripheral or small lesions. The ultrasound images provide crucial information for the optimal approach and significantly improve sampling accuracy, reducing the need for multiple passes.
Q 12. How do you assess the adequacy of a TBLB sample?
Assessing the adequacy of a TBLB sample is crucial for an accurate diagnosis. Several factors are considered:
Sample Size and Quality: Sufficient tissue is essential for pathologists to perform a thorough analysis. The sample should be large enough and well-represented, with minimal crush artifacts. A small or fragmented sample might lead to an inconclusive diagnosis.
Tissue Type: The type of tissue obtained must align with the suspected pathology. For instance, if the patient presents with a suspected malignancy, the sample should contain sufficient viable neoplastic tissue for proper diagnosis.
Pathology Report: The pathology report is the ultimate determinant of sample adequacy. It details the findings, including tissue type, cellularity, and diagnostic implications. In cases where the initial sample is inadequate, repeat bronchoscopy with additional tissue sampling might be necessary.
Example: If a small, fragmented sample is obtained, I would discuss the findings with the pathologist and consider a repeat procedure using alternative techniques or image guidance to obtain a more substantial and representative sample.
Q 13. What are the quality control measures you implement to ensure accurate TBLB results?
Ensuring accurate TBLB results requires stringent quality control measures at every stage of the process. These include:
- Proper Patient Selection: Careful patient selection based on clinical presentation, imaging findings, and assessment of risk factors helps ensure that the procedure is appropriate and increases the chance of obtaining a diagnostic sample.
- Sterile Technique: Maintaining strict sterile technique during the procedure minimizes the risk of infection and ensures accurate sample collection.
- Appropriate Sample Handling: Proper labeling, fixation, and transportation of the tissue samples are crucial to prevent degradation and ensure accurate processing and analysis by the pathologist. I personally use specific transport media according to the sample type.
- Regular Equipment Maintenance: Regular calibration and maintenance of bronchoscopic equipment are essential to ensure optimal image quality and function.
- Regular Staff Training: Continuous training and competency assessments for all staff involved in the procedure maintain high standards of practice.
Continuous Improvement: We actively participate in quality assurance programs, audits, and review processes to continuously refine our techniques and ensure the highest possible standards of care.
Q 14. How do you manage a bleeding complication during a TBLB?
Bleeding complications during TBLB are a concern. The severity of bleeding ranges from minimal to life-threatening. Management depends on the severity and location of the bleed.
Mild Bleeding: Mild bleeding often resolves spontaneously or with simple measures such as direct pressure with the bronchoscope or application of local hemostatic agents such as epinephrine.
Moderate to Severe Bleeding: More substantial bleeding requires more aggressive intervention. Techniques include:
- Bronchial artery embolization: This procedure involves the injection of embolic material into the bleeding bronchial artery to stop the flow of blood. This would be done in radiology by a interventional radiologist.
- Surgical intervention: In rare instances, surgery might be needed to control life-threatening bleeding. This is typically reserved for cases where less invasive methods are unsuccessful.
Example: I once encountered a patient who experienced moderate bleeding after a TBLB. We initially managed the bleeding with local epinephrine and direct pressure. When the bleeding persisted, we consulted with Interventional radiology and performed a bronchial artery embolization which successfully stopped the bleeding.
Prevention: Preventive measures such as careful selection of biopsy techniques, precise targeting of the lesion, and the use of appropriate instruments (e.g. cryobiopsy for reducing bleeding) can minimize the risk of bleeding complications.
Q 15. What are the ethical considerations involved in performing a TBLB?
Ethical considerations in Transbronchial Lung Biopsy (TBLB) primarily revolve around obtaining informed consent, balancing risks and benefits, and ensuring patient safety and well-being. The procedure involves potential complications, so it’s crucial that patients understand these risks and the procedure’s purpose before giving consent. This necessitates a clear explanation of the procedure, including its potential benefits, alternatives (if any), and the likelihood of complications, such as bleeding, pneumothorax (collapsed lung), or infection. The patient must also understand that the biopsy might not provide a definitive diagnosis and that further testing may be necessary. Furthermore, ethical considerations include ensuring the patient’s autonomy in decision-making and addressing any anxieties or concerns they may have. For example, if a patient is hesitant due to a fear of needles or the procedure itself, addressing those concerns compassionately and professionally is paramount. Transparency and open communication are key to ensuring ethical practice.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the role of a respiratory therapist in assisting with a TBLB procedure.
A respiratory therapist plays a vital role in assisting with TBLB, acting as an indispensable member of the procedure team. Their responsibilities begin pre-procedure with patient assessment, including pulmonary function tests (PFTs) to evaluate respiratory status and identify any potential risks. During the procedure, they monitor the patient’s vital signs closely, including oxygen saturation, heart rate, respiratory rate, and blood pressure. They also assist with the bronchoscope insertion and positioning, maintaining airway patency and suctioning as needed. They are skilled in managing airway complications that might arise, such as bronchospasm or hypoxemia (low blood oxygen levels). Post-procedure, the respiratory therapist monitors the patient’s recovery, administering oxygen therapy, providing respiratory support, and educating the patient on post-procedure care and signs of complications such as a pneumothorax. Their expertise in respiratory physiology and critical care is crucial for ensuring patient safety and a smooth procedure.
Q 17. How would you explain the procedure and potential risks to a patient before a TBLB?
Explaining the TBLB procedure and potential risks to a patient requires a clear, compassionate, and patient-centered approach. I would begin by explaining the purpose of the biopsy, emphasizing that it’s designed to obtain a tissue sample from the lung to help diagnose a suspected lung condition. I would then describe the procedure in simple terms, mentioning that a thin, flexible tube (bronchoscope) will be inserted through the nose or mouth into the airways to reach the suspicious area. The procedure will be performed under sedation, minimizing discomfort. Crucially, I would discuss the potential benefits of the procedure, such as obtaining a definitive diagnosis to guide treatment, while highlighting the potential risks. These risks would include bleeding, pneumothorax (collapsed lung), infection, and rarely, heart rhythm abnormalities. I’d explain the likelihood of these complications, emphasizing that they are generally low but nonetheless possible. I’d also mention that there’s a chance the biopsy might not yield enough tissue for a definitive diagnosis. Finally, I would answer any questions the patient might have and ensure they fully understand the risks and benefits before giving their informed consent. I often use analogies, such as comparing the bronchoscope to a very thin, flexible straw to help patients visualize the procedure.
Q 18. What are the limitations of TBLB?
TBLB, while a valuable diagnostic tool, has several limitations. One key limitation is its inability to reach peripheral lesions (lesions located far away from the central airways). The bronchoscope’s reach is limited, and lesions situated deep within the lung parenchyma may be inaccessible. Another limitation is the possibility of obtaining an inadequate or non-diagnostic tissue sample. This can happen if the lesion is too small, too difficult to access, or if the biopsy technique fails to obtain sufficient tissue. The procedure also has a risk of complications, as mentioned previously, which can limit its use in certain patients, such as those with severe respiratory compromise or bleeding disorders. Finally, it’s not suitable for all lung diseases. For example, diffuse interstitial lung diseases might not provide enough diagnostic information from a localized biopsy. These limitations highlight the importance of careful patient selection and the need to consider alternative diagnostic approaches when necessary.
Q 19. How do you handle unexpected findings during a TBLB procedure?
Unexpected findings during a TBLB procedure, such as profuse bleeding or a sudden respiratory deterioration, necessitate a rapid and decisive response. The immediate priority is to ensure patient safety. In case of significant bleeding, the bronchoscope might be used to apply pressure or inject hemostatic agents to control the bleeding. If respiratory distress occurs, supplemental oxygen will be administered, and if needed, the patient may be intubated and placed on mechanical ventilation. Depending on the severity of the situation, the procedure might be terminated. The patient’s vital signs will be monitored continuously, and further investigations and interventions will be carried out as needed. The entire team needs to be prepared to handle such contingencies. Clear communication amongst the team is crucial; it is important to document the unexpected finding and all subsequent actions taken.
Q 20. How do you differentiate between benign and malignant findings in a TBLB specimen?
Differentiating between benign and malignant findings in a TBLB specimen relies heavily on the expertise of a pathologist who analyzes the tissue sample under a microscope. Key features examined include cellular morphology (shape and appearance of cells), the degree of cellular atypia (abnormalities in cell structure), and the presence of mitotic figures (cells undergoing division). Malignant cells typically exhibit significant atypia, including irregular nuclei, increased nuclear-to-cytoplasmic ratio, and abnormal chromatin patterns. Immunohistochemical stains (using antibodies to identify specific proteins) are often used to characterize the cells further and help determine their origin and type. Furthermore, the pathologist considers the architectural features of the tissue sample, such as the arrangement and organization of cells, to assess the presence of invasion or metastasis. For instance, the presence of glandular structures might indicate an adenocarcinoma, whereas the formation of nests or sheets of cells might suggest a squamous cell carcinoma. However, definitive diagnosis often needs a comprehensive approach combining clinical, radiological, and pathological findings.
Q 21. What are the specific safety protocols you adhere to during TBLB procedures?
Specific safety protocols during TBLB procedures are stringent and meticulously followed to minimize risks to the patient. These protocols include pre-procedure assessment of the patient’s respiratory and cardiovascular status, including obtaining informed consent. The procedure is performed under strict sterile conditions, following guidelines for infection control. Monitoring the patient’s vital signs throughout the procedure is crucial, with adjustments made to oxygen supply and sedation levels as needed. Appropriate emergency equipment, such as suction apparatus and resuscitation equipment, should always be readily available. Proper sedation and analgesia protocols are adhered to to minimize patient discomfort. Post-procedure, patients are monitored closely for any signs of complications, such as bleeding, pneumothorax, or infection, and receive appropriate post-procedure care. Continuous monitoring and communication between the medical team members ensure patient safety and the smooth execution of the procedure.
Q 22. Discuss your experience with reporting TBLB results to referring physicians.
Reporting Transbronchial Lung Biopsy (TBLB) results requires meticulous attention to detail and clear communication. My approach involves a structured report that includes macroscopic descriptions of the obtained tissue, details on the location of the biopsy within the lung (as best determined), and a concise summary of the microscopic findings provided by the pathologist. I always correlate the findings with the clinical presentation and imaging data to create a comprehensive interpretation.
For instance, if a patient presented with a suspicious nodule on CT scan, and the TBLB showed granulomatous inflammation, I would report this finding, its implications (e.g., possibility of sarcoidosis), and recommendations for further investigation such as additional imaging or serological tests. I always strive to provide a clinically relevant interpretation, avoiding overly technical language that might confuse the referring physician. I am also readily available to discuss the results in more detail if needed, explaining the significance of the findings and answering any questions they may have.
A crucial aspect is emphasizing the limitations of the procedure. For example, if the sample size was small, or the biopsy site wasn’t precisely targeted, I highlight these factors in the report to ensure appropriate clinical management. Open communication and collaborative discussion are key to optimizing patient care.
Q 23. What are the key differences between transbronchial needle aspiration (TBNA) and TBLB?
Both transbronchial needle aspiration (TBNA) and transbronchial lung biopsy (TBLB) are minimally invasive procedures used to obtain tissue samples from the lung for diagnosis, but they differ significantly in their technique and the type of sample obtained.
- TBNA uses a needle to aspirate cells from a lesion. It’s ideal for obtaining cytological samples, particularly in lesions close to the airway. The yield of tissue is generally less than in TBLB, and the obtained material is usually limited to cells or small fragments.
- TBLB involves the use of forceps to obtain larger tissue fragments. This allows for better histological evaluation and a more definitive diagnosis, especially for processes like granulomas or tumors that require architectural assessment. However, it carries a slightly higher risk of complications, such as bleeding or pneumothorax, due to the larger tissue sample obtained.
In short: TBNA is like taking a small sample of juice from a fruit, while TBLB is more like taking a slice of the fruit itself. The choice between the two depends on factors like lesion accessibility, the type of diagnosis suspected, and patient-specific factors.
Q 24. Describe your experience with managing post-procedure complications like infection.
Post-procedure complications following TBLB, such as infection and pneumothorax (collapsed lung), are rare but require careful attention. My experience involves a proactive approach to minimizing risks and managing any complications effectively.
- Infection: Prophylactic antibiotics are not routinely given unless there is a specific indication (like immunocompromised status). Post-procedure monitoring includes observing for fever, cough, and increased sputum production. If an infection develops, prompt treatment with appropriate antibiotics based on cultures is initiated.
- Pneumothorax: This is monitored through chest X-ray post-procedure. Small pneumothoraces often resolve spontaneously, but larger ones may require chest tube insertion. Oxygen therapy can assist in re-expansion of the lung.
Patient education plays a critical role. I emphasize the importance of reporting any concerning symptoms (e.g., shortness of breath, chest pain) to their healthcare provider immediately. Close follow-up and prompt intervention are essential for optimal patient outcomes. Proper sterile technique during the procedure itself is paramount in preventing these complications.
Q 25. What are the latest advancements and technologies in TBLB?
TBLB continues to evolve. Several advancements are improving diagnostic accuracy and reducing risks:
- Advanced imaging guidance: Integration of techniques like endobronchial ultrasound (EBUS) and electromagnetic navigation bronchoscopy (ENB) allows for more precise targeting of lesions, particularly those that are difficult to reach with conventional bronchoscopy. This leads to improved diagnostic yield and minimizes the risk of complications.
- Improved instrumentation: The development of smaller, more flexible forceps and needles enhances maneuverability and accessibility, facilitating biopsies of challenging lesions.
- Cryobiopsy: This technique uses cryoprobes to freeze and fragment tissue samples, which facilitates the collection of larger and more representative samples from a wider range of lesions. It also aids in hemostasis during and after the procedure.
These advancements represent significant progress in making TBLB a safer and more effective diagnostic tool.
Q 26. How do you stay updated on the best practices and guidelines for TBLB?
Staying current on best practices and guidelines for TBLB involves a multifaceted approach:
- Professional societies: Active participation in relevant professional societies like the American Thoracic Society (ATS) and the European Respiratory Society (ERS) provides access to the latest research, guidelines, and updates in the field.
- Peer-reviewed journals: Regularly reviewing leading journals in pulmonology and respiratory medicine keeps me abreast of the newest advancements and evidence-based practices.
- Continuing medical education (CME): Participation in CME activities, conferences, and workshops allows for engagement with experts and exposure to the most recent innovations and techniques.
- Collaborative networks: Maintaining close connections with colleagues and other specialists in the field enables the exchange of experiences and best practices.
This ongoing learning ensures I provide the highest quality of care and adhere to the most current and evidence-based guidelines in TBLB procedures.
Q 27. How would you troubleshoot a difficult-to-reach lesion during TBLB?
Troubleshooting a difficult-to-reach lesion during TBLB necessitates a systematic and adaptable approach.
- Assessment: Carefully review the imaging studies (CT, PET scans) to precisely locate the lesion’s position relative to the airways.
- Bronchoscopic navigation: Utilize advanced bronchoscopic techniques such as EBUS or ENB, which provide real-time imaging guidance to navigate to the lesion effectively.
- Adjusting technique: If necessary, alter the approach angle or the type of instrument used (e.g., switching to a smaller forceps or needle).
- Seeking assistance: In complex cases, don’t hesitate to consult with experienced colleagues or seek guidance from specialists proficient in advanced bronchoscopic techniques.
- Alternative techniques: If TBLB proves unsuccessful, consider alternative diagnostic approaches, such as video-assisted thoracoscopic surgery (VATS) or percutaneous needle biopsy.
Flexibility, expertise in various bronchoscopic techniques, and a willingness to adapt are crucial for successful management of challenging cases.
Q 28. Describe a challenging TBLB case and how you overcame the challenges.
One particularly challenging case involved a patient with a small, peripheral lung nodule detected on CT, highly suspicious for malignancy. The lesion was located in a segmental bronchus difficult to access with standard bronchoscopy. Initial attempts at TBLB using conventional techniques proved unsuccessful.
To overcome this challenge, we employed EBUS-guided bronchoscopy. EBUS provided real-time ultrasound imaging of the lung parenchyma, enabling precise targeting of the nodule. Using this guidance, we successfully obtained a biopsy sample. The pathology revealed adenocarcinoma, confirming the clinical suspicion. The patient then underwent surgery based on this definitive diagnosis.
This case highlighted the crucial role of advanced bronchoscopic techniques in improving the diagnostic yield for difficult-to-reach lesions. The successful use of EBUS-guided TBLB avoided the need for more invasive procedures and allowed for timely and effective management.
Key Topics to Learn for Transbronchial Lung Biopsy Interview
- Indications and Contraindications: Understanding the appropriate patient populations for TBLB and situations where it’s not suitable. Consider factors like disease severity, patient comorbidities, and alternative diagnostic options.
- Procedure Technique: Mastering the steps involved, from bronchoscope insertion and navigation to biopsy acquisition and specimen handling. Think about potential complications and how to mitigate them.
- Complications and Management: Thoroughly understand potential risks such as bleeding, pneumothorax, infection, and airway compromise. Prepare to discuss preventative measures and emergency response strategies.
- Interpreting Results: Familiarize yourself with the process of analyzing biopsy samples, correlating findings with clinical presentation, and understanding the limitations of the procedure.
- Pre- and Post-Procedure Care: Detail the necessary preparations before the procedure, including patient education and consent. Outline the essential post-procedure monitoring and recovery steps.
- Technological Advancements: Stay abreast of the latest technological advancements in bronchoscopy and biopsy techniques, including navigation systems and image-guided procedures.
- Ethical Considerations: Discuss the ethical considerations surrounding informed consent, risk assessment, and potential limitations of the procedure.
- Comparison to Alternative Diagnostic Methods: Be prepared to discuss TBLB in the context of other diagnostic modalities, highlighting its strengths and weaknesses relative to them.
Next Steps
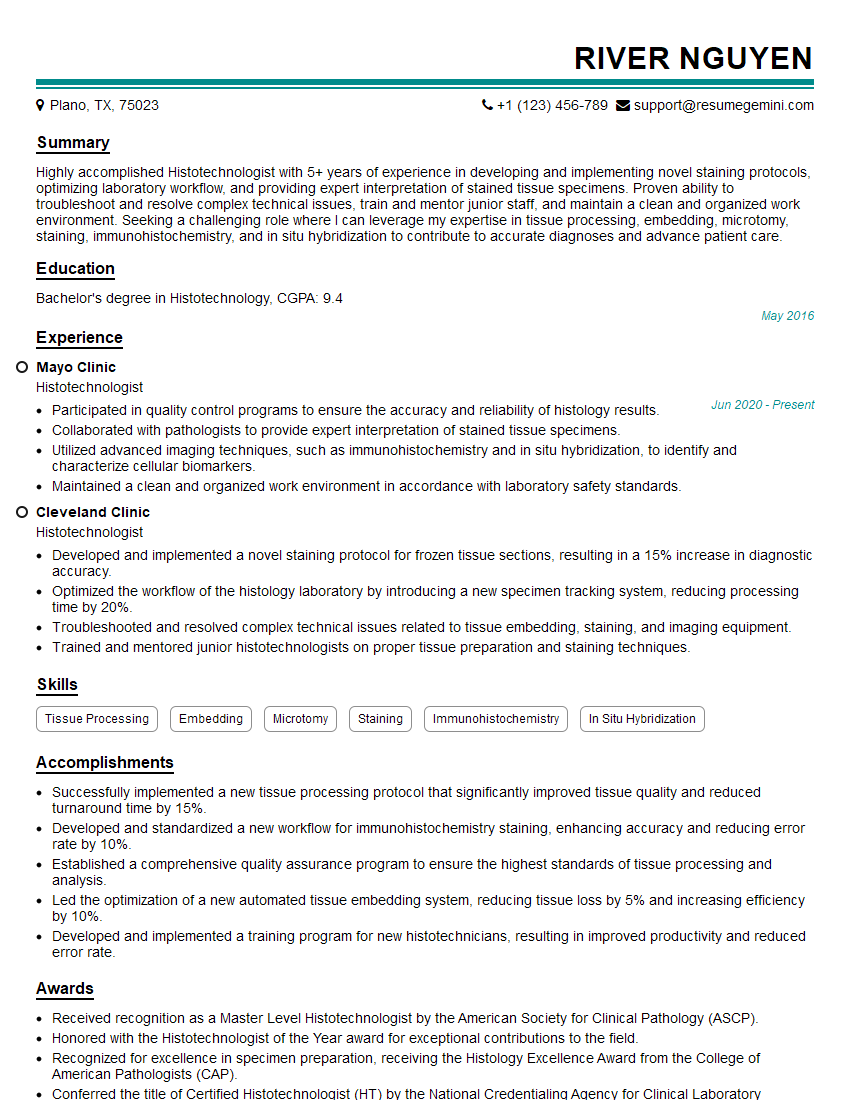
Mastering Transbronchial Lung Biopsy significantly enhances your expertise in pulmonary medicine and opens doors to advanced roles and research opportunities. To make the most of your preparation, a strong, ATS-friendly resume is crucial for capturing the attention of recruiters. ResumeGemini is a trusted resource to help you craft a professional and impactful resume that highlights your skills and experience effectively. ResumeGemini offers examples of resumes tailored to Transbronchial Lung Biopsy professionals, enabling you to create a document that truly showcases your qualifications. Take the next step in your career journey – build a resume that reflects your expertise and helps you land your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.