Unlock your full potential by mastering the most common Tumor Resection interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Tumor Resection Interview
Q 1. Describe the different surgical approaches for tumor resection.
Tumor resection, the surgical removal of a tumor, employs various approaches tailored to the tumor’s location, size, and type. The choice of approach significantly impacts the extent of surgery, potential complications, and the patient’s recovery.
- Open Surgery: This traditional method involves a large incision to directly access and remove the tumor. It offers excellent visualization and allows for thorough exploration of the surrounding tissues. For example, a large, centrally located lung tumor might necessitate a thoracotomy (incision into the chest wall).
- Minimally Invasive Surgery (MIS): This approach utilizes smaller incisions, often assisted by laparoscopy or robotics. Smaller incisions lead to less pain, reduced scarring, and quicker recovery times. Laparoscopic cholecystectomy (gallbladder removal) is a classic example, and this technique is increasingly used for certain types of colorectal or kidney tumors.
- Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiation Therapy (SBRT): While not strictly surgical resection, these techniques use highly focused radiation beams to destroy tumors with pinpoint accuracy, often avoiding the need for a larger surgical procedure. This is particularly useful for small, well-defined tumors in hard-to-reach areas of the brain or body.
- Endoscopic Surgery: Involves inserting a thin, flexible tube with a camera and surgical instruments to reach and remove tumors through natural orifices, like the mouth or anus. This is beneficial for tumors in the gastrointestinal tract or some types of brain tumors.
The selection of surgical approach is a multidisciplinary decision involving surgeons, oncologists, radiologists, and other specialists.
Q 2. Explain the concept of ‘surgical margins’ and their importance in tumor resection.
Surgical margins refer to the amount of healthy tissue removed along with the tumor. Achieving clear margins is paramount to prevent tumor recurrence. Imagine cutting out a cookie – you need to cut a bit beyond the edges to ensure you don’t leave any crumbs behind.
- Negative margins (R0 resection): No microscopic cancer cells are found at the edge of the resected tissue. This is the ideal scenario.
- Positive margins (R1 resection): Microscopic cancer cells are found at the edge of the resected tissue. This necessitates further treatment, often adjuvant therapies like chemotherapy or radiation.
- Close or positive margins (R2 resection): Cancer cells are found close to the edges of the resection or are macroscopically visible on the specimen, indicating incomplete resection and a significantly higher risk of recurrence.
The desired margin width depends on the type and aggressiveness of the tumor. For example, a highly aggressive tumor might require wider margins to minimize recurrence compared to a slow-growing tumor. Pathologists meticulously examine the resected tissue under the microscope to determine the margin status.
Q 3. What are the key considerations for choosing the optimal surgical technique for a specific tumor?
Choosing the optimal surgical technique is a complex process that considers several factors:
- Tumor characteristics: Size, location, type (benign or malignant), and aggressiveness greatly influence surgical strategy. A small, well-localized brain tumor might be amenable to SRS, while a large, invasive liver tumor may require a complex open resection.
- Patient factors: Overall health, age, comorbidities (other medical conditions), and fitness for surgery influence the choice of technique. Minimally invasive techniques might be preferred for older or frail patients.
- Extent of disease: Metastatic disease (cancer spread to other parts of the body) may alter the surgical approach. Resectability might be limited if the tumor is extensively involved with adjacent structures.
- Surgical expertise: The availability of skilled surgeons with experience in specific techniques is crucial. Complex procedures require specialized training and equipment.
- Oncological goals: The primary goal is to achieve complete resection with negative margins and improve patient outcomes.
A multidisciplinary team approach is critical, with input from surgeons, oncologists, and radiologists to develop the best surgical plan.
Q 4. How do you assess the resectability of a tumor pre-operatively?
Pre-operative assessment of resectability aims to determine whether the tumor can be completely removed surgically without causing unacceptable morbidity (harm) to the patient. This involves a comprehensive evaluation:
- Imaging studies: CT scans, MRI, and PET scans precisely locate and characterize the tumor, assessing its size, invasion into adjacent organs, and presence of metastases.
- Biopsy: A tissue sample is obtained to confirm the diagnosis and determine the tumor’s grade and type, which impacts the surgical strategy.
- Clinical examination: A thorough physical examination helps identify any signs of distant metastasis or local extension of the tumor.
- Functional assessments: Depending on the tumor location, tests might be performed to assess organ function, such as pulmonary function tests before lung surgery.
If the tumor is deemed unresectable due to extensive spread or involvement of critical structures, other treatment strategies like chemotherapy, radiotherapy, or targeted therapy are considered.
Q 5. Discuss the role of imaging (CT, MRI, PET) in planning tumor resection.
Imaging plays a vital role in planning tumor resection. Different modalities provide complementary information:
- CT scans: Provide detailed anatomical information, showing tumor size, location, and relationship to adjacent structures.
- MRI scans: Offer superior soft tissue contrast, helping delineate the tumor margins and identify infiltration into surrounding tissues.
- PET scans: Detect metabolically active tumors, identifying areas of increased glucose uptake, helping to distinguish tumor from normal tissue and detecting distant metastases.
These imaging studies are integrated with clinical findings and biopsy results to create a three-dimensional map of the tumor, allowing surgeons to plan the optimal surgical approach, anticipate potential challenges, and develop a detailed surgical plan. Advanced imaging techniques like 3D reconstructions can help surgeons simulate the resection process before the actual procedure.
Q 6. What are the common complications associated with tumor resection?
Tumor resection, while life-saving, carries potential complications:
- Bleeding: Intraoperative and postoperative bleeding can be significant, especially with large tumors or those in highly vascular areas.
- Infection: Surgical site infections are a potential risk, especially in immunocompromised patients.
- Damage to adjacent organs: Tumors often lie close to vital structures, and damage during resection is possible. This could result in nerve injury, organ dysfunction, or fistula formation.
- Postoperative pain: Significant pain is expected after major surgery, and appropriate pain management is crucial.
- Recurrence: Despite complete resection, tumor recurrence is a possibility, necessitating ongoing surveillance.
- Embolization: Release of tumor cells during surgery, potentially leading to spread.
The risk of complications varies depending on the tumor’s location, size, type, and the patient’s overall health. A thorough pre-operative assessment, meticulous surgical technique, and close postoperative monitoring are essential to minimize these risks.
Q 7. How do you manage intraoperative bleeding during tumor resection?
Managing intraoperative bleeding is crucial during tumor resection to ensure patient safety and optimal surgical outcome. The approach is multi-faceted:
- Careful dissection: Meticulous surgical technique, using precise instruments and careful identification of blood vessels, minimizes bleeding.
- Hemostasis techniques: Various techniques are employed to control bleeding, including electrocautery (using heat to seal blood vessels), clips, sutures, and sponges.
- Surgical sealant: Fibrin sealant or other hemostatic agents can be applied to control bleeding from small vessels.
- Blood transfusion: If significant bleeding occurs, blood transfusions may be necessary.
- Vascular surgery consultation: In cases of uncontrollable bleeding, a vascular surgeon might be consulted to repair damaged blood vessels.
Proactive strategies to minimize bleeding include pre-operative assessment of the patient’s coagulation profile and use of cell salvage techniques to recover and re-infuse the patient’s own blood.
Q 8. Explain the importance of multidisciplinary team approach in tumor resection.
A multidisciplinary team approach in tumor resection is paramount for optimal patient outcomes. It’s not just about the surgeon’s skill; it’s about a coordinated effort from various specialists who bring unique perspectives and expertise to the table. Think of it like a well-orchestrated symphony, where each instrument (specialist) plays a vital role in creating a harmonious and successful result.
- Oncologist: Determines the type and stage of cancer, guides treatment strategies, and monitors response to therapy.
- Radiologist: Provides crucial imaging guidance (CT, MRI, PET scans) for precise tumor localization and surgical planning.
- Pathologist: Analyzes tissue samples during and after surgery to confirm diagnosis, assess margins, and guide further treatment.
- Surgeon: Performs the resection, aiming for complete tumor removal with minimal damage to surrounding healthy tissue.
- Anesthesiologist: Ensures patient safety and comfort during the procedure.
- Nurse Navigator/Case Manager: Coordinates care, assists with appointments, and provides emotional support.
For example, in a complex pancreatic cancer resection, the oncologist might recommend neoadjuvant chemotherapy to shrink the tumor before surgery, making the resection technically easier and potentially improving survival rates. The radiologist uses advanced imaging techniques to delineate the tumor’s exact boundaries, enabling the surgeon to perform a precise operation while preserving vital structures. Post-surgery, the pathologist’s analysis guides the oncologist’s decisions on adjuvant therapies.
Q 9. Describe your experience with minimally invasive surgical techniques in tumor resection.
Minimally invasive surgical techniques, such as laparoscopy and robotic-assisted surgery, are increasingly preferred for tumor resection whenever feasible. These approaches offer several advantages over traditional open surgery, including smaller incisions, reduced pain, shorter hospital stays, and faster recovery times. Imagine the difference between a large, open wound versus several small puncture sites – the recovery is dramatically different.
My experience encompasses a wide range of minimally invasive procedures for various tumor types. For instance, I’ve successfully performed laparoscopic colectomy for colon cancer, laparoscopic nephrectomy for kidney tumors, and thoracoscopic resection for lung nodules. These techniques demand precision and specialized skills, often requiring the use of specialized instruments and 3D visualization systems.
The choice between minimally invasive and open surgery depends on several factors, including the tumor’s location, size, and accessibility, as well as the patient’s overall health. Not all tumors are amenable to minimally invasive approaches. In cases where a clean surgical margin cannot be achieved with minimally invasive surgery, an open approach may be necessary.
Q 10. How do you handle unexpected findings during a tumor resection?
Unexpected findings during tumor resection are not uncommon. Experienced surgeons always anticipate potential variations from preoperative imaging and planning. The key is to adapt swiftly and decisively, while maintaining patient safety. Think of it like navigating an unexpected detour during a journey; you need to find the best alternative route to reach your destination.
My approach involves a systematic process:
- Immediate Assessment: Carefully assess the unexpected finding – is it an extension of the tumor, an adjacent organ involvement, or an unforeseen vascular anomaly?
- Consult Team: Immediately consult with the multidisciplinary team (oncologist, pathologist, radiologist) to discuss the findings and develop a revised surgical strategy.
- Modify Approach: Adjust the surgical plan as needed – this might involve extending the resection, performing a more radical procedure, or perhaps even abandoning the planned approach if the findings suggest it’s no longer safe or feasible.
- Patient Communication: Keep the patient and their family informed of the changes in the surgical plan and the implications for treatment.
For instance, during a liver resection, if I find unexpected vascular involvement not seen on preoperative imaging, I might need to consult a vascular surgeon and modify my approach to ensure safe removal of the tumor while preserving vital blood vessels.
Q 11. What are the different types of surgical closure techniques used after tumor resection?
Surgical closure techniques after tumor resection depend on several factors, including the location of the surgery, the size of the incision, and the condition of the tissues. The goal is always to achieve secure hemostasis (stop bleeding), minimize tension on the wound, and promote optimal healing. Think of it like carefully putting together a complex puzzle, where each piece must fit perfectly to create a stable and aesthetically pleasing result.
- Layer Closure: This is the most common method, involving the closure of each tissue layer (fascia, muscle, subcutaneous tissue, skin) individually using absorbable or non-absorbable sutures. This provides strong, layered support and reduces the risk of wound complications.
- Staple Closure: Surgical staples are often used for skin closure, particularly for larger incisions, offering faster closure time compared to sutures. However, staples are more prone to infection and are thus usually not applied to deeper layers.
- Mesh Reinforcement: In cases of significant tissue loss or tension, surgical mesh can be used to reinforce the wound closure, improving wound stability and reducing the risk of hernia formation.
- Vacuum-Assisted Closure (VAC): A specialized technique used for large, complex wounds that often involve significant tissue damage. A negative pressure dressing helps to promote wound healing and reduce fluid accumulation.
The choice of closure technique is always individualized and is based on factors specific to the patient and the nature of the surgery. It’s a crucial aspect of the overall surgical procedure that significantly impacts the patient’s recovery and long-term outcome.
Q 12. Describe your experience with robotic-assisted surgery for tumor resection.
Robotic-assisted surgery has revolutionized tumor resection in many areas, providing significant advantages over traditional laparoscopy and open surgery. The enhanced dexterity, precision, and three-dimensional visualization offered by robotic systems enable surgeons to perform complex procedures with greater accuracy and reduced invasiveness. It’s like having an extra pair of highly skilled hands with superior vision.
My experience with robotic-assisted surgery includes procedures such as robotic prostatectomy, robotic nephrectomy, and robotic colorectal resection. The da Vinci Surgical System is the most commonly used robotic platform, allowing for intricate maneuvers within confined spaces. The smaller incisions lead to decreased pain, quicker recovery, and better cosmetic results.
However, robotic-assisted surgery is not a universal solution. Cost, surgeon training requirements, and the complexity of the robotic system itself limit its widespread adoption for all tumor types and surgical scenarios.
Q 13. How do you determine the appropriate adjuvant therapies (chemo, radiation) post-resection?
The decision regarding adjuvant therapies (chemotherapy and/or radiation) after tumor resection is a crucial one, often requiring multidisciplinary collaboration. The goal is to eliminate any remaining microscopic cancer cells and reduce the risk of recurrence. It’s a complex equation balancing potential benefits against potential side effects.
Several factors determine the appropriate adjuvant therapy:
- Tumor type and grade: Some cancers are more sensitive to chemotherapy or radiation than others.
- Stage of cancer: Higher-stage cancers typically necessitate more aggressive adjuvant therapies.
- Surgical margins: Positive margins (cancer cells at the edge of the resected tissue) often indicate a higher risk of recurrence and necessitate adjuvant treatment.
- Patient’s overall health: The patient’s ability to tolerate the side effects of chemotherapy or radiation plays a significant role.
- Molecular markers: The presence of certain molecular markers in the tumor can influence the choice of adjuvant therapy.
For example, a patient with stage II colon cancer and clear surgical margins may not require adjuvant chemotherapy, whereas a patient with stage III colon cancer and positive margins would likely benefit from adjuvant chemotherapy or chemoradiotherapy. The decision is always individualized and based on a thorough evaluation of all these factors.
Q 14. What are the key performance indicators (KPIs) you use to measure success in tumor resection?
Measuring success in tumor resection goes beyond simply removing the tumor. It encompasses a holistic approach encompassing patient safety, efficacy, and long-term outcomes. It’s not just about winning the battle; it’s about winning the war against cancer.
Key performance indicators (KPIs) I use include:
- Complete Resection Rate: Percentage of patients undergoing complete tumor removal with clear margins.
- Positive Margin Rate: Percentage of patients with cancer cells at the edge of the resected tissue (indicates need for further treatment).
- Surgical Morbidity and Mortality Rates: Rates of complications and deaths following surgery.
- Length of Hospital Stay: Shorter stays indicate efficient and effective surgery.
- Recurrence Rate: Percentage of patients experiencing tumor recurrence after surgery.
- Disease-Free Survival Rate: Percentage of patients alive without evidence of disease at specific time points post-surgery.
- Overall Survival Rate: Percentage of patients alive after surgery, considering all causes of death.
- Patient Satisfaction Scores: Assessing patients’ experiences with their surgical care, pain management, and recovery.
Regular monitoring and analysis of these KPIs help to continuously improve surgical techniques, optimize treatment strategies, and ultimately enhance patient outcomes.
Q 15. Discuss your experience with different types of surgical instruments and technologies.
My experience encompasses a wide range of surgical instruments and technologies used in tumor resection. This includes both traditional techniques and advanced minimally invasive approaches. For example, I’m proficient with various types of scalpels, forceps, retractors, and dissecting instruments, selecting the most appropriate tools based on the tumor’s location, size, and characteristics. In minimally invasive surgery, I have extensive experience with laparoscopic instruments, robotic surgical systems (like the da Vinci system), and specialized endoscopic tools. The choice of technology depends on factors like the patient’s overall health, the tumor’s accessibility, and the need for precision. For instance, robotic surgery offers enhanced dexterity and visualization, particularly beneficial in complex cases involving delicate structures near vital organs. Furthermore, I’m familiar with advanced imaging technologies like intraoperative ultrasound and fluorescence imaging, which assist in real-time tumor identification and boundary delineation, allowing for more complete resection while minimizing damage to healthy tissue.
- Traditional Instruments: Scalpels, dissecting scissors, forceps, retractors, suction devices.
- Minimally Invasive Instruments: Laparoscopic instruments, robotic surgical systems, specialized endoscopes.
- Imaging Technologies: Intraoperative ultrasound, fluorescence imaging, navigation systems.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage a patient with a large or complex tumor requiring extensive resection?
Managing a patient with a large or complex tumor requiring extensive resection necessitates a meticulous, multi-disciplinary approach. It begins with a thorough preoperative evaluation, including advanced imaging (CT, MRI, PET scans) to precisely define the tumor’s extent and relationship to surrounding vital structures. This allows us to plan the surgical strategy carefully. Often, a staged resection might be necessary, breaking the procedure into smaller, manageable steps to reduce risk and improve patient recovery. This could involve initial debulking surgery to reduce tumor size, followed by a more radical resection at a later stage. We collaborate closely with oncologists, radiotherapists, and other specialists to determine the optimal approach, often incorporating neoadjuvant (pre-surgical) chemotherapy or radiation to shrink the tumor and improve resectability. During surgery, advanced techniques like nerve monitoring and intraoperative imaging are crucial to ensure precise resection while preserving healthy tissue and function. Post-operatively, close monitoring and a tailored rehabilitation program are essential.
For instance, a patient with a large pancreatic tumor might require a Whipple procedure (pancreaticoduodenectomy), a complex operation involving resection of parts of the pancreas, duodenum, gallbladder, and sometimes the stomach. Careful planning and execution, including meticulous vascular control, are crucial for successful outcomes. Post-operative care typically includes intensive monitoring for complications such as pancreatic fistula or infection.
Q 17. Explain your approach to patient counseling and communication regarding the risks and benefits of tumor resection.
Patient counseling is a cornerstone of my practice. I believe in clear, empathetic communication. Before the procedure, I explain the diagnosis, treatment options (including potential non-surgical options), and the rationale behind recommending tumor resection. I discuss the potential benefits, including improved survival rates, reduced tumor burden, and symptom relief, as well as the potential risks, such as bleeding, infection, nerve damage, and the possibility of incomplete resection. I present realistic expectations and answer all questions thoroughly. I use visual aids such as diagrams and imaging scans to illustrate the procedure and its potential consequences. I actively encourage patients and their families to express concerns and to participate in shared decision-making. I ensure that patients understand the importance of following post-operative instructions carefully and schedule follow-up appointments to monitor progress and address any concerns.
For example, when explaining the risks of a lung resection to a patient, I would emphasize the possibility of pneumothorax (collapsed lung), respiratory complications, and potential impact on lung function, providing clear examples of how these complications can be managed.
Q 18. How do you ensure patient safety during and after tumor resection?
Ensuring patient safety is paramount. This starts with rigorous preoperative preparation, including a comprehensive medical history review, appropriate blood work, and risk assessment. During surgery, meticulous technique, strict adherence to sterile protocols, and continuous monitoring of vital signs are essential. We use advanced technologies like nerve monitoring and intraoperative imaging to guide the resection and minimize damage to healthy tissue. A skilled surgical team, including experienced nurses and anesthesiologists, plays a crucial role in maintaining patient safety. After surgery, close monitoring of the patient’s vital signs, wound healing, and potential complications is vital. Pain management, early mobilization, and respiratory support, as needed, are implemented to facilitate a safe recovery.
For example, during a brain tumor resection, meticulous microsurgical technique, constant monitoring of neurological function (using evoked potentials), and the use of neuromonitoring equipment are all vital to minimize surgical risk.
Q 19. Describe your experience with managing post-operative pain and complications.
Managing post-operative pain and complications is a crucial aspect of patient care. We employ a multimodal approach to pain management, including both pharmacological (analgesics, epidurals) and non-pharmacological methods (physical therapy, ice packs). Early mobilization and respiratory exercises are encouraged to prevent complications like pneumonia and deep vein thrombosis. Regular monitoring of vital signs, wound healing, and potential complications, such as infection or bleeding, are crucial. I work closely with a team of specialists, including pain management specialists and physical therapists, to provide tailored support to each patient. We actively monitor patients for signs of infection, such as fever, elevated white blood cell count, or localized inflammation. Prompt treatment with antibiotics is initiated when necessary. Regular follow-up appointments are scheduled to assess recovery progress and address any arising concerns.
For example, after a major abdominal resection, we might utilize a patient-controlled analgesia (PCA) pump for pain management and implement prophylactic measures to prevent deep vein thrombosis, such as compression stockings and anticoagulants.
Q 20. How do you handle a surgical complication during tumor resection?
Handling surgical complications requires immediate action and a calm, decisive approach. The first step involves identifying the complication, assessing its severity, and taking immediate steps to stabilize the patient’s condition. This often includes managing bleeding, correcting electrolyte imbalances, and addressing any life-threatening issues. Depending on the nature of the complication, the surgical approach might need to be modified, additional procedures might be necessary, or the surgery might even need to be abandoned. Open communication with the patient and family is crucial, explaining the complication, the actions being taken, and the potential implications. I always ensure that documentation of the complication and the response is thorough and accurate. After the immediate crisis is resolved, a thorough analysis of the complication is conducted to identify contributing factors and to prevent similar occurrences in the future. This often involves reviewing the surgical technique, equipment, and intraoperative monitoring data.
For instance, if unexpected massive bleeding occurs during a liver resection, immediate steps are taken to control the bleeding, including surgical clamping of vessels, packing the bleeding area, or conversion to an open procedure if necessary. Post-operative care would include close monitoring for blood loss and transfusion, if needed.
Q 21. What are your strategies for preventing surgical site infections after tumor resection?
Preventing surgical site infections (SSIs) is a high priority. We adhere to strict sterile techniques throughout the entire surgical process, including meticulous skin preparation, use of sterile drapes and instruments, and maintenance of a sterile surgical field. Prophylactic antibiotics are administered according to established guidelines, usually before the incision is made. Maintaining normothermia (normal body temperature) during surgery is important, as hypothermia can increase the risk of infection. Wound closure techniques are carefully selected to minimize dead space and promote efficient healing. Post-operatively, we monitor patients for any signs of infection and promptly administer antibiotics if necessary. Patient education about wound care and hygiene is essential, along with appropriate follow-up care. Additionally, maintaining a clean and safe surgical environment is crucial, and regular monitoring of infection rates and adherence to protocols is part of continuous quality improvement efforts.
For example, in cases of high-risk patients (e.g., those with diabetes), additional measures might be employed, such as the use of specialized wound dressings or negative-pressure wound therapy to optimize wound healing and prevent SSIs.
Q 22. How do you assess the effectiveness of the resection based on pathology reports?
Assessing the effectiveness of tumor resection relies heavily on the pathology report, which provides crucial information about the extent of the surgical removal. We look for several key indicators:
- Resection Margins: This is the most critical aspect. The pathologist examines the tissue surrounding the tumor to determine if any cancerous cells remain. A ‘negative’ or ‘clear’ margin indicates that no cancer cells were found at the edge of the resected tissue. A ‘positive’ margin means cancer cells were present at the resection edge, requiring further treatment. The distance of the margin (e.g., 1mm, 5mm) is also significant, with larger margins generally indicating a more complete resection.
- Tumor Grade and Stage: The report will confirm the tumor’s grade (how aggressive it is) and stage (how far it has spread). This helps us understand the initial disease extent and the likelihood of recurrence.
- Lymphovascular Invasion (LVI): The report details whether cancer cells have invaded the lymphatic vessels or blood vessels, providing insight into the risk of metastasis (spread to other parts of the body).
- Perineural Invasion (PNI): This indicates cancer cell invasion into nerves, which can influence prognosis and treatment decisions.
For example, a pathology report showing negative margins, a well-differentiated tumor (low grade), and absence of LVI suggests a successful resection with a better prognosis. Conversely, positive margins necessitate further surgery or adjuvant therapies like radiation or chemotherapy.
Q 23. Discuss your experience with different types of tissue reconstruction techniques after tumor resection.
Tissue reconstruction after tumor resection is crucial for restoring function and improving cosmetic outcomes. The technique chosen depends entirely on the location and extent of the resection, as well as the patient’s overall health. I have experience with a range of techniques, including:
- Local Flaps: These involve repositioning adjacent tissue to fill the defect. This is often used for smaller defects and offers good functional and cosmetic results. For example, a local flap can be used to reconstruct a defect after a resection of a skin cancer on the face.
- Free Flaps: These involve moving tissue from a distant site, often with its own blood supply, to the defect site. This is necessary for larger defects or those where local tissue is insufficient. For example, a free fibula flap might be used in jaw reconstruction after a tumor resection.
- Prostheses: Artificial implants, such as those used in breast reconstruction after mastectomy, can provide functional and cosmetic restoration.
- Synthetic Materials: Various synthetic materials may be used to fill defects, particularly in situations where tissue transplantation is not feasible.
Selecting the appropriate technique requires meticulous pre-operative planning, considering factors such as blood supply, tissue availability, and functional requirements. The goal is always to achieve the best possible functional and aesthetic outcomes while minimizing complications.
Q 24. What is your approach to managing a patient with a recurrent tumor after resection?
Managing recurrent tumor after resection is a complex process requiring a multidisciplinary approach. The first step is confirming the recurrence through imaging (CT, MRI, PET) and biopsy. Treatment strategies depend on several factors:
- Location and Extent of Recurrence: A localized recurrence might be amenable to surgical resection, while widespread recurrence may require systemic therapy.
- Patient’s Overall Health and Prior Treatments: The patient’s general health status and previous treatments significantly influence treatment options.
- Tumor Type and Histology: The specific type of tumor and its characteristics will determine the best therapeutic approach.
Treatment options may include:
- Surgery: If feasible, surgical resection of the recurrent tumor is often the preferred approach, with the aim of achieving negative margins.
- Radiation Therapy: This is often used in conjunction with surgery or as a primary treatment modality for recurrent tumors that are not surgically resectable.
- Chemotherapy: Systemic chemotherapy can be employed to target the cancer cells throughout the body, especially in cases of metastatic disease.
- Targeted Therapy: Newer therapies targeting specific molecular pathways within the cancer cells can be effective in certain types of tumors.
Regular follow-up is crucial to monitor for recurrence and manage any side effects of treatment.
Q 25. How do you stay current with the latest advancements in tumor resection techniques?
Staying current with advancements in tumor resection is essential for providing the best possible patient care. My approach includes:
- Active Participation in Professional Organizations: Membership in organizations such as the American College of Surgeons and relevant specialty societies provides access to continuing medical education, conferences, and journals.
- Regular Review of Peer-Reviewed Literature: I dedicate time to reading leading surgical journals and reviewing relevant research articles to remain informed about new techniques and technologies.
- Attendance at Conferences and Workshops: Attending surgical conferences and workshops allows for direct interaction with leading experts and exposure to the latest innovations.
- Collaboration with Colleagues: Sharing knowledge and experience with colleagues through discussions and case reviews helps to broaden my perspective and stay abreast of current best practices.
- Participation in Research: Active involvement in research projects related to tumor resection keeps me engaged in the latest advancements and provides opportunities for personal growth.
Q 26. What are your strengths and weaknesses as a surgeon performing tumor resections?
Strengths: I pride myself on my meticulous surgical technique, detailed pre-operative planning, and effective communication with patients and their families. My experience with complex cases and diverse reconstruction techniques allows me to address a wide range of challenges. I am also adept at multidisciplinary collaboration, working effectively with oncologists, radiologists, and pathologists to achieve optimal outcomes.
Weaknesses: Like any surgeon, I am constantly striving for improvement. One area I am actively working on is enhancing my proficiency with minimally invasive surgical techniques. While I have experience, further refinement in this area would enhance patient recovery and reduce invasiveness.
Q 27. Describe a challenging case involving tumor resection and how you overcame the challenges.
One particularly challenging case involved a large, invasive pancreatic tumor located close to major blood vessels and the bile duct. The tumor’s proximity to critical structures presented a significant risk of major complications during resection. The challenge was to achieve complete tumor removal while minimizing damage to adjacent structures and preserving vital functions.
To overcome this challenge, we employed a multidisciplinary approach. Pre-operative imaging, including detailed CT scans and angiography, was crucial for accurate surgical planning. During surgery, we utilized advanced surgical techniques, including intraoperative ultrasound, to precisely locate and delineate the tumor’s boundaries. The use of specialized surgical instruments and meticulous dissection allowed for safe and complete tumor resection with minimal damage to surrounding tissues.
Post-operatively, the patient required intensive care due to the complexity of the procedure. However, through careful monitoring and management, he recovered well and is now cancer-free. This case highlighted the importance of thorough pre-operative planning, precise surgical technique, and a robust post-operative care strategy in managing complex tumor resections.
Key Topics to Learn for Tumor Resection Interview
- Oncological Principles: Understanding tumor biology, staging, and grading systems; differentiating benign and malignant tumors.
- Surgical Techniques: Mastery of various resection techniques (e.g., en bloc resection, extended resection, minimally invasive approaches); familiarity with different surgical instruments and technologies.
- Pre-operative Planning: Importance of detailed imaging analysis (CT, MRI, PET); collaborative discussions with multidisciplinary teams (oncologists, radiologists, pathologists); patient selection criteria and risk assessment.
- Intraoperative Considerations: Real-time assessment of tumor margins; handling of critical structures (major vessels, nerves); strategies for managing intraoperative complications.
- Post-operative Management: Wound care; pain management; monitoring for complications (e.g., infection, bleeding, recurrence); adjuvant therapies (chemotherapy, radiation).
- Advanced Techniques: Experience with robotic surgery, image-guided surgery, or other advanced technologies relevant to tumor resection.
- Ethical Considerations: Informed consent; discussion of treatment options and prognosis with patients and families; managing difficult cases and challenging ethical dilemmas.
- Research and Innovation: Familiarity with current research trends and advancements in tumor resection techniques and technologies.
Next Steps
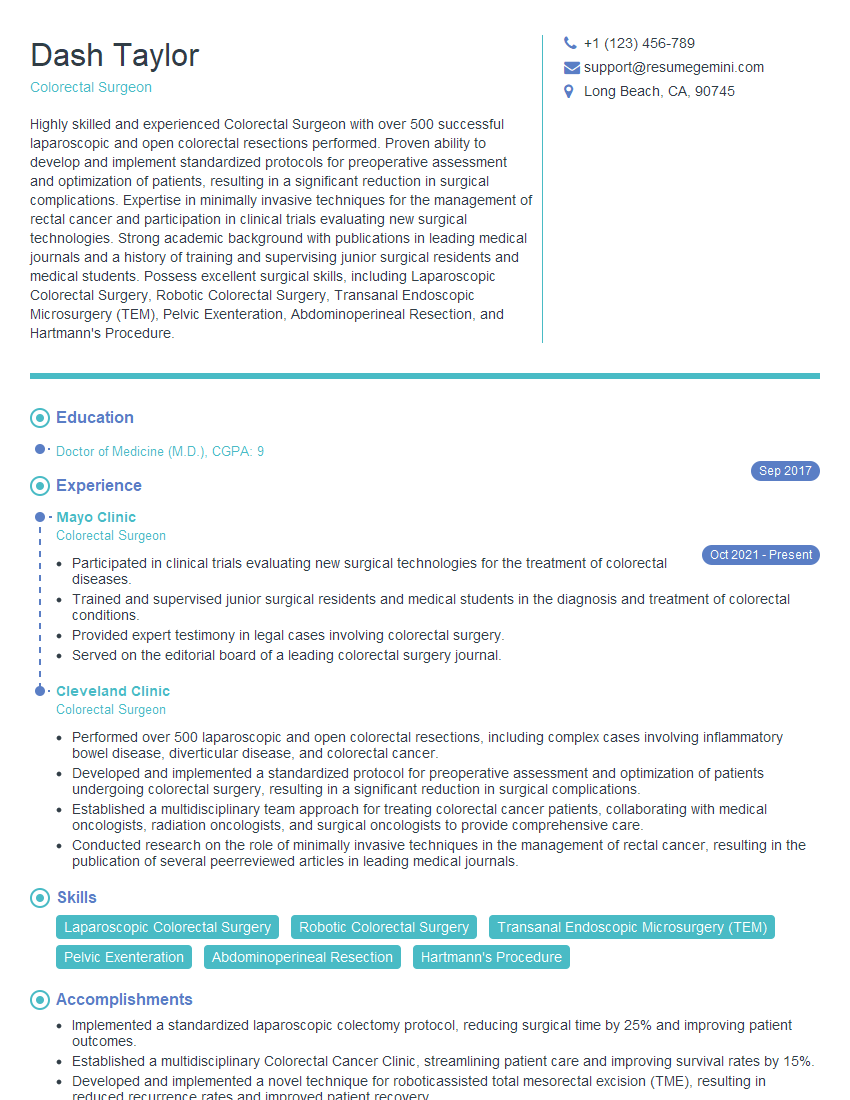
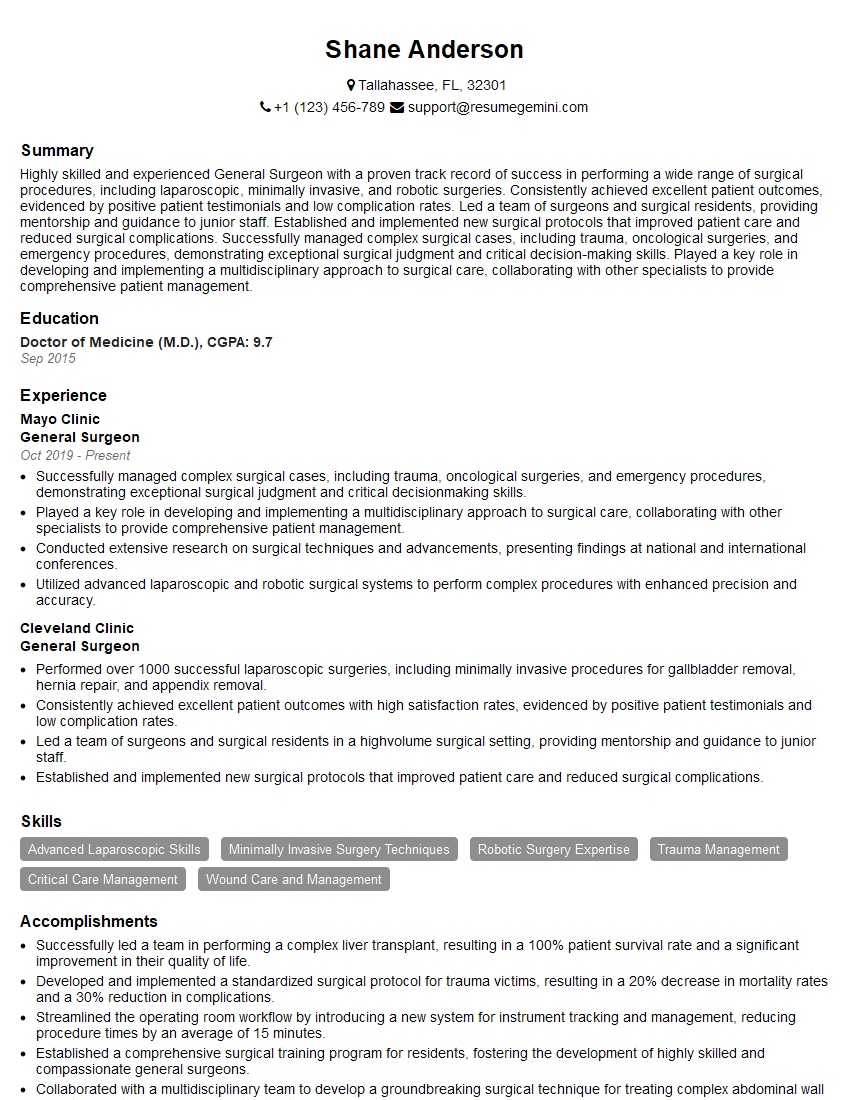
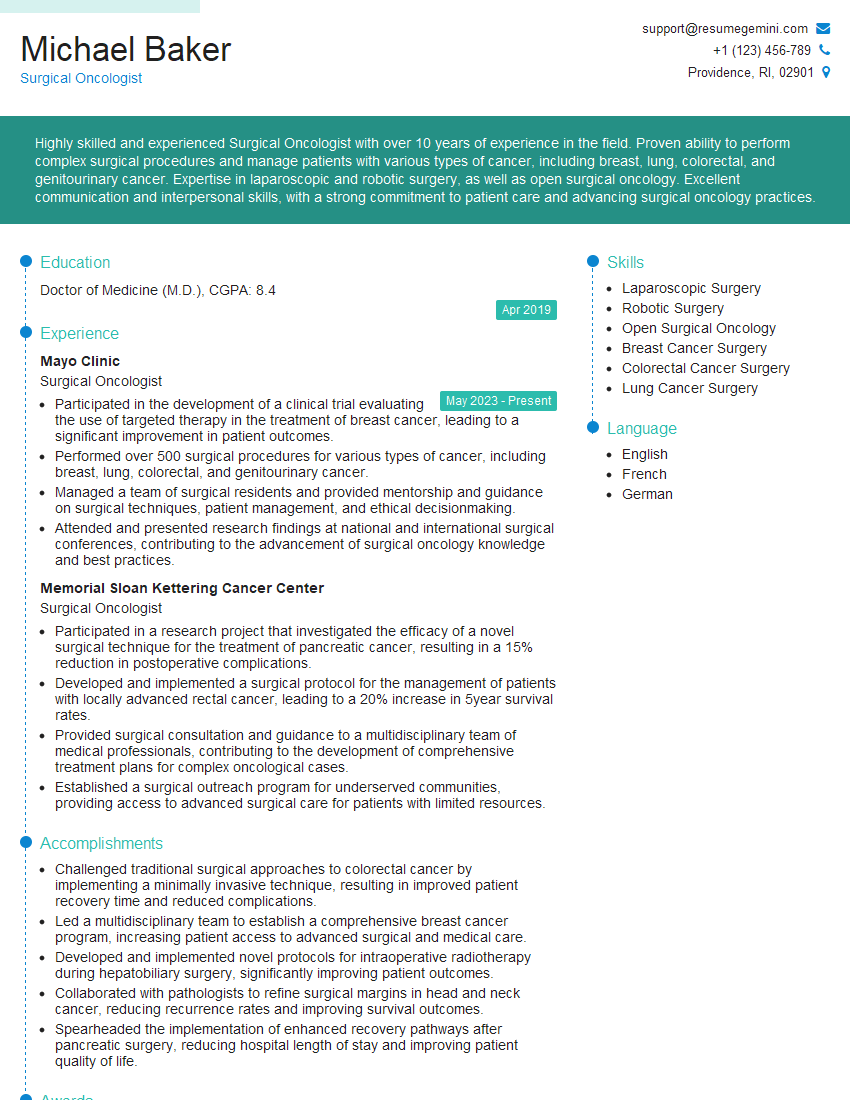
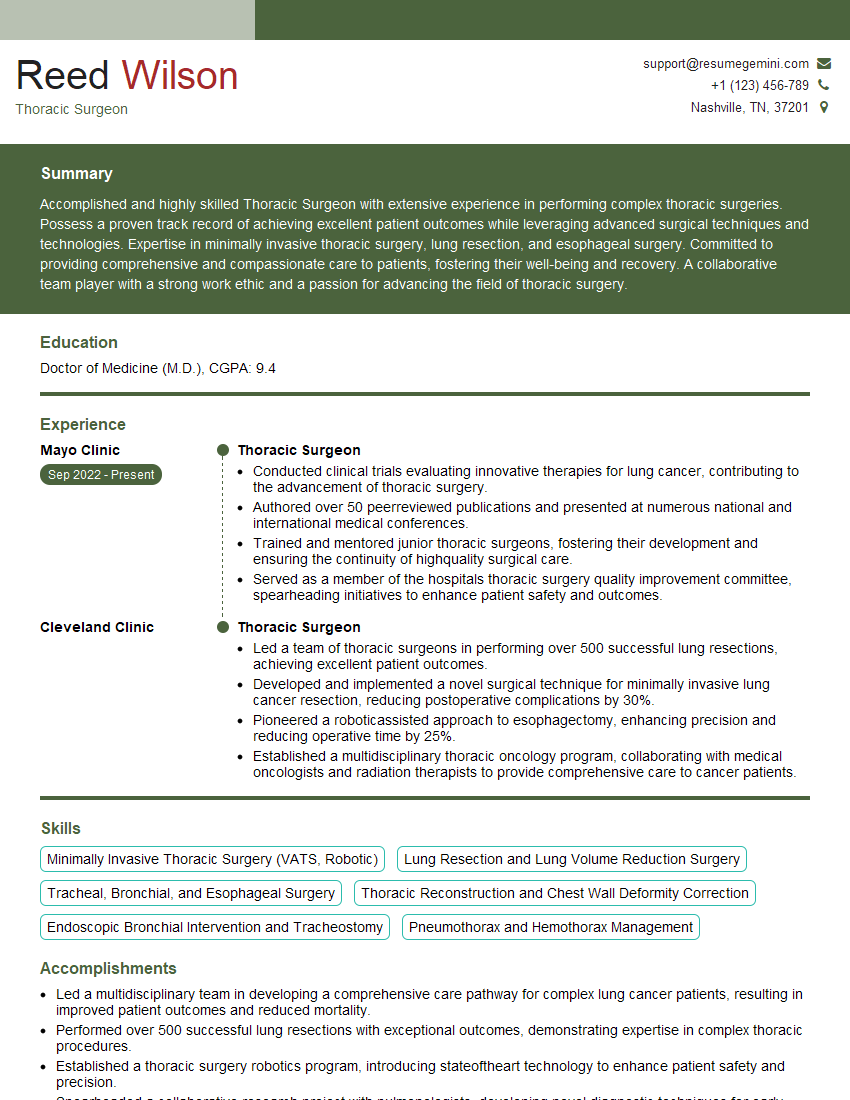
Mastering tumor resection techniques is crucial for advancing your career in surgical oncology. It demonstrates a high level of skill and expertise, opening doors to leadership roles and specialized opportunities. To maximize your job prospects, it’s essential to create a compelling, ATS-friendly resume that highlights your skills and experience effectively. We highly recommend using ResumeGemini to build a professional resume tailored to your specific field. ResumeGemini provides tools and resources to craft a standout resume, and examples of resumes specifically designed for candidates in Tumor Resection are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.