Cracking a skill-specific interview, like one for Tympanometry, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Tympanometry Interview
Q 1. Explain the principle behind tympanometry.
Tympanometry is a quick, painless test that measures the eardrum’s (tympanic membrane) mobility and the middle ear’s pressure. Imagine the middle ear as a small, air-filled room. The tympanometer introduces varying amounts of air pressure into the ear canal, while simultaneously measuring the eardrum’s movement. This movement reflects the middle ear’s pressure and the eardrum’s flexibility. A healthy middle ear will show a characteristic movement in response to these pressure changes, providing information about the integrity of the middle ear system.
Q 2. Describe the different types of tympanograms (Type A, B, C).
Tympanograms are categorized into different types based on the shape of the resulting graph. Each type suggests a different middle ear status:
- Type A: This is the normal tympanogram. It shows a peak at or near atmospheric pressure, indicating a healthy middle ear with normal eardrum mobility. Think of this as a perfectly inflated balloon responding normally to pressure changes.
- Type B: This tympanogram shows a flat line, meaning there’s no significant movement of the eardrum. This suggests fluid or blockage in the middle ear, making the eardrum immobile. Imagine a balloon that is completely filled with water – it cannot move.
- Type C: This tympanogram shows a peak at a negative pressure. This signifies negative pressure in the middle ear, often due to Eustachian tube dysfunction. Think of a slightly deflated balloon that is harder to expand. The peak will still be visible but occurs at a lower pressure than normal.
Q 3. What are the normal values for tympanometric measurements?
Normal tympanometric values vary slightly depending on the equipment used, but generally include:
- Peak Pressure: Between -100 and +100 daPa (decaPascals), ideally near 0 daPa (atmospheric pressure).
- Peak Compliance (or admittance): This is a measure of eardrum mobility and varies with age and equipment. Typically, a value within normal limits for the individual’s age will be considered normal.
- Eardrum stiffness: Reflected indirectly in the shape and width of the peak. A narrow peak can indicate stiffness, while a wide peak suggests less stiffness.
It’s crucial to always refer to the specific normative data provided by the manufacturer of the tympanometer used.
Q 4. How do you interpret a Type B tympanogram?
A Type B tympanogram, characterized by a flat line, almost always indicates a problem with the middle ear. The lack of peak suggests that the eardrum is not moving in response to pressure changes. This lack of mobility strongly suggests the presence of:
- Middle ear effusion (fluid): Fluid in the middle ear space prevents the eardrum from moving freely.
- Otosclerosis (hardening of the ossicles): Although less common in causing a completely flat tympanogram, it can severely restrict eardrum movement.
- Tympanic membrane perforation: A hole in the eardrum will prevent the pressure changes from impacting the eardrum’s movement.
- Cholesteatoma: A growth in the middle ear which can fill the space and limit mobility.
Further investigations such as otoscopy (visual examination of the eardrum) are necessary to determine the exact cause.
Q 5. What are the potential causes of a Type C tympanogram?
A Type C tympanogram, with its peak at negative pressure, primarily suggests Eustachian tube dysfunction. The Eustachian tube connects the middle ear to the nasopharynx (back of the nose and throat) and is responsible for equalizing pressure across the eardrum. When the Eustachian tube is blocked or not functioning properly, negative pressure builds up in the middle ear, causing the eardrum to retract inwards.
Potential causes of a Type C tympanogram include:
- Upper respiratory infections (URIs): Swelling and inflammation from colds or allergies can obstruct the Eustachian tube.
- Allergies: Similar to URIs, allergic reactions can cause inflammation.
- Barotrauma (pressure changes): Sudden pressure changes (like during air travel or scuba diving) can cause temporary dysfunction.
- Structural abnormalities: Rarely, anatomical abnormalities might affect the Eustachian tube’s function.
Q 6. How do you interpret a Type A tympanogram with a shallow peak?
A Type A tympanogram with a shallow peak indicates reduced mobility of the eardrum, even though the pressure is normal. This suggests that the middle ear system may be stiff, restricting normal eardrum movement. This can be due to several factors, including:
- Otosclerosis: Abnormal bone growth in the middle ear restricts movement of the ossicles (tiny bones that transmit sound).
- Tympanosclerosis: Scarring of the eardrum due to prior ear infections makes the eardrum less flexible.
- Middle ear inflammation: Even without fluid, inflammation can stiffen the middle ear structures.
Further testing and evaluation may be needed to pinpoint the precise cause and guide treatment.
Q 7. What is the significance of measuring static admittance in tympanometry?
Static admittance, often presented as a component of the tympanogram reading, is a measure of the eardrum’s compliance (flexibility) at the peak pressure. It reflects how easily the eardrum vibrates in response to sound. A reduced static admittance, despite a normal peak pressure (Type A), implies stiffness or restricted movement. Conversely, increased static admittance might suggest flaccidity or excessive mobility of the eardrum.
Measuring static admittance helps differentiate between various middle ear conditions, offering a more comprehensive understanding beyond just peak pressure and identifying subtle abnormalities that may otherwise be missed. For example, distinguishing between a healthy Type A tympanogram and a Type A tympanogram with stiffness related to otosclerosis.
Q 8. Explain the procedure for performing tympanometry on an adult patient.
Tympanometry in adults is a straightforward procedure. First, the patient’s ear canal is inspected using an otoscope to ensure there’s no visible obstruction like cerumen (earwax) or foreign bodies. Then, a soft, disposable ear tip is attached to the tympanometer probe. The probe is gently inserted into the external ear canal, ensuring a good seal is achieved. The tympanometer automatically introduces a series of air pressure changes into the ear canal while simultaneously measuring the compliance (movement) of the eardrum. The results are displayed graphically as a tympanogram. This typically takes only a few minutes and is generally painless. It’s crucial to explain the procedure to the patient beforehand, addressing any anxieties they might have. For instance, I often tell patients it feels like a brief puff of air in the ear. The entire process is usually well-tolerated by adults who understand its purpose.
Q 9. Explain the procedure for performing tympanometry on a pediatric patient.
Tympanometry on pediatric patients requires a slightly different approach due to their age and potential lack of cooperation. A thorough explanation to the parent or guardian is essential, emphasizing the quick and painless nature of the test. Depending on the child’s age and developmental stage, different techniques might be needed. For infants, it might be necessary to perform the test while they are sleeping or being held securely by a parent. For toddlers and preschoolers, distraction techniques like playing games or singing songs can be helpful. The same otoscopic examination is crucial, and a smaller, age-appropriate ear tip must be selected. The test’s duration should be kept as short as possible. Positive reinforcement and praise after the procedure can significantly impact the child’s overall experience and future cooperation. I often use stickers or small toys as rewards.
Q 10. How do you handle a patient who is unable to cooperate during tympanometry?
Managing uncooperative patients during tympanometry requires patience and creativity. The approach will depend on the patient’s age and the reason for their lack of cooperation. For children, using distraction methods such as toys, videos, or games is a common strategy. For adults, a calm and reassuring approach is key. Explaining the procedure clearly and answering their questions can alleviate anxiety. If the patient remains uncooperative despite these efforts, postponing the test and rescheduling it at a time when they are more relaxed or with the assistance of a parent or caregiver might be necessary. In some cases, sedation may be considered, but this should be a last resort and requires a medical professional’s judgment. Documenting the reason for the uncooperative behaviour and any attempts made to facilitate the test is crucial for record-keeping.
Q 11. What are the limitations of tympanometry?
While tympanometry is a valuable diagnostic tool, it does have limitations. Firstly, it cannot differentiate between certain middle ear pathologies. For example, it may show a similar tympanogram pattern for otosclerosis (a bone disorder affecting the middle ear) and ossicular discontinuity (disruption of the tiny bones in the middle ear). Secondly, the presence of cerumen or other obstructions in the ear canal can significantly affect the accuracy of the results. Thirdly, tympanometry solely assesses the middle ear; it doesn’t provide information about the inner ear or the auditory nerve. Lastly, patient cooperation is critical; a poor seal can lead to inaccurate results. Therefore, tympanometry should be interpreted in conjunction with other audiological tests for a comprehensive assessment.
Q 12. How does tympanometry differ from other middle ear assessment techniques?
Tympanometry differs from other middle ear assessment techniques in its objective measurement of middle ear pressure and eardrum mobility. Unlike otoscopy (visual inspection), tympanometry provides quantitative data. Compared to acoustic reflex testing (measuring muscle responses in the middle ear), tympanometry gives a broader picture of middle ear status. It is also distinct from pure-tone audiometry which evaluates hearing sensitivity but doesn’t assess middle ear function. Tympanometry is a non-invasive, objective test providing information about middle ear pressure and compliance, unlike subjective tests such as behavioral audiometry which relies on patient responses.
Q 13. What are the potential artifacts that can affect tympanometry results?
Several artifacts can affect tympanometry results. A poor probe-ear seal is a common one, leading to inaccurate pressure and compliance measurements. Excessive cerumen or other foreign bodies in the ear canal can also obstruct sound waves and produce erroneous readings. Patient movement during the test can cause fluctuations in the data. Finally, equipment malfunction or improper calibration of the tympanometer can also lead to unreliable results. Recognizing these potential artifacts and implementing appropriate measures like ensuring a proper seal and patient stillness are crucial for obtaining accurate and reliable tympanometry findings.
Q 14. How do you troubleshoot common problems encountered during tympanometry?
Troubleshooting tympanometry problems involves a systematic approach. If you obtain a flat tympanogram, first ensure a proper seal is achieved. If the problem persists, check the equipment calibration. If you get a type B tympanogram (suggestive of fluid in the middle ear), verify the presence of any obstructions in the ear canal. If you experience issues with the instrument’s functionality, consult the manufacturer’s manual or seek technical support. Always document the troubleshooting steps taken and the final results to ensure accurate record-keeping and to aid in interpretation. Remember, patience and attention to detail are key in troubleshooting tympanometry issues.
Q 15. What are the indications for performing tympanometry?
Tympanometry is an objective test that assesses the middle ear’s function. It’s indicated whenever we suspect a problem with the middle ear space, hearing loss, or eustachian tube dysfunction. Think of it like checking the pressure and movement within a tiny, important drum in your ear. We use it to diagnose a wide range of conditions.
- Hearing loss: To determine if the hearing loss is conductive (middle ear problem) or sensorineural (inner ear or nerve problem).
- Middle ear effusion: To detect fluid buildup behind the eardrum, common in ear infections (otitis media).
- Eustachian tube dysfunction: To evaluate the function of the tube connecting the middle ear to the back of the throat, crucial for pressure equalization.
- Pre-surgical evaluation: To assess middle ear status before surgery (e.g., stapedectomy).
- Monitoring disease progression: To track changes in middle ear conditions over time, particularly in children with recurrent ear infections.
Essentially, any time we want to know what’s going on *inside* the middle ear, tympanometry is a valuable tool.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you document tympanometry findings?
Tympanometry results are documented using a standardized format, typically including:
- Type curve: This is represented by a letter (A, B, C, As, Ad) corresponding to the shape of the graph generated during the test, reflecting the pressure and compliance of the middle ear system. Each letter indicates a different middle ear status.
- Peak pressure (in daPa): The pressure at which the middle ear shows maximum compliance (movement). This indicates how well the eustachian tube is functioning.
- Static compliance (ml): A measure of the mobility of the eardrum and ossicles. Low compliance suggests stiffness in the system, while high compliance might indicate a flaccid eardrum.
- Ear canal volume (ml): This measures the size of the ear canal and helps differentiate between middle ear problems and issues within the ear canal itself. A high volume might suggest a perforation.
- Patient demographics and test date: This ensures the results are properly identified and easily retrievable.
A simple example might be documented as: Type A, Peak pressure: +50 daPa, Static compliance: 1.5 ml, Ear canal volume: 1.0 ml.
Q 17. How do you correlate tympanometry results with other audiological findings?
Tympanometry results are crucial in interpreting audiometric findings (pure-tone audiometry and speech audiometry). They help distinguish the *type* of hearing loss present. For example:
- Conductive hearing loss: If pure-tone audiometry shows a conductive hearing loss (bone conduction is normal, air conduction is impaired), tympanometry might reveal a type B curve (indicating middle ear fluid), a type C curve (negative middle ear pressure), or an abnormally low static compliance.
- Sensorineural hearing loss: If audiometry indicates a sensorineural hearing loss (both air and bone conduction are impaired), the tympanogram would typically be normal (type A). This helps confirm that the problem lies in the inner ear or auditory nerve, not the middle ear.
- Mixed hearing loss: A combination of conductive and sensorineural components will show a conductive component on audiometry and an abnormal tympanogram reflecting the middle ear problem.
In essence, tympanometry adds objective data to subjective audiometry results, offering a more complete picture of the hearing mechanism.
Q 18. What are the different probes used in tympanometry?
Different probes are used depending on the manufacturer and the age of the patient. The core components remain consistent, but design variations exist:
- 226 Hz probe: The most common probe tone frequency. It strikes a balance between sensitivity and practicality.
- Infant probes: These are smaller and more appropriately sized for use in young children.
- Probes with integrated microphone: Some probes incorporate a microphone to measure acoustic reflexes in addition to standard tympanometry.
The key element is a loudspeaker for emitting sound, a microphone for detecting sound reflections, and a system for delivering controlled air pressure changes into the ear canal. The design is optimized to provide a comfortable and effective testing experience.
Q 19. Explain the importance of ear canal volume measurement in tympanometry.
Ear canal volume measurement is crucial for several reasons. It’s like taking a peek at the shape and size of the space leading to the eardrum.
- Differentiating middle ear pathology from ear canal pathology: A normal ear canal volume is essential for interpreting the tympanogram accurately. An abnormally large volume suggests a perforation or a patent pressure equalization (PE) tube in the eardrum. An abnormally small volume could indicate impacted cerumen (earwax) obstructing the ear canal.
- Evaluating the presence of perforation: A high ear canal volume with a type B curve strongly suggests a perforation in the eardrum because air is freely flowing into the middle ear space.
- Ensuring test accuracy: If the ear canal volume is outside the normal range, it invalidates the tympanometry results. In this case, the ear canal must be cleaned of any debris before repeating the test.
In essence, accurate ear canal volume measurement is fundamental to getting reliable and interpretable tympanometry results.
Q 20. How do you interpret tympanometry results in the presence of otitis media?
In otitis media (middle ear infection), the most common tympanometry finding is a type B tympanogram. This means the middle ear space is filled with fluid, preventing the eardrum from moving normally in response to pressure changes. The graph shows a flat line with no peak compliance.
However, it’s important to note that a type B curve is not always diagnostic of otitis media; it can be caused by other factors (e.g., impacted cerumen, perforation). Therefore, correlation with clinical examination, otoscopy, and other audiological tests is essential.
Occasionally, you might see a type C tympanogram (negative pressure) in the early stages of otitis media or during resolution, as the eustachian tube attempts to clear the fluid.
Q 21. How do you interpret tympanometry results in the presence of otosclerosis?
Otosclerosis, a bony overgrowth in the middle ear, often leads to a reduced mobility of the ossicles (tiny bones in the middle ear). This typically results in a type As tympanogram. This signifies that the middle ear compliance is reduced compared to normal, indicating stiffness in the system. The peak pressure is usually normal, distinguishing it from other conditions.
Sometimes, you may see a type B curve in severe cases, where the ossicular fixation is so significant that the eardrum movement is dramatically impaired. It is important to combine tympanometry findings with other clinical data and audiological tests to make a conclusive diagnosis.
Q 22. Describe the role of tympanometry in the diagnosis of Eustachian tube dysfunction.
Tympanometry plays a crucial role in diagnosing Eustachian tube dysfunction (ETD) by assessing the pressure equalization in the middle ear. The Eustachian tube connects the middle ear to the nasopharynx, and its primary function is to ventilate the middle ear, maintaining pressure equilibrium with the atmospheric pressure. In ETD, this function is impaired.
A normal tympanogram shows a peak at or near atmospheric pressure, indicating proper Eustachian tube function. However, in ETD, we may see a negative middle ear pressure (indicating a blockage or poor ventilation), a flat tympanogram (suggesting fluid in the middle ear), or even a type B tympanogram if there’s significant middle ear effusion.
For example, a patient presenting with recurrent ear infections and hearing loss might undergo tympanometry. If the test reveals a negative middle ear pressure and a reduced compliance, it strongly suggests ETD, possibly contributing to the patient’s symptoms. This information helps guide further investigations and treatment strategies, such as decongestants or even surgical intervention in severe cases.
Q 23. What is the relationship between tympanometry and acoustic reflexes?
Tympanometry and acoustic reflexes are closely related, both providing valuable insights into the functionality of the middle ear system. Acoustic reflexes are involuntary muscle contractions in the middle ear (stapedius muscle) in response to intense sounds. These contractions are measured during tympanometry.
The presence and characteristics of the acoustic reflex can be informative. A normal acoustic reflex suggests that the middle ear conduction pathway is intact, and the stapedius muscle is functioning properly. Absence of the acoustic reflex can indicate pathology affecting either the conductive pathway (e.g., ossicular chain disruption) or the neural pathways involved in the reflex arc. This is a critical parameter for differentiating between conductive and sensorineural hearing loss.
Think of it like this: tympanometry assesses the overall mechanics of the middle ear (like checking if a car’s engine is turning over), while the acoustic reflex tests a specific aspect of the middle ear’s function (like checking if the car’s horn works). Together, they provide a comprehensive picture.
Q 24. Explain how middle ear pressure is measured using tympanometry.
Tympanometry measures middle ear pressure indirectly using a specialized probe placed in the ear canal. This probe delivers a tone of specific frequency and measures the impedance (resistance to sound) across the tympanic membrane (eardrum).
The probe changes the air pressure in the ear canal systematically, and the impedance of the tympanic membrane is measured at each pressure step. The point of lowest impedance indicates the pressure that equates the pressure in the middle ear with the external environment. This is shown graphically as a peak in the tympanogram. This peak represents the static middle ear pressure. It’s like finding the equilibrium point between two different water levels using a pipe that connects them; the lowest resistance point signifies when they’re equally balanced. The pressure is then measured in daPa (decapascals).
For instance, a peak around 0 daPa suggests normal middle ear pressure, while a negative peak signifies negative middle ear pressure, a common finding in Eustachian tube dysfunction.
Q 25. What are the safety precautions to consider while conducting tympanometry?
Safety during tympanometry is paramount. The most critical precaution involves ensuring the probe tip is clean and disinfected between patients to prevent the spread of infection. The probe should never be forced into the ear canal. Gentle insertion is key to prevent discomfort and potential injury to the ear canal.
It is also essential to properly position and stabilize the patient’s head during the test to avoid movement artifacts that could affect the accuracy of the results. If the patient experiences any discomfort or pain during the procedure, the test should be stopped immediately. A clear explanation of the procedure beforehand can help alleviate patient anxiety. Contraindications include an active ear infection or a perforated eardrum where the air pressure changes could cause further damage.
Q 26. How can you ensure the accuracy and reliability of tympanometry results?
Ensuring accurate and reliable tympanometry results requires attention to several factors. First, the equipment should be properly calibrated and maintained regularly. This includes checking the probe’s functionality and ensuring the accuracy of the pressure readings. Calibration ensures the readings are not biased or affected by instrument malfunction.
The examiner’s skill and experience also play a significant role. Proper probe placement and patient positioning are critical. An experienced audiologist will know how to interpret subtle variations and avoid artifacts. Repeat testing can be performed if there’s any doubt about the results. Finally, ensuring appropriate patient cooperation is crucial; a restless or uncooperative patient can produce inaccurate readings.
Q 27. How do you explain tympanometry results to a patient and their family?
Explaining tympanometry results to a patient and their family requires clear, simple language, avoiding technical jargon. I would start by explaining the purpose of the test: to evaluate the function of the middle ear and assess the health of the eardrum and the air pressure behind it.
I would then use visual aids, like the actual tympanogram printout, to show them the findings. For example, I might say, “This graph shows the pressure in your middle ear. This peak indicates that your eardrum is moving normally and the pressure is where it should be.” Or, “The results show some fluid or blockage, affecting the pressure behind your eardrum; this may be the reason for your hearing difficulties.” I would avoid using technical terms like compliance or impedance unless specifically requested and explained in a relatable way. Finally, I would discuss what the results suggest, the next steps, and answer any questions they might have.
Q 28. What are the current trends and advancements in tympanometry technology?
Current trends in tympanometry technology are focused on improving efficiency, accuracy, and integration with other diagnostic tools. Advances include automated systems that reduce the time and skill required for the test, leading to improved workflow. There’s an increasing integration of tympanometry with other diagnostic tools, such as acoustic reflex testing and otoacoustic emissions (OAEs), providing a more comprehensive evaluation of hearing.
Miniaturization and improved probe design are making the test more comfortable for patients, and some systems now offer digital recording and storage of results, improving record keeping and access to data. Research is exploring the use of new algorithms and artificial intelligence (AI) to better interpret tympanograms, leading to more precise diagnoses and facilitating early detection of middle ear problems.
Key Topics to Learn for Tympanometry Interview
- Basic Principles of Tympanometry: Understanding the underlying physics of sound and pressure, and how they relate to middle ear function.
- Types of Tympanograms: Familiarize yourself with interpreting different tympanogram types (A, As, B, C) and their clinical significance. Practice associating specific patterns with potential middle ear pathologies.
- Equipment and Procedure: Know the different types of tympanometers, the steps involved in performing a test, and potential sources of error or artifacts.
- Clinical Applications: Understand how tympanometry is used to diagnose middle ear disorders, such as otitis media, otosclerosis, and Eustachian tube dysfunction. Be prepared to discuss specific case scenarios.
- Interpreting Results: Develop your skills in accurately analyzing tympanograms and correlating findings with patient history and other audiological test results.
- Limitations of Tympanometry: Be aware of the situations where tympanometry may not provide a conclusive diagnosis and understand its limitations in certain patient populations.
- Differential Diagnosis: Practice distinguishing between different middle ear conditions based on tympanometry findings and other clinical information.
- Troubleshooting: Be prepared to discuss common problems encountered during tympanometry and how to address them.
Next Steps
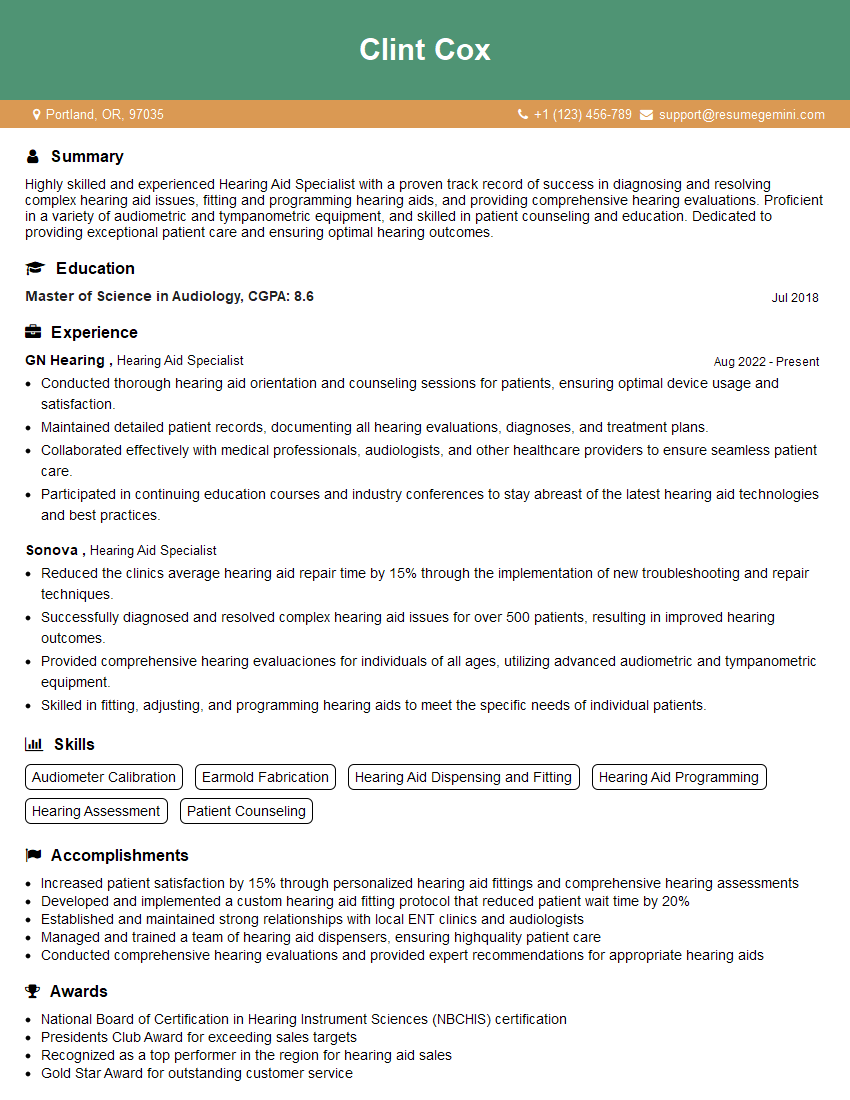
Mastering tympanometry is crucial for career advancement in audiology and related fields. A strong understanding of this essential diagnostic tool opens doors to a wider range of opportunities and demonstrates a high level of clinical competence. To maximize your job prospects, crafting a compelling and ATS-friendly resume is paramount. ResumeGemini is a trusted resource to help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Tympanometry are available through ResumeGemini, allowing you to showcase your expertise and land your dream role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.