Preparation is the key to success in any interview. In this post, we’ll explore crucial Vaginal Birth After Cesarean interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Vaginal Birth After Cesarean Interview
Q 1. Define Vaginal Birth After Cesarean (VBAC).
Vaginal Birth After Cesarean (VBAC) refers to a woman giving birth vaginally after having had a previous cesarean delivery. It’s a perfectly viable option for many women, offering the potential benefits of a vaginal birth, but it’s crucial to understand the associated risks and carefully evaluate the individual’s suitability for a VBAC attempt.
Q 2. What are the contraindications for VBAC?
Several contraindications exist for VBAC. These are situations where attempting a VBAC poses an unacceptably high risk of complications. These include:
- Classical or T-shaped uterine scar: This type of scar is significantly more prone to rupture during labor.
- Previous uterine rupture: The risk of a second rupture is substantially increased.
- Two or more prior cesarean deliveries: The risk of uterine rupture increases with each subsequent cesarean.
- Uterine scar dehiscence (separation of the scar): Any evidence of the scar not fully healing or weakening would be a contraindication.
- Active genital herpes: This can transmit the infection to the baby during delivery.
- Significant pelvic abnormality or disproportion between the baby’s size and the mother’s pelvis: This may make vaginal delivery difficult or impossible.
- Presence of a medical condition prohibiting pushing: Conditions such as significant cardiovascular issues or a history of severe hemorrhage can make vaginal delivery unsafe.
It’s important to remember that the presence of any of these contraindications doesn’t automatically preclude a VBAC. Each case is carefully assessed on an individual basis.
Q 3. Describe the criteria for a successful VBAC candidate.
A successful VBAC candidate typically meets several criteria. These criteria help determine if a trial of labor after cesarean (TOLAC) is appropriate and safe:
- Low-risk pregnancy: No significant complications during the current pregnancy.
- Previous low transverse uterine incision: This type of incision is less likely to rupture than a classical or T-shaped incision. This is often visualized on prior cesarean notes and/or ultrasound.
- Adequate pelvic structure: The mother’s pelvis is large enough to accommodate the baby.
- Access to immediate emergency care: A hospital with on-site cesarean delivery capacity is essential.
- Experienced healthcare providers: Physicians and nurses proficient in managing VBAC.
- Appropriate monitoring techniques: Continuous electronic fetal monitoring is crucial throughout labor.
- Patient understanding and informed consent: The mother must understand the risks and benefits and make an informed decision.
For example, a woman with a previous low transverse uterine incision, a singleton pregnancy, and no other risk factors would be a suitable candidate for a VBAC trial. Conversely, a woman with a previous classical incision or a history of uterine rupture would not be a suitable candidate.
Q 4. Explain the role of continuous electronic fetal monitoring during VBAC.
Continuous electronic fetal monitoring (EFM) plays a vital role during VBAC. It provides real-time assessment of the fetal heart rate, allowing for early detection of fetal distress. This is particularly crucial in VBAC because of the increased risk of uterine rupture. Changes in the fetal heart rate pattern, such as late decelerations or bradycardia, can indicate compromised fetal oxygenation and may signal a potential uterine rupture or other obstetric emergency necessitating immediate intervention. The continuous monitoring helps clinicians promptly identify and respond to these potentially life-threatening situations. For instance, a sudden drop in the fetal heart rate accompanied by maternal pain could indicate a uterine rupture and require immediate action.
Q 5. What are the potential risks associated with VBAC?
While VBAC offers potential benefits, it’s essential to acknowledge the associated risks. The most significant risk is uterine rupture, where the uterine scar tears open during labor. This is a serious complication that can lead to significant maternal and fetal morbidity and mortality. Other risks include:
- Postpartum hemorrhage: Excessive bleeding after delivery.
- Infection: Increased risk of infection compared to vaginal birth without prior cesarean.
- Repeat cesarean delivery: If vaginal delivery fails.
- Placenta accreta/increta/percreta: Abnormal implantation of the placenta which can be more likely with previous uterine surgery.
The likelihood of these risks depends on various factors, including the type of uterine incision, the number of previous cesareans, and maternal risk factors. These risks are carefully weighed against the potential benefits before a decision regarding VBAC is made.
Q 6. How do you assess the risk of uterine rupture during VBAC?
Assessing the risk of uterine rupture during VBAC involves a comprehensive evaluation of the patient’s history and current condition. This includes a thorough review of previous medical records, particularly the type of uterine incision performed in the prior cesarean. Factors such as the presence of a classical incision (significantly increases the risk), previous uterine rupture, number of prior cesarean sections, and other associated risk factors (e.g., advanced maternal age, preeclampsia) are considered. Furthermore, the current labor is closely monitored for signs suggestive of rupture, such as fetal heart rate abnormalities and maternal pain. The likelihood of uterine rupture is discussed with the patient to facilitate shared decision making.
Q 7. Discuss the management of a suspected uterine rupture during labor.
Suspected uterine rupture during labor is a serious obstetric emergency requiring immediate intervention. Management involves:
- Immediate cessation of labor: Pushing should be stopped immediately.
- Rapid assessment of maternal and fetal status: This includes assessing vital signs, fetal heart rate, and abdominal examination.
- Initiation of intravenous fluids and blood transfusion: Preparation for potential massive blood loss.
- Emergency cesarean delivery: This is typically the definitive treatment, even if the rupture is not visually confirmed.
- Surgical repair of the uterine rupture: This is performed during the cesarean section.
- Postoperative care: Includes monitoring for ongoing hemorrhage and infection.
The key is rapid recognition and immediate action. Delay in treatment can significantly increase maternal and fetal morbidity and mortality. The scenario dictates that swift transfer to an OR for immediate C-section takes priority.
Q 8. What are the key elements of informed consent for VBAC?
Informed consent for a Vaginal Birth After Cesarean (VBAC) is crucial. It ensures the patient understands the procedure completely, including its benefits, risks, and alternatives, empowering them to make an informed decision. Key elements include a clear explanation of the procedure itself, outlining what a VBAC entails and how it differs from a repeat cesarean. It also requires a thorough discussion of the potential benefits, such as faster postpartum recovery, reduced risk of complications associated with major surgery, and the emotional satisfaction of a vaginal delivery. Crucially, it must detail the potential risks, such as uterine rupture (a tear in the uterine scar), which is the most significant risk, as well as slower labor progression, postpartum hemorrhage, and the need for emergency cesarean.
- Procedure Details: A clear explanation of the VBAC process, including labor management strategies.
- Benefits: Faster recovery, reduced risk of surgical complications, potential for a more satisfying birth experience.
- Risks: Uterine rupture, postpartum hemorrhage, slower labor progression, need for emergency Cesarean.
- Alternatives: Repeat Cesarean section, detailed explanation of why this might be the safer option in certain circumstances.
- Questions and Answers: Ample opportunity for the patient to ask questions and receive clear, concise answers.
- Documentation: A signed consent form indicating the patient understands all aspects of the procedure and risks.
Q 9. Describe the process of obtaining informed consent for VBAC.
Obtaining informed consent for VBAC is a multi-step process that requires significant time and detailed communication. It begins with a thorough review of the patient’s medical history, focusing on prior cesarean(s), including the indication for the previous cesarean, the type of incision (classical vs. low transverse), and any other relevant medical conditions. I then explain the VBAC process, emphasizing both the potential benefits and risks in a clear and non-judgmental manner. I use visual aids like diagrams to illustrate the uterine scar and potential rupture sites. I actively encourage the patient to ask questions, and I answer them honestly and thoroughly. This discussion isn’t a one-time event; often multiple consultations are needed to ensure complete understanding. Finally, once the patient expresses comprehension and is comfortable making a decision, the consent form is reviewed line by line, ensuring the patient understands each element before signing.
For example, with a patient who had a previous low transverse uterine incision and a straightforward pregnancy, the discussion might focus more on the benefits and less on the specific risks of uterine rupture, while the converse would be true for a patient with a classical incision or other risk factors. The goal is to tailor the discussion to each individual patient’s unique circumstances.
Q 10. How do you counsel patients on the risks and benefits of VBAC?
Counseling patients on the risks and benefits of VBAC requires a balanced approach. I always start by highlighting that VBAC is a safe option for many women, but it is not without risks. I use a collaborative approach, sharing evidence-based information without imposing my personal opinion. The benefits often include faster recovery, shorter hospital stays, and fewer potential complications associated with major surgery. The risks, however, are centered around uterine rupture, which while rare, can be life-threatening to both mother and baby. Other potential risks include postpartum hemorrhage, infection, and the need for an emergency cesarean. To make it relatable, I often use real-life examples and statistics, avoiding overly technical medical jargon. I always emphasize shared decision-making, ensuring the patient understands that the choice is theirs, based on a clear understanding of the situation.
For instance, I might share statistics on the success rate of VBAC in similar cases, but I also explicitly discuss what a uterine rupture entails and what procedures would be taken to manage it. The goal is to empower the patient to make a decision that aligns with her personal values and risk tolerance.
Q 11. What are the emotional and psychological considerations for women considering VBAC?
Emotional and psychological considerations are paramount in VBAC decisions. Many women experience anxiety about the possibility of uterine rupture, stemming from their previous Cesarean experience or concerns for their baby’s safety. Previous negative birth experiences can significantly impact their emotional state, and some may feel pressure from family or societal expectations. Some women may harbor feelings of failure related to their previous Cesarean birth, while others may have strong desires for a vaginal birth, leading to heightened emotional investment in the VBAC attempt. Therefore, creating a safe and supportive environment for open communication and addressing these emotions is key. I often collaborate with a psychologist or counselor if additional support is needed.
I find it beneficial to provide reassurance and empower these women by acknowledging their feelings and working to reduce anxiety through education and realistic expectations. I emphasize that a planned VBAC doesn’t mean failure if a Cesarean becomes necessary.
Q 12. Explain your experience with managing VBAC labor.
My approach to managing VBAC labor centers on continuous fetal monitoring, careful assessment of labor progress, and proactive management of potential complications. Each VBAC labor is unique, requiring personalized attention. I carefully monitor the mother’s vital signs, including blood pressure, pulse, and temperature, and the baby’s heart rate using electronic fetal monitoring. Regular vaginal exams assess cervical dilation and effacement. I remain vigilant for signs of uterine rupture, such as sudden abdominal pain, fetal distress, or maternal hypotension. Should these signs appear, immediate action, including Cesarean delivery, is taken.
For instance, I had a patient who experienced slower than expected progress during VBAC. Instead of immediate intervention, we utilized various supportive measures, including amniotomy and position changes, to promote natural labor progression. Continuous monitoring allowed us to detect subtle changes in fetal heart rate, leading to a timely Cesarean when necessary, resulting in a safe outcome for both mother and child.
Q 13. Describe your approach to pain management during VBAC.
Pain management during VBAC is individualized to the patient’s preferences and labor progression. A variety of options are available, including non-pharmacological methods like breathing techniques, water immersion, and massage, alongside pharmacological options such as epidurals, intravenous opioids, and nitrous oxide. My approach is to provide multimodal analgesia tailored to the woman’s specific needs and pain tolerance level. I prefer to initiate pain management earlier in labor, rather than waiting until the pain is unbearable, enabling more effective pain relief and reducing the risk of unnecessary interventions.
For example, a patient might prefer an epidural for complete pain relief, while another might choose to rely on non-pharmacological techniques until later stages of labor. The key is to maintain open communication, provide choices, and ensure the patient feels in control of her pain management.
Q 14. How do you monitor fetal well-being during VBAC labor?
Continuous electronic fetal monitoring (EFM) is the cornerstone of fetal well-being assessment during VBAC labor. EFM provides a continuous record of the fetal heart rate, allowing detection of any abnormalities indicative of fetal distress. I supplement EFM with intermittent auscultation, listening to the fetal heart rate using a Doppler or fetoscope to ensure accurate monitoring. I also monitor the frequency and strength of contractions and assess the mother’s vital signs. Any signs of fetal distress, such as late decelerations or tachycardia, trigger immediate intervention, often involving repositioning the mother, increasing intravenous fluids, and potentially administering oxygen.
If concerning patterns emerge despite supportive measures, a prompt Cesarean delivery is undertaken to prevent adverse outcomes. Regular assessments of maternal vital signs and ongoing communication with the patient are vital parts of this continuous monitoring process.
Q 15. What are the signs of labor dystocia in a VBAC patient?
Labor dystocia in a VBAC patient, meaning a difficult labor, can manifest in several ways, often subtly different than in nulliparous women. It’s crucial to remember that uterine scar rupture is a rare but serious complication we must always consider. Signs might include:
- Prolonged active phase of labor: The cervix isn’t dilating or descending at the expected rate. For example, a woman might be in active labor for many hours with minimal progress.
- Arrest of descent: The baby’s head stops moving down the birth canal despite adequate contractions.
- Secondary arrest of dilation: The cervix stops dilating after it’s been progressing.
- Abnormal fetal heart rate patterns: These can indicate fetal distress and necessitate immediate intervention. Changes like late decelerations or prolonged decelerations are especially worrisome.
- Maternal signs of distress: Exhaustion, high levels of anxiety, or severe pain may indicate underlying issues.
- Changes in uterine contractions: Weak, infrequent, or uncoordinated contractions can hinder labor progress. Conversely, abnormally strong or prolonged contractions might also be a cause for concern.
It’s important to note that these signs aren’t always definitive. A thorough assessment, including a careful review of the patient’s history and regular monitoring of the mother and baby, is essential for accurate diagnosis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage labor dystocia during a VBAC attempt?
Managing labor dystocia in a VBAC attempt requires a multi-faceted approach, prioritizing the safety of both mother and baby. The management strategy is highly individualized, depending on the specific causes and severity of the dystocia.
- Careful monitoring: Continuous fetal heart rate monitoring and regular cervical examinations are paramount.
- Augmentation of labor: If contractions are inadequate, augmentation with oxytocin may be considered, but it must be carefully titrated and closely monitored to avoid hyperstimulation of the uterus, which is a significant risk in VBAC patients.
- Amniotomy: Artificial rupture of the membranes can sometimes stimulate labor progress, but it carries risks, and is a decision to be carefully considered based on the circumstances.
- Change in position: Encouraging the mother to change positions can help improve fetal descent and labor progression.
- Pain management: Effective pain management is crucial, allowing the mother to relax and conserve energy for labor. Epidural analgesia is a common choice, but other methods should be considered as per the patient’s wishes and clinical situation.
- Operative delivery: If conservative measures fail to resolve the dystocia, or if there are signs of fetal distress or maternal exhaustion, an operative vaginal delivery (forceps or vacuum) or cesarean birth might be necessary. The decision to proceed with an operative vaginal delivery needs careful consideration of the maternal history, risks of uterine rupture, and fetal factors.
Close collaboration between the obstetrician, anesthesiologist, and nursing staff is vital for effective and safe management.
Q 17. What is your experience with operative vaginal delivery in VBAC cases?
Operative vaginal delivery (OVD) in VBAC cases is a carefully considered option, used when vaginal delivery is deemed appropriate but augmentation of labor has failed to achieve progress or there are concerns about fetal wellbeing. The decision is highly individualized and dependent on multiple factors, including cervical dilation, station of the presenting part, fetal head position and molding, maternal pelvis shape, and the overall clinical picture.
In my experience, the success rate of OVD in VBAC is highly dependent on careful patient selection. We favor vacuum extraction over forceps, as forceps are considered more likely to cause perineal or cervical trauma. However, the ultimate choice depends on the specifics of each individual case. The use of OVD is always balanced against the risk of uterine rupture, which is a potentially life-threatening event.
Continuous fetal monitoring is essential during OVD to detect any signs of fetal distress. We closely monitor the mother for signs of vaginal or cervical lacerations and also for uterine rupture, which is particularly important in a VBAC case.
Q 18. Describe your experience with managing postpartum hemorrhage after VBAC.
Postpartum hemorrhage (PPH) is a significant concern after VBAC, as it has a slightly higher incidence compared to vaginal delivery in nulliparous women. Our management strategy follows established guidelines emphasizing early recognition and prompt intervention.
- Early recognition: Close monitoring of blood loss, vital signs, and uterine tone is essential in the immediate postpartum period. We use visual estimation of blood loss, coupled with regular weighing of saturated pads.
- Uterine massage: Gentle uterine massage is the first-line treatment to improve uterine tone and reduce bleeding.
- Pharmacological intervention: Oxytocin is the primary medication for managing PPH, given intravenously or intramuscularly. If oxytocin is ineffective, other uterotonics such as methylergonovine or carboprost tromethamine may be used.
- Surgical intervention: If conservative measures fail to control the bleeding, surgical interventions such as uterine artery embolization or hysterectomy may be necessary. These are life-saving procedures performed when the mother’s condition is critical.
Preventing PPH is crucial. We emphasize proactive measures such as active management of the third stage of labor (controlled cord traction and administration of uterotonics) and careful assessment of the placenta for any retained fragments.
Q 19. What are the postpartum considerations specific to VBAC?
Postpartum considerations specific to VBAC include a heightened awareness of potential complications like uterine rupture and PPH, as mentioned earlier. However, other aspects are also crucial:
- Pain management: VBAC patients may experience more pain postpartum due to the stress on the uterine scar. We offer various pain relief options, including analgesics and, where necessary, epidural analgesia.
- Uterine scar surveillance: While less common, the possibility of delayed uterine rupture remains. Therefore, we recommend follow-up appointments to assess the healing process of the uterine scar and address any concerns.
- Emotional support: VBAC patients may experience more anxiety and emotional stress throughout their pregnancy and postpartum period. Offering emotional support and psychological counselling as needed is highly important.
- Breastfeeding support: While not unique to VBAC, breastfeeding can be helpful in uterine involution, and dedicated breastfeeding support should be provided.
- Early mobilization: Encouraging early ambulation helps prevent complications like deep vein thrombosis, a potential risk in all postpartum patients.
Regular monitoring and individualized care are paramount in ensuring a healthy recovery.
Q 20. How do you counsel patients on breastfeeding after VBAC?
Counseling patients on breastfeeding after VBAC is similar to counseling any postpartum mother, emphasizing its benefits for both mother and baby. However, we may need to address concerns specifically related to the VBAC experience.
We provide information on the benefits of breastfeeding, including promoting maternal-infant bonding, providing optimal nutrition for the baby, and facilitating uterine involution. We also emphasize that breastfeeding itself does not increase the risk of uterine rupture.
We often address concerns about potential pain or discomfort in the abdomen, particularly if the mother had a prior cesarean section. We discuss pain management strategies like warm compresses, positioning techniques, and appropriate analgesics to ensure comfortable breastfeeding.
We encourage early initiation of breastfeeding and provide comprehensive support, involving lactation consultants as needed, to overcome any difficulties and ensure successful breastfeeding outcomes.
Q 21. What are the common complications associated with VBAC?
Common complications associated with VBAC include:
- Uterine rupture: This is the most serious complication, though rare. It can lead to life-threatening hemorrhage for the mother and fetal distress or death. Risk factors include prior uterine surgery, prior classical cesarean incision, and labor dystocia.
- Postpartum hemorrhage (PPH): As discussed previously, PPH has a slightly higher incidence in VBAC compared to vaginal delivery in nulliparous women.
- Infection: The risk of infection is similar to that in other vaginal deliveries but proper care and monitoring to prevent infection remains crucial.
- Perineal trauma: Similar to other vaginal deliveries, tearing can occur in the perineum.
- Uterine atony: Weakness of the uterine muscles, potentially resulting in excessive bleeding.
Many of these risks can be mitigated through careful patient selection, meticulous monitoring during labor, and prompt intervention when complications arise.
Q 22. Explain the difference between a trial of labor after Cesarean (TOLAC) and VBAC.
While often used interchangeably, TOLAC (Trial of Labor After Cesarean) and VBAC (Vaginal Birth After Cesarean) have a subtle but important distinction. TOLAC refers to the process of attempting a vaginal birth after a previous cesarean. It encompasses the entire labor experience, from the start of contractions until the outcome – either a successful vaginal delivery or a repeat cesarean. VBAC, on the other hand, refers to the successful outcome of a TOLAC; it specifically means a woman successfully delivers vaginally after a previous cesarean. Think of TOLAC as the journey and VBAC as the destination. A woman can undergo a TOLAC without achieving a VBAC if a repeat cesarean becomes necessary.
Q 23. How do you assess the adequacy of uterine scar integrity?
Assessing uterine scar integrity is crucial for determining a woman’s suitability for TOLAC. We use a combination of methods:
- Ultrasound: A transabdominal ultrasound is typically performed to visualize the uterine scar. We look for characteristics like thickness, width, and presence of any irregularities or thinning, which could indicate a higher risk of uterine rupture.
- Careful review of previous cesarean notes and operative reports: This helps us understand the type of incision (low transverse or classic), any complications during the previous surgery, and the overall surgical technique used. A classic incision carries a significantly higher risk of rupture than a low transverse incision.
- Patient history and physical exam: We thoroughly discuss previous pregnancies and deliveries, looking for any factors that might influence scar integrity. The physical exam helps rule out any current uterine abnormalities.
It’s important to remember that even with thorough assessment, there’s always a small risk of uterine rupture, which is why continuous monitoring during labor is essential.
Q 24. What are the latest guidelines and recommendations regarding VBAC?
Current guidelines on VBAC emphasize a personalized approach, considering both maternal and fetal well-being. Recommendations generally include:
- Careful patient selection: Only women with a low-risk profile and a single low-transverse uterine scar are usually considered candidates for TOLAC.
- Continuous electronic fetal monitoring during labor: This helps detect any signs of fetal distress that might necessitate a rapid cesarean.
- Immediate access to emergency cesarean section: A fully equipped operating room and anesthesia team must be readily available throughout labor.
- Shared decision-making: Women need thorough counseling about the risks and benefits of both TOLAC and repeat cesarean, allowing them to make an informed choice.
The specific guidelines may vary slightly depending on the institution and the individual patient’s circumstances, but the focus is always on safety and individualized care.
Q 25. Describe your experience with VBAC in high-risk pregnancies.
My experience with VBAC in high-risk pregnancies underscores the importance of individualized risk assessment and close monitoring. For instance, I’ve managed women with gestational diabetes who required extra vigilance for both maternal and fetal well-being during labor. Others presented with pre-eclampsia, necessitating careful blood pressure control and frequent fetal monitoring. In these situations, I worked closely with a multidisciplinary team including maternal-fetal medicine specialists, anesthesiologists, and neonatologists, to ensure the safety of both mother and baby. The decision for a TOLAC was always made on a case-by-case basis, weighing potential benefits against potential risks. For example, in a case of severe preeclampsia, the risks of continuing labor might outweigh the benefits of a VBAC, even with close monitoring, and an earlier cesarean would be the safer approach. Every situation is unique, and the goal is always to make the best, safest choice for the individual patient.
Q 26. How do you address patient anxieties and concerns about VBAC?
Addressing patient anxieties about VBAC is a key part of my practice. Many women fear uterine rupture, and this is a valid concern. I address this by providing evidence-based information, explaining the risks and benefits in a clear and understandable way. I emphasize that we use continuous monitoring to detect any potential issues early, and that a repeat cesarean is always an option if necessary. I encourage open communication and answer questions patiently, fostering a trusting relationship. I often share success stories (while maintaining patient confidentiality) to show that VBAC is a safe option for many women, and I also emphasize the emotional benefits of a vaginal birth for many women who desire it. Creating a supportive and collaborative environment helps to alleviate anxiety and empowers women to make informed decisions.
Q 27. What are your strategies for supporting VBAC patients during labor?
My approach to supporting VBAC patients during labor focuses on evidence-based care and continuous emotional support. This includes:
- Continuous electronic fetal monitoring: This is essential for detecting any signs of fetal distress.
- Frequent vaginal exams: To assess labor progress and identify any potential complications.
- Pain management: Offering various options, including epidural analgesia, to help women manage their pain effectively.
- Emotional support: Providing a calm and reassuring presence, empowering women through education, and allowing for partner or doula involvement.
- Labor augmentation strategies: Used judiciously if labor is not progressing satisfactorily.
Throughout the labor process, I prioritize open communication and collaboration with the patient and her support system, ensuring that everyone is involved in the decision-making process.
Q 28. How do you evaluate the success of a VBAC attempt?
Evaluating the success of a VBAC attempt involves considering multiple factors beyond simply whether a vaginal delivery occurred.
- Vaginal delivery without complications: A successful VBAC is one without uterine rupture, postpartum hemorrhage, or other significant maternal or neonatal complications.
- Maternal and fetal well-being: Postpartum assessment includes monitoring for signs of infection, hemorrhage, and uterine atony. Neonatal assessment involves checking for signs of hypoxia or other complications during or after delivery.
- Patient satisfaction: A woman’s overall experience and feelings about her labor and delivery are important aspects to consider.
A successful VBAC is one that prioritizes the health and well-being of both mother and child, respects patient autonomy, and leaves the patient feeling empowered and satisfied with her birth experience.
Key Topics to Learn for Vaginal Birth After Cesarean (VBAC) Interview
- Maternal Anatomy and Physiology Post-Cesarean: Understand the changes in the uterine scar and its implications for VBAC.
- Risk Assessment and Patient Selection: Learn the criteria for identifying suitable candidates for VBAC and those who are not.
- Labor Management in VBAC: Discuss the strategies for monitoring labor progress, managing potential complications, and making informed decisions during labor.
- Intrapartum Complications and Management: Explore potential complications specific to VBAC, such as uterine rupture, and their management protocols.
- Postpartum Care Specific to VBAC: Understand the specific postpartum care considerations for women who have undergone VBAC.
- Evidence-Based Practices in VBAC: Familiarize yourself with the latest research and guidelines surrounding VBAC.
- Patient Counseling and Shared Decision-Making: Understand the importance of effective communication and shared decision-making with patients considering VBAC.
- Ethical Considerations in VBAC: Explore the ethical implications of VBAC decisions and potential conflicts of interest.
- Comparison of VBAC Outcomes with Repeat Cesarean: Be prepared to discuss the benefits and risks of VBAC compared to repeat cesarean.
- Role of Ultrasound in VBAC: Understand how ultrasound can be used to assess the uterine scar and predict potential complications.
Next Steps
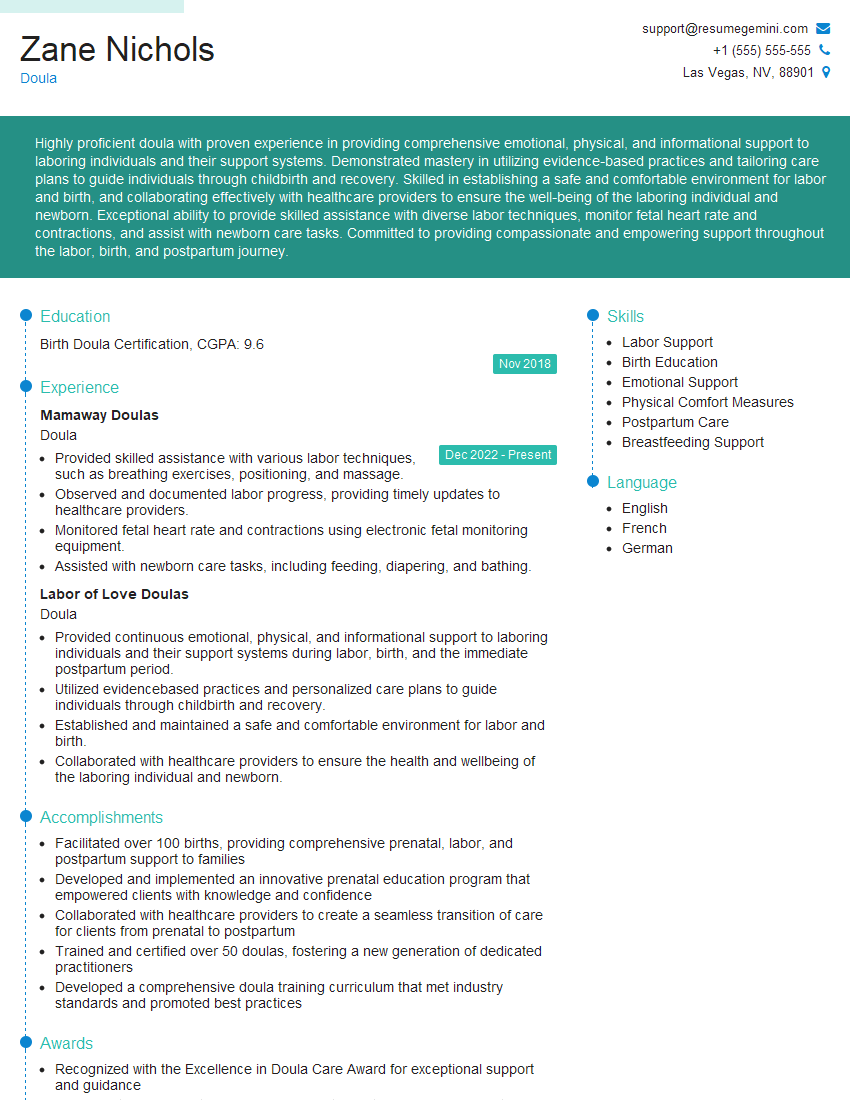
Mastering the intricacies of Vaginal Birth After Cesarean significantly enhances your value as a healthcare professional, opening doors to specialized roles and advanced opportunities. A strong resume is crucial in showcasing your expertise. To increase your job prospects, create an ATS-friendly resume that effectively highlights your VBAC knowledge and experience. We highly recommend using ResumeGemini to build a professional and impactful resume that stands out. ResumeGemini provides examples of resumes tailored to Vaginal Birth After Cesarean to help guide your process. Take the next step towards your career advancement today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.