Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Vulvar and Vaginal Disorders interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Vulvar and Vaginal Disorders Interview
Q 1. Describe the diagnostic criteria for lichen sclerosus.
Lichen sclerosus (LS) is a chronic inflammatory skin condition primarily affecting the vulva, but can also involve the perianal area. Diagnosis relies on clinical presentation and biopsy. It’s not a single disease with a definitive test, rather a diagnosis made by recognizing a characteristic pattern.
- Clinical Presentation: This is the cornerstone of diagnosis. Look for porcelain-white, thinned, atrophic skin with loss of normal skin markings. There may be fissures, erosions, or excoriations. The affected area feels paper-thin and may be itchy or painful. Vulvar stenosis (narrowing of the vaginal opening) can occur in severe cases, particularly in children.
- Biopsy: While clinical presentation is often sufficient, a skin biopsy is sometimes necessary to confirm the diagnosis and rule out other conditions. Histology reveals a characteristic pattern of thinning of the epidermis, loss of rete ridges, and a subepidermal lymphocytic infiltrate.
Think of it like this: imagine a delicate piece of parchment paper. That’s how the vulvar skin can look in LS. The biopsy confirms the microscopic features which solidify the diagnosis. It’s crucial to differentiate LS from other conditions that might present similar symptoms, like psoriasis or other inflammatory dermatoses.
Q 2. Explain the management options for vulvar vestibulitis syndrome.
Vulvar vestibulitis syndrome (VVS) is characterized by chronic vulvar pain, primarily at the vestibule (the area just inside the vaginal opening). Management focuses on pain relief and improving quality of life. There is no single ‘cure’, rather a multi-pronged approach tailored to the individual.
- Pain Management: This is paramount. Options include topical anesthetics (like lidocaine), amitriptyline (an antidepressant with analgesic properties), gabapentin (an anticonvulsant used for nerve pain), and physical therapy (such as pelvic floor muscle relaxation techniques).
- Lifestyle Modifications: Avoiding irritants (like scented soaps, harsh detergents, tight clothing), maintaining good hygiene practices, and stress management techniques are crucial.
- Trigger Identification: Working with a patient to identify specific triggers that worsen pain is important. These might include sexual activity, certain fabrics, or even specific foods. Avoiding these triggers can significantly reduce symptoms.
- Biofeedback and Pelvic Floor Therapy: These can help to identify and address muscle tension which is commonly associated with VVS.
- Hormonal Therapy: In some cases, hormone replacement therapy may be helpful, particularly in postmenopausal women.
For example, a patient might benefit from a combination of topical lidocaine before intercourse, pelvic floor physical therapy, and stress reduction techniques. The management is personalized and requires a collaborative approach between patient and clinician.
Q 3. What are the common causes of vaginal dryness?
Vaginal dryness, or lack of sufficient lubrication, is a common complaint affecting women of all ages, especially those in perimenopause or postmenopause. Several factors contribute.
- Hormonal Changes: Decreased estrogen levels, most prominently during perimenopause and menopause, lead to thinning and decreased elasticity of the vaginal walls, reducing natural lubrication.
- Medications: Certain medications, such as antidepressants, antihistamines, and blood pressure medications, can contribute to vaginal dryness as a side effect.
- Lifestyle Factors: Factors such as insufficient sexual stimulation, inadequate hydration, smoking, and certain medical conditions (e.g., Sjogren’s syndrome) can all play a role.
- Postpartum Changes: Breastfeeding and the hormonal shifts after delivery can temporarily reduce vaginal lubrication.
- Medical Conditions: Certain autoimmune diseases, like Sjögren’s syndrome, can lead to decreased production of lubricating fluids.
It’s important to remember that vaginal dryness is a symptom and the underlying cause needs investigation. For instance, a woman experiencing vaginal dryness during perimenopause may require hormone replacement therapy while a woman experiencing it after starting a new medication might need to discuss alternatives with her doctor.
Q 4. How would you differentiate between bacterial vaginosis and candidiasis?
Bacterial vaginosis (BV) and candidiasis (yeast infection) are two common causes of vaginitis (vaginal inflammation), but they have distinct characteristics. Differentiating them is essential for appropriate treatment.
- Bacterial Vaginosis (BV): Caused by an imbalance of the normal vaginal flora, leading to an overgrowth of anaerobic bacteria. Common symptoms include a thin, greyish-white discharge with a fishy odor, particularly after intercourse. On examination, there’s often a homogeneous discharge that adheres to the vaginal walls. The pH of the vaginal fluid is typically elevated (greater than 4.5).
- Candidiasis (Yeast Infection): Caused by an overgrowth of the fungus Candida albicans. Symptoms usually include thick, white, curd-like discharge, intense itching, and vulvar redness. The pH is usually normal or slightly acidic.
A key difference is the discharge. Imagine BV as a thin, watery, fishy-smelling discharge, while candidiasis presents as a thick, white, cottage cheese-like discharge. Microscopic examination of vaginal secretions, along with pH testing, is helpful in making a definitive diagnosis.
Q 5. Discuss the treatment approach for recurrent urinary tract infections in women.
Recurrent urinary tract infections (UTIs) are a significant problem for women, defined as two or more UTIs within six months or three or more within a year. Management goes beyond treating the acute infection and aims to prevent recurrence.
- Treating the Acute Infection: This usually involves a course of antibiotics, tailored to the specific bacteria causing the infection.
- Post-coital Prophylaxis: For women who frequently get UTIs after sexual intercourse, taking a single dose of antibiotics after intercourse can be effective in prevention.
- Cranberry Supplements: Some evidence suggests that cranberry supplements may help prevent UTIs by inhibiting bacterial adherence to the urinary tract, but the effect isn’t consistently powerful enough to be considered primary treatment.
- Increased Fluid Intake: Drinking plenty of fluids helps flush out bacteria from the urinary tract.
- Voiding After Intercourse: Urinating after sexual activity helps to remove bacteria from the urethra.
- Long-term Suppressive Antibiotics: In some cases of very frequent UTIs, a doctor might prescribe a low dose of antibiotics for several months to help suppress bacterial growth. This approach should be carefully considered due to the risk of antibiotic resistance.
A crucial part is identifying contributing factors. These might include anatomical abnormalities, sexual practices, or underlying medical conditions. For example, a woman with recurrent UTIs might benefit from a combination of post-coital prophylaxis and increased fluid intake.
Q 6. What are the risk factors for vulvar cancer?
Vulvar cancer is relatively rare, but several risk factors increase the likelihood of developing it. These factors aren’t always individually conclusive, but their presence increases the overall risk.
- Human Papillomavirus (HPV): Certain high-risk HPV types are strongly linked to vulvar cancer. Infection with these viruses is a significant risk factor.
- Smoking: Smoking significantly increases the risk of several cancers, including vulvar cancer.
- Chronic Inflammation or Lichen Sclerosus: Long-standing vulvar inflammation or the skin condition lichen sclerosus increase the risk of developing vulvar cancer.
- Immunosuppression: Individuals with weakened immune systems, such as those with HIV/AIDS or organ transplant recipients, are at higher risk.
- Age: The risk of vulvar cancer increases with age, with most cases occurring after age 50.
- Fair Skin and Genetic Predisposition: Some research suggests that individuals with fair skin and a family history of vulvar cancer may have an increased risk.
Think of it as a combination of factors – the more risk factors a woman has, the greater her overall risk. It’s important to be aware of these risk factors and engage in regular screenings and preventive measures.
Q 7. Explain the role of HPV in cervical cancer and other vulvar/vaginal cancers.
Human papillomavirus (HPV) plays a central role in the development of cervical cancer and many other anogenital cancers, including vulvar and vaginal cancers. It’s a sexually transmitted infection, and many different types exist. Some are high-risk, meaning they are strongly associated with cancer.
- HPV and Cervical Cancer: Persistent infection with high-risk HPV types is the main cause of cervical cancer. Regular Pap smears and HPV testing can detect precancerous lesions, allowing for early intervention and prevention of cancer development.
- HPV and Vulvar/Vaginal Cancers: High-risk HPV types are also strongly implicated in the development of vulvar and vaginal cancers. The mechanism is similar to that in cervical cancer: persistent infection leads to cellular changes that can progress to cancer over time.
- HPV Vaccines: HPV vaccines are highly effective in preventing infection with the high-risk HPV types responsible for most cervical, vulvar, and vaginal cancers. They are recommended for adolescents and young adults, before sexual activity begins.
The link between HPV and these cancers highlights the importance of vaccination and regular screenings. Early detection and treatment of HPV-related lesions can significantly reduce the risk of developing cancer.
Q 8. Describe the different types of vulvodynia.
Vulvodynia is a chronic vulvar pain condition, lasting at least three months. It’s categorized based on the location and characteristics of the pain. The most common types are:
- Generalized vulvodynia: Pain is widespread across the vulvar area, often described as a constant burning, aching, or irritation.
- Vestibulodynia: Pain is specifically localized to the vulvar vestibule (the area around the vaginal opening). This is often provoked by touch or pressure, making intercourse or even wearing tight clothing painful.
- Provoked vestibulodynia: Pain is only present when the vestibule is touched or during activities like intercourse.
- Unprovoked vestibulodynia: Pain is present even without any direct touch or pressure.
Diagnosing vulvodynia often involves a thorough history and physical exam, excluding other possible causes like infections or skin conditions. There isn’t one single test to diagnose it.
Imagine it like a persistent toothache – the pain is the primary symptom, and finding the exact cause can be challenging.
Q 9. How would you assess a patient presenting with pelvic organ prolapse?
Assessing a patient with pelvic organ prolapse involves a comprehensive approach. It begins with a detailed history, focusing on symptoms like vaginal pressure, bulging, urinary or bowel dysfunction, and pain. The physical exam is crucial, including:
- Visual inspection: Observing the perineum and vagina for any visible prolapse.
- Digital examination: Assessing the support of the pelvic organs with fingers, feeling for the position of the cervix, uterus, bladder, and rectum.
- Pelvic exam with a speculum: A speculum allows for a closer look at the vaginal walls and cervix to better visualize the prolapse.
- Imaging studies (if needed): Ultrasound, MRI, or cystourethroscopy might be utilized to further evaluate the extent and severity of the prolapse.
The staging of the prolapse (how far the organs have descended) is determined using standardized systems like the POP-Q system, which provides quantitative measurements. It’s important to remember that the patient’s symptoms, not just the stage of the prolapse, should guide treatment decisions.
Think of it like checking a building’s foundation; we need to assess the structure from several angles to fully understand its stability and the extent of any damage.
Q 10. What are the non-surgical management options for pelvic floor dysfunction?
Non-surgical management of pelvic floor dysfunction focuses on strengthening and relaxing the pelvic floor muscles as needed. Options include:
- Pelvic floor physical therapy (PFPT): A trained therapist guides exercises to strengthen weak muscles or relax overly tight ones. This often involves biofeedback to help patients learn to contract and relax their muscles correctly.
- Lifestyle modifications: This could include weight management, avoiding constipation (through diet and increased fluids), and stopping smoking (as it weakens connective tissue).
- Pessary fitting: A pessary is a removable device inserted into the vagina to support prolapsed organs. Different types of pessaries exist to address various prolapse types.
- Electrical stimulation: Mild electrical currents can be used to stimulate pelvic floor muscles, helping them strengthen.
These treatments are often employed in combination and are tailored to the individual patient’s needs and the type of pelvic floor dysfunction they experience.
It’s like rehabilitating an injured muscle; we use various techniques to help the muscles regain their strength and function.
Q 11. Discuss the use of topical corticosteroids in the treatment of vulvar dermatoses.
Topical corticosteroids are a mainstay in treating inflammatory vulvar dermatoses (skin conditions). They reduce inflammation and itching. The choice of corticosteroid (strength and formulation) depends on the severity and type of dermatosis. Examples include:
- Hydrocortisone cream (low potency): Suitable for mild conditions like contact dermatitis.
- Clobetasol propionate ointment (high potency): Reserved for severe conditions like lichen sclerosus, but use is limited due to potential side effects with prolonged use.
It’s crucial to use topical corticosteroids as directed by a physician. Prolonged or excessive use can lead to skin thinning, striae (stretch marks), and other adverse effects. Regular monitoring is necessary, particularly with high-potency corticosteroids.
Imagine it like applying a soothing balm to an irritated area; it helps to reduce inflammation and itching but should be used carefully to avoid overuse.
Q 12. Describe the different types of vaginal infections and their treatment.
Many different vaginal infections can occur, each requiring a specific approach to treatment. Common types include:
- Bacterial vaginosis (BV): An imbalance in the vaginal flora, often treated with metronidazole or clindamycin.
- Vulvovaginal candidiasis (yeast infection): Caused by Candida species, typically treated with antifungal medications like fluconazole or clotrimazole.
- Trichomoniasis: A sexually transmitted infection (STI) caused by the parasite Trichomonas vaginalis, treated with metronidazole or tinidazole.
- Vulvar and Vaginal Atrophy: Often linked to reduced estrogen levels, treated with vaginal estrogen creams or tablets.
Accurate diagnosis is vital; a swab for microscopic examination and culture will help identify the causative agent. Self-treating vaginal infections can be problematic, delaying appropriate treatment and potentially leading to complications.
Think of it like diagnosing a plant disease; you need to correctly identify the pathogen before applying the appropriate treatment.
Q 13. Explain the role of hormone replacement therapy in managing menopausal symptoms.
Hormone replacement therapy (HRT) can effectively manage menopausal symptoms, particularly those related to estrogen deficiency. These symptoms include:
- Vasomotor symptoms: Hot flashes, night sweats.
- Urogenital atrophy: Vaginal dryness, painful intercourse.
- Sleep disturbances: Insomnia.
HRT involves replacing estrogen (and sometimes progesterone, depending on the individual’s situation and uterus status) to alleviate these symptoms. Different routes of administration exist (oral, transdermal, topical), each with advantages and disadvantages.
However, the decision to use HRT should be individualized, considering the patient’s age, risk factors for specific diseases (like breast cancer or cardiovascular disease), and symptom severity. Regular monitoring is crucial while on HRT.
Imagine it as replenishing essential nutrients; HRT restores hormonal balance, alleviating many uncomfortable symptoms.
Q 14. What are the common causes of abnormal uterine bleeding?
Abnormal uterine bleeding (AUB), defined as irregular or excessive bleeding, has many potential causes. These include:
- Hormonal imbalances: Ovulatory dysfunction, thyroid disorders, polycystic ovary syndrome (PCOS).
- Structural abnormalities: Uterine fibroids, polyps, endometrial hyperplasia, cancer.
- Coagulation disorders: Problems with blood clotting.
- Medications: Some medications can cause AUB as a side effect.
- Pregnancy-related causes: Miscarriage, ectopic pregnancy.
A thorough evaluation is necessary to determine the cause, often involving a physical exam, imaging studies (ultrasound), and potentially a biopsy to rule out serious conditions like cancer.
It’s like investigating a car problem; multiple components could be at fault, and a comprehensive diagnostic approach is needed to find the root cause.
Q 15. How would you manage a patient with a suspected case of endometriosis?
Managing suspected endometriosis involves a multi-pronged approach focusing on accurate diagnosis and personalized treatment. The first step is a thorough history taking, including menstrual cycle details, pain characteristics (location, severity, duration), and bowel/bladder symptoms. A pelvic exam is crucial, checking for tenderness and any abnormalities. Imaging, such as a transvaginal ultrasound or MRI, is often necessary to visualize endometrial implants. Laparoscopy, a minimally invasive surgical procedure, provides definitive diagnosis by visualizing and often removing implants. Treatment depends on the severity of symptoms and the patient’s desire for future fertility. Options include pain management (NSAIDs, hormonal contraceptives, analgesics), hormonal therapies (GnRH agonists/antagonists, progestins), and surgery (laparoscopy or laparotomy) to remove implants. For women desiring fertility, surgery may be the primary treatment, while for those who don’t, hormonal suppression might be the best option. Regular follow-ups are crucial to monitor symptoms and treatment effectiveness.
For example, a 28-year-old patient presenting with severe dysmenorrhea and deep dyspareunia (painful intercourse) would undergo a detailed history and pelvic exam. If the exam is suggestive of endometriosis, a transvaginal ultrasound and/or laparoscopy would be recommended to confirm the diagnosis. Treatment would be tailored to her symptoms and fertility desires. If she wishes to conceive, surgery to remove visible implants might be the first step. If she does not, then hormonal therapy might be the most effective management strategy.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Discuss the use of biofeedback in the management of pelvic floor disorders.
Biofeedback is a valuable tool in managing pelvic floor disorders (PFDs) like overactive bladder, fecal incontinence, and chronic pelvic pain. It involves using sensors to monitor muscle activity in the pelvic floor, providing real-time feedback to the patient. This allows them to learn how to consciously control these muscles, improving relaxation and strengthening as needed. For instance, in patients with overactive bladder, biofeedback helps them recognize and manage bladder contractions before they lead to urgency or incontinence. In patients with chronic pelvic pain, biofeedback can help identify and release tension in the pelvic floor muscles, reducing pain and discomfort. The process typically involves several sessions with a trained therapist, who guides the patient through exercises and provides personalized feedback. Success depends on patient engagement and consistent practice of learned techniques outside of therapy sessions.
Imagine a patient struggling with urinary urgency and frequency. Biofeedback can show her the muscle contractions associated with her urge, allowing her to learn techniques to relax her pelvic floor and delay urination. Over time, this can lead to a significant reduction in her symptoms. Similarly, a patient experiencing chronic pelvic pain might learn to release tension in the pelvic floor muscles through biofeedback, leading to a decrease in pain and improved quality of life.
Q 17. What are the common side effects of hormone therapy?
Hormone therapy, often used to manage menopausal symptoms or other gynecological conditions, can have various side effects. These vary depending on the type and dose of hormones used. Common side effects include:
- Breast tenderness or enlargement: This is often reported, especially in the early stages of therapy.
- Mood changes: Some women experience irritability, anxiety, or depression.
- Headaches: Hormone fluctuations can trigger headaches in some individuals.
- Fluid retention: Leading to swelling in the legs, ankles, and hands.
- Weight gain: Although not universally experienced, weight gain is a potential side effect.
- Increased risk of blood clots: This is a more serious side effect and necessitates careful monitoring.
- Vaginal bleeding or spotting (if taking estrogen): This is usually less common in combination hormone therapy, which also contains progestin.
It’s crucial to remember that not all women experience these side effects, and the severity varies. Open communication with a healthcare provider is vital for discussing potential side effects and adjusting treatment plans as needed. The benefits of hormone therapy should always be weighed against the potential risks, considering the individual patient’s health status and personal preferences.
Q 18. Explain the difference between primary and secondary amenorrhea.
Amenorrhea refers to the absence of menstruation. Primary amenorrhea is defined as the absence of menarche (the first menstrual period) by age 15, or the absence of secondary sexual characteristics (breast development, pubic hair) by age 13. Secondary amenorrhea is the absence of menstruation for three or more consecutive cycles in a woman who previously had regular periods. Primary amenorrhea usually points towards an underlying anatomical or hormonal issue, such as Turner syndrome, uterine abnormalities, or hypothalamic amenorrhea. Secondary amenorrhea can have various causes, including pregnancy, breastfeeding, significant weight loss, intense exercise, stress, hormonal imbalances, or certain medical conditions.
For instance, a 16-year-old girl who has never had a period and shows no signs of puberty would be diagnosed with primary amenorrhea, requiring a thorough evaluation. In contrast, a 30-year-old woman who has consistently had regular periods but now experiences amenorrhea for several months requires a different investigation to exclude potential causes such as pregnancy, polycystic ovary syndrome (PCOS), or thyroid problems.
Q 19. How would you counsel a patient with a diagnosis of infertility?
Counseling a patient diagnosed with infertility requires sensitivity, empathy, and a comprehensive understanding of the emotional and psychological impact of this diagnosis. The first step involves validating their feelings, acknowledging the distress and grief that often accompany infertility. It’s important to provide a safe and non-judgmental space where the patient can express their concerns openly. Next, a thorough explanation of the diagnosis, including the possible causes and treatment options, is crucial. Discussing available options such as assisted reproductive technologies (ART), such as IVF, or lifestyle modifications is important, emphasizing shared decision-making. It is vital to address realistic expectations about the success rates of different treatments, managing hopes and avoiding false promises. The process also involves exploring coping mechanisms for stress and supporting their emotional well-being, potentially involving referrals to support groups or mental health professionals.
Imagine a couple struggling with infertility for years. They may be feeling a mix of disappointment, frustration, and isolation. Providing accurate information about their situation, potential treatment choices, and realistic success rates empowers them to make informed decisions and cope with the challenges they face. A referral to a support group could provide emotional support and connection with others experiencing similar circumstances.
Q 20. Discuss the impact of stress on vulvovaginal health.
Stress significantly impacts vulvovaginal health. Chronic stress alters the body’s hormonal balance, impacting vaginal lubrication, pH, and immune function. This can lead to an increased susceptibility to vaginal infections, such as yeast infections or bacterial vaginosis. Stress can also exacerbate existing vulvovaginal conditions like vulvodynia (vulvar pain) or lichen sclerosus (a skin condition causing vulvar itching and discomfort). Furthermore, stress can affect the pelvic floor muscles, leading to tension and pain, contributing to conditions like vaginismus (involuntary muscle spasms making intercourse painful) or pelvic floor dysfunction. Managing stress through techniques like yoga, meditation, deep breathing exercises, or therapy can positively impact vulvovaginal health.
For example, a woman experiencing high levels of work-related stress might notice increased vaginal dryness, recurrent yeast infections, and painful intercourse. Addressing the underlying stress through lifestyle modifications and therapeutic interventions could lead to significant improvements in her vulvovaginal health.
Q 21. What are the ethical considerations in managing patients with complex vulvar conditions?
Ethical considerations in managing patients with complex vulvar conditions are multifaceted. Maintaining patient autonomy and informed consent is paramount. Patients should fully understand their diagnoses, treatment options, potential risks, and benefits before making decisions. Confidentiality is crucial, ensuring that sensitive information is protected. Balancing the patient’s best interests with potential conflicts of interest, such as financial incentives related to specific treatments, requires careful navigation. Providing access to equitable care, irrespective of socioeconomic status, insurance coverage, or other factors, is essential. Transparency about the limitations of certain treatments and potential uncertainties is crucial in managing expectations. Finally, involving multidisciplinary teams when necessary, ensuring collaboration among specialists and access to appropriate support services, aligns with the ethical obligation of providing optimal patient care.
For example, a patient with a rare vulvar cancer requires careful consideration of treatment options. The physician must ensure that the patient fully understands her diagnosis, prognosis, and all available treatment modalities, including their risks and benefits, before making any decisions about her care. Involving other specialists, such as oncologists, surgeons, and psychologists, ensures a holistic approach and supports the patient’s best interests.
Q 22. Explain the importance of patient education in managing vulvar and vaginal disorders.
Patient education is paramount in managing vulvar and vaginal disorders. Empowered patients are better equipped to actively participate in their treatment, leading to improved outcomes and quality of life. This involves a multifaceted approach encompassing several key areas:
Understanding the Condition: Clearly explaining the diagnosis, its causes, and potential complications in terms the patient can easily grasp is crucial. For instance, explaining a yeast infection as an overgrowth of natural yeast rather than a sign of poor hygiene can alleviate unnecessary anxiety.
Treatment Options: Discussing various treatment modalities, including their benefits, risks, and potential side effects, enables patients to make informed decisions. This could involve explaining the difference between topical antifungal creams and oral medications for a yeast infection, outlining the pros and cons of each.
Lifestyle Modifications: Many vulvar and vaginal disorders benefit from lifestyle changes. This could include dietary adjustments, stress management techniques, or hygiene practices. For example, advising patients with recurrent urinary tract infections to increase their fluid intake and practice proper wiping techniques after urination.
Symptom Monitoring and Follow-up: Patients need to know what symptoms warrant immediate medical attention and when routine follow-up appointments are necessary. This proactive approach prevents complications and ensures timely intervention.
Addressing Emotional Well-being: Vulvar and vaginal disorders can significantly impact a patient’s self-esteem and body image. Addressing these emotional concerns through open communication and providing resources for support is essential.
Ultimately, effective patient education fosters a collaborative partnership between the healthcare provider and the patient, resulting in better disease management and improved patient outcomes.
Q 23. Discuss the role of imaging in diagnosing vulvar and vaginal conditions.
Imaging plays a vital, albeit often secondary, role in diagnosing vulvar and vaginal conditions. While a thorough history and physical examination are usually sufficient for initial assessment, imaging techniques can provide additional information and assist in differentiating between various conditions.
Ultrasound: Transvaginal ultrasound is commonly used to assess pelvic organ prolapse, identify masses, and evaluate the uterine and ovarian structures. It’s non-invasive and provides real-time images.
MRI: Magnetic resonance imaging offers superior soft tissue contrast and is particularly valuable in evaluating complex cases, such as vulvar lesions, deep infiltrating endometriosis, or assessing the extent of a prolapse.
CT Scan: Computed tomography scans are less frequently used but can be helpful in visualizing bony structures and assessing for the presence of fistulas or other complex anatomical abnormalities.
Colposcopy: This procedure involves using a magnifying instrument to visualize the cervix and vagina, particularly useful in evaluating abnormal cervical or vaginal cells detected during a Pap smear. Biopsies can be taken if needed.
The choice of imaging modality depends on the suspected diagnosis and clinical context. It’s important to remember that imaging alone rarely provides a definitive diagnosis; it needs to be integrated with clinical findings and other diagnostic tests for a comprehensive evaluation.
Q 24. Describe the surgical management options for vaginal prolapse.
Surgical management of vaginal prolapse addresses the underlying anatomical defects causing the prolapse. The choice of procedure depends on the type and severity of the prolapse, the patient’s age, overall health, and preferences. Several surgical approaches exist:
Anterior Colporrhaphy: Repairs the anterior vaginal wall prolapse (cystocele).
Posterior Colporrhaphy: Repairs the posterior vaginal wall prolapse (rectocele).
Sacrocolpopexy: A more extensive procedure that involves attaching the vaginal apex to the sacrum, providing strong support and suitable for severe prolapse.
Colpocleisis: A simpler procedure that closes the vaginal opening; it’s often chosen for older women who are not sexually active.
Uterine Suspension Procedures: If the uterus is also involved, procedures such as uterine suspension can be performed.
Mesh Repair: Synthetic mesh can be used to reinforce the repaired tissues and provide extra support, although its use is now debated more due to potential complications.
The choice of surgical technique requires careful consideration of individual patient factors and involves a detailed discussion between the surgeon and patient to make an informed decision. Post-operative care is crucial for successful healing and preventing recurrence.
Q 25. What are the long-term implications of untreated pelvic organ prolapse?
Untreated pelvic organ prolapse can lead to several long-term implications, significantly impacting a woman’s quality of life:
Increased Symptoms: Symptoms such as pelvic pressure, bulging, urinary and bowel dysfunction will likely worsen over time.
Urinary Tract Infections (UTIs): Incomplete bladder emptying due to prolapse can increase the risk of recurrent UTIs.
Bowel Dysfunction: Difficulty with bowel movements (constipation or fecal incontinence) can become more prevalent.
Pain: Chronic pelvic pain can develop due to the pressure and strain on pelvic structures.
Sexual Dysfunction: Prolapse can lead to discomfort during intercourse and decreased sexual function.
Psychological Impact: The physical symptoms and impact on daily activities can negatively affect a woman’s body image, self-esteem, and mental health.
Ulceration and Necrosis: In severe cases, the prolapsed tissue can become ulcerated or necrotic, leading to serious infections and complications.
Addressing prolapse early through conservative measures or surgery can prevent these long-term complications and maintain a better quality of life.
Q 26. Discuss the use of pessaries in managing pelvic organ prolapse.
Pessaries are non-surgical devices used to support pelvic organs and alleviate symptoms of pelvic organ prolapse. They are inserted into the vagina and provide mechanical support to the prolapsed tissues. Different types of pessaries exist, each designed to address specific types of prolapse.
Ring Pessary: Provides general support for vaginal prolapse.
Donut Pessary: Offers support for anterior and posterior wall prolapse.
Cube Pessary: Suitable for uterine prolapse.
Gemellus Pessary: Supports the vaginal apex.
Pessaries are generally well-tolerated but require regular follow-up visits to ensure proper fit and check for any complications, like erosion or infection. They aren’t suitable for all women. Factors such as vaginal anatomy, co-morbidities, and patient preference all influence their suitability. Pessaries are often considered a temporary or conservative treatment option until surgery, or if surgery is not desired.
Q 27. Explain the principles of pelvic floor muscle training (Kegel exercises).
Pelvic floor muscle training, commonly known as Kegel exercises, involves strengthening the muscles of the pelvic floor. These muscles support the bladder, uterus, and rectum. Strengthening these muscles can help improve urinary and bowel control, reduce prolapse symptoms, and enhance sexual function.
Identifying the Muscles: Imagine trying to stop the flow of urine midstream. The muscles you contract are the pelvic floor muscles. It’s crucial to correctly identify these muscles to perform Kegels effectively.
Correct Technique: Contract the pelvic floor muscles, holding the contraction for 3-5 seconds, then relax for the same amount of time. Avoid contracting your abdominal, buttock, or thigh muscles.
Consistency: Perform Kegel exercises regularly, several times a day, for optimal results. Aim for 3 sets of 10-15 repetitions.
Progression: As you gain strength, increase the duration of the contractions and the number of repetitions. This gradual progression avoids injury and maximizes benefit.
Biofeedback: Biofeedback techniques can help individuals learn to properly contract the pelvic floor muscles and monitor their progress.
While Kegel exercises are generally safe and effective, it’s always advisable to seek guidance from a healthcare professional or pelvic floor physical therapist to ensure proper technique and address any specific concerns or conditions.
Key Topics to Learn for Vulvar and Vaginal Disorders Interview
- Vulvovaginal Candidiasis: Diagnosis, differential diagnosis (bacterial vaginosis, trichomoniasis), treatment options, and patient education strategies.
- Bacterial Vaginosis: Understanding the microbial shift, clinical presentation, diagnostic methods (Amsel criteria, Nugent score), and appropriate management approaches, including consideration of antibiotic resistance.
- Vulvodynia: Differentiating between various types (provoked, unprovoked), exploring diagnostic pathways (including the role of physical examination and patient history), and outlining non-pharmacological and pharmacological management strategies.
- Trichomoniasis: Recognizing the clinical presentation, understanding diagnostic tests (microscopic examination, nucleic acid amplification tests), and implementing effective treatment protocols, emphasizing the importance of partner treatment.
- Lichen Sclerosus: Identifying the characteristic clinical features, discussing biopsy findings, and outlining treatment strategies, including topical corticosteroids and close monitoring for malignancy.
- Vestibulodynia: Understanding the pathophysiology, differentiating it from other vulvar pain conditions, and exploring various treatment approaches, such as physical therapy and local anesthetic agents.
- Pelvic Floor Dysfunction: Its impact on vulvar and vaginal health, and the integration of pelvic floor physical therapy into management plans.
- Menopausal Changes and their impact on Vulvovaginal Health: Understanding hormonal changes and their effects, and strategies for managing vulvovaginal atrophy.
- Psychosocial Aspects of Vulvar and Vaginal Disorders: The impact on quality of life, and the importance of addressing psychological factors in patient care.
- Applying evidence-based medicine to treatment decisions: Critically appraising clinical guidelines and research to inform practice.
Next Steps
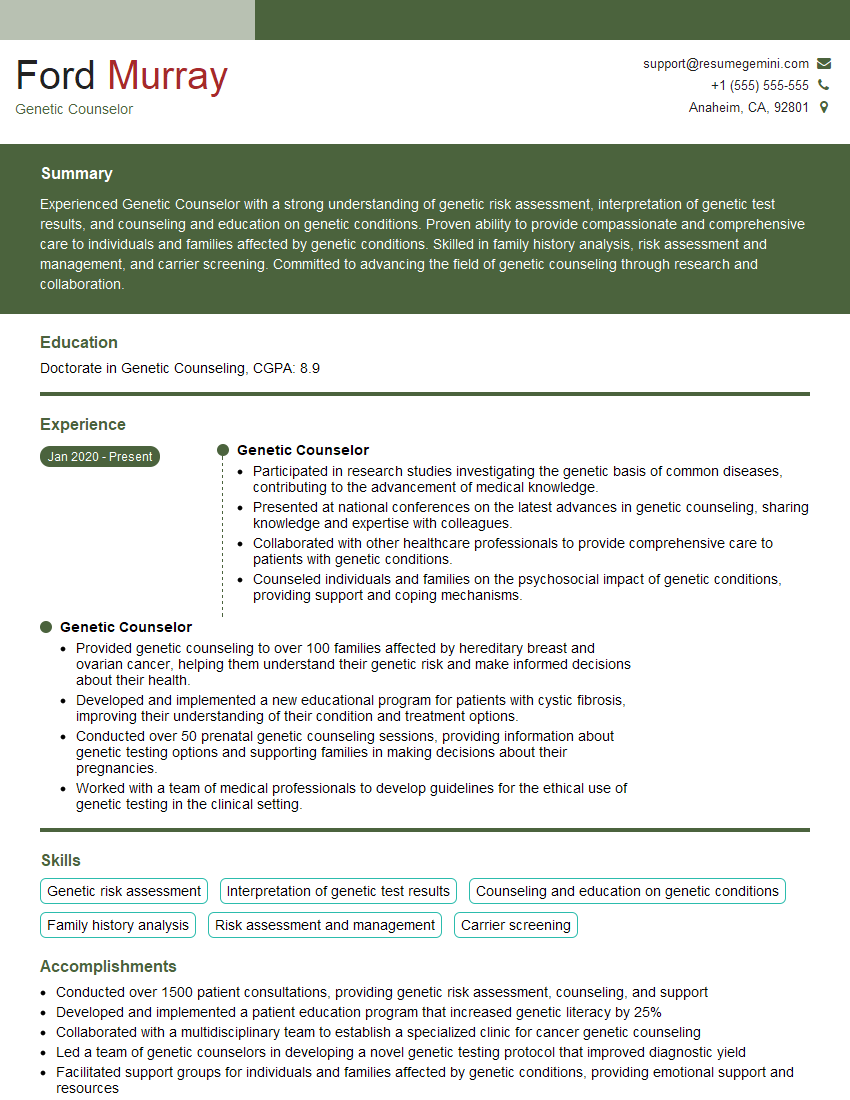
Mastering the intricacies of Vulvar and Vaginal Disorders is crucial for a successful career in women’s health. A strong understanding of these conditions demonstrates expertise and empathy, leading to increased opportunities and career advancement. To maximize your job prospects, invest time in creating a compelling, ATS-friendly resume that showcases your skills and experience. ResumeGemini is a trusted resource that can help you build a professional resume tailored to highlight your expertise in this specialized area. Examples of resumes tailored to Vulvar and Vaginal Disorders are available to provide further guidance.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.