The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Vulvar Surgery interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Vulvar Surgery Interview
Q 1. Describe your experience with vulvectomy procedures.
My experience with vulvectomy procedures encompasses a wide range of cases, from simple local excisions for benign conditions like condyloma acuminata to complex radical vulvectomies for advanced vulvar cancers. I’ve performed various types of vulvectomies, including partial, simple, and radical procedures, tailoring the approach to each patient’s unique anatomical features and the extent of the disease. For example, a patient with a small, well-defined vulvar lesion might require only a local excision, while a patient with extensive vulvar cancer might need a radical vulvectomy with inguinal lymph node dissection. Pre-operative planning, including imaging studies such as MRI and CT scans, is crucial to accurately assess the extent of disease and guide surgical strategy. Post-operative care involves meticulous wound management, pain control, and close monitoring for complications like infection or lymphocele formation. In all cases, patient education and psychological support are vital throughout the process. I am also experienced in reconstructive techniques to minimize cosmetic and functional deficits after vulvectomy, employing various flaps and grafts as needed.
Q 2. Explain your approach to managing Bartholin’s gland cysts.
My approach to managing Bartholin’s gland cysts is guided by the size, symptoms, and the patient’s preference. Small, asymptomatic cysts often require no intervention and can be monitored. For symptomatic cysts (pain, inflammation), I usually begin with conservative management, including warm sitz baths and antibiotics if there’s evidence of infection. For larger, recurrent, or symptomatic cysts, I generally recommend marsupialization, a minor surgical procedure where a small incision is made to drain the cyst and create an opening for drainage. This method effectively prevents recurrence in the majority of patients. Word catheter insertion is another option, but I prefer marsupialization because it’s less likely to cause stenosis. In cases of Bartholin’s gland abscess, incision and drainage is essential, followed by appropriate antibiotic therapy. I always discuss the various treatment options with the patient, ensuring they understand the risks and benefits of each procedure.
Q 3. How do you diagnose and treat vulvar vestibulitis?
Diagnosing vulvar vestibulitis relies on a careful history, physical examination, and often, exclusion of other conditions. The hallmark symptom is pain at the vestibule, the area surrounding the vaginal opening. Physical examination may reveal tenderness to palpation and sometimes erythema. Cotton swab testing can help identify localized tenderness. Diagnosing vestibulitis often involves ruling out other conditions like infections (bacterial vaginosis, candidiasis), vulvar lichen planus, or other dermatologic issues. Treatment options are primarily focused on pain management and can include topical anesthetics, corticosteroids, and amitriptyline. In some cases, vestibulectomy might be considered for severe, intractable cases that do not respond to conservative treatment. Regular follow-up is important to monitor pain levels and adjust treatment accordingly.
Q 4. Discuss your experience with vulvar cancer staging and treatment.
Vulvar cancer staging involves a multidisciplinary approach, combining clinical examination, imaging (MRI, CT), and pathology findings. The FIGO staging system is commonly used to classify the extent of the disease. Treatment strategies vary depending on the stage, histologic type, and patient factors. Early-stage vulvar cancers often are treated with surgical excision, often with sentinel lymph node biopsy. For advanced-stage cancers, more extensive surgery, such as radical vulvectomy with inguinal lymph node dissection, may be necessary. Adjuvant radiation therapy and chemotherapy are commonly used for locally advanced or metastatic disease. The specific treatment plan is determined in consultation with a multidisciplinary team, including gynecologic oncologists, radiation oncologists, and medical oncologists. Patient education and psychological support are crucial, as the diagnosis and treatment can be emotionally challenging.
Q 5. What are the different surgical techniques for vulvar lichen sclerosus?
Surgical techniques for vulvar lichen sclerosus are rarely indicated except in severe cases with significant stenosis or persistent symptoms unresponsive to medical therapy. The most common procedure is vulvoplasty which aims to restore normal anatomy. This involves excision of the affected skin and careful reconstruction to alleviate stenosis and improve comfort. The decision to pursue surgery is made cautiously, as the risks and benefits are carefully weighed against the potential for scarring and complications. The aim is to improve quality of life, but many patients respond well to topical therapies alone.
Q 6. Explain your approach to managing vulvar Paget’s disease.
Managing vulvar Paget’s disease involves a multidisciplinary approach focusing on complete surgical excision of the affected area. The goal is to achieve clear surgical margins, often confirmed by frozen section analysis during surgery. Because of its potential to recur, wide local excision with close monitoring is critical. In cases where complete surgical excision is challenging, adjuvant therapies such as radiation therapy may be considered. Regular follow-up is crucial to monitor for recurrence and ensure early detection of any relapse. I always emphasize the importance of ongoing vigilance and regular self-examination for patients with a history of vulvar Paget’s disease.
Q 7. How do you counsel patients on the risks and benefits of vulvar surgery?
Counseling patients on the risks and benefits of vulvar surgery is a crucial aspect of my practice. I begin by explaining the nature of the condition, the proposed surgical procedure, and the rationale behind the recommendation. We discuss the potential benefits, such as symptom relief, improved quality of life, and reduced risk of cancer recurrence (where applicable). I also meticulously explain the potential risks, including bleeding, infection, scarring, nerve damage, potential for complications with urinary or bowel function, and the need for potential further reconstructive surgery. We thoroughly explore alternative treatment options (when available) and their associated risks and benefits. I encourage patients to ask questions, express their concerns, and participate actively in the decision-making process. Providing detailed, individualized information helps patients make informed choices and feel empowered throughout their treatment journey.
Q 8. Describe your experience with sentinel lymph node biopsy in vulvar cancer.
Sentinel lymph node biopsy (SLNB) is a minimally invasive surgical technique used to determine whether vulvar cancer has spread to the regional lymph nodes. It’s crucial in staging the cancer and guiding treatment decisions. In my experience, SLNB involves injecting a radioactive tracer and/or blue dye around the tumor. These substances travel to the sentinel lymph nodes – the first lymph nodes to which cancer cells are likely to spread. We then identify and remove these nodes during surgery. Pathological examination of these nodes reveals whether cancer cells are present, significantly influencing the need for further lymph node dissection (a more extensive procedure).
The success of SLNB hinges on accurate tracer injection and meticulous node identification. False negative rates are a concern, so careful surgical technique and experienced pathology review are essential. I routinely use both radioisotope and blue dye to increase the sensitivity. If the sentinel nodes are negative, we avoid the morbidity associated with a complete lymph node dissection. Conversely, a positive result necessitates further surgical intervention.
For instance, I recently managed a patient with a clinically node-negative vulvar squamous cell carcinoma. SLNB revealed negative sentinel nodes, allowing us to avoid a more extensive lymphadenectomy, minimizing complications such as lymphedema. However, in another case, positive sentinel nodes led to an inguinal lymph node dissection, followed by adjuvant therapy.
Q 9. How do you manage postoperative complications after vulvar surgery?
Postoperative complications after vulvar surgery can range from minor to severe, requiring diligent management. Common complications include infection, hematoma (blood collection), seroma (fluid collection), wound dehiscence (wound separation), and lymphocele (lymph fluid collection). Pain management is a significant aspect of post-operative care, as discussed in the next question.
My approach involves meticulous surgical technique to minimize complications. Prophylactic antibiotics are used to reduce infection risk. Close monitoring of vital signs, wound inspection, and prompt intervention for any signs of infection or hematoma formation are crucial. Drainage tubes may be placed to prevent fluid accumulation. Seroma or lymphocele formation may require aspiration or surgical drainage.
Pain management, as mentioned, is central. We also pay close attention to nutritional support to aid healing and wound care to prevent infection and promote optimal tissue repair. Patient education on wound care, activity limitations, and recognizing signs of complications is paramount to successful post-operative recovery.
Q 10. What is your approach to pain management in vulvar surgery patients?
Pain management in vulvar surgery patients is a priority, recognizing that this area is highly sensitive. We employ a multimodal approach, combining pharmacological and non-pharmacological methods. Preemptive analgesia—pain medication before surgery—is vital, aiming to reduce postoperative pain intensity and opioid requirements.
Postoperatively, we utilize a combination of analgesics, including opioids (for severe pain, used sparingly and with careful monitoring for side effects), non-steroidal anti-inflammatory drugs (NSAIDs), and adjuvant analgesics such as gabapentinoids (for neuropathic pain). Regular assessment of pain levels is done using validated pain scales. Patient-controlled analgesia (PCA) pumps may be employed, giving patients greater control over their pain management.
Non-pharmacological approaches include ice packs, positioning strategies, and regular wound assessment. We also provide patient education on pain management strategies, including breathing exercises and relaxation techniques. In cases of persistent or intractable pain, referral to a pain management specialist is considered.
Q 11. Describe your experience with reconstructive surgery following vulvar cancer resection.
Reconstructive surgery following vulvar cancer resection is often necessary to restore function and improve quality of life. The extent of reconstruction depends on the size and location of the resection, and the patient’s overall health. The goals are to achieve adequate wound closure, preserve function (such as sexual function and continence), and minimize aesthetic deformity.
Techniques vary but may include local flaps (using nearby tissue), skin grafts, or free flaps (tissue transferred from a more distant site). Local flaps are often preferred for smaller defects, offering less morbidity. For larger defects, skin grafts may be necessary but carry a higher risk of graft failure. Free flaps, while more complex, provide better aesthetic results and function for extensive resections.
In practice, choosing the right reconstructive method involves careful consideration of the patient’s individual needs and surgical expertise. For example, a patient with a small vulvar lesion might only require a local advancement flap, whereas a patient with extensive resection may necessitate a more extensive reconstruction with a free flap. Post-operative monitoring includes wound assessment, functional evaluation, and psychological support.
Q 12. How do you utilize imaging modalities in the diagnosis and treatment of vulvar lesions?
Imaging modalities play a crucial role in the diagnosis and treatment of vulvar lesions. These include clinical examination, which remains the cornerstone; however, imaging techniques enhance our ability to characterize lesions and guide management decisions.
Ultrasound is commonly used for initial assessment, helping distinguish between superficial and deeper lesions, and estimating lesion size. MRI provides excellent soft tissue contrast and can be used to stage tumors, assess depth of invasion, and evaluate the extent of lymph node involvement. CT scans are less frequently used in vulvar cancer, but can be useful in evaluating distant metastases.
In cases where a specific diagnosis remains uncertain after other investigations, biopsy remains the gold standard. Imaging guides the biopsy, ensuring sampling of the most suspicious areas. This combined approach enables a more precise diagnosis, appropriate staging, and tailored treatment planning. For example, MRI might reveal the extent of involvement before a wide local excision is planned.
Q 13. What are the common types of vulvar cancer, and how do you approach each?
The most common type of vulvar cancer is squamous cell carcinoma, accounting for the majority of cases. Other less frequent types include melanoma, basal cell carcinoma, and adenocarcinoma. Our approach varies depending on the type and stage of cancer.
Squamous cell carcinoma is usually treated with wide local excision, aiming to remove the tumor with a margin of healthy tissue. SLNB or inguinal lymph node dissection is performed based on the clinical and pathological findings. Further treatment like radiation therapy or chemotherapy may be indicated depending on the stage.
Melanoma is managed differently, often requiring wider excision margins due to its aggressive nature. Sentinel lymph node biopsy is vital in staging and guiding adjuvant therapies like immunotherapy or targeted therapies. Basal cell carcinoma is generally treated with local excision, and rarely metastasizes. Adenocarcinoma management depends on the type and subtype and might involve similar approaches to squamous cell carcinoma.
Q 14. Explain your understanding of the lymphatic drainage of the vulva.
Understanding the lymphatic drainage of the vulva is crucial for staging and treating vulvar cancer, as the spread of cancer often follows lymphatic pathways. The vulva’s lymphatic drainage is complex, and not all parts drain in the same way. The anterior vulva drains primarily to the superficial inguinal lymph nodes, while the posterior vulva drains to the superficial and deep inguinal nodes. Some drainage can occur to the external iliac nodes.
The superficial inguinal lymph nodes are located in the groin, and are the first lymph nodes to which cancer cells from the vulva are likely to spread. The deep inguinal lymph nodes are located deeper within the groin. The external iliac nodes are located higher in the abdomen. Understanding this drainage pattern helps guide decisions on whether to perform SLNB or a complete inguinal lymph node dissection based on the location and stage of the tumor.
Clinically, knowledge of lymphatic drainage guides the planning and execution of SLNB and lymph node dissections. Failure to appreciate the variations in lymphatic drainage patterns can lead to inadequate surgical staging and suboptimal treatment.
Q 15. Discuss your experience with minimally invasive techniques in vulvar surgery.
Minimally invasive techniques in vulvar surgery aim to reduce trauma, improve cosmetic outcomes, and shorten recovery times compared to traditional open surgeries. My experience encompasses a wide range of these techniques, including laser surgery, electrosurgery, and the use of specialized instruments for precise dissection. For instance, we utilize CO2 laser vaporization for treating vulvar intraepithelial neoplasia (VIN) in early stages. This allows for precise ablation of the affected tissue with minimal bleeding and scarring. Another example is the use of laparoscopy for certain cases of vulvar cancer where lymph node dissection is required. This reduces the size of the incision, thereby minimizing postoperative pain and scarring. The choice of technique depends on several factors including the size, location and type of lesion, patient’s overall health, and personal preference.
We carefully assess each patient individually to determine the most appropriate minimally invasive approach. This involves thorough imaging studies (such as MRI and CT scans), biopsies to confirm the diagnosis and assess the extent of the disease, and considering the patient’s overall health and preferences.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage patients with recurrent vulvar cancer?
Managing recurrent vulvar cancer is a complex process requiring a multidisciplinary approach. The first step involves thorough staging to determine the extent of the recurrence – is it local, regional, or distant? This is done through imaging studies (CT, MRI, PET), biopsies, and sometimes exploratory surgery. Treatment strategies are tailored based on these findings. Local recurrences might be managed with re-excision surgery, sometimes with the addition of radiation therapy. Regional recurrence may necessitate pelvic lymph node dissection or more extensive surgery. For distant metastases, systemic therapies such as chemotherapy or targeted therapies are the primary treatment options. The psychological impact on patients is significant, and we actively involve oncology social workers and support groups to help them cope with the challenges.
For example, a patient with a small local recurrence after a previous wide local excision may be a candidate for a second resection, potentially with adjuvant radiation therapy to reduce the risk of further recurrence. However, a patient with distant metastases would be offered systemic therapies aimed at managing the disease and improving their quality of life.
Q 17. Describe your experience with the use of chemotherapy and radiation therapy in vulvar cancer.
Chemotherapy and radiation therapy play crucial roles in the management of vulvar cancer, often used in conjunction with surgery. Chemotherapy is predominantly used for advanced-stage vulvar cancer or as adjuvant therapy after surgery to reduce the risk of recurrence. Common chemotherapeutic agents include cisplatin, 5-fluorouracil, and carboplatin. Radiation therapy, either external beam or brachytherapy (internal radiation), is frequently used before surgery to downsize large tumors (neoadjuvant therapy), after surgery (adjuvant therapy) to eradicate any microscopic cancer cells, or as the primary treatment in patients who are not surgical candidates. The specific regimen depends on various factors including the stage of cancer, the patient’s overall health, and previous treatments. Careful monitoring of side effects is crucial, as both chemotherapy and radiation therapy can have significant toxicities.
For example, a patient with a large, locally advanced vulvar cancer may receive concurrent chemoradiotherapy to shrink the tumor before surgery to improve surgical outcomes. Conversely, a patient with early-stage vulvar cancer who undergoes surgery may receive adjuvant radiation therapy to minimize the chance of recurrence.
Q 18. How do you assess the surgical margins in vulvar cancer resection?
Accurate assessment of surgical margins is paramount in vulvar cancer surgery to ensure complete removal of the cancerous tissue and minimize the risk of recurrence. During surgery, we meticulously inspect the resected specimen, paying close attention to the edges of the excised tissue. Frozen section analysis, a rapid pathology technique, provides immediate assessment of the margins during the procedure. If positive margins (cancer cells at the edge of the resected tissue) are identified, further resection is performed to achieve negative margins. Permanent sections (formaldehyde-fixed, paraffin-embedded sections) provide a more definitive analysis post-surgery. Ink marking of the surgical margins is crucial to ensure proper orientation during pathological examination.
Imagine the surgical specimen as a cake. We meticulously examine the ‘crust’ (margins) to make sure there’s no ‘filling’ (cancer cells) left behind. If we find cancer cells on the edge, we need to take away a bit more of the cake until the edge is clean.
Q 19. What are the key considerations for postoperative follow-up care in vulvar surgery?
Postoperative follow-up care is critical for detecting any recurrence and managing potential complications. The frequency of follow-up visits varies depending on the stage of cancer and the surgical procedure. It typically involves regular physical examinations, imaging studies (MRI, CT scans), and blood tests. Early detection of recurrence is crucial for effective treatment. Pain management, wound care, and addressing any sexual dysfunction are also important aspects of postoperative care. We provide our patients with clear instructions on wound care, pain management strategies, and encourage them to contact us immediately if they experience any complications or concerning symptoms.
For instance, a patient with early-stage vulvar cancer may have follow-up appointments every 3-6 months for the first 2 years, then less frequently thereafter. Patients are educated on the importance of self-examination and reporting any unusual changes promptly.
Q 20. Describe your experience with different types of skin grafts in vulvar reconstruction.
Vulvar reconstruction after surgery can involve various types of skin grafts depending on the extent of the resection and the individual patient’s anatomy. Commonly used grafts include split-thickness skin grafts (STSG) and full-thickness skin grafts (FTSG). STSGs are thinner and easier to harvest, but they may have a less aesthetically pleasing outcome. FTSG offers better color and texture match, but requires a larger donor site. Other options include local flaps, which are more complex but offer superior results in terms of color match and texture. The choice of graft is individualized based on the defect size, location, and the patient’s overall health and preferences. Careful surgical planning and meticulous surgical technique are essential to ensure graft viability and successful reconstruction.
Choosing between a STSG and FTSG is similar to selecting the right type of paint for a wall. A STSG is like a basic coat of paint – functional but may not be as aesthetically pleasing. An FTSG is like a high-quality finish – a better match but requiring more effort.
Q 21. How do you address psychological and emotional needs of patients undergoing vulvar surgery?
Addressing the psychological and emotional needs of patients undergoing vulvar surgery is an integral part of our care. Vulvar surgery can have a profound impact on body image, sexuality, and self-esteem. We provide a supportive and empathetic environment where patients feel comfortable expressing their concerns. Open communication with the patient and their family is paramount. We often involve oncology social workers, psychologists, or sex therapists to provide additional support as needed. Patient education is crucial, explaining the procedure, potential complications, and realistic expectations regarding recovery. Support groups can also be invaluable, allowing patients to connect with others who share similar experiences.
For example, proactively addressing concerns about body image and sexual function through open dialogue and referral to appropriate specialists can significantly improve the patient’s emotional well-being during and after the treatment journey.
Q 22. Explain your knowledge of advanced surgical techniques for vulvar surgery.
Advanced surgical techniques in vulvar surgery aim to minimize scarring, preserve function, and achieve optimal oncological outcomes. This involves a nuanced understanding of vulvar anatomy and physiology.
Laser surgery: CO2 and Erbium lasers offer precise tissue ablation with minimal bleeding, ideal for treating condyloma acuminata, lichen sclerosus, and VIN. The precision allows for preservation of healthy tissue.
Minimally invasive techniques: Techniques like local excision with precise margins, including the use of surgical loupes and potentially sentinel lymph node biopsy, help minimize invasiveness compared to more extensive procedures.
Robotic surgery: Although not yet as widely adopted as in other fields, robotic assistance could potentially improve precision and dexterity in complex vulvar surgeries, particularly in deep infiltrating disease.
Advanced reconstruction: For significant resections, sophisticated reconstructive techniques such as skin grafts, flaps (e.g., labial, gracilis), and tissue expansion are crucial for restoring anatomical integrity and improving quality of life. The choice depends on the defect size and location.
For example, in a case of extensive vulvar cancer, we might utilize a combination of robotic-assisted dissection for precise tumor removal, followed by a gracilis myocutaneous flap for reconstruction.
Q 23. Discuss your understanding of the different types of vulvar dystrophies.
Vulvar dystrophies are a group of chronic inflammatory conditions affecting the vulvar skin. They are often grouped into lichen sclerosus, lichen planus, and other dystrophies (e.g., hyperplastic dystrophy, mixed dystrophy). Accurate diagnosis relies on clinical examination, histopathology, and sometimes additional tests to rule out other conditions.
Lichen sclerosus: Characterized by thinning of the epidermis, inflammation, and often white, porcelain-like patches. It’s associated with significant discomfort and can lead to scarring and stenosis (narrowing) of the vaginal introitus.
Lichen planus: Presents with purplish, flat-topped papules or plaques, often with an itchy and burning sensation. This condition can affect other mucosal sites.
Other dystrophies: This category encompasses a range of presentations, including hyperplastic dystrophy (thickening of the epithelium) and mixed dystrophies (combination of features).
Differentiating these conditions is crucial as their management differs. For instance, lichen sclerosus often responds well to topical corticosteroids, while lichen planus may require other therapies, potentially including immunosuppressants.
Q 24. How do you manage patients with vulvar disorders related to autoimmune diseases?
Managing vulvar disorders in the context of autoimmune diseases requires a multidisciplinary approach. The vulvar manifestations are often part of a broader systemic picture, and treatment needs to consider both local and systemic effects.
Careful history and examination: We thoroughly evaluate the patient’s medical history, focusing on the autoimmune disease and its management. A complete vulvar examination is essential, possibly including biopsies to confirm the diagnosis.
Collaboration with specialists: Close collaboration with rheumatologists, dermatologists, and other relevant specialists is crucial to coordinate treatment strategies. For example, a patient with lupus and vulvar lesions might require immunosuppressive medication managed by their rheumatologist while also needing topical treatments for the vulvar symptoms.
For example, a patient with vulvar lichen planus and a history of rheumatoid arthritis might require careful consideration of immunosuppressants to manage both conditions, balancing their efficacy against potential side effects.
Q 25. Describe your experience with the use of lasers in vulvar surgery.
Lasers have significantly advanced vulvar surgery. Their precision and ability to minimize bleeding make them particularly useful in several scenarios.
CO2 laser: Provides excellent hemostasis (stops bleeding) and precise vaporization, particularly suitable for treating condyloma acuminata, warts, and superficial lesions.
Erbium: YAG laser: Offers less thermal damage than CO2, making it useful for treating superficial lesions and improving cosmetic outcomes. It’s especially useful in cases of lichen sclerosus.
My experience shows that laser surgery often leads to faster healing times, reduced pain, and improved cosmetic results compared to traditional surgical techniques, particularly for superficial lesions. However, it’s important to note that lasers are not suitable for all vulvar conditions; deeper lesions may still require traditional excision.
Q 26. How do you approach the diagnosis and treatment of vulvar intraepithelial neoplasia (VIN)?
Vulvar intraepithelial neoplasia (VIN) is a precancerous condition characterized by abnormal cell growth in the vulvar epithelium. Diagnosis and treatment require a multi-pronged approach.
Diagnosis: Begins with a thorough history and physical examination. Colposcopy, a magnified examination of the vulva, helps identify suspicious areas. Biopsy is crucial to confirm the diagnosis and determine the severity (VIN 1, VIN 2, VIN 3).
Treatment: Varies based on the severity and extent of VIN. Options include:
- Wide local excision: Removal of the affected tissue with a margin of healthy tissue.
- Laser ablation: Precise removal of the abnormal tissue using lasers (CO2 or Erbium).
- Topical treatments: Certain topical therapies can be used for mild VIN, but their efficacy and the risk of recurrence are considerations.
A crucial aspect is regular follow-up to monitor for recurrence or progression to invasive cancer. The treatment strategy is individualized, considering factors such as the patient’s age, extent of disease, and desire for fertility.
Q 27. What are the indications and contraindications for various vulvar surgical procedures?
The choice of vulvar surgical procedure depends on many factors, including the specific condition, its extent, the patient’s age and overall health, and her desires for future fertility.
Indications:
- Vulvar cancer: Surgical excision, with lymph node dissection if indicated.
- VIN: Wide local excision, laser ablation, or topical therapy.
- Benign vulvar lesions: Local excision, laser treatment.
- Lichen sclerosus with severe stenosis: Vulvoplasty.
Contraindications:
- Severe medical comorbidities that increase surgical risk.
- Extensive disease that is not surgically resectable.
- Patient refusal of surgery.
For example, a patient with early-stage vulvar cancer might undergo a wide local excision with sentinel lymph node biopsy, whereas a patient with extensive disease might require more extensive surgery including lymph node dissection and potential reconstructive procedures.
Q 28. Describe your experience collaborating with other specialists in the management of complex vulvar cases.
Managing complex vulvar cases necessitates a multidisciplinary approach. Effective collaboration is paramount for optimal patient care.
Oncologists: Consultation with medical and radiation oncologists is essential for cases involving vulvar cancer, particularly for advanced stages or treatment planning.
Dermatologists: Their expertise is invaluable in the diagnosis and management of inflammatory conditions like lichen sclerosus and lichen planus.
Pathologists: Accurate diagnosis depends on their meticulous analysis of biopsy specimens to ensure appropriate treatment strategies.
Radiologists: Imaging studies like MRI and CT scans are crucial in staging cancer and guiding surgical planning.
Plastic surgeons/Reconstructive surgeons: Their input is critical for complex cases requiring significant surgical reconstruction after tumor removal.
I routinely collaborate with these specialists, ensuring comprehensive care, clear communication, and a cohesive treatment plan tailored to the individual patient’s needs.
Key Topics to Learn for Vulvar Surgery Interview
- Vulvar Anatomy and Physiology: Thorough understanding of the normal and variant anatomy, including blood supply, lymphatic drainage, and innervation. Consider the implications of anatomical variations in surgical planning.
- Benign Vulvar Diseases: Diagnosis and management of common conditions like vulvar vestibulitis, lichen sclerosus, condyloma acuminata, and Bartholin’s gland cysts. Focus on differential diagnosis and surgical techniques.
- Malignant Vulvar Diseases: Staging, diagnostic workup, and surgical management of vulvar cancers (e.g., squamous cell carcinoma, melanoma). Understand the principles of radical vulvectomy and lymphadenectomy.
- Surgical Techniques: Mastering various surgical approaches, including local excision, wide local excision, laser surgery, and reconstructive techniques. Practice explaining the rationale behind choosing specific surgical techniques for different cases.
- Post-operative Care and Complications: Develop a comprehensive understanding of post-operative management, including pain control, wound care, and the recognition and management of potential complications (e.g., infection, bleeding, fistula formation).
- Advanced Imaging and Pathology: Familiarity with imaging modalities used in vulvar surgery (e.g., ultrasound, MRI) and interpretation of vulvar pathology reports. Be prepared to discuss your approach to interpreting imaging findings in clinical scenarios.
- Ethical and Legal Considerations: Understanding informed consent, patient autonomy, and the ethical dilemmas specific to vulvar surgery. Be ready to discuss these aspects in a professional and thoughtful manner.
Next Steps
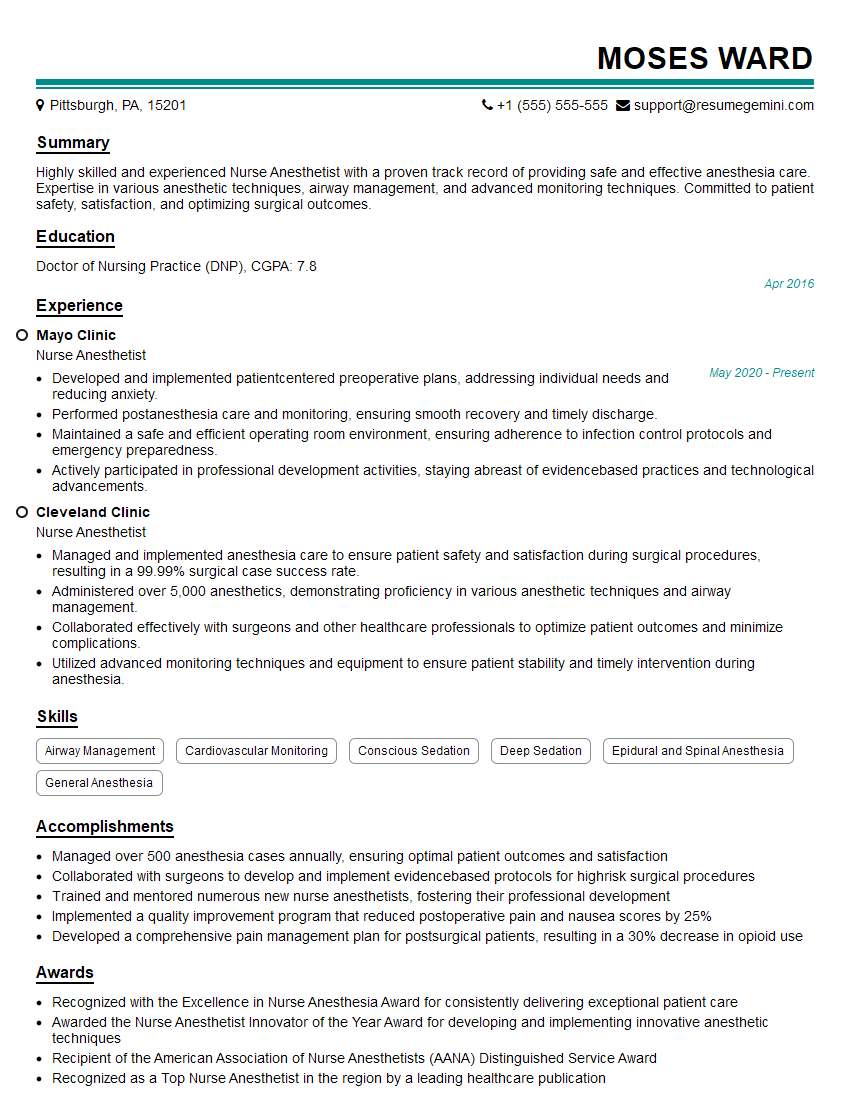
Mastering vulvar surgery is crucial for a successful and rewarding career in gynecology or a related subspecialty. A strong foundation in this area demonstrates your expertise and commitment to providing excellent patient care. To enhance your job prospects, create an ATS-friendly resume that effectively showcases your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to vulvar surgery to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.