Unlock your full potential by mastering the most common Diagnostic Ultrasound interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Diagnostic Ultrasound Interview
Q 1. Explain the principles of ultrasound imaging.
Ultrasound imaging, also known as sonography, relies on the principle of echolocation, similar to how bats navigate. A transducer sends high-frequency sound waves (ultrasound) into the body. These waves bounce off different tissues and organs, creating echoes. The transducer then receives these echoes, and a computer processes them to create an image on a screen. The image displays variations in tissue density – denser tissues reflect more sound waves, appearing brighter on the image, while less dense tissues reflect fewer waves and appear darker.
Think of it like shining a flashlight in a dark room. Hard objects like walls will reflect more light back to you, while soft objects like curtains will absorb more and reflect less. Ultrasound works on a similar principle, but instead of light, it uses sound waves and instead of your eyes, a computer processes the returning echoes to construct the image.
Q 2. Describe the different types of ultrasound transducers and their applications.
Ultrasound transducers are essentially specialized microphones and speakers that convert electrical energy into ultrasound waves and vice versa. There are several types:
- Linear Transducers: These produce a rectangular image with excellent resolution, ideal for superficial structures like muscles, tendons, and breasts. Think of a high-resolution photograph; you can see fine details.
- Curvilinear (Convex) Transducers: These have a curved surface, creating a wider field of view. They are often used for abdominal, pelvic, and cardiac imaging, allowing for visualization of larger areas.
- Phased Array Transducers: These use multiple small crystals to electronically steer the beam, enabling the creation of images from various angles without physically moving the transducer. They are frequently used for cardiac imaging and are particularly valuable in examining areas that are difficult to access.
- Endocavitary Transducers: These transducers are designed for internal use, such as transvaginal or transrectal probes for gynecological or prostate examinations. These provide very high-resolution images of internal structures.
- Intraoperative Transducers: These smaller transducers are used during surgical procedures to provide real-time imaging guidance.
The choice of transducer depends on the specific organ or area being examined and the desired level of detail. For example, a linear transducer is ideal for evaluating superficial structures, while a curvilinear transducer is better suited for larger organs like the liver or kidneys.
Q 3. What are the artifacts commonly encountered in ultrasound imaging, and how are they identified and mitigated?
Artifacts are inaccuracies or distortions in the ultrasound image that can mislead the interpretation. Several common artifacts include:
- Acoustic Shadowing: This occurs behind highly reflective structures (like stones or bones), creating a dark shadow area. It’s important to recognize shadowing as it may obscure underlying structures.
- Acoustic Enhancement: The opposite of shadowing; this appears as a brighter area behind fluid-filled structures (like cysts). This is because sound waves travel faster through fluid, resulting in increased reflection.
- Refraction: Bending of sound waves when passing through interfaces of different acoustic impedances, leading to inaccurate image positioning.
- Reverberation: Multiple reflections of sound waves between two strong reflectors (e.g., air and tissue interfaces), creating repeating parallel lines.
- Mirror Image: A duplication of a structure caused by reflection off a strong reflector (e.g., diaphragm).
Identifying artifacts requires experience and knowledge of ultrasound physics. Careful attention to the image’s characteristics, combined with correlation with clinical information, is key. Mitigating artifacts often involves changing transducer frequency, adjusting the gain settings, or changing the scanning angle.
Q 4. Explain the acoustic window concept in ultrasound.
The acoustic window refers to the area of the body where ultrasound waves can easily pass through to reach the target organ or structure. This is crucial because bone and air significantly impede the passage of sound waves. Therefore, ideal acoustic windows are areas with minimal air or bone between the transducer and the target.
For example, in an abdominal ultrasound, the intercostal spaces (between the ribs) offer an acoustic window to visualize the liver or spleen. Similarly, the bladder provides a good window for visualizing pelvic organs. Choosing the appropriate acoustic window is crucial for obtaining optimal images and accurate assessment.
Q 5. How do you adjust the gain, TGC, and depth settings during an ultrasound exam?
These controls are crucial for image optimization:
- Gain: This overall amplifies the returning echoes. Increasing the gain brightens the entire image, making weaker echoes more visible. However, excessive gain can introduce noise. I usually adjust the gain to make structures visible without excessive noise.
- Time Gain Compensation (TGC): This allows for differential amplification at different depths. It’s like adjusting the brightness at different levels of the image to compensate for the attenuation of sound waves as they travel deeper into tissue. For example, in abdominal scans, the TGC is often increased in the deeper portions to compensate for the attenuation of ultrasound energy.
- Depth: This setting controls the imaging depth. The depth is set based on the location and size of the structure of interest. For example, I use a shallow depth for thyroid imaging and greater depths for abdominal imaging.
Optimizing these settings is a critical skill requiring experience and practice; it’s an iterative process where I adjust gain and TGC to achieve optimal visualization of the organ of interest at the selected depth.
Q 6. Describe the steps involved in performing an abdominal ultrasound.
Performing an abdominal ultrasound involves several steps:
- Patient Preparation: The patient should have fasted for at least 6-8 hours before the exam to minimize bowel gas, which can interfere with image quality.
- Positioning: The patient is usually positioned supine (lying on their back). Different positions may be used to optimize visualization of specific organs.
- Transducer Selection: A curvilinear transducer is typically used due to its wider field of view.
- Scanning Technique: The transducer is systematically moved across the abdomen, using gentle pressure to maintain contact. Various scanning planes (longitudinal and transverse) are used to visualize the organs completely.
- Image Acquisition: Images are acquired of the liver, gallbladder, spleen, kidneys, pancreas, aorta, and inferior vena cava. Doppler imaging may also be used to assess blood flow.
- Image Interpretation: The images are carefully examined for any abnormalities in size, shape, texture, or blood flow.
- Report Generation: A written report summarizing the findings is generated for the referring physician.
Q 7. How do you prepare a patient for a transvaginal ultrasound?
Patient preparation for a transvaginal ultrasound is straightforward but essential for patient comfort and optimal image quality:
- Empty Bladder: A full bladder can interfere with visualization of pelvic organs. Patients are usually instructed to void before the exam.
- Optional: A vaginal exam or speculum insertion may be performed, but this is not always necessary, and the ultrasound can be done directly with the probe.
- Lubricating Gel: A sterile gel is applied to the transducer to facilitate smooth insertion and optimal sound wave transmission.
- Positioning: Patients usually lie on their back with their knees bent or in the lithotomy position. The examiner uses gentle pressure during probe insertion.
It’s crucial to explain the procedure thoroughly to the patient, ensuring comfort and alleviating any anxiety. Maintaining patient dignity and providing reassurance throughout the exam is paramount.
Q 8. Explain the Doppler effect and its use in ultrasound.
The Doppler effect is the change in frequency of a wave (in this case, ultrasound) for an observer moving relative to its source. Imagine a speeding ambulance: the siren’s pitch is higher as it approaches you (frequency increases) and lower as it moves away (frequency decreases). In ultrasound, this principle allows us to measure the speed and direction of blood flow within vessels.
In ultrasound, the transducer emits sound waves. When these waves encounter moving red blood cells, the reflected waves’ frequency changes. This frequency shift, or Doppler shift, is then processed by the machine to produce a Doppler signal. The greater the shift, the faster the blood flow. The direction of the shift indicates whether the blood is flowing towards or away from the transducer.
This is crucial for diagnosing conditions like vascular stenosis (narrowing of blood vessels) where a high velocity of flow is observed at the stenosis point. It also helps visualize blood clots and assess the patency (openness) of arteries and veins.
Q 9. Describe the difference between pulsed-wave and continuous-wave Doppler.
Both pulsed-wave (PW) and continuous-wave (CW) Doppler utilize the Doppler effect to measure blood flow, but they differ significantly in their techniques and applications.
- Pulsed-Wave Doppler: Uses short bursts of ultrasound waves, allowing the machine to determine both the velocity and the depth of the blood flow. It provides range resolution, meaning we know where in the body the measured velocity is coming from. However, its ability to accurately measure high velocities is limited by the pulse repetition frequency (PRF). Imagine trying to count fast-moving cars; if your counting rate is too low, you’ll miss some cars.
- Continuous-Wave Doppler: Continuously transmits and receives ultrasound waves. It’s excellent for measuring high velocities accurately because it has no PRF limitations; it’s like having a much faster car-counting mechanism. However, it lacks range resolution; we know the velocity but not the exact location. This is like knowing how fast the cars are going but not knowing which lane they’re in.
Therefore, PW Doppler is preferred for most vascular assessments where both velocity and depth information are needed, while CW Doppler is better suited for measuring very high velocities, such as in severe stenosis or assessing the direction of flow in specific regions.
Q 10. What are the safety precautions associated with ultrasound imaging?
While ultrasound is considered a safe imaging modality, several precautions must be observed. The primary concern is the potential for bioeffects associated with prolonged exposure to high-intensity ultrasound. This is why we always adhere to the ALARA principle – As Low As Reasonably Achievable.
- Minimizing Exposure Time: We perform only necessary scans and keep the exposure duration as short as possible.
- Using Appropriate Acoustic Output Power: We adjust the output power (intensity) to the minimum necessary to achieve a diagnostic image quality. Higher output power means higher risk.
- Thermal and Mechanical Indices: Modern ultrasound machines provide thermal index (TI) and mechanical index (MI) measurements, indicating the risk of heating (thermal) or cavitation (mechanical) effects. We monitor these indices and adjust parameters to keep them within safe limits.
- Focused Beams: Using a focused beam concentrates the ultrasound energy, reducing the exposure to surrounding tissue.
- Patient Positioning and Technique: Proper patient positioning and scan technique minimize the time needed for acquisition of appropriate images.
- Avoidance of unnecessary repeat scans:Careful optimization of settings avoids unnecessary scanning and repeats.
For pregnant patients, special considerations are given to minimize exposure and potential risk to the fetus, adhering to guidelines and recommendations provided by relevant organizations.
Q 11. How do you identify and document pathology findings in an ultrasound report?
Documenting pathology findings in an ultrasound report requires a structured and precise approach. It involves a systematic description of the location, size, shape, and characteristics of any abnormality.
For example, a description of a liver lesion might include:
- Location: “A hypoechoic (darker than normal) lesion is identified in segment VII of the right lobe of the liver.”
- Size: “The lesion measures 2.5 cm in its longest dimension.”
- Shape: “The lesion is well-circumscribed and round.”
- Echogenicity: “The lesion shows hypoechoic internal echoes with posterior acoustic enhancement (brighter area behind the lesion).”
- Vascularity (if Doppler is used): “Color Doppler demonstrates no internal vascularity.”
The report should also include a summary of the findings, differential diagnoses (possible explanations for the findings), and recommendations for further investigations, if needed. Standardized terminology and reporting formats are employed to ensure clarity and consistency across different ultrasound facilities.
High-quality images are crucial and should be included in the report as evidence of the described findings.
Q 12. Explain the limitations of ultrasound imaging.
Ultrasound imaging, while powerful, has limitations. Its efficacy depends on the acoustic properties of the tissues being imaged and the skill of the operator. Here are key limitations:
- Gas Interference: Air or gas in the intestines or lungs significantly attenuates (reduces the intensity of) the ultrasound waves, creating shadowing and making visualization of underlying structures difficult.
- Bone Interference: Bone also reflects and attenuates ultrasound, limiting visualization of structures behind it. This is why obtaining detailed images of the brain is challenging using ultrasound unless a transcranial approach is applied.
- Operator Dependence: Image quality and the diagnostic accuracy strongly depend on the operator’s expertise. This includes expertise in technical aspects of the ultrasound machine, understanding the different modalities and how to apply them in different clinical scenarios.
- Limited Penetration: Ultrasound doesn’t penetrate deep into the body as effectively as other imaging modalities, such as CT or MRI.
- Inability to image certain tissues effectively: Visualization of some tissues can be challenging due to their similar acoustic characteristics.
Understanding these limitations allows radiologists and sonographers to choose the most appropriate imaging modality for each clinical question and to interpret results cautiously.
Q 13. Describe your experience with different ultrasound modalities (e.g., 2D, M-mode, Doppler).
Throughout my career, I have extensive experience with various ultrasound modalities. My expertise encompasses 2D imaging, M-mode, and Doppler techniques, all of which are essential tools in my daily practice.
- 2D (grayscale) Imaging: This is the most common mode, providing anatomical information in a two-dimensional plane. I use this extensively for evaluating the size, shape, and texture of organs and identifying abnormalities.
- M-mode (motion mode) Imaging: M-mode shows the movement of structures over time, providing information about cardiac function or fetal heart rate. I frequently use this for cardiac assessments.
- Doppler Imaging: I’m proficient in using both pulsed-wave and continuous-wave Doppler to assess blood flow in various vessels. This is critical for diagnosing vascular diseases and guiding interventions.
I have applied these techniques across a wide range of clinical applications, including abdominal, vascular, obstetric, gynecological, and musculoskeletal examinations. My experience includes both routine examinations and complex cases requiring advanced techniques.
Q 14. How do you ensure the quality of ultrasound images?
Ensuring the quality of ultrasound images is crucial for accurate diagnosis. It involves a multi-faceted approach, encompassing both technical aspects and procedural practices.
- Proper Transducer Selection: Choosing the right transducer frequency for the specific anatomical region is key. Higher frequencies provide better resolution for superficial structures, while lower frequencies are better for deeper penetration.
- Optimal Gain and TGC Adjustments: Correct adjustment of gain (overall amplification) and time-gain compensation (TGC, amplifying signals at different depths) optimizes the image brightness and contrast, allowing for better visualization of details.
- Appropriate Focusing and Depth Settings: Adjusting the focus and depth settings to center the area of interest ensures that the image is sharpest and most detailed.
- Proper Patient Preparation: Adequate patient preparation, such as emptying the bladder or using bowel cleansing solutions, can greatly improve image quality by eliminating interference from gas or other substances.
- Image Optimization Techniques: Employing advanced imaging techniques such as harmonic imaging, compound imaging, or speckle reduction technology can improve image quality, particularly when encountering challenging circumstances.
- Quality Assurance Programs: Regular participation in quality assurance programs including phantom studies, and attending continuing medical education sessions help to maintain consistently high standards of image quality.
Regular calibration and maintenance of the ultrasound equipment are also essential to ensure optimal performance and image quality.
Q 15. How do you handle challenging or difficult ultrasound exams?
Challenging ultrasound exams often arise from factors like patient body habitus (obesity), bowel gas obscuring structures, or the presence of scar tissue. My approach is systematic and involves a multi-pronged strategy. First, I carefully assess the patient’s history and clinical indication for the exam to tailor my technique. For example, if I’m facing difficulty visualizing the gallbladder due to bowel gas, I might have the patient change positions or use a harmonic imaging technique to penetrate deeper. If significant obesity is hindering visualization, I may employ higher-frequency transducers to improve resolution in shallower areas, focusing on optimizing the acoustic window to achieve the best possible images. If the challenge is related to patient movement, I may employ techniques like asking them to hold their breath or repositioning them.
Secondly, I utilize advanced imaging techniques such as compound imaging, spatial compounding, or contrast-enhanced ultrasound when appropriate. If I encounter significant limitations despite these techniques, I thoroughly document the limitations in my report and communicate these findings clearly to the referring physician, possibly suggesting alternative imaging modalities like CT or MRI if necessary. This collaborative approach ensures optimal patient care. I also consider my own limitations, and if I feel I am not able to adequately perform the exam, I will promptly consult a more senior colleague for assistance.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are your strategies for communicating with patients during an ultrasound exam?
Effective communication is paramount in ultrasound. I start by introducing myself and explaining the procedure in simple, non-medical terms, addressing any concerns or anxieties the patient might have. For example, I explain what the ultrasound will show and what it won’t. I emphasize the importance of staying still during parts of the exam and reassure them that the ultrasound itself is painless. Maintaining eye contact and a calm, reassuring tone is crucial. I actively listen to their questions and provide clear, honest answers.
Throughout the exam, I maintain a conversational tone, updating them on my progress. I try to build rapport by acknowledging any discomfort they may experience and providing breaks when needed. After the exam, I summarize my findings in clear, simple language, without using medical jargon. If the findings are complex, I prepare a concise, written summary for the referring physician and discuss the preliminary findings with the patient if appropriate and consistent with hospital guidelines.
Q 17. Describe your experience with PACS systems.
I have extensive experience working with Picture Archiving and Communication Systems (PACS). My experience includes retrieving, reviewing, and interpreting ultrasound images from the PACS, dictating reports directly into the system, using PACS tools to manage my workflow and measure distances on images, and utilizing advanced PACS functionalities for image manipulation and analysis. This expertise is crucial for streamlining the workflow, improving image management, ensuring efficient access to images from multiple modalities, and minimizing administrative tasks. I’m proficient in using various PACS interfaces and understand the importance of maintaining image security and compliance with HIPAA regulations.
For example, I’m familiar with using the PACS to retrieve prior images for comparison in longitudinal studies, such as monitoring fetal growth during pregnancy, or tracking the size of a mass over time. The ability to access images and reports from previous exams immediately within the PACS provides an invaluable advantage in delivering effective patient care.
Q 18. How do you maintain and troubleshoot ultrasound equipment?
Maintaining ultrasound equipment involves a combination of preventative measures and prompt troubleshooting. Preventative maintenance includes regular cleaning and disinfection of the transducer and machine, checking cable connections and ensuring optimal system settings. We also adhere to a regular schedule for preventative maintenance contracts provided by the manufacturer, including periodic servicing and calibration.
Troubleshooting is an essential skill. When encountering equipment issues, I start by systematically checking obvious things such as power supply, transducer connections, and gel application. If the problem persists, I consult the system’s troubleshooting manual, utilize built-in diagnostic tools and then, if the problem remains, contact biomedical engineering for more advanced repairs. For example, if I encounter an issue with image quality, I would first check the transducer frequency, TGC (Time Gain Compensation) settings and system settings. Learning to recognize subtle patterns associated with malfunctioning systems is crucial. Accurate record keeping of maintenance and repair activities is vital for safety and regulatory compliance.
Q 19. Explain the role of sonography in various medical specialties (e.g., cardiology, obstetrics).
Sonography plays a crucial role across many medical specialties. In cardiology, echocardiography uses ultrasound to assess the structure and function of the heart, identifying conditions such as valvular disease, cardiomyopathy, and congenital heart defects. In obstetrics, ultrasound is essential for monitoring fetal growth and development, detecting abnormalities, and guiding procedures like amniocentesis.
In abdominal radiology, ultrasound is used to image the liver, gallbladder, kidneys, pancreas, and spleen, helping diagnose various conditions like gallstones, liver cirrhosis, and kidney stones. In vascular surgery, Doppler ultrasound evaluates blood flow in arteries and veins, aiding in the diagnosis of deep vein thrombosis (DVT) and peripheral arterial disease (PAD). In musculoskeletal imaging, musculoskeletal ultrasound is increasingly used to evaluate tendons, ligaments, muscles and joints.
Essentially, ultrasound’s versatility stems from its non-invasive nature, real-time imaging capabilities, and affordability, making it a cornerstone of many diagnostic workflows.
Q 20. How do you stay updated on the latest advancements in ultrasound technology?
Staying current in ultrasound requires a multi-faceted approach. I regularly attend professional conferences such as those hosted by the American Institute of Ultrasound in Medicine (AIUM) and the Society of Diagnostic Medical Sonography (SDMS). These provide opportunities to learn about the newest technologies and techniques. I also actively participate in continuing medical education (CME) courses, both in-person and online, focusing on advancements in specific areas of interest, like elastography or contrast-enhanced ultrasound.
Furthermore, I read peer-reviewed journals like the Journal of Ultrasound in Medicine and Radiology to stay abreast of the latest research findings. Online resources, professional societies’ websites, and manufacturer training materials also provide valuable information. Engaging in discussions with colleagues and sharing experiences is vital for professional development. Continuous learning ensures I provide the best possible patient care using state-of-the-art techniques and technologies.
Q 21. Describe your experience with different types of ultrasound contrast agents.
Ultrasound contrast agents are used to enhance the visualization of blood vessels or tissue structures. I have experience using different types, primarily microbubble-based agents. These microbubbles are injected intravenously and selectively accumulate in certain tissues, increasing the reflectivity of ultrasound waves and improving image contrast.
Examples include agents like SonoVue (sulfur hexafluoride microbubbles) which are commonly used in cardiac and liver imaging. The choice of contrast agent and the technique used depends heavily on the specific clinical application. For instance, contrast-enhanced ultrasound (CEUS) of the liver might use a different agent and approach compared to a contrast echocardiogram. I am trained in properly administering the contrast agents, understanding their safety profiles, and recognizing potential adverse effects, always adhering to strict protocols to ensure patient safety. Proper training and protocol adherence are essential to make informed decisions about the appropriate use and administration of ultrasound contrast agents.
Q 22. What is your understanding of elastography and its applications?
Elastography is a relatively new ultrasound technique that assesses the stiffness or elasticity of tissues. It works on the principle that diseased tissues often have different stiffness compared to healthy tissues. This difference in stiffness is measured by applying either a shear wave (shear wave elastography or SWE) or compression (strain elastography) to the tissue and analyzing how it propagates or deforms.
Applications: Elastography has found significant applications in several areas, notably in:
- Liver disease: Differentiating between benign and malignant liver lesions, assessing the severity of liver fibrosis (scarring) in conditions like chronic hepatitis C and non-alcoholic fatty liver disease (NAFLD).
- Breast imaging: Helping to distinguish between benign and malignant breast masses, improving the accuracy of breast cancer detection.
- Thyroid nodules: Characterizing thyroid nodules and assisting in the decision of whether biopsy is necessary.
- Musculoskeletal imaging: Assessing muscle and tendon injuries, identifying areas of fibrosis or scarring.
For example, in liver assessment, a stiff area detected by elastography could suggest the presence of a malignancy or significant fibrosis, requiring further investigation. The quantitative nature of elastography provides valuable objective data supplementing conventional ultrasound findings.
Q 23. How do you differentiate between benign and malignant findings on ultrasound?
Differentiating between benign and malignant findings on ultrasound relies on a combination of features, and no single characteristic guarantees a definitive diagnosis. It requires a holistic approach integrating imaging findings with clinical history and other investigations (like blood tests or biopsies).
Features suggesting malignancy:
- Irregular borders: Malignant lesions often have irregular, poorly defined margins, unlike benign lesions which tend to have smooth, well-defined borders.
- Hypoechogenicity: Malignant lesions frequently appear darker (hypoechoic) on ultrasound than surrounding tissue.
- Vascularity: Malignant lesions often demonstrate increased blood flow, which can be visualized using color Doppler imaging. This increased vascularity may manifest as internal vascularity or a marked increase in peripheral vascularity.
- Microcalcifications: Tiny calcium deposits are often seen in malignant breast lesions.
- Size and growth: Rapid growth or large size can raise concerns. However, this should always be taken in context with the specific organ and tissue.
Features suggesting benignity:
- Smooth borders: Well-defined and smooth margins.
- Homogenous echotexture: Uniform appearance throughout the lesion.
- Absence of vascularity: Minimal or no internal blood flow.
- Characteristic features: Some benign lesions have specific ultrasound appearances (e.g., simple cysts in the breast often appear anechoic – fluid filled with no internal echoes).
It’s crucial to remember that these are guidelines, not absolute rules. A definitive diagnosis often requires a biopsy and histopathological examination.
Q 24. Describe your experience with image-guided procedures.
I have extensive experience in performing and assisting with various image-guided procedures using ultrasound. This includes:
- Biopsies: Guiding needles to obtain tissue samples for pathological examination from organs such as the liver, kidney, thyroid, breast, and lymph nodes.
- Drainage procedures: Using ultrasound guidance to place drains to evacuate fluid collections like abscesses or hematomas.
- Injections: Guiding injections into joints (e.g., for steroid injections), masses, or other targeted areas.
- Ablation procedures: Assisting in procedures like radiofrequency ablation or cryoablation to destroy tumors under ultrasound visualization.
For example, during a liver biopsy, real-time ultrasound ensures precise needle placement, minimizing the risk of damage to surrounding blood vessels and structures. The procedure’s success depends heavily on the accuracy and skill in ultrasound-guided needle navigation. My experience encompasses a range of patient populations and pathologies, requiring adaptability and precision in different anatomical locations and with varied needle sizes and techniques.
Q 25. Explain your understanding of radiation safety in ultrasound.
Ultrasound is considered a safe imaging modality, as it does not utilize ionizing radiation. However, there are safety considerations relating to:
- Thermal bioeffects: High intensity ultrasound can generate heat in tissues. This is usually not a significant concern with diagnostic ultrasound, which uses lower intensity outputs, but prolonged exposures at higher intensities should be avoided.
- Mechanical bioeffects: Cavitation (the formation and collapse of gas bubbles in tissues) can occur at very high ultrasound intensities, though this is not a concern with standard diagnostic procedures.
- ALARA principle: The ALARA principle (As Low As Reasonably Achievable) should be followed. This means using the lowest ultrasound output necessary to obtain diagnostic images, minimizing the exposure time, and using appropriate transducer selection.
In practice, we always select the lowest intensity setting capable of providing a high-quality image. We also keep the transducer in contact with the patient only as long as necessary. For instance, when scanning a pregnant patient, we strive for brevity and appropriate settings, considering the developing fetus’s well-being. Understanding these bioeffects helps minimize potential risks and ensures patient safety.
Q 26. How would you handle a situation where you suspect medical error?
Suspecting a medical error requires a systematic and careful approach prioritizing patient safety and ethical conduct. My steps would be:
- Immediate action: If the suspected error poses an immediate threat to the patient, take immediate steps to mitigate the harm and stabilize the patient.
- Documentation: Thoroughly and accurately document all observations, actions taken, and conversations related to the suspected error. This documentation should be objective and factual.
- Internal reporting: Report the suspected error through the appropriate internal channels within the institution, following established protocols.
- Collaboration: Consult with colleagues, supervisors, or other relevant healthcare professionals to assess the situation and discuss appropriate next steps. This might involve reviewing the case with other radiologists or obtaining additional imaging.
- Patient communication: Communicate with the patient and their family in a compassionate and transparent manner, explaining the situation and the steps being taken to address it.
- Incident report: Complete a detailed incident report according to institutional guidelines, providing all relevant information.
- Learning from the error: Participate in any subsequent reviews or analyses of the event to identify contributing factors and prevent similar occurrences in the future.
The goal is not to assign blame but to learn from the experience and improve patient safety. Open communication and collaboration are crucial in addressing medical errors effectively.
Q 27. Describe your experience working within a team environment.
I thrive in team environments. My experience has shown me that effective teamwork is essential for providing high-quality patient care. I actively participate in interdisciplinary teams involving radiologists, physicians, nurses, and other healthcare professionals. This includes:
- Collaborative diagnosis: Sharing findings and collaborating with referring physicians to ensure accurate diagnoses and appropriate management plans.
- Procedure assistance: Actively assisting in image-guided procedures, communicating clearly with the procedural team to ensure accurate and safe performance of the procedure.
- Mentoring and teaching: Sharing my knowledge and experience with junior colleagues, fostering a supportive learning environment.
- Communication and coordination: Maintaining clear and effective communication with all team members, ensuring smooth workflow and efficient use of resources.
For example, during a complex case involving multiple specialists, I’ve found that effective communication and collaboration across different disciplines are critical for achieving optimal outcomes for the patient. My role often involves explaining complex imaging findings to non-radiology colleagues in a way that is easily understood, allowing for collaborative decision-making.
Key Topics to Learn for Diagnostic Ultrasound Interview
- Image Acquisition Techniques: Understanding various transducer types (linear, curved, phased array), their applications, and optimizing image quality through TGC, depth, and focus adjustments.
- Anatomy & Physiology: Thorough knowledge of abdominal, pelvic, obstetric, small parts, and vascular anatomy relevant to ultrasound imaging. This includes understanding normal variations and common pathologies.
- Pathology Recognition: Identifying and differentiating various pathologies, such as cysts, masses, stones, and vascular abnormalities, based on their sonographic appearance. Practice analyzing images and correlating findings with clinical presentations.
- Instrumentation & Equipment: Familiarity with ultrasound machine operation, including controls, settings, and troubleshooting common technical issues. Understanding image processing techniques and artifact recognition is crucial.
- Patient Care & Safety: Understanding patient preparation, positioning, and communication techniques. Knowledge of safety protocols and radiation safety principles is essential.
- Measurements & Reporting: Accurate performance of measurements (e.g., fetal biometry, organ size) and generating comprehensive and concise ultrasound reports. Knowing relevant reporting standards and terminology.
- Hemodynamics & Doppler Principles: Understanding the principles of Doppler ultrasound, including spectral and color Doppler, and their application in assessing blood flow and vascular disease.
- Quality Assurance & Quality Control: Understanding the importance of maintaining equipment quality and adhering to quality assurance protocols to ensure accurate and reliable imaging.
- Ethical and Legal Considerations: Understanding professional ethics, patient confidentiality, and legal responsibilities related to the practice of diagnostic ultrasound.
Next Steps
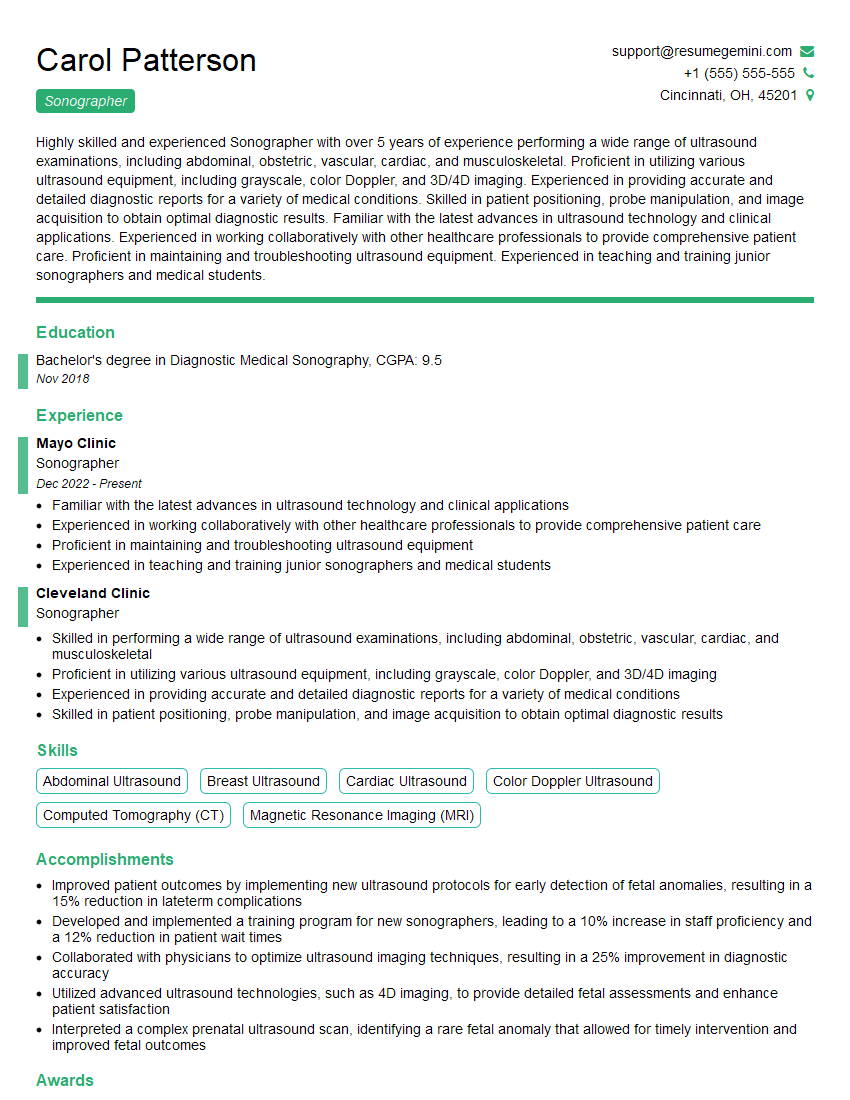
Mastering Diagnostic Ultrasound opens doors to a rewarding career with excellent growth potential in a constantly evolving field. To maximize your job prospects, create a strong, ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume that will catch the eye of recruiters. Examples of resumes tailored to Diagnostic Ultrasound professionals are available to guide you through the process. Invest time in crafting a compelling resume—it’s your first impression!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.