Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Ocular Disease Diagnosis and Treatment interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Ocular Disease Diagnosis and Treatment Interview
Q 1. Explain the diagnostic process for age-related macular degeneration (AMD).
Age-related macular degeneration (AMD) is a leading cause of vision loss in older adults, affecting the macula, the central part of the retina responsible for sharp, central vision. Diagnosing AMD involves a multi-step process focusing on identifying characteristic signs and symptoms.
Detailed Medical History: A comprehensive review of the patient’s family history (AMD is often hereditary), lifestyle (smoking increases risk), and overall health is crucial. We also inquire about symptoms like blurred vision, distorted vision (metamorphopsia), or the presence of a scotoma (blind spot).
Visual Acuity Test: This standard eye exam measures the sharpness of vision. Reduced visual acuity, especially in the central field, points towards macular involvement.
Amsler Grid Test: This simple test helps detect distortions in central vision. Patients look at a grid and report any wavy lines or missing areas, indicating macular damage.
Ophthalmoscopy: Using an ophthalmoscope, we examine the retina directly. We look for characteristic features of AMD such as drusen (yellow deposits under the retina), pigmentary changes (areas of discoloration), and neovascularization (abnormal blood vessel growth).
Optical Coherence Tomography (OCT): This advanced imaging technique provides detailed cross-sectional images of the retina. OCT helps in assessing the thickness of the retinal layers and identifying features of both dry and wet AMD.
Fluorescein Angiography: This test involves injecting a dye into the arm and taking pictures of the retina to visualize blood vessel leakage in wet AMD.
For example, a patient presenting with blurred central vision, metamorphopsia, and drusen visible on ophthalmoscopy, confirmed by OCT showing subretinal fluid, would likely be diagnosed with wet AMD. Early detection through regular eye exams, especially after age 50, is vital for timely intervention.
Q 2. Describe the different types of glaucoma and their management strategies.
Glaucoma encompasses a group of eye diseases characterized by progressive optic nerve damage, often associated with increased intraocular pressure (IOP). There are several types, each requiring different management strategies.
Open-Angle Glaucoma: This is the most common type, where the angle between the iris and cornea remains open, but the drainage of fluid from the eye is impaired, leading to elevated IOP. Management typically involves IOP-lowering medications (e.g., prostaglandin analogs, beta-blockers), laser procedures (e.g., laser peripheral iridotomy), or surgery (e.g., trabeculectomy).
Angle-Closure Glaucoma: This occurs when the iris blocks the drainage angle, causing a sudden and dramatic rise in IOP. This is a medical emergency requiring immediate treatment with medications to lower IOP and potentially surgery (e.g., iridotomy) to relieve the blockage.
Normal-Tension Glaucoma: In this type, optic nerve damage occurs despite normal IOP levels. The exact cause is unknown, and management focuses on protecting the optic nerve through medications or surgery, even with normal IOP.
Congenital Glaucoma: This is a rare type present at birth due to abnormalities in the drainage system. Early diagnosis and surgical intervention are crucial.
Treatment strategies are highly individualized, depending on the type of glaucoma, severity of the disease, and the patient’s overall health. Regular monitoring of IOP and optic nerve health is vital to prevent further vision loss.
For instance, a patient with open-angle glaucoma might be started on eye drops to lower IOP, followed by periodic monitoring of their optic nerve health using visual field tests and OCT imaging. If the medication isn’t enough to control the IOP, laser treatment or surgery may be considered.
Q 3. What are the common causes of diabetic retinopathy, and how is it diagnosed?
Diabetic retinopathy is a leading cause of blindness in working-age adults with diabetes. It’s a complication where high blood sugar levels damage the blood vessels in the retina. The common causes include:
Poorly controlled blood sugar: Chronically elevated blood glucose levels are the primary driver of diabetic retinopathy.
Hypertension (high blood pressure): High blood pressure exacerbates the damage to retinal blood vessels.
Duration of diabetes: The longer a person has diabetes, the greater the risk of developing retinopathy.
Genetic predisposition: While not a direct cause, genetic factors can influence the susceptibility to retinopathy.
Diagnosis typically involves:
Dilated eye exam: This allows the ophthalmologist to thoroughly examine the retina for signs of retinopathy, including microaneurysms (small bulges in blood vessels), hemorrhages (bleeding), and exudates (fluid leakage).
Fluorescein angiography: This helps visualize blood vessel leakage and blockages.
Optical Coherence Tomography (OCT): This assesses the thickness and structure of the retina and helps detect macular edema (swelling).
For instance, a patient with type 1 diabetes for 15 years who presents with blurred vision and is found to have microaneurysms and hemorrhages during a dilated eye exam would be diagnosed with diabetic retinopathy. Early detection and tight blood sugar control are vital in managing and preventing vision loss.
Q 4. Discuss the treatment options for cataracts.
Cataracts are a clouding of the eye’s natural lens, leading to blurred or hazy vision. The primary treatment is surgical removal of the clouded lens and its replacement with an artificial intraocular lens (IOL).
Phacoemulsification: This is the most common cataract surgery technique. A small incision is made in the eye, and the clouded lens is broken up using ultrasound and then aspirated. An IOL is then implanted.
Extracapsular Cataract Extraction (ECCE): In this less common method, a larger incision is made, and the lens is removed in one piece. An IOL is then implanted.
The choice of surgical technique depends on several factors, including the patient’s overall health, the severity of the cataract, and the surgeon’s expertise. Pre-operative evaluation includes assessing visual acuity, determining the appropriate IOL power, and checking for any other eye conditions. Post-operative care involves regular follow-up appointments to monitor healing and visual recovery. Complications are rare but can include infection, inflammation, or retinal detachment. Careful selection and preparation by both patient and surgeon significantly reduce risk.
For example, a patient experiencing significant vision impairment due to cataracts would undergo a phacoemulsification procedure, with the type of IOL selected depending on their individual needs and refractive error correction desires.
Q 5. How do you differentiate between different types of uveitis?
Uveitis is inflammation of the uvea, the middle layer of the eye. Differentiation among the various types is crucial for effective management because they have distinct causes and treatment strategies. Uveitis is categorized based on the location of the inflammation:
Anterior Uveitis: This involves the iris and ciliary body and is characterized by pain, redness, and photophobia (light sensitivity). Causes can include infections (e.g., herpes simplex virus), autoimmune diseases (e.g., ankylosing spondylitis), and trauma.
Intermediate Uveitis: Inflammation affects the vitreous humor (the gel-like substance filling the eye). Symptoms may include floaters, blurred vision, and decreased visual acuity. Possible causes include infections and autoimmune disorders.
Posterior Uveitis: This involves the choroid and retina. Symptoms can include blurry vision, floaters, and visual field defects. Causes include infections (e.g., toxoplasmosis), autoimmune diseases, and sarcoidosis.
Panuveitis: This is a severe form involving all parts of the uvea.
Diagnosis involves a thorough eye examination, including slit-lamp biomicroscopy to visualize the inflammation, and often includes imaging studies (e.g., OCT, fluorescein angiography) to assess the extent of inflammation and identify the underlying cause. Systemic evaluation may be necessary to identify associated systemic conditions. Treatment typically involves corticosteroids (either topical, systemic, or intraocular), immunosuppressive agents, and/or treatment of the underlying infection or disease.
For example, a patient presenting with severe eye pain, redness, and decreased vision may be diagnosed with anterior uveitis after a detailed examination reveals inflammation of the iris. Treatment might involve topical corticosteroids to reduce the inflammation. If the uveitis is severe or recurrent, systemic immunosuppression may be necessary.
Q 6. What are the risk factors for developing dry eye disease, and what are the treatment modalities?
Dry eye disease (DED) is a common condition characterized by insufficient tear production or excessive tear evaporation, leading to discomfort, dryness, and potential damage to the ocular surface. Several risk factors contribute to DED:
Age: Tear production tends to decrease with age.
Gender: Women are more frequently affected, possibly due to hormonal influences.
Environmental factors: Dry air, wind, and smoke can accelerate tear evaporation.
Medications: Some medications, such as antihistamines and diuretics, can reduce tear production.
Underlying medical conditions: Autoimmune diseases like Sjögren’s syndrome can significantly impact tear production.
Contact lens wear: Prolonged or improper contact lens use can contribute to DED.
Treatment modalities for DED aim to improve tear film stability and reduce inflammation. These include:
Artificial tears: Frequent use of lubricating eye drops provides temporary relief.
Punctal plugs: Small plugs inserted into the tear drainage points (puncta) reduce tear outflow.
Lid hygiene: Cleaning the eyelids to remove debris and improve gland function.
Warm compresses: Improve meibomian gland function.
Cyclosporine eye drops: These immunosuppressant drops reduce inflammation.
Autologous serum eye drops: Drops containing the patient’s own serum can provide lubrication and healing.
For example, a patient complaining of persistent eye dryness, burning, and gritty sensation might be diagnosed with DED. The treatment plan could involve artificial tears, lid hygiene, and potentially cyclosporine eye drops, depending on the severity and underlying cause.
Q 7. Explain the use of OCT in retinal disease diagnosis.
Optical Coherence Tomography (OCT) is a non-invasive imaging technique providing high-resolution cross-sectional images of the retina and other ocular structures. Its use in retinal disease diagnosis is invaluable.
Macular diseases: OCT is crucial in diagnosing and monitoring AMD, diabetic macular edema, and other macular pathologies. It allows precise measurement of retinal layer thickness, detection of fluid accumulation, and assessment of structural changes.
Glaucoma: OCT helps evaluate the optic nerve head, assessing its thickness and identifying glaucomatous damage. It’s also used to monitor disease progression.
Retinal detachments: OCT can visualize retinal layers and identify retinal tears or detachments.
Vitreoretinal diseases: OCT can help visualize epiretinal membranes, macular holes, and other vitreoretinal pathologies.
Neuro-ophthalmic diseases: OCT can be used to assess the thickness of the retinal nerve fiber layer (RNFL), providing information about optic nerve health and assessing potential nerve fiber loss.
For example, in a patient suspected of having diabetic macular edema, OCT can clearly demonstrate the presence of fluid accumulation in the macular region, enabling the ophthalmologist to quantify the severity and tailor treatment accordingly. OCT’s ability to visualize subtle structural changes provides more precise information compared to traditional methods.
Q 8. Describe your approach to managing a patient with a suspected retinal detachment.
Suspected retinal detachment is a serious condition requiring immediate attention. My approach begins with a thorough dilated fundus examination to visualize the retina and identify the type and extent of detachment. This often involves using indirect ophthalmoscopy, which provides a wider field of view than direct ophthalmoscopy. I’ll assess for the presence of retinal tears, the location and size of the detachment, and the presence of any associated complications like vitreous hemorrhage.
Based on the findings, I’ll determine the urgency of intervention. For rhegmatogenous retinal detachments (those caused by a tear), prompt surgical intervention is usually necessary to prevent further retinal damage and vision loss. This might involve pneumatic retinopexy (injection of gas into the eye), scleral buckling (placing a band around the sclera to indent the eye and reattach the retina), or vitrectomy (surgical removal of vitreous gel and repair of the tear).
For non-rhegmatogenous retinal detachments (often associated with conditions like traction from scar tissue or exudative detachments from inflammation), management might involve addressing the underlying cause, such as treating inflammation or managing traction. Regular monitoring is crucial in these cases. Throughout the process, patient education about the condition, the treatment plan, and potential risks and outcomes is vital. I always emphasize the importance of post-operative compliance with instructions to maximize the chances of a successful outcome.
For instance, I recently managed a patient with a superior temporal retinal detachment who presented with sudden onset of floaters and a curtain falling over his vision. Immediate vitrectomy and scleral buckling successfully reattached the retina and restored his vision. Early detection and swift intervention were crucial in this case.
Q 9. What are the indications for performing visual field testing?
Visual field testing, also known as perimetry, assesses the extent of a patient’s peripheral and central vision. It’s indicated in a wide range of conditions affecting the visual pathway, from the retina to the visual cortex in the brain.
- Suspected glaucoma: Visual field testing is essential for diagnosing and monitoring glaucoma, where damage to the optic nerve causes characteristic visual field loss.
- Neurological conditions: Conditions such as stroke, multiple sclerosis, and brain tumors can cause visual field defects. Perimetry can help identify the location and extent of the neurological damage.
- Retinal disorders: Diseases like macular degeneration and retinal detachment can lead to specific patterns of visual field loss, assisting in diagnosis and monitoring.
- Optic neuritis: Visual field testing is used to evaluate the severity and location of damage to the optic nerve.
- Following head trauma: Visual field testing is crucial to assess for any damage to the visual pathways following head injury.
- Pre- and post-operative assessment: Perimetry is valuable for assessing visual function before and after surgery, especially in procedures involving the retina or optic nerve.
In essence, if there’s any suspicion of damage anywhere along the visual pathway, a visual field test is an invaluable diagnostic tool.
Q 10. How do you interpret a visual field test result?
Interpreting a visual field test involves analyzing the visual field map generated by the test. The map shows the areas where the patient can and cannot see. A normal visual field is typically symmetrical, with a wide range of peripheral vision.
We look for several key features:
- Scotomas: These are areas of reduced or absent vision within the visual field. Their size, shape, and location are important clues to the underlying cause. A central scotoma, for example, suggests macular involvement.
- Altitudinal defects: These affect either the upper or lower half of the visual field and often indicate vascular compromise or retinal problems affecting specific vascular territories.
- Arcuate scotomas: These are curved scotomas often associated with glaucoma, and follow the course of the retinal nerve fiber bundles.
- Bjerrum scotomas: These are scotomas that appear near the blind spot and are common in early glaucoma.
- Symmetry: Asymmetry between the two eyes strongly suggests pathology.
The interpretation isn’t simply about identifying defects but also involves correlating the pattern of loss with the patient’s medical history and other clinical findings, including ophthalmoscopic examination and imaging studies. For example, a nasal step in the visual field, combined with glaucomatous cupping of the optic disc on ophthalmoscopy, would strongly suggest glaucoma.
Q 11. Explain the role of fluorescein angiography in ophthalmic diagnosis.
Fluorescein angiography is a valuable ophthalmic imaging technique that uses a fluorescent dye, fluorescein, injected intravenously to visualize the blood vessels of the retina and choroid. This allows for detailed assessment of vascular perfusion, leakage, and abnormalities.
Its role in diagnosis is multifaceted:
- Diabetic retinopathy: It helps identify microaneurysms, neovascularization, and macular edema – crucial features of diabetic retinopathy.
- Age-related macular degeneration (AMD): It differentiates between wet and dry AMD, detecting choroidal neovascularization (CNV) characteristic of wet AMD.
- Retinal vascular occlusions: It helps visualize the extent of retinal ischemia in central retinal vein occlusion (CRVO) or central retinal artery occlusion (CRAO).
- Choroidal neovascularization (CNV): It is essential for identifying and characterizing CNV associated with AMD and other conditions.
- Retinal tumors: It can help assess the vascularity of retinal tumors.
For example, in a patient with suspected wet AMD, fluorescein angiography would reveal the presence and characteristics of CNV, guiding treatment decisions. The images show the dye as it flows through the retinal and choroidal vessels, highlighting areas of leakage or blockage which are otherwise hard to detect during a standard ophthalmoscopic exam.
Q 12. Describe the different types of corneal dystrophies and their management.
Corneal dystrophies are a group of inherited disorders affecting the cornea’s transparency and structure. They’re categorized based on the affected corneal layer and the nature of the deposits.
Some common types include:
- Fuchs’ endothelial dystrophy: This affects the endothelium, the innermost layer of the cornea, leading to corneal edema, blurry vision, and eventual vision loss. Management involves observation in early stages, followed by corneal transplantation in advanced cases.
- Granular dystrophy: Characterized by granular deposits in the stroma (the middle layer), causing hazy vision. Treatment is often symptomatic, with contact lenses providing temporary vision improvement. In severe cases, penetrating keratoplasty (PKP) or deep anterior lamellar keratoplasty (DALK) may be considered.
- Lattice dystrophy: This type shows lattice-like deposits in the stroma, resulting in reduced vision and recurrent corneal erosions. Management can include phototherapeutic keratectomy (PTK) to remove the superficial corneal deposits. In severe cases, transplantation may be required.
- Reis-Bücklers dystrophy: This is characterized by recurrent corneal erosions and stromal opacities. Management is often aimed at symptomatic relief and may include bandage contact lenses or amniotic membrane transplantation to promote healing.
Management of corneal dystrophies is highly individualized and depends on the severity, type of dystrophy, and the patient’s age. Options range from conservative management with lubricating eye drops and contact lenses to more aggressive interventions like corneal transplantation.
Q 13. Discuss the surgical management of strabismus.
Strabismus, or misalignment of the eyes, can be surgically corrected to improve both the cosmetic appearance and the binocular vision. The surgical approach is highly individualized and depends on factors such as the type of strabismus (esotropia – inward turning, exotropia – outward turning, hypertropia – upward turning, hypotropia – downward turning), the age of the patient, and the amount of deviation.
The surgery involves weakening or strengthening the extraocular muscles (muscles that control eye movement).
- Muscle Recession: The insertion of a muscle is moved backward on the eye, weakening its pull.
- Muscle Resection: A portion of the muscle is removed, shortening it and strengthening its pull.
- Muscle Transposition: The insertion of a muscle is moved to a different location on the eye to change the direction of its pull.
The surgeon carefully plans the type and amount of surgery needed based on pre-operative measurements and assessments, aiming for alignment of the eyes with optimal binocular vision. Post-operative care involves monitoring eye alignment, managing inflammation, and following up with the patient to ensure the success of the surgery and assess potential for recurrence. The goal is not only to align the eyes but also to restore or improve binocular vision, allowing for optimal depth perception.
Q 14. What are the signs and symptoms of optic neuritis?
Optic neuritis is inflammation of the optic nerve, which can cause a wide range of visual disturbances.
The signs and symptoms can vary, but common presentations include:
- Sudden vision loss: This can range from mild blurring to complete loss of vision, often affecting one eye more than the other.
- Pain: Pain is often associated with eye movement. It’s described as an aching or throbbing sensation.
- Color vision changes: Patients may experience diminished color vision, particularly red-green color discrimination deficits.
- Visual field defects: Central scotomas (blind spots in the center of the visual field) are commonly observed.
It’s crucial to note that optic neuritis can be a symptom of multiple sclerosis (MS) or other inflammatory or autoimmune disorders. A thorough neurological evaluation is often necessary to rule out these underlying conditions. Management typically includes high-dose corticosteroids to reduce inflammation and improve visual recovery. Visual recovery can be slow and incomplete, and regular monitoring is crucial. In patients with recurrent optic neuritis, investigation for autoimmune conditions like MS is essential.
Q 15. Explain the management of a patient with a corneal ulcer.
Managing a corneal ulcer requires a prompt and aggressive approach to prevent vision-threatening complications. Think of the cornea as the windshield of your eye – a corneal ulcer is like a crack that needs immediate repair.
Diagnosis: The process begins with a thorough examination including slit-lamp biomicroscopy to assess the ulcer’s size, depth, and characteristics. We’ll also look for signs of infection, such as hypopyon (pus in the anterior chamber). A corneal scraping might be necessary to identify the causative organism (bacteria, fungus, or amoeba) through culture and sensitivity testing.
Treatment: Treatment depends on the identified pathogen. Bacterial ulcers are often treated with topical antibiotics, sometimes administered frequently (every hour initially). Fungal ulcers typically require longer courses of antifungal medications. Severe cases may necessitate hospitalization and intravenous antibiotics. We might also use topical corticosteroids carefully, as these can be problematic if used too early or in high doses, particularly with bacterial infections. Pain management is crucial, and we’ll use topical anesthetic drops for immediate relief and oral analgesics for longer-term comfort.
Monitoring: Regular follow-up appointments are essential to monitor the ulcer’s healing progress. We’ll closely assess the size, depth, and presence of any complications. The frequency of appointments depends on the severity of the ulcer and the patient’s response to treatment. In some cases, therapeutic contact lenses might be used to protect the cornea and promote healing.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess visual acuity in pediatric patients?
Assessing visual acuity in pediatric patients requires different methods than with adults, as they may not be able to articulate their vision accurately. It’s like trying to understand the world through the eyes of a small child—we have to adapt our approach.
Infants (birth to 6 months): We primarily assess the presence of preferential looking. We use visual evoked potentials (VEPs) or other objective tests to evaluate visual function. This checks for the infant’s ability to fixate on objects and follow movements.
Toddlers (6 months to 3 years): We might employ the Teller Acuity Cards, which use preferential looking to determine visual acuity. The Cardiff Acuity Cards are another option using picture cards. Simple tests that assess visual tracking and fixation are also useful.
Preschoolers (3 to 5 years): Allen figures are commonly used to assess visual acuity. These charts use familiar pictures instead of letters or numbers. We also evaluate their ability to perform tasks that require visual function, such as picking up small objects.
Older children (5+ years): Once children can understand instructions and cooperate, we can typically use standard visual acuity charts like the Snellen chart.
Remember, careful observation, patience, and appropriate toys are all vital components of performing a pediatric eye exam.
Q 17. What are the indications for performing a phacoemulsification procedure?
Phacoemulsification, often called cataract surgery, is the most common way to remove cataracts. Think of a cataract as a clouding of the eye’s natural lens, which can be compared to a cloudy window preventing clear vision.
Indications for Phacoemulsification include:
- Cataracts causing significant vision impairment: When the cataract interferes with daily activities such as driving or reading.
- Impaired quality of vision: Reduced contrast sensitivity, glare, or halos around lights.
- Failure of conservative management: When glasses or other non-surgical methods no longer provide adequate visual correction.
- Bilateral cataracts: In some cases, we may opt to perform phacoemulsification on both eyes, but the timing of this depends on several factors.
- Secondary causes: Cataract formation as a result of other eye conditions or injuries.
The procedure is indicated when the visual impairment caused by the cataract significantly impacts a patient’s quality of life. We will discuss the risks and benefits of the surgery with the patient before proceeding.
Q 18. Describe the post-operative care instructions for cataract surgery.
Post-operative care instructions for cataract surgery are crucial for preventing complications and ensuring optimal healing. Think of it like nurturing a delicate plant after transplanting it – gentle care is vital for its healthy growth.
Immediate Post-op (first 24 hours): Patients will experience some discomfort, usually well-managed with prescribed analgesics. They should avoid rubbing or pressing their eyes. We’ll provide instructions on using eye drops (antibiotics, steroids) as prescribed.
Short-term Post-op (first week): Patients will have frequent follow-up appointments to monitor healing and intraocular pressure. They should avoid strenuous activities and swimming.
Long-term Post-op (beyond one week): Patients should continue using prescribed eye drops as directed and schedule regular eye exams to monitor intraocular pressure and assess the health of the implant. They should report any unusual symptoms like increased pain, redness, or decreased vision immediately.
Providing clear, concise, and patient-specific instructions—in writing and verbally—is critical. We encourage patients to ask questions and address any concerns they may have.
Q 19. What are the different types of intraocular lenses (IOLs)?
Intraocular lenses (IOLs) are artificial lenses implanted during cataract surgery to replace the cloudy natural lens. There are several types, each with its own advantages and disadvantages; choosing the right one depends on the patient’s specific needs and preferences. Think of it like choosing the right pair of glasses – different lenses for different vision needs.
Types of IOLs include:
- Monofocal IOLs: These correct vision for either distance or near vision, but not both. A common choice, they are relatively inexpensive and reliable.
- Multifocal IOLs: These IOLs have multiple focal points, providing good vision at both near and far distances. They may reduce the need for glasses after surgery but can sometimes cause side effects like glare or halos.
- Accommodative IOLs: These IOLs can change shape slightly, allowing some degree of focus adjustment for both near and far vision. They offer a good compromise between the monofocal and multifocal, but their effectiveness can vary.
- Toric IOLs: These IOLs correct astigmatism, a common refractive error that causes blurry vision. This can significantly improve visual acuity.
The choice of IOL is a personalized decision based on factors such as the patient’s age, lifestyle, refractive error, and overall health. We will discuss the pros and cons of each type to guide the patient to the best option for their specific needs.
Q 20. Discuss the management of a patient with orbital cellulitis.
Orbital cellulitis is a serious infection of the tissues surrounding the eye. Think of it as an infection spreading behind the windshield of your eye—it needs immediate attention to prevent serious complications.
Diagnosis: Diagnosis is made through clinical examination, including assessment of symptoms such as pain, swelling, redness, and fever. Imaging studies such as CT or MRI scans might be necessary to rule out complications like abscess formation or cavernous sinus thrombosis.
Management: Management involves aggressive antibiotic treatment, often with intravenous antibiotics, to combat the infection. Hospitalization may be required for close monitoring and intravenous administration. Early diagnosis and treatment are crucial to prevent serious complications such as vision loss, meningitis, or even death.
Important Considerations: Immediate referral to an ophthalmologist and possibly an otolaryngologist is essential due to the potential life-threatening nature of orbital cellulitis. We will closely monitor the patient’s response to treatment and adjust medication as needed.
Q 21. What are the different types of contact lenses, and how do you select the appropriate one for a patient?
Contact lenses offer an alternative to glasses for vision correction. Choosing the right type depends on several factors; it’s like finding the perfect shoe—it needs to fit the individual and their lifestyle.
Types of Contact Lenses:
- Soft Contact Lenses: These lenses are made from flexible materials, generally comfortable and easy to wear. They come in various modalities, including daily disposables, weekly, and monthly.
- Rigid Gas Permeable (RGP) Lenses: These lenses are made from a firm material that allows oxygen to pass through, providing better vision correction for certain conditions such as astigmatism and keratoconus. They are generally more durable and offer sharper vision.
- Specialty Contact Lenses: These include lenses designed for specific conditions like keratoconus, dry eye, or aphakia.
Selecting the Appropriate Contact Lens: The selection process involves a thorough eye examination, assessment of the patient’s lifestyle and preferences, and evaluation of corneal health. Factors such as the patient’s refractive error, corneal curvature, tear film quality, and lifestyle will all play a role in determining the best type of contact lens. Patient education and follow-up are crucial to ensure success and safe contact lens wear. Proper fitting is essential to prevent complications.
Q 22. Explain the different types of refractive errors and their correction methods.
Refractive errors are vision problems that occur when the shape of the eye prevents light from focusing correctly on the retina, resulting in blurry vision. The main types are myopia (nearsightedness), hyperopia (farsightedness), astigmatism, and presbyopia (age-related farsightedness).
- Myopia: The eye is too long, or the cornea is too curved, causing distant objects to appear blurry. Correction involves concave lenses (minus lenses) in eyeglasses or contact lenses, or refractive surgery like LASIK to flatten the cornea.
- Hyperopia: The eye is too short, or the cornea is too flat, resulting in blurry near vision. Correction involves convex lenses (plus lenses) in eyeglasses or contact lenses, or refractive surgery to steepen the cornea.
- Astigmatism: The cornea is irregularly shaped, causing blurred vision at all distances. Correction involves cylindrical lenses in eyeglasses or contact lenses to compensate for the irregular curvature, or refractive surgery to reshape the cornea.
- Presbyopia: This age-related condition occurs due to the lens’s decreased ability to accommodate (focus on near objects). It’s corrected with reading glasses, multifocal contact lenses, or refractive surgery such as multifocal IOL implantation.
Choosing the right correction method depends on the individual’s refractive error, age, lifestyle, and overall health. For example, a young adult with high myopia might benefit from LASIK, while an older adult with presbyopia might prefer multifocal contact lenses or reading glasses.
Q 23. Describe the use of gonioscopy in glaucoma diagnosis.
Gonioscopy is a crucial diagnostic procedure used to visualize the angle where the iris meets the cornea (the iridocorneal angle). This angle is vital because it houses the drainage system of the eye (trabecular meshwork), responsible for removing aqueous humor. Blockage in this drainage angle is a primary cause of glaucoma.
During gonioscopy, a special lens (a goniolens) is applied to the eye, allowing the examiner to view the angle structures under magnification. This allows for the assessment of the angle’s width (open-angle vs. narrow-angle glaucoma), presence of any pathologies like synechiae (adhesions), and the overall health of the trabecular meshwork. This information is vital in determining the type of glaucoma and guiding treatment decisions. For instance, a patient with narrow-angle glaucoma might require prompt intervention to prevent acute angle-closure glaucoma, a sight-threatening condition. In open-angle glaucoma, gonioscopy helps rule out anatomical causes and aids in the selection of appropriate treatment strategies.
Q 24. What are the common complications associated with laser surgery in ophthalmology?
Laser surgery, while highly advanced and effective for many ophthalmic conditions, carries potential complications. These vary depending on the specific procedure but can include:
- Infection: Any surgical procedure carries a risk of infection, which can lead to serious consequences if not managed promptly.
- Inflammation: Post-operative inflammation is common but can be severe in some cases, potentially affecting visual acuity.
- Bleeding: Minor bleeding is possible, but significant hemorrhage can threaten vision.
- Dry eye: Certain laser procedures, such as LASIK, can affect tear production, leading to dry eye syndrome.
- Decreased visual acuity: While the goal is improved vision, some procedures can result in a reduction in visual acuity or the development of halos or glare.
- Increased intraocular pressure: Some laser procedures, especially those targeting glaucoma, can temporarily or permanently raise intraocular pressure.
- Retinal detachment: In procedures near the retina, there is a risk of retinal tear or detachment.
The risk of these complications varies depending on several factors including the surgeon’s experience, the patient’s overall health, and the specific laser procedure. Detailed pre-operative counseling is essential to ensure informed consent.
Q 25. How do you counsel patients about the risks and benefits of various treatment options?
Patient counseling is paramount in ophthalmology. It’s a shared decision-making process where I explain the condition, available treatment options, their respective risks and benefits, and potential outcomes in clear, understandable terms. I use visual aids, such as diagrams and images, to aid comprehension. For instance, when discussing cataract surgery, I’d explain the procedure, potential benefits (improved vision), risks (infection, inflammation), and different types of intraocular lenses (IOLs) available, allowing the patient to choose the best option based on their individual needs and preferences. I always answer questions patiently and encourage them to express their concerns. The goal is to empower patients to make informed decisions about their eye health.
I always ensure that the patient understands the natural progression of their disease without treatment and the potential consequences of delaying or refusing treatment. I document everything clearly in the patient’s medical record, including the discussions and the patient’s chosen treatment plan. Follow-up appointments are crucial to monitor progress, address any concerns, and make necessary adjustments to the treatment plan.
Q 26. Describe your experience with managing patients with low vision.
Managing patients with low vision requires a holistic approach. It’s not just about treating the underlying eye condition; it’s also about improving the patient’s quality of life by maximizing their remaining vision and adapting to their visual limitations. This involves:
- Comprehensive eye exam: To determine the cause and extent of vision loss.
- Low vision aids: Prescribing and fitting devices like magnifiers, telescopes, or electronic aids.
- Adaptive strategies: Teaching patients techniques to adapt to their vision loss, such as using larger print, improved lighting, or assistive technology.
- Referral to other specialists: Referring patients to occupational therapists, social workers, or rehabilitation specialists for further support.
- Emotional support: Addressing the emotional and psychological impact of vision loss, as it can be very challenging for patients to adjust.
I recently worked with a patient who had macular degeneration. Through a combination of low vision aids, adaptive strategies, and regular follow-up, we significantly improved her ability to read and perform daily tasks, restoring a sense of independence and enhancing her quality of life. This collaborative approach, focusing on patient empowerment, is crucial in managing low vision effectively.
Q 27. Explain your familiarity with different types of ophthalmic imaging modalities (e.g., OCT, fundus photography, etc.).
I’m proficient in using various ophthalmic imaging modalities to diagnose and monitor ocular diseases. These include:
- Optical Coherence Tomography (OCT): Provides high-resolution cross-sectional images of the retina and optic nerve, crucial for diagnosing and monitoring conditions like macular degeneration, glaucoma, and diabetic retinopathy. I use OCT to assess retinal thickness, detect macular edema, and evaluate the nerve fiber layer of the optic nerve.
- Fundus photography: Provides detailed images of the retina and optic disc, invaluable for detecting and documenting retinal pathologies, such as diabetic retinopathy, age-related macular degeneration, and vascular occlusions. I utilize fundus photos for monitoring disease progression and evaluating treatment response.
- Fluorescein angiography (FA): Involves injecting a fluorescent dye to visualize blood vessels in the retina. It helps detect vascular abnormalities, leakage, and neovascularization, crucial in diagnosing conditions like diabetic retinopathy and age-related macular degeneration.
- Indocyanine green angiography (ICGA): Similar to FA, but uses a different dye to visualize the choroidal circulation. Useful for evaluating choroidal neovascularization and other choroidal pathologies.
- Visual field testing: Assesses the extent of peripheral vision, essential for detecting and monitoring glaucoma and other conditions affecting the visual field.
The choice of imaging modality depends on the suspected condition and the clinical question being addressed. For example, OCT is invaluable for detailed retinal layer analysis, while fundus photography provides a broader overview of retinal pathology.
Q 28. How do you stay current with the latest advancements in ocular disease diagnosis and treatment?
Staying current in ophthalmology requires a multifaceted approach:
- Professional journals and publications: I regularly read peer-reviewed journals such as Ophthalmology, JAMA Ophthalmology, and others, to stay abreast of the latest research findings and clinical trials.
- Medical conferences and meetings: Attending national and international ophthalmology conferences provides opportunities for learning about cutting-edge techniques and interacting with leading experts in the field.
- Continuing medical education (CME): Participating in CME courses and workshops helps maintain and update my knowledge base and fulfills continuing education requirements.
- Professional organizations: Active membership in professional organizations, like the American Academy of Ophthalmology, provides access to resources, educational materials, and networking opportunities.
- Collaboration with colleagues: Regular discussions and collaborations with colleagues in different settings allow the exchange of knowledge and experiences.
Continuous learning is crucial for providing patients with the best possible care and incorporating the most effective and up-to-date treatment strategies into my practice.
Key Topics to Learn for Ocular Disease Diagnosis and Treatment Interview
- Basic Ocular Anatomy and Physiology: Understanding the structure and function of the eye is fundamental. This includes the cornea, lens, retina, and optic nerve.
- Common Ocular Diseases: Develop a strong understanding of the etiology, pathogenesis, and clinical presentation of common diseases like glaucoma, cataracts, age-related macular degeneration (AMD), diabetic retinopathy, and dry eye disease.
- Diagnostic Techniques: Master the principles and applications of various diagnostic tools, including visual acuity testing, ophthalmoscopy, tonometry, visual field testing, optical coherence tomography (OCT), and fluorescein angiography.
- Treatment Modalities: Familiarize yourself with medical and surgical management options for different ocular diseases. This includes pharmacotherapy, laser treatments, and surgical interventions.
- Image Interpretation: Develop proficiency in interpreting various ophthalmic images, including OCT scans, fundus photographs, and fluorescein angiograms.
- Patient Communication and Counseling: Practice explaining complex medical information clearly and compassionately to patients and their families. This includes discussing diagnosis, treatment options, and potential risks and benefits.
- Ethical Considerations in Ocular Care: Understand the ethical implications of diagnosis and treatment decisions, including informed consent and patient autonomy.
- Current Research and Advances: Stay updated on the latest research and advancements in ocular disease diagnosis and treatment. Demonstrate your awareness of emerging technologies and therapeutic approaches.
- Problem-Solving and Clinical Reasoning: Practice applying your knowledge to solve clinical scenarios and make informed diagnostic and therapeutic decisions. Consider case studies and hypothetical situations.
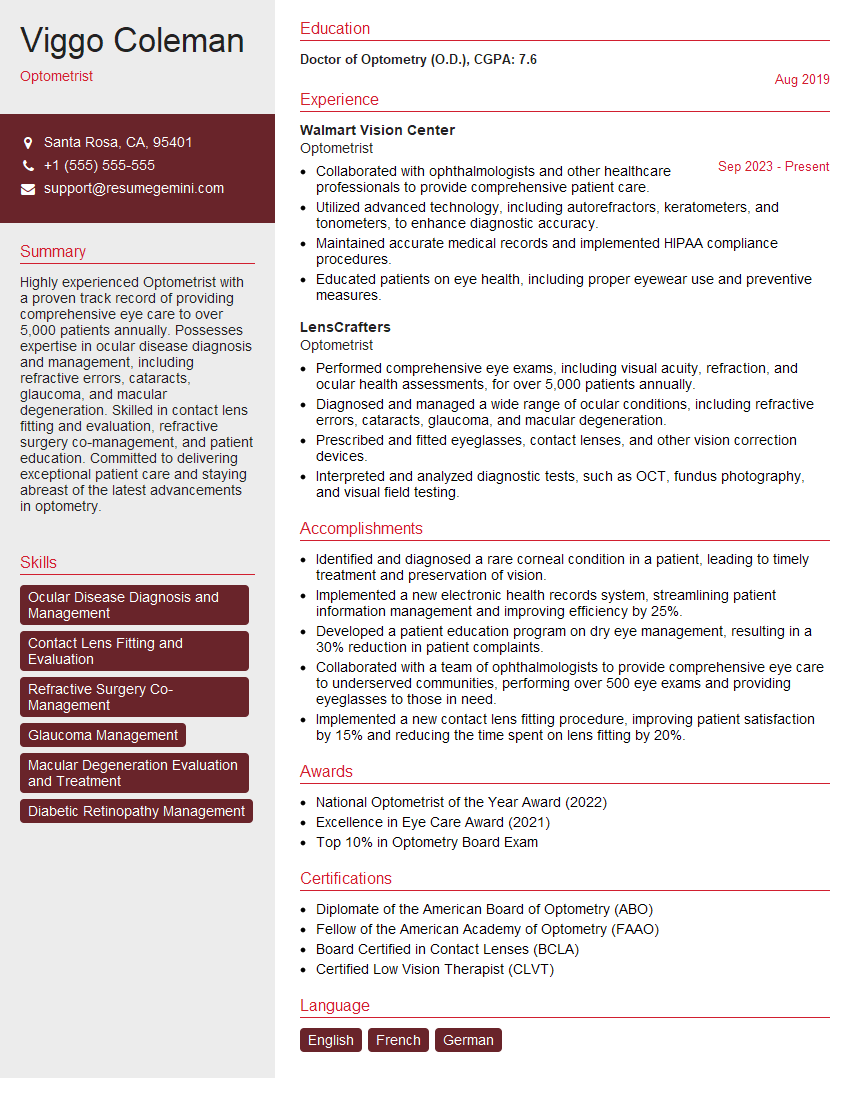
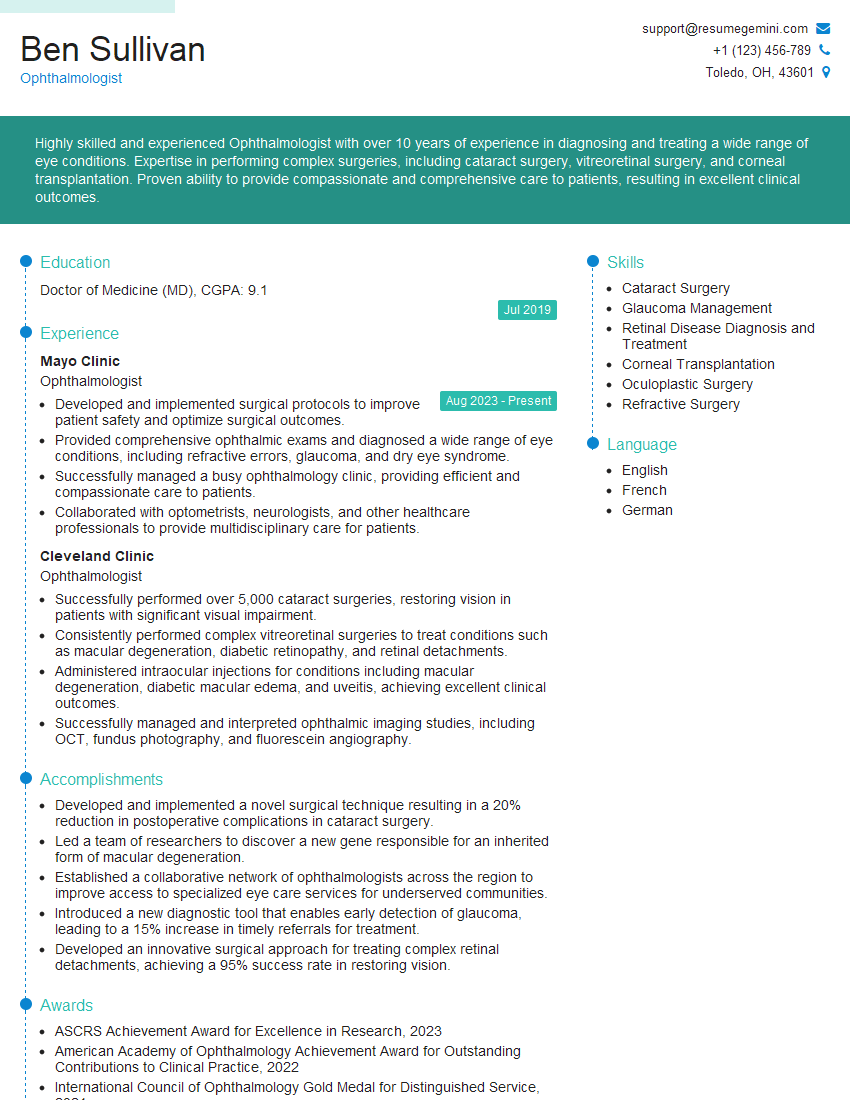
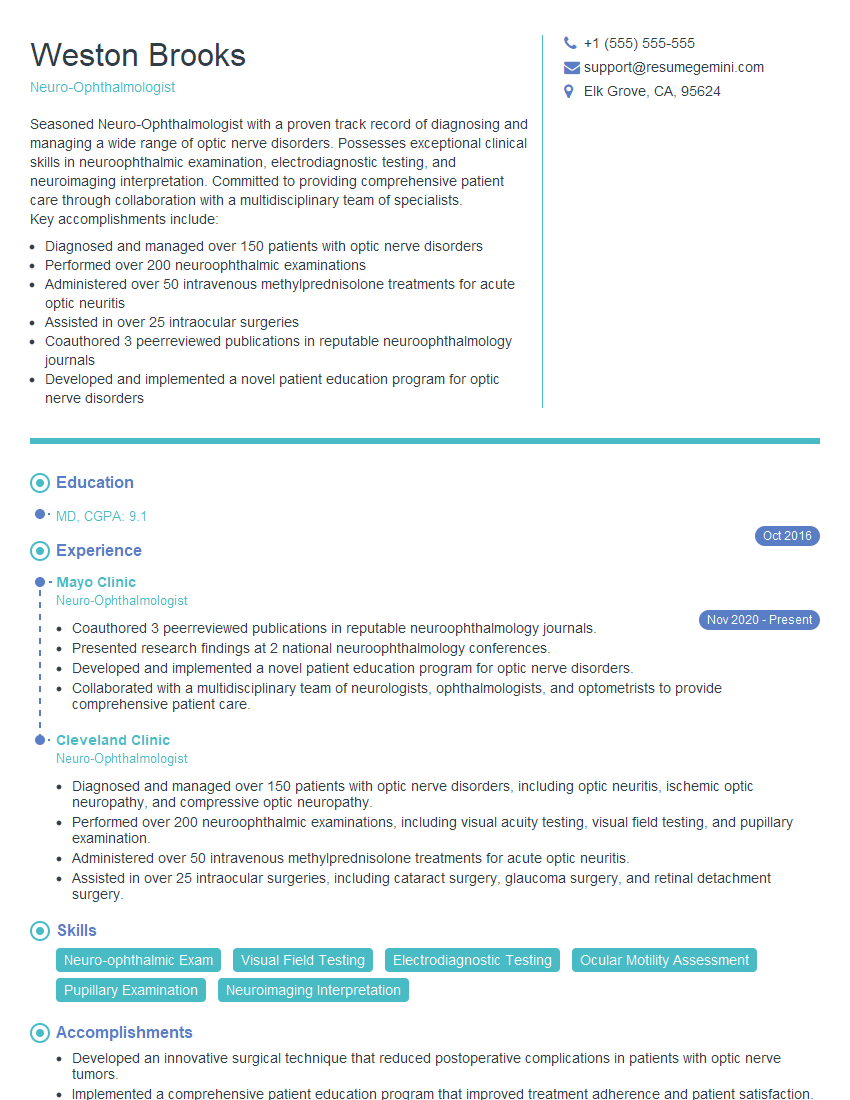
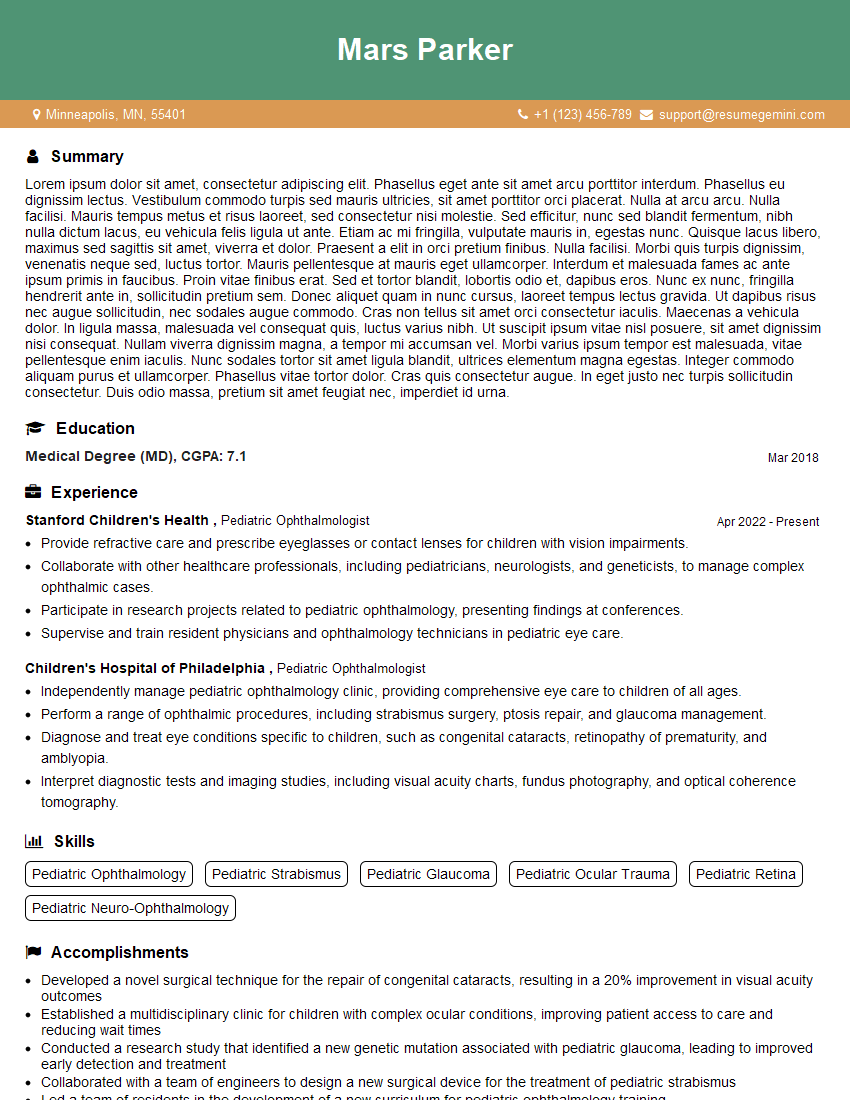
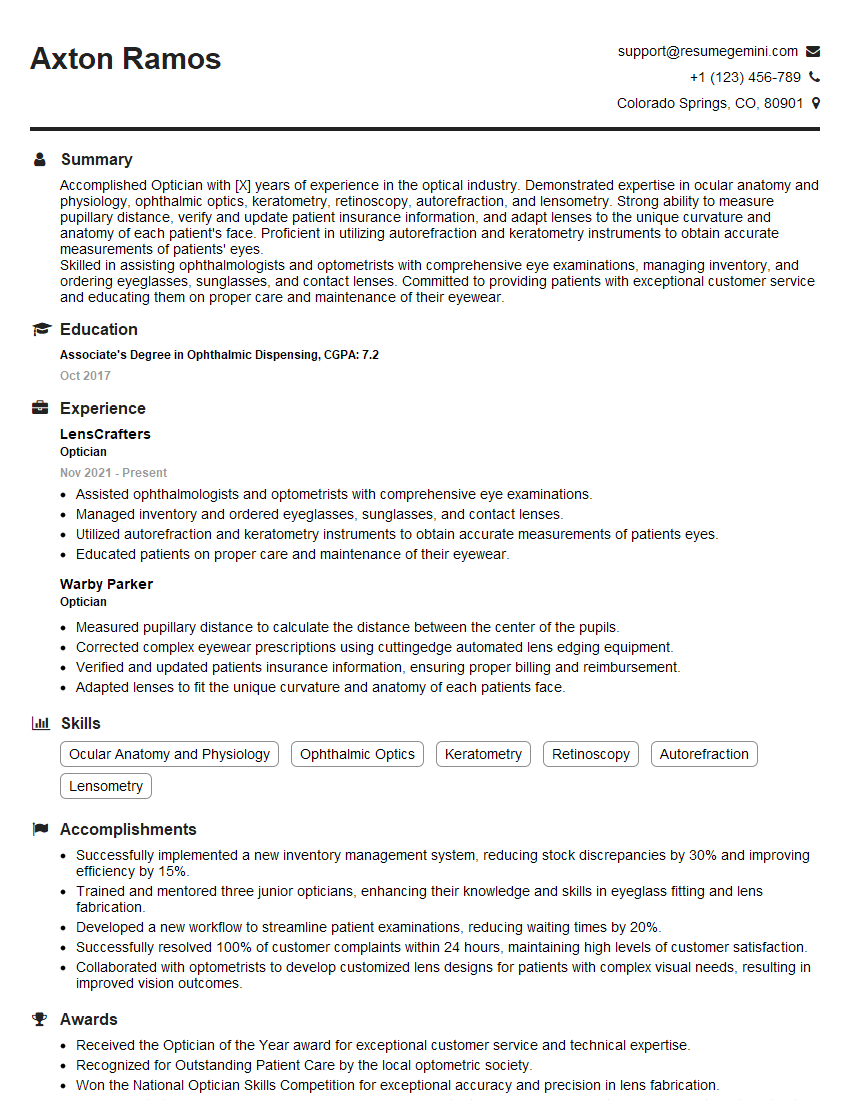
Next Steps
Mastering Ocular Disease Diagnosis and Treatment is crucial for career advancement in this specialized field. A strong understanding of these topics will significantly enhance your interview performance and open doors to exciting opportunities. To maximize your chances of success, it’s essential to create a compelling and ATS-friendly resume that showcases your skills and experience effectively. We highly recommend using ResumeGemini to build a professional resume that stands out. ResumeGemini provides valuable resources and examples of resumes tailored specifically to Ocular Disease Diagnosis and Treatment, helping you present yourself in the best possible light to potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.