Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Patient Monitoring and Risk Stratification interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Patient Monitoring and Risk Stratification Interview
Q 1. Explain the difference between continuous and intermittent patient monitoring.
The core difference between continuous and intermittent patient monitoring lies in the frequency of data collection. Continuous monitoring involves the constant, uninterrupted observation of vital signs and other physiological parameters. Think of it like a live stream of your patient’s health data. Intermittent monitoring, on the other hand, involves periodic checks at predetermined intervals. This is more like taking snapshots of the patient’s condition at specific points in time.
Continuous Monitoring: This approach is crucial for patients in critical care settings, like intensive care units (ICUs), where immediate detection of changes is paramount. Examples include continuous ECG monitoring, continuous blood pressure monitoring (using arterial lines), and continuous pulse oximetry. These provide real-time insight into the patient’s condition, allowing for prompt interventions if necessary.
Intermittent Monitoring: This method is more suitable for patients with stable conditions or those in less critical areas. Vital signs (temperature, pulse, respiration, blood pressure) are checked manually or automatically at set intervals, for example, every four hours or every shift. This is more cost-effective and less intrusive than continuous monitoring but risks missing subtle, yet important, changes.
Analogy: Imagine monitoring a pot of water on a stove. Continuous monitoring is like constantly watching the water to ensure it doesn’t boil over. Intermittent monitoring is like checking the water every few minutes. The approach chosen depends entirely on the risk and the situation.
Q 2. Describe various patient monitoring technologies and their applications.
Patient monitoring technologies are diverse and constantly evolving. They can be broadly categorized based on the physiological parameter they measure.
- Electrocardiogram (ECG): Measures the electrical activity of the heart, detecting arrhythmias and other cardiac issues. This can range from simple 12-lead ECGs to sophisticated continuous ECG monitoring systems.
- Pulse Oximetry: Measures blood oxygen saturation (SpO2) and pulse rate, indicating respiratory function. Simple pulse oximeters are readily available, while advanced systems can provide continuous monitoring and alarms for low SpO2.
- Blood Pressure Monitoring: Measures blood pressure, indicating circulatory function. Methods range from manual sphygmomanometry to automated devices and invasive arterial lines for continuous monitoring.
- Temperature Monitoring: Measures body temperature, an indicator of infection or other physiological disturbances. This can be done using traditional thermometers or advanced systems with continuous temperature sensing.
- Respiratory Monitoring: Monitors breathing rate, depth, and effort, including capnography (measuring carbon dioxide levels in exhaled breath). This is vital in respiratory failure or post-operative settings.
- Telemetry Systems: These wireless systems transmit patient data to central monitoring stations, allowing remote observation of multiple patients. They enhance mobility while still maintaining vigilance.
- Implantable Devices: These include pacemakers and defibrillators that continuously monitor and adjust heart rhythm. Data from these devices can be remotely accessed for analysis and management.
The application of these technologies depends on the patient’s condition and the clinical setting. For instance, continuous ECG is essential during cardiac surgery, while intermittent blood pressure monitoring might suffice for routine check-ups.
Q 3. How do you interpret electrocardiogram (ECG) data?
Interpreting ECG data requires significant training and expertise. It involves analyzing the waveform’s various components – P wave, QRS complex, and T wave – to identify the heart’s electrical activity. The process involves assessing:
- Heart Rate: The number of heartbeats per minute.
- Rhythm: The regularity of heartbeats, identifying arrhythmias such as atrial fibrillation, bradycardia, or tachycardia.
- Waveform Morphology: The shape and size of the various waves, which can indicate myocardial ischemia (reduced blood flow to the heart), hypertrophy (enlarged heart muscle), or other cardiac abnormalities.
- Intervals and Segments: The durations of specific intervals and segments, providing information about conduction pathways and ventricular repolarization.
Example: A prolonged QRS complex could indicate a bundle branch block, a condition affecting the heart’s electrical conduction system. The presence of ST segment elevation could signify an acute myocardial infarction (heart attack).
Software and AI: Modern ECG interpretation often involves sophisticated software and, increasingly, artificial intelligence (AI) to assist clinicians in identifying patterns and potential abnormalities. However, expert review is always crucial for accurate diagnosis and management.
Q 4. What are the key indicators used for risk stratification in heart failure patients?
Risk stratification in heart failure (HF) patients is crucial for guiding treatment and improving outcomes. Key indicators include:
- Ejection Fraction (EF): The percentage of blood pumped out of the left ventricle with each contraction. A reduced EF (<40%) indicates reduced heart function and higher risk.
- New York Heart Association (NYHA) Functional Classification: This system classifies the severity of HF based on symptoms and limitations. Higher NYHA classes indicate more severe disease and increased risk.
- Brain Natriuretic Peptide (BNP) and N-terminal pro-BNP (NT-proBNP): These biomarkers are released by the heart in response to stress and indicate the severity of HF. Higher levels suggest increased risk.
- Renal Function: Estimated glomerular filtration rate (eGFR) reflects kidney function. Impaired renal function is associated with worse outcomes in HF.
- Comorbidities: The presence of other conditions such as diabetes, hypertension, and chronic obstructive pulmonary disease (COPD) increases the risk of adverse events.
- History of Hospitalizations: Previous hospitalizations for HF indicate higher risk of future events.
These indicators are often combined to create a comprehensive risk profile for individual patients, allowing for personalized treatment strategies and improved risk management.
Q 5. Explain the importance of data accuracy and integrity in patient monitoring.
Data accuracy and integrity are paramount in patient monitoring. Inaccurate data can lead to misdiagnosis, inappropriate treatment, and potentially life-threatening consequences. Maintaining data accuracy involves:
- Calibration and Maintenance of Devices: Regularly calibrating monitoring equipment to ensure accuracy and promptly addressing any malfunctions.
- Proper Sensor Placement: Ensuring sensors are correctly placed to obtain accurate readings. Poor sensor placement can lead to artifact and inaccurate data.
- Data Validation: Implementing procedures to validate data, identifying and correcting any errors or inconsistencies.
- Data Security and Privacy: Protecting patient data from unauthorized access and ensuring compliance with relevant regulations (e.g., HIPAA).
- Regular Audits: Conducting regular audits of data collection and analysis processes to identify areas for improvement and prevent errors.
Example: An incorrectly calibrated blood pressure cuff could lead to inaccurate readings, potentially resulting in inappropriate treatment decisions. Similarly, a poorly placed ECG electrode could lead to noisy data, obscuring important diagnostic information.
Q 6. How do you handle conflicting data from different monitoring sources?
Conflicting data from different monitoring sources can arise due to various factors, including sensor malfunction, interference, or variations in measurement techniques. Handling these conflicts requires a systematic approach:
- Identify the Source of Discrepancy: The first step is to carefully examine the data from each source, identifying potential sources of error (e.g., sensor malfunction, incorrect placement, patient movement).
- Review Patient History and Clinical Context: Consider the patient’s overall clinical picture. Does the conflicting data align with other findings and the patient’s current condition?
- Verify Sensor Function and Placement: Check that all sensors are properly functioning and correctly positioned. Recheck the connections and the integrity of the data transmission.
- Cross-Reference with Other Data: Compare the conflicting data with other available information, such as physical examination findings, laboratory results, and medical history.
- Consult with Colleagues: If the discrepancy cannot be resolved, seek expert advice from colleagues, such as a cardiologist or critical care specialist.
In many cases, a combination of factors will lead to the best interpretation of seemingly contradictory data. Documenting the conflict and resolution process is vital for maintaining accurate records and ensuring patient safety.
Q 7. Describe your experience with remote patient monitoring systems.
I have extensive experience with remote patient monitoring (RPM) systems, having worked on projects involving both the implementation and analysis of data from these systems. My experience includes:
- System Implementation: I’ve been involved in selecting, configuring, and deploying RPM systems for various patient populations, including those with chronic heart failure, diabetes, and hypertension.
- Data Analysis: I have experience analyzing data from RPM systems, identifying trends, patterns, and potential issues. This includes developing algorithms to identify patients at risk of deterioration.
- Alert Management: I’ve worked on developing and implementing alert systems to notify healthcare providers of significant changes in patient data, facilitating timely interventions.
- Patient Education and Support: I’ve participated in designing and delivering patient education programs to ensure patients understand how to use RPM devices and communicate effectively with their care teams.
- Integration with EHRs: I have experience integrating RPM data into electronic health record (EHR) systems, ensuring seamless data flow and improved clinical workflow.
Example: In one project, we implemented an RPM system for heart failure patients, collecting data on weight, blood pressure, and symptoms. Analysis of this data enabled us to proactively identify patients at risk of hospitalization, allowing for timely interventions and reducing hospital readmissions.
Q 8. What are the ethical considerations related to patient data privacy and security?
Patient data privacy and security are paramount ethical considerations in healthcare. We’re dealing with highly sensitive information that, if compromised, could lead to significant harm – identity theft, financial loss, and reputational damage, to name a few. The ethical considerations revolve around several key principles:
- Confidentiality: This means ensuring that only authorized individuals have access to patient data. Strong access controls, encryption, and data anonymization techniques are crucial.
- Integrity: Maintaining the accuracy and completeness of patient data is essential. Robust data validation processes and audit trails help ensure data integrity.
- Availability: Authorized personnel need timely access to patient data when needed. This requires reliable systems and robust disaster recovery plans.
- Transparency: Patients should be informed about how their data is collected, used, and protected. Clear and concise privacy policies are essential.
- Accountability: Clear lines of responsibility should be established for data security and privacy breaches. This includes robust incident response plans.
For example, imagine a scenario where a hospital’s patient monitoring system is hacked, exposing patients’ medical records. This breach not only violates patient privacy but also erodes trust in the healthcare system. Ethical guidelines like HIPAA (in the US) provide a framework for handling such sensitive information responsibly.
Q 9. Explain the role of predictive analytics in risk stratification.
Predictive analytics plays a crucial role in risk stratification by leveraging historical data and advanced algorithms to identify individuals at higher risk of developing adverse health events. This allows for proactive interventions and personalized care.
For example, a predictive model might analyze a patient’s medical history, lab results, lifestyle factors, and genetic information to predict their likelihood of experiencing a heart attack within the next five years. Patients identified as high-risk could then be enrolled in preventive programs, such as cardiac rehabilitation or medication management, significantly reducing their risk.
These models typically employ machine learning techniques like logistic regression, support vector machines, or neural networks to analyze complex datasets and identify patterns indicative of risk. The output is often a risk score, which helps clinicians prioritize patients who need more attention and resources.
Q 10. How do you identify and address potential biases in risk stratification models?
Bias in risk stratification models is a significant concern. It can lead to disparities in care, where certain patient populations are unfairly categorized as high- or low-risk, based on factors unrelated to their actual health status. Identifying and addressing these biases is crucial for equitable healthcare.
Several strategies help mitigate bias:
- Data auditing: Carefully examine the dataset for imbalances in representation across different demographic groups.
- Feature engineering: Develop features that reduce reliance on potentially biased variables. For instance, instead of relying solely on socioeconomic status, focus on easily measurable health indicators.
- Algorithmic fairness techniques: Employ techniques that explicitly address fairness concerns, such as fair classification algorithms that minimize disparate impact across groups.
- Regular model evaluation: Continuously monitor model performance across different subgroups to identify any emerging biases.
- Transparency and explainability: Use models that are easily interpretable so that biases can be detected and addressed more easily.
For instance, a risk model trained on a dataset predominantly representing one ethnic group might underperform for other groups, leading to inaccurate risk predictions. By carefully auditing the data and employing appropriate algorithmic fairness techniques, we can build more equitable and reliable risk stratification models.
Q 11. Describe your experience with different risk stratification tools and methodologies.
My experience encompasses a wide range of risk stratification tools and methodologies. I’ve worked extensively with both rule-based systems and machine learning models. Rule-based systems are simpler, easier to interpret, and excellent for well-defined scenarios. However, they may struggle with complex interactions and nuances in patient data.
On the other hand, machine learning models, particularly those based on neural networks or ensemble methods, can capture more complex relationships within the data. However, they require larger datasets and careful tuning to avoid overfitting and bias.
I have practical experience with specific tools like Apache Spark for large-scale data processing and various machine learning libraries such as scikit-learn and TensorFlow for model building and evaluation. I’ve also worked with commercially available risk stratification tools designed for specific conditions, such as cardiovascular disease or sepsis risk prediction, tailoring their applications based on the specific needs of the healthcare setting.
Q 12. What are the limitations of current patient monitoring technologies?
Current patient monitoring technologies, while significantly advanced, still face several limitations:
- Data overload and integration challenges: The sheer volume of data generated by various monitoring devices can be overwhelming, and integrating this data from different systems can be complex and time-consuming.
- Algorithm limitations: Current algorithms might not always accurately capture the subtleties of human physiology, leading to false positives or negatives.
- Lack of personalization: Many technologies lack personalization, failing to account for individual patient characteristics and preferences.
- Data privacy and security concerns: The large amount of sensitive patient data collected requires robust security measures to prevent breaches and ensure compliance with privacy regulations.
- Cost and accessibility: Many advanced monitoring technologies are expensive and may not be accessible to all patients, creating disparities in care.
- Alert fatigue: The constant stream of alerts from monitoring systems can lead to alert fatigue among healthcare professionals, potentially causing delays in responding to critical events.
Addressing these limitations requires a multi-faceted approach involving improvements in data integration, algorithm development, personalization, and user interface design, as well as efforts to reduce cost and improve accessibility.
Q 13. How do you communicate complex patient data to healthcare professionals?
Communicating complex patient data effectively to healthcare professionals requires a clear, concise, and visually appealing approach. Avoid overwhelming them with raw data; instead, focus on presenting key findings and actionable insights.
My strategy typically involves:
- Summarization: Provide concise summaries of key findings, highlighting significant changes or trends.
- Visualization: Use charts, graphs, and dashboards to present data visually, making it easier to understand complex patterns.
- Prioritization: Highlight critical findings that require immediate attention.
- Contextualization: Provide context for the data, explaining the implications and recommendations.
- Interactive tools: Utilize interactive dashboards that allow healthcare professionals to explore the data in more detail.
For example, instead of presenting a long list of vital signs, I might present a graph showing trends over time, highlighting any significant deviations from the norm. This approach ensures that crucial information is immediately apparent, enabling quicker decision-making.
Q 14. How do you stay updated on the latest advancements in patient monitoring and risk stratification?
Staying updated in this rapidly evolving field requires a proactive and multi-pronged approach:
- Regularly attending conferences and workshops: Participating in relevant conferences and workshops allows me to learn about the latest advancements from leading experts in the field.
- Reading peer-reviewed publications: Staying abreast of the latest research and findings through journals such as JAMA, The Lancet, and other specialized publications in biomedicine and healthcare informatics is critical.
- Networking with colleagues: Engaging with other professionals through online communities, professional organizations, and collaborations enables sharing of knowledge and insights.
- Online courses and training programs: Taking online courses and participating in training programs on new technologies and methodologies keeps my skillset sharp.
- Following key opinion leaders and influencers: Staying informed about advancements through social media and online platforms frequented by leading researchers and clinicians is valuable.
This combination of active learning and professional engagement keeps my knowledge up-to-date and allows me to contribute effectively to the field.
Q 15. Describe a time you had to troubleshoot a malfunctioning patient monitoring device.
During my time at County General Hospital, we experienced an issue with a malfunctioning cardiac monitor. The monitor was intermittently displaying inaccurate heart rate readings, sometimes showing flatlines even when the patient had a palpable pulse. This was a critical situation requiring immediate attention.
My troubleshooting began with a methodical approach. First, I visually inspected all connections, ensuring the leads were securely attached to both the patient and the monitor. I checked for any loose wires or damaged cables. I then reviewed the monitor’s internal diagnostics, accessed through its menu system. This revealed an error code indicating a potential problem with the sensor module.
Following the manufacturer’s troubleshooting guide, I attempted to reset the monitor. This involved powering it down completely and then restarting it. When this didn’t resolve the issue, I replaced the sensor module, a relatively straightforward process. After the replacement, the monitor displayed accurate readings. Finally, I documented the entire troubleshooting process, including the error codes, actions taken, and the resolution, within the device’s log and the patient’s electronic health record.
This experience reinforced the importance of understanding both the device’s functionality and the manufacturer’s troubleshooting guidelines. A timely and accurate response ensured patient safety and avoided potential misdiagnosis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you prioritize patients based on their risk stratification scores?
Prioritizing patients based on risk stratification scores involves a multi-faceted approach that balances urgency with resource allocation. We utilize a tiered system, often incorporating both physiological and clinical parameters.
Patients with the highest risk stratification scores, indicating an immediate threat to their well-being, such as those experiencing acute respiratory distress or showing signs of sepsis, are given top priority. These patients receive immediate attention from the medical team, including rapid assessment, intervention, and continuous monitoring.
Next in priority are patients with intermediate risk scores, who require regular monitoring and timely intervention should their condition worsen. For example, a post-surgical patient with elevated heart rate and blood pressure would fall into this category. These patients are monitored closely, and their scores are reassessed frequently.
Finally, patients with lower risk scores still require regular monitoring and surveillance, but their care can be managed proactively rather than reactively. This allows healthcare providers to allocate resources effectively while ensuring all patients receive appropriate attention.
The entire process is dynamic and responsive; changes in a patient’s condition warrant immediate reassessment and potential re-prioritization. It’s essentially a constant balancing act, prioritizing critical care while managing overall workload.
Q 17. Explain your understanding of different scoring systems used in risk stratification.
Several scoring systems are used in risk stratification, each designed to assess different aspects of a patient’s condition. The choice of system depends on the specific clinical context.
- APACHE II (Acute Physiology and Chronic Health Evaluation II): A widely used system that incorporates physiological variables like blood pressure, respiratory rate, and temperature to predict mortality risk in critically ill patients.
- SOFA (Sequential Organ Failure Assessment): Focuses on organ dysfunction and is particularly useful in assessing the severity of sepsis and other critical illnesses. It scores six organ systems (respiratory, cardiovascular, hepatic, renal, neurological, and coagulation).
- NEWS2 (National Early Warning Score 2): A simpler system that uses readily available physiological measurements (like heart rate, respiratory rate, oxygen saturation, blood pressure, and temperature) to identify patients at risk of deterioration. It’s easier to implement than the more complex scores and often used in broader hospital settings.
- MEWS (Modified Early Warning Score): Similar to NEWS2, providing a quick assessment of risk.
Each system has its strengths and limitations. For instance, APACHE II is more comprehensive but requires more data, whereas NEWS2 is simpler but may miss subtle indicators of deterioration. The selection of the appropriate scoring system is crucial for accurate risk stratification and timely intervention.
Q 18. What is the role of patient monitoring in improving clinical outcomes?
Patient monitoring plays a crucial role in improving clinical outcomes by enabling early detection of adverse events, facilitating timely interventions, and supporting informed clinical decision-making.
Early Detection: Continuous monitoring allows for the immediate identification of subtle changes in vital signs or other physiological parameters, which might otherwise go unnoticed until the patient’s condition significantly deteriorates. For example, an early warning system can detect a gradual drop in oxygen saturation before it becomes a life-threatening event.
Timely Intervention: Early detection allows for prompt interventions, such as adjusting medication, providing supplemental oxygen, or initiating advanced life support. The quicker the intervention, the better the chance of a positive outcome.
Informed Decision Making: The data collected through patient monitoring provides clinicians with a comprehensive picture of the patient’s physiological state, guiding them towards the most appropriate treatment strategies. Data analysis can identify trends and patterns, aiding in the prediction of potential complications and allowing for preventative measures.
Ultimately, by combining early warning, rapid response, and evidence-based decision-making, patient monitoring significantly improves patient safety, reduces complications, and leads to better overall clinical outcomes.
Q 19. How do you ensure the effective integration of patient monitoring data into electronic health records (EHRs)?
Effective integration of patient monitoring data into EHRs is paramount for streamlining workflows and ensuring seamless access to critical information. This is achieved through a combination of technological and procedural strategies.
HL7 Integration: Utilizing Health Level Seven (HL7) standards ensures interoperability between the patient monitoring system and the EHR. This allows for the automated transfer of physiological data (heart rate, blood pressure, etc.) directly into the patient’s chart, eliminating manual entry and reducing errors.
Data Standardization: Employing standardized data formats, such as DICOM (Digital Imaging and Communications in Medicine) for waveforms and structured data formats for numeric values, guarantees consistent and easily interpretable data. This facilitates both human review and automated analysis.
Data Validation: Implementing data validation rules ensures the accuracy and reliability of the transferred data. This includes checking for outliers and inconsistencies, which can flag potential errors or equipment malfunctions.
Workflow Optimization: Integrating patient monitoring data directly into the EHR should be designed to streamline clinical workflows. For example, critical alerts should be prominently displayed in the EHR, enabling immediate clinician response.
By implementing these strategies, we can ensure that patient monitoring data is readily available to healthcare providers, improving their decision-making abilities and enhancing patient care. This process also reduces the administrative burden associated with manual data entry and promotes overall efficiency.
Q 20. Explain the concept of early warning systems in patient monitoring.
Early warning systems (EWS) in patient monitoring are designed to proactively identify patients at risk of clinical deterioration. These systems continuously monitor key physiological parameters and trigger alerts when values exceed pre-defined thresholds.
Components of an EWS: Typically, an EWS uses a scoring system (like NEWS2 or MEWS) based on vital signs (heart rate, respiratory rate, blood pressure, temperature, oxygen saturation). The scores are calculated automatically by the monitoring system. When the score reaches a critical level, an alert is generated, notifying the appropriate healthcare personnel.
Alerting Mechanisms: Alerts can be delivered via various methods, including visual indicators on the monitor, audible alarms, and notifications sent to clinicians’ mobile devices or computer systems. The severity of the alert typically correlates with the risk level.
Benefits of an EWS: EWS significantly enhance patient safety by enabling early intervention in cases of impending clinical deterioration, allowing for timely treatment and improved patient outcomes. It can reduce mortality and length of stay in hospitals.
Example: Imagine a patient whose respiratory rate steadily increases over several hours. An EWS continuously monitors this parameter and would generate an alert if it exceeds the pre-set threshold. This early warning would prompt the nursing staff to assess the patient and potentially initiate interventions to prevent respiratory failure.
Q 21. How do you contribute to the development and improvement of patient monitoring protocols?
Contributing to the development and improvement of patient monitoring protocols involves a multi-pronged approach that combines clinical expertise with a deep understanding of technology and data analysis.
Data Analysis: I actively participate in reviewing patient monitoring data to identify trends and patterns. This includes analyzing data from various sources to identify areas where protocols could be improved for better early detection of at-risk patients. For instance, we may discover a correlation between specific parameter changes and adverse events that might not have been previously recognized.
Protocol Development: My involvement in protocol development often starts with identifying areas for improvement in patient safety or efficiency. We might design new algorithms for early warning systems, incorporating newly developed scoring systems or adapting existing ones to our specific patient population. This frequently involves collaboration with clinicians, biostatisticians, and IT professionals.
Technology Evaluation: I evaluate and recommend new patient monitoring technologies to ensure we are using the most effective and up-to-date equipment and software. This might involve comparing the performance of different monitoring systems, assessing their accuracy, and ensuring their seamless integration with existing systems.
Education and Training: To ensure consistent application of protocols, I contribute to the development and delivery of training programs for healthcare professionals. This might involve teaching clinicians how to interpret patient monitoring data, use new technologies effectively, and implement new protocols correctly.
Through this ongoing process of data analysis, protocol development, technology assessment, and staff training, I contribute directly to continuous improvement of patient safety and care quality.
Q 22. What are the challenges of implementing patient monitoring programs in diverse healthcare settings?
Implementing patient monitoring programs across diverse healthcare settings presents a unique set of challenges. The biggest hurdle is often the heterogeneity of resources and infrastructure. A state-of-the-art hospital will have vastly different technological capabilities and staffing levels compared to a rural clinic. This disparity impacts the choice of monitoring technology, data integration capabilities, and the availability of trained personnel to manage the system and interpret the data.
- Technology Compatibility: Integrating new monitoring systems with existing Electronic Health Records (EHRs) and other healthcare IT systems can be complex and costly, requiring significant technical expertise. Inconsistent data standards further complicate matters.
- Staffing and Training: Adequate training for clinical staff on using the monitoring system, interpreting alerts, and taking appropriate action is crucial. However, limited time and resources can hinder effective training and ongoing professional development.
- Data Security and Privacy: Protecting patient data is paramount. Robust security measures are needed to prevent data breaches and ensure compliance with regulations like HIPAA. This becomes even more challenging in resource-constrained environments.
- Cost and Resource Allocation: The initial investment in hardware, software, and staff training can be significant, often exceeding the budget of smaller healthcare facilities. Ongoing maintenance and updates also contribute to the cost.
- Workflow Integration: Seamlessly integrating patient monitoring into existing clinical workflows is essential to avoid disrupting care. Careful planning and change management are crucial for successful implementation.
For example, I once worked on a project to implement a remote patient monitoring program in a network of rural clinics. The biggest challenge was ensuring reliable internet connectivity and providing sufficient training to staff who were unfamiliar with technology. We addressed this by investing in satellite internet access and delivering tailored, hands-on training sessions. We also developed user-friendly interfaces to minimize the learning curve.
Q 23. How do you interpret and respond to alerts generated by patient monitoring systems?
Interpreting alerts from patient monitoring systems requires a systematic approach. It’s crucial to avoid alarm fatigue, a condition where healthcare professionals become desensitized to alerts due to frequent false positives or low-priority warnings. My approach involves a tiered response system, prioritizing alerts based on urgency and clinical significance.
- Prioritization: Alerts are categorized into critical (e.g., cardiac arrest), urgent (e.g., severe hypotension), and non-urgent (e.g., minor arrhythmia). Critical alerts trigger immediate action, while urgent alerts require prompt attention. Non-urgent alerts may require review and follow-up based on the patient’s overall clinical picture.
- Contextualization: I always consider the patient’s medical history, current medications, and other relevant clinical data when evaluating an alert. An abnormal heart rate, for instance, might be expected in a patient with known heart conditions but would be a cause for concern in a previously healthy individual.
- Verification: I never rely solely on an alert; I always verify the information with a physical examination and review other relevant data points. This step is essential to rule out false alarms or technical errors.
- Communication: Effective communication with the care team is vital. Depending on the nature of the alert, I may notify the attending physician, nurse, or other relevant healthcare professionals. Clear and concise communication is crucial to ensure a timely and coordinated response.
For example, I once received a critical alert indicating a significant drop in blood oxygen saturation (SpO2) in a post-operative patient. I immediately verified the reading, performed a physical examination, and discovered the patient was experiencing respiratory distress. I notified the attending surgeon and respiratory therapist, initiating emergency intervention.
Q 24. Describe your experience with data visualization techniques for patient monitoring data.
Data visualization is essential for effectively communicating complex patient monitoring data and identifying trends. I have extensive experience using various techniques to present data in a clear, concise, and actionable manner.
- Time-series graphs: These are ideal for visualizing physiological parameters over time, allowing us to quickly identify patterns and anomalies. Examples include heart rate, blood pressure, and respiratory rate plotted against time.
- Scatter plots: Useful for exploring correlations between different variables. For example, a scatter plot could show the relationship between heart rate and blood pressure.
- Heatmaps: Effective for representing the distribution of data across different time periods or patient groups. For example, a heatmap could show the frequency of alerts across different hours of the day.
- Dashboards: I frequently use interactive dashboards to present key patient metrics in a centralized and easily accessible manner, providing a comprehensive overview of the patient’s condition at a glance.
I’ve used these techniques to develop dashboards that provide clinicians with real-time insights into patient status and allow for rapid identification of potential problems. For instance, a dashboard might highlight patients at risk of sepsis based on their vital signs and laboratory results, enabling early intervention.
In one project, we used a combination of time-series graphs and heatmaps to track the incidence of medication errors related to patient monitoring systems. This visualization helped pinpoint specific times of day or weeks when errors were most frequent, leading to improvements in training and workflow adjustments.
Q 25. How do you use patient monitoring data to inform treatment decisions?
Patient monitoring data plays a crucial role in informing treatment decisions. By providing continuous and objective insights into a patient’s physiological state, it enhances the accuracy and timeliness of clinical decision-making. This allows for personalized treatment plans and improved patient outcomes.
- Early Detection of Deterioration: Continuous monitoring allows for the early detection of subtle changes in a patient’s condition, which might otherwise go unnoticed. This early warning system enables timely interventions, preventing adverse events.
- Medication Adjustments: Monitoring data, such as blood pressure and heart rate, can guide medication adjustments to optimize therapeutic effects and minimize side effects.
- Treatment Response Assessment: Monitoring data helps evaluate the effectiveness of treatments and interventions. For example, we can track changes in heart rate and oxygen saturation after administering a medication to determine if it’s having the desired effect.
- Risk Stratification: Patient monitoring data is a key component of risk stratification. By analyzing data such as vital signs, laboratory results, and other physiological parameters, we can identify patients at high risk of adverse events.
For example, I once worked with a team managing patients with chronic heart failure. Using patient-generated data from wearable sensors, we could precisely adjust medication dosages based on individual responses. This resulted in fewer hospital readmissions and improved quality of life.
Q 26. What are the key performance indicators (KPIs) you track to assess the effectiveness of a patient monitoring program?
Key Performance Indicators (KPIs) are essential for evaluating the effectiveness and impact of a patient monitoring program. They provide objective measures of success and help identify areas for improvement.
- Alert Accuracy: The percentage of alerts that accurately reflect a clinically significant event. A high accuracy rate indicates the system is effectively identifying genuine problems.
- Mean Time to Respond: The average time it takes to respond to alerts. A shorter response time suggests prompt and effective interventions.
- Reduction in Adverse Events: A decline in the incidence of adverse events, such as cardiac arrests, respiratory failure, or falls, indicates the program is effectively improving patient safety.
- Length of Stay: A reduction in hospital length of stay suggests improved efficiency and faster patient recovery.
- Readmission Rates: A decrease in readmission rates signifies the program is effectively preventing complications and improving patient outcomes.
- Patient Satisfaction: Gathering feedback from patients on their experience with the monitoring program provides valuable insights into the usability and impact of the system.
These KPIs are regularly tracked and analyzed to ensure the program is achieving its goals and to identify opportunities for optimization. Regular reporting and review sessions with stakeholders are also essential for ensuring continuous improvement.
Q 27. Describe your experience working with interdisciplinary teams on patient monitoring and risk stratification initiatives.
Successful patient monitoring and risk stratification initiatives require a strong interdisciplinary team approach. I have extensive experience collaborating with physicians, nurses, pharmacists, data scientists, and IT specialists. Effective collaboration relies on clear communication, shared goals, and respect for each team member’s expertise.
- Shared Decision-Making: Key decisions related to program implementation, data interpretation, and treatment plans are made collaboratively, ensuring input from all relevant stakeholders.
- Regular Communication: We utilize regular meetings, emails, and other communication channels to ensure seamless information flow and coordinated efforts.
- Defined Roles and Responsibilities: Each team member has clearly defined roles and responsibilities, ensuring accountability and preventing overlap.
- Conflict Resolution: A mechanism for resolving conflicts and disagreements is established to ensure productive collaborations.
- Data Sharing and Integration: Secure platforms and processes are used for sharing and integrating data from various sources, ensuring all team members have access to relevant information.
In one project, our team developed a predictive model for identifying patients at high risk of sepsis. This required close collaboration between clinicians who provided medical expertise, data scientists who developed the model, and IT specialists who ensured data integrity and accessibility. The success of this project hinged on the effective communication and teamwork among these diverse individuals.
Key Topics to Learn for Patient Monitoring and Risk Stratification Interview
- Physiological Monitoring Techniques: Understanding various monitoring modalities (ECG, SpO2, BP, respiratory rate), their limitations, and artifact interpretation. Consider practical application in different clinical settings (ICU, ward, remote monitoring).
- Data Analysis and Interpretation: Mastering the analysis of patient data to identify trends, anomalies, and potential risks. Explore different statistical approaches and visualization techniques used in risk prediction.
- Risk Stratification Models: Familiarize yourself with common risk stratification tools and scoring systems used in various patient populations (e.g., cardiac risk, sepsis risk). Understand their underlying principles and limitations.
- Clinical Decision Support Systems (CDSS): Explore how CDSS utilize patient monitoring data for risk prediction and clinical decision support. Consider practical examples of how these systems improve patient outcomes.
- Ethical and Legal Considerations: Understand the ethical implications of data privacy, data security, and informed consent in the context of patient monitoring and risk stratification.
- Technological Advancements: Stay updated on emerging technologies in patient monitoring, such as wearable sensors, AI-powered analytics, and telehealth platforms. Discuss their impact on risk stratification and patient care.
- Problem-Solving and Critical Thinking: Practice analyzing complex patient scenarios, identifying potential risks, and developing appropriate interventions. Focus on developing a structured approach to problem-solving in this field.
Next Steps
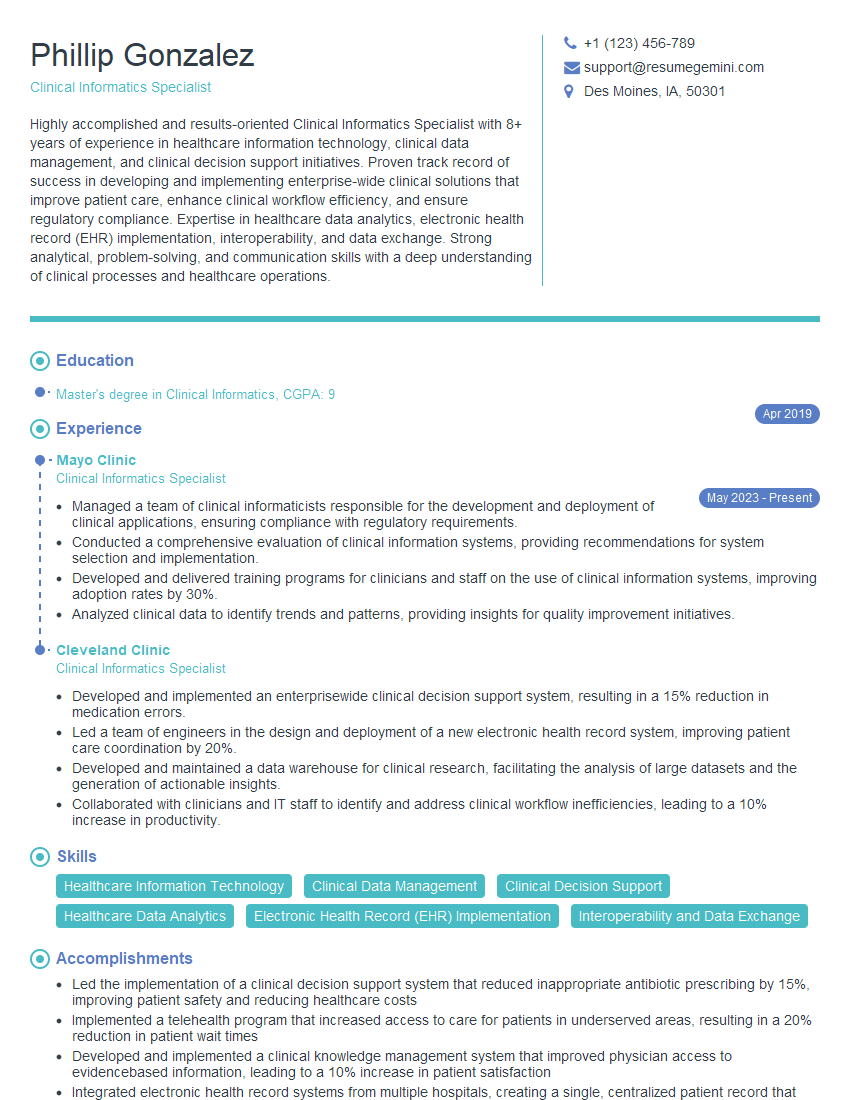
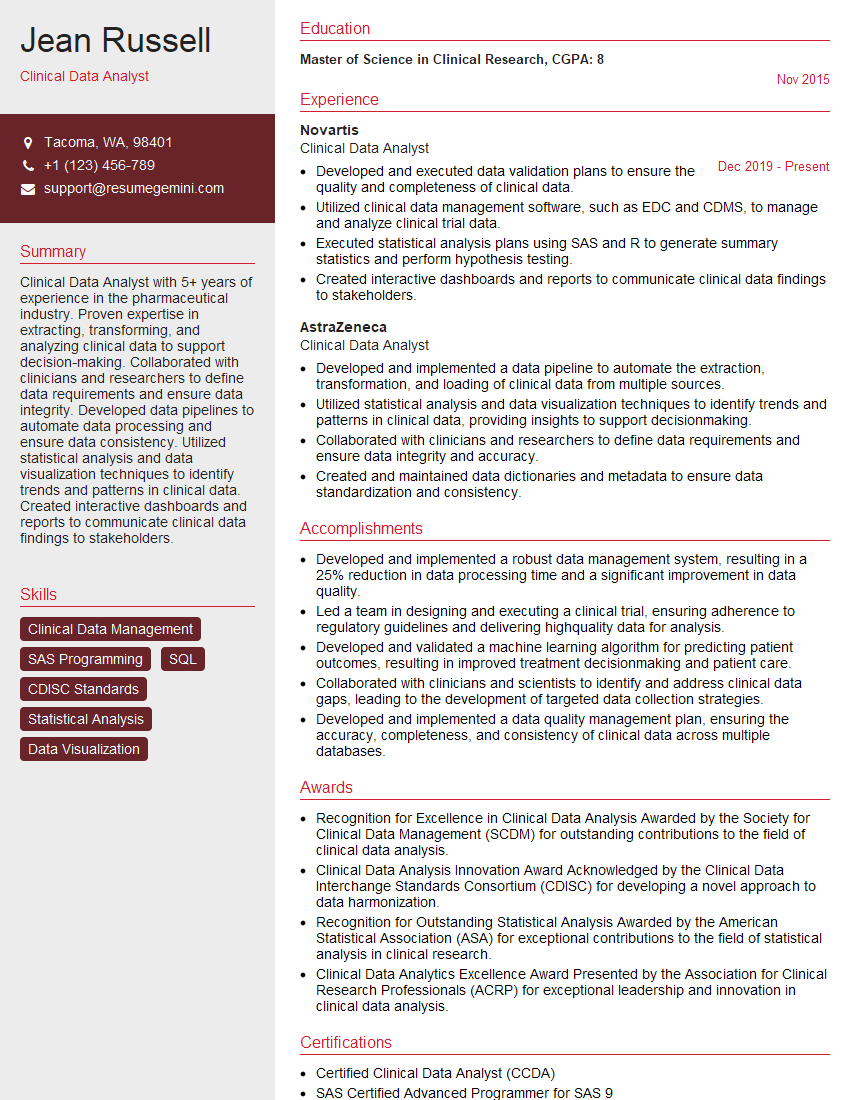
Mastering Patient Monitoring and Risk Stratification is crucial for career advancement in healthcare. It demonstrates your ability to leverage technology for improved patient care and proactive risk management – highly valued skills in today’s dynamic healthcare landscape. To stand out, create a strong, ATS-friendly resume that showcases your expertise effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We offer examples of resumes tailored to Patient Monitoring and Risk Stratification to help you get started. Invest the time to craft a compelling resume; it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.