The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Pleural Procedures interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Pleural Procedures Interview
Q 1. Describe the indications for thoracentesis.
Thoracentesis, a procedure involving needle insertion into the pleural space to remove fluid, is indicated in several scenarios. Its primary purpose is diagnostic and therapeutic. Diagnostically, it helps determine the nature of pleural fluid, identifying conditions like infection (empyema), malignancy (metastatic cancer), congestive heart failure, or pulmonary embolism. Therapeutically, it’s used to relieve respiratory distress caused by significant pleural effusion, which is a build-up of fluid in the pleural space. Imagine a lung struggling to expand because it’s compressed by excess fluid; thoracentesis helps alleviate this pressure, improving breathing. This procedure is also helpful in relieving symptoms like dyspnea (shortness of breath) and chest pain associated with pleural effusion.
- Diagnostic: Determining the cause of pleural effusion (e.g., infection, cancer, heart failure).
- Therapeutic: Relieving respiratory distress caused by large pleural effusions; improving breathing and reducing symptoms.
Q 2. What are the contraindications for thoracentesis?
Contraindications to thoracentesis, meaning situations where it shouldn’t be performed, are primarily related to the risk of complications. These include situations where the risk outweighs the benefits. A significant localized infection over the puncture site, for example, increases the risk of spreading the infection. Similarly, severe coagulopathy (bleeding disorders) increases the chance of significant hemorrhage. Uncooperative patients pose a risk of accidental needle movement. Finally, a very small or inaccessible pleural effusion may not justify the risks of the procedure.
- Uncooperative patient: Inability to remain still during the procedure.
- Severe coagulopathy: Increased risk of bleeding.
- Localized infection at puncture site: Risk of spreading infection.
- Very small or inaccessible pleural effusion: Risk outweighs benefit.
Q 3. Explain the procedure for performing a thoracentesis, including patient positioning and needle insertion technique.
Performing a thoracentesis requires meticulous technique to minimize complications. The patient is typically positioned sitting upright, leaning forward, to allow the fluid to gravitate to the lower part of the pleural space, making it easier to access. Alternatively, a lateral decubitus position may be used. The chosen site, usually the posterior mid-axillary line, is carefully identified using anatomical landmarks and percussion or ultrasound to confirm the presence of fluid and avoid vital structures. Local anesthesia is injected. Using aseptic technique, a small-gauge needle is inserted through the skin and intercostal space, aiming towards the fluid collection. Aspiration is then performed using a syringe or connected to a collection system. Continuous monitoring of the patient’s vital signs, including oxygen saturation, is crucial throughout the procedure. Ultrasound guidance is frequently used to increase accuracy and minimize risks.
Needle Insertion Technique: The needle should be advanced slowly and steadily. Aspiration should be intermittent, avoiding rapid removal of large volumes of fluid to prevent sudden hypotension (low blood pressure) or re-expansion pulmonary edema. The patient should be monitored closely for signs of complications throughout the procedure.
Q 4. How do you manage complications during a thoracentesis (e.g., pneumothorax, bleeding)?
Complications during thoracentesis, although rare with proper technique, necessitate immediate management. Pneumothorax, the collapse of a lung due to air entering the pleural space, is a significant risk and requires immediate chest tube insertion to re-expand the lung. Bleeding, another potential complication, may require observation, pressure dressing, or in severe cases, surgical intervention. Infection at the puncture site can be managed with antibiotics. Hypotension (low blood pressure) from rapid fluid removal requires fluid resuscitation. Early recognition of signs like sudden shortness of breath, chest pain, or oxygen desaturation, demands prompt intervention. Monitoring vital signs throughout and post-procedure is essential. It’s critical to have resuscitation equipment readily available. In the event of a major complication, immediate consultation with a thoracic surgeon or critical care team may be required.
Q 5. What are the different types of pleural drainage catheters?
While thoracentesis uses a needle for fluid removal, pleural drainage catheters are used for longer-term drainage. Several types exist, each with unique characteristics. Small-bore catheters are often used for smaller effusions and are less likely to cause bleeding or pneumothorax. Large-bore catheters are used for larger effusions or when significant drainage is anticipated. Some catheters have a pigtail design, which reduces the risk of lung injury. Flutter valves can facilitate drainage without the need for a water seal system. The choice of catheter depends on factors like the size and nature of the effusion, the patient’s clinical status, and the preference of the physician. The goal is to provide effective drainage while minimizing complications.
Q 6. Explain the indications for placing a chest tube.
Chest tube placement, involving inserting a drainage tube into the pleural space, is indicated when there’s a need for prolonged drainage of air or fluid. This is crucial in managing various conditions. Pneumothorax, requiring removal of air to re-expand the lung, is a primary indication. Hemothorax (blood in the pleural space), often following trauma, requires drainage to prevent further complications. Empyema (infected pleural fluid), often requiring prolonged drainage and antibiotic treatment, benefits greatly from chest tube placement. Additionally, chest tubes may be used for postoperative drainage after thoracic surgery or to manage pleural effusions that don’t respond adequately to thoracentesis.
Q 7. Describe the technique for placing a chest tube.
Chest tube insertion is a sterile procedure usually performed under local or regional anesthesia. The insertion site, typically in the fifth or sixth intercostal space in the mid-axillary line, is selected carefully, often using fluoroscopy or ultrasound guidance. A small incision is made, and blunt dissection is used to create a path for the tube. The chest tube is then inserted into the pleural space, careful to avoid injury to the lung or major vessels. Once in place, the tube is secured with sutures, and a water-seal drainage system is attached. The system helps prevent air from re-entering the pleural space. Post-insertion, a chest x-ray confirms proper tube placement and the absence of complications. The patient is closely monitored for complications, and the drainage is carefully measured and documented. The chest tube is typically removed once drainage is minimal and the lung is fully expanded.
Q 8. How do you manage air leaks and bleeding associated with chest tubes?
Managing air leaks and bleeding associated with chest tubes requires a systematic approach. Air leaks, often indicated by continuous bubbling in the water seal chamber of the drainage system, usually resolve spontaneously as the lung re-expands. However, persistent or significant leaks may necessitate interventions. These include ensuring the chest tube is properly placed and secured, checking for any kinks or obstructions in the tubing, and assessing for ongoing lung injury. Sometimes, a surgical intervention might be necessary to address persistent air leaks. Bleeding, on the other hand, requires close monitoring of the drainage output. A gradual decrease in bleeding is expected, but a sudden surge or persistent, significant bleeding necessitates immediate attention. This may involve increasing suction, confirming tube placement and patency, or, in more severe cases, returning to the operating room for surgical intervention or angiographic embolization.
Imagine a scenario where a patient has a persistent air leak after a lung resection. We would first check for any kinks in the tubing or ensure the chest tube is appropriately positioned. If the leak persists, we would consider using a larger-bore chest tube or even surgical intervention to close the air leak source. Similarly, if a patient’s chest tube drainage suddenly increases significantly, we’d immediately assess the patient for signs of instability and investigate the cause, potentially involving radiology (chest CT) to rule out major bleeding sources.
Q 9. What are the indications for pleurodesis?
Pleurodesis is a procedure aimed at obliterating the pleural space, thus preventing recurrent pleural effusions. It’s indicated in patients with recurrent malignant pleural effusions that significantly compromise respiratory function despite repeated thoracentesis or when such procedures carry a high risk. Other indications include recurrent benign pleural effusions, such as those seen in tuberculosis or rheumatoid arthritis, where conservative management has failed. Essentially, pleurodesis is considered when the risk of recurrent pleural fluid accumulation outweighs the risks of the procedure itself. It is a last resort for patients with significant respiratory compromise due to recurrent effusions.
For example, a patient with malignant mesothelioma experiencing repeated, large pleural effusions leading to shortness of breath despite repeated thoracenteses would be a strong candidate for pleurodesis.
Q 10. Describe different pleurodesis techniques (e.g., talc pleurodesis, chemical pleurodesis).
Several techniques exist for pleurodesis. Talc pleurodesis involves instilling talc powder into the pleural space. Talc induces a sterile inflammatory reaction that leads to pleural thickening and adhesion, effectively obliterating the space. Chemical pleurodesis utilizes various sclerosing agents such as bleomycin, tetracycline, or doxycycline. These agents also stimulate inflammation and fibrosis within the pleural space, ultimately achieving pleural obliteration. The choice of technique depends on factors such as the patient’s overall health, the nature of the effusion (malignant vs. benign), and institutional preferences. The procedure is typically performed under image guidance (fluoroscopy or ultrasound) to ensure proper placement of the sclerosing agent.
Consider a patient with a recurrent benign pleural effusion. Talc pleurodesis might be a suitable option due to its efficacy and relative simplicity. However, in a patient with a malignant pleural effusion and compromised respiratory function, chemical pleurodesis using a less irritating agent like bleomycin might be preferred to minimize potential complications.
Q 11. What are the potential complications of pleurodesis?
Pleurodesis, while effective, carries potential complications. These include pain, which can range from mild discomfort to severe chest pain requiring strong analgesics. Dyspnea (shortness of breath) can occur due to lung restriction from pleural thickening. Fever is common due to the inflammatory reaction, although usually self-limiting. Respiratory distress syndrome is a rare, but potentially life-threatening complication. Infection, although rare with sterile technique, is also a possibility. Finally, there’s a chance of pulmonary emboli which is carefully monitored through the process.
For instance, a patient might experience significant post-pleurodesis pain requiring strong analgesics and respiratory physiotherapy. Careful monitoring for signs of respiratory distress or infection is crucial in the post-procedure period.
Q 12. How do you interpret a chest x-ray following a pleural procedure?
Interpreting a chest x-ray after a pleural procedure involves assessing several key features. First, we look for complete or partial lung expansion, indicating successful removal of pleural fluid or air. We check for the presence and position of chest tubes, ensuring they are properly placed and not kinked. We evaluate for any residual pleural fluid or air collections. Finally, we assess for any signs of complications such as pneumothorax (collapsed lung), pleural thickening, or atelectasis (collapsed lung segment). The presence of these complications would necessitate further intervention.
For example, a post-pleurodesis chest x-ray might show complete lung expansion with no significant pleural fluid remaining, indicating a successful procedure. However, if we see a large pneumothorax, we would immediately intervene with chest tube placement or surgical repair.
Q 13. How do you manage post-procedural pain?
Post-procedural pain management is crucial after pleural procedures. This involves a multimodal approach combining analgesics such as NSAIDs (non-steroidal anti-inflammatory drugs) and opioids, as needed. Regional anesthesia, such as intercostal nerve blocks, can effectively reduce pain. Adjunctive therapies like physiotherapy, including deep breathing exercises and coughing techniques, can improve lung expansion and reduce pain. Patient education about pain management strategies and the importance of respiratory physiotherapy is vital.
For a patient experiencing moderate post-pleurodesis pain, we might prescribe a combination of NSAIDs and a low dose of opioid analgesics, supplemented by intercostal nerve blocks and respiratory physiotherapy. Regular pain assessment and modification of the analgesic regimen based on the patient’s response are essential.
Q 14. What are the indications for a video-assisted thoracoscopic surgery (VATS) for pleural disease?
Video-assisted thoracoscopic surgery (VATS) offers a minimally invasive approach to managing pleural disease. Indications for VATS include diagnostic procedures such as pleural biopsy for the evaluation of pleural effusions of uncertain etiology. It’s also indicated for therapeutic procedures such as the removal of pleural tumors (tumorectomy), pleurodesis, decortication (removal of thick pleural peel), and management of empyema (pus in the pleural space). VATS generally offers advantages over open thoracotomy in terms of reduced post-operative pain, shorter hospital stays and faster recovery times. The choice of VATS versus open surgery depends on various factors including the nature and extent of the pleural disease and the surgeon’s expertise.
For example, a patient with a suspicious pleural mass identified on imaging might undergo a VATS pleural biopsy for diagnosis. If a malignant pleural mesothelioma is confirmed, VATS pleurectomy/decortication could be offered as a treatment option.
Q 15. Describe the advantages and disadvantages of VATS compared to other pleural procedures.
Video-assisted thoracoscopic surgery (VATS) offers several advantages over traditional open thoracotomy for pleural procedures. It’s minimally invasive, resulting in less pain, smaller incisions, shorter hospital stays, and faster recovery times. Think of it like keyhole surgery compared to open-heart surgery – less trauma to the body. However, VATS does have limitations. It requires specialized equipment and expertise, and may not be suitable for all patients, particularly those with complex or extensive pleural disease. For instance, a patient with massive adhesions within their pleural space might be better suited to an open procedure. Furthermore, VATS may not provide as extensive a view as an open procedure, potentially limiting the extent of surgery that can be performed in a single session. Other pleural procedures, such as thoracentesis (needle drainage) are simpler and less invasive, but only address fluid removal and don’t allow for tissue biopsy or surgical intervention. The choice between VATS and other procedures depends on the specific clinical scenario, the patient’s overall health, and the surgeon’s expertise.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you differentiate between transudative and exudative pleural effusions?
The key difference between transudative and exudative pleural effusions lies in their underlying cause. Transudative effusions are caused by systemic factors that alter fluid balance across the pleural membrane, like heart failure or liver cirrhosis. Imagine it like a leaky pipe – the system is failing to regulate fluid properly. The fluid is typically watery and low in protein and cells. Exudative effusions, on the other hand, result from inflammation or infection within the pleural space itself, such as pneumonia or cancer. This leads to increased permeability of the pleural membrane, allowing fluid, protein, and cells to leak into the pleural space. Think of it like a damaged pipe, allowing fluid to leak out aggressively. Exudative effusions are characterized by higher protein and cell counts in the fluid.
Q 17. What are the common causes of pleural effusion?
Pleural effusions, essentially fluid buildup in the pleural space, have a wide range of causes. The most common culprits include:
- Congestive heart failure: This is a leading cause, due to increased hydrostatic pressure in the pulmonary circulation.
- Pneumonia and other infections: Inflammation due to infection can increase pleural permeability.
- Malignancy: Cancer cells can directly invade the pleura or indirectly cause effusion through lymphatic obstruction.
- Pulmonary embolism: A blood clot in the lung can lead to pleural inflammation and effusion.
- Tuberculosis: Infection causes inflammation and subsequent effusion.
- Autoimmune diseases like rheumatoid arthritis and lupus: These can trigger inflammation in the pleura.
- Liver cirrhosis: Reduced albumin levels lead to fluid accumulation.
- Renal failure: Impaired fluid and electrolyte balance contributes to effusion.
Therefore, a thorough investigation is crucial to pinpoint the underlying cause of any pleural effusion.
Q 18. Explain the Light’s criteria for differentiating transudative and exudative effusions.
Light’s criteria are used to help differentiate between transudative and exudative pleural effusions based on the characteristics of the pleural fluid. While not definitive, they provide a valuable clinical guide. The criteria are:
- Pleural fluid protein/serum protein ratio > 0.5
- Pleural fluid LDH/serum LDH ratio > 0.6
- Pleural fluid LDH > 2/3 the upper limit of normal serum LDH
If one or more of these criteria are met, the effusion is considered exudative. If none are met, it is likely transudative. It’s important to note that Light’s criteria are not foolproof and exceptions exist. Further investigations are always necessary to establish a definitive diagnosis.
Q 19. Describe the role of cytology and microbiology in the evaluation of pleural fluid.
Cytology and microbiology play vital roles in evaluating pleural fluid. Cytology examines the cellular components of the fluid under a microscope, looking for malignant cells. This is crucial in diagnosing pleural malignancies. Finding malignant cells confirms the diagnosis of cancer and guides treatment decisions. Microbiology involves culturing the fluid to identify any bacteria, fungi, or other infectious agents. This helps diagnose infectious pleural effusions, such as those caused by tuberculosis or pneumonia. Positive cultures guide antibiotic or antifungal therapy. In many cases, both cytology and microbiology are performed simultaneously to provide a comprehensive evaluation of the pleural fluid, ultimately contributing to an accurate and timely diagnosis.
Q 20. What are the different types of pleural malignancy?
Pleural malignancy can stem from various sources. The most common types include:
- Metastatic lung cancer: Cancer cells spread from the lung to the pleura.
- Metastatic breast cancer: Breast cancer cells spread to the pleura.
- Metastatic lymphoma: Lymphoma cells infiltrate the pleural space.
- Primary pleural mesothelioma: A rare cancer arising from the lining of the pleura, often linked to asbestos exposure.
- Primary lung cancer directly involving the pleura: In some cases, lung cancer initially grows and directly involves the pleura.
Accurate diagnosis requires a combination of clinical history, imaging studies (chest X-ray, CT scan), and pleural fluid analysis.
Q 21. How do you manage malignant pleural effusions?
Managing malignant pleural effusions requires a multi-pronged approach, targeting both symptom relief and underlying disease control. The primary goal is to alleviate respiratory distress caused by fluid accumulation. This is often achieved through:
- Thoracentesis: Repeated drainage of fluid with a needle.
- Pleurodesis: A procedure that chemically or surgically scars the pleural lining, preventing further fluid accumulation.
- Indwelling pleural catheters (IPC): Long-term drainage system.
Beyond fluid management, treatment focuses on addressing the underlying cancer. This may include chemotherapy, radiation therapy, or targeted therapy, depending on the type and stage of the cancer. The approach is tailored to each patient’s individual circumstances and overall health status. Palliative care plays a crucial role in improving quality of life and addressing symptom management.
Q 22. What is a pleural biopsy and when is it indicated?
A pleural biopsy is a procedure where a small sample of tissue is taken from the pleura, the thin membrane surrounding the lungs. It’s crucial for diagnosing various pleural diseases, primarily when imaging studies (like chest X-rays or CT scans) are inconclusive or suggest a need for tissue confirmation. Think of it like taking a small sample to examine under a microscope for a more precise diagnosis.
A pleural biopsy is indicated when there’s a pleural effusion (fluid buildup in the pleural space) of uncertain origin, suspected malignancy (cancer) involving the pleura, or evaluation of inflammatory or infectious processes affecting the pleura. For example, if a patient has a persistent pleural effusion and imaging findings suggest malignancy, a pleural biopsy is necessary to confirm the diagnosis and guide treatment.
Q 23. Describe the different techniques for pleural biopsy.
Several techniques exist for pleural biopsy, each with its advantages and disadvantages:
- Blind Needle Biopsy: This is a relatively simple procedure where a needle is inserted into the pleural space, guided by palpation and anatomical landmarks. While less invasive, the success rate is lower due to potential difficulties in accurately targeting the lesion.
- Ultrasound-Guided Biopsy: This technique uses ultrasound imaging to visualize the pleural effusion and guide needle placement, leading to a higher success rate and fewer complications. This is now the preferred approach in many institutions.
- CT-Guided Biopsy: CT scanning provides excellent anatomical detail, allowing precise targeting of pleural lesions, especially those deep within the pleural space. This is often utilized for lesions that are difficult to reach with ultrasound.
- Thoracoscopic Biopsy (Video-Assisted Thoracoscopic Surgery – VATS): A minimally invasive surgical approach, VATS offers the best visualization of the pleura. A small incision is made, and a scope with a camera is inserted to visualize and obtain a tissue sample. This allows for more extensive sampling and is useful for complex cases.
- Open Biopsy: This is a more invasive surgical approach, reserved for cases where other methods fail or when larger tissue samples are required. It involves a larger incision in the chest wall.
The choice of technique depends on several factors, including the location and size of the lesion, the patient’s overall health, and the available equipment and expertise.
Q 24. What are the risks and complications associated with pleural biopsy?
Pleural biopsy carries inherent risks and potential complications, including:
- Bleeding: Minor bleeding is common, but major hemorrhage is a rare but serious complication.
- Pneumothorax (collapsed lung): This is a relatively common complication, especially with needle biopsies. It can range from mild to life-threatening.
- Infection: Infection at the biopsy site is a possibility, requiring antibiotic treatment.
- Pain: Post-procedural pain is expected, but it can be managed with analgesics.
- Injury to adjacent structures: Injury to blood vessels, nerves, or other organs is possible, though rare.
The risk of complications varies depending on the technique used. For example, VATS carries a higher risk of bleeding and infection than ultrasound-guided needle biopsy, but it also offers the best visualization and may lead to a more definitive diagnosis.
Q 25. Discuss the role of imaging (CT, Ultrasound) in guiding pleural procedures.
Imaging plays a crucial role in guiding pleural procedures and significantly improves safety and success rates. Both CT and ultrasound are essential:
- Ultrasound: Real-time imaging allows for precise visualization of the pleural effusion, the location of the lesion, and the proximity of vital structures. It’s particularly useful for guiding needle biopsies because it allows the physician to see the needle as it enters the pleural space.
- CT Scan: Provides excellent anatomical detail, showing the extent of the pleural effusion, the size and location of the lesion, and the relationship to adjacent structures. CT-guided biopsies are often used for complex cases or when the lesion is difficult to reach with ultrasound.
The choice between ultrasound and CT depends on the specific clinical scenario. In many cases, ultrasound is the preferred method due to its non-invasiveness, real-time visualization, and portability.
Q 26. How do you manage a patient with a persistent air leak after chest tube placement?
A persistent air leak after chest tube placement is a significant complication that requires careful management. The first step involves assessing the severity of the air leak and its cause. This might involve reviewing the chest tube placement, checking for any ongoing bleeding, and assessing the patient’s overall clinical status. Strategies to manage this include:
- Observation: For small, self-limiting leaks, close monitoring may suffice.
- Chest Tube Management: Ensuring proper placement and ensuring no kinks or obstructions in the tubing is crucial.
- Supplemental Oxygen: Increasing oxygen delivery can help to minimize the air leak.
- Surgical intervention: If conservative measures fail, surgical intervention (thoracoscopic or open repair) may be necessary to address underlying lung injury or bronchial disruption.
- Airtight Seal: Thorough assessment of the chest tube insertion site and use of appropriate seal techniques are crucial for preventing air leaks.
It’s crucial to remember that persistent air leaks can lead to tension pneumothorax, a life-threatening condition requiring immediate intervention.
Q 27. What are the key performance indicators (KPIs) you would track for pleural procedure success?
Key performance indicators (KPIs) for pleural procedure success include:
- Procedure success rate: The percentage of procedures successfully completed without major complications.
- Diagnostic yield: The percentage of biopsies that provide a definitive diagnosis.
- Complication rate: The incidence of pneumothorax, bleeding, infection, or other complications.
- Length of hospital stay: Shorter hospital stays indicate a more efficient and effective procedure.
- Patient satisfaction: Assessing patient experience and satisfaction with the procedure and post-procedure care.
- Mortality rate: The incidence of death related to the procedure.
Regular monitoring of these KPIs allows for continuous quality improvement and helps to identify areas where processes can be optimized.
Q 28. Describe your experience with managing post-procedural complications.
Throughout my career, I’ve managed a wide range of post-procedural complications following pleural procedures. This includes managing pneumothoraces (using chest tubes, supplemental oxygen, and occasionally surgical intervention), treating post-biopsy bleeding (with blood transfusions if needed and close monitoring), and addressing infections (with appropriate antibiotic therapy). One particular case that stands out involved a patient who developed a persistent air leak after a CT-guided biopsy. Despite several attempts at conservative management, the leak persisted. We ultimately resorted to VATS to identify and repair the underlying lung injury, successfully resolving the air leak and ensuring the patient’s recovery.
My approach to managing complications is always guided by a systematic assessment of the patient’s condition, prompt intervention when necessary, and close monitoring to ensure optimal outcomes. Early recognition and management are key to preventing serious complications.
Key Topics to Learn for Pleural Procedures Interview
- Anatomy and Physiology of the Pleura: Understanding pleural spaces, layers, and their normal function is fundamental. Consider the implications of variations from the norm.
- Diagnostic Procedures: Thorough knowledge of chest x-rays, CT scans, and ultrasound in identifying pleural effusions, pneumothorax, and other pleural pathologies is crucial. Be prepared to discuss interpretation and limitations of these modalities.
- Thoracentesis: Master the technique, indications, contraindications, and potential complications. Practice explaining the procedure to a patient and addressing their concerns.
- Pleurodesis: Understand the various methods, patient selection criteria, and the rationale behind this procedure. Be ready to compare and contrast different approaches.
- Chest Tube Insertion and Management: This is a cornerstone of pleural procedure management. Focus on indications, insertion techniques, troubleshooting complications (e.g., air leaks, kinks), and removal criteria.
- Pleural Biopsy: Be familiar with different biopsy techniques and their applications. Understand the indications and interpretation of results.
- Management of Pneumothorax: Discuss both conservative and interventional management strategies, including needle decompression and chest tube insertion.
- Understanding and Managing Complications: Interviewers will assess your understanding of potential complications like bleeding, infection, and lung injury. Be prepared to discuss preventative measures and management strategies.
- Evidence-Based Practice: Demonstrate familiarity with current guidelines and best practices in pleural procedures. Be ready to discuss relevant research and clinical trials.
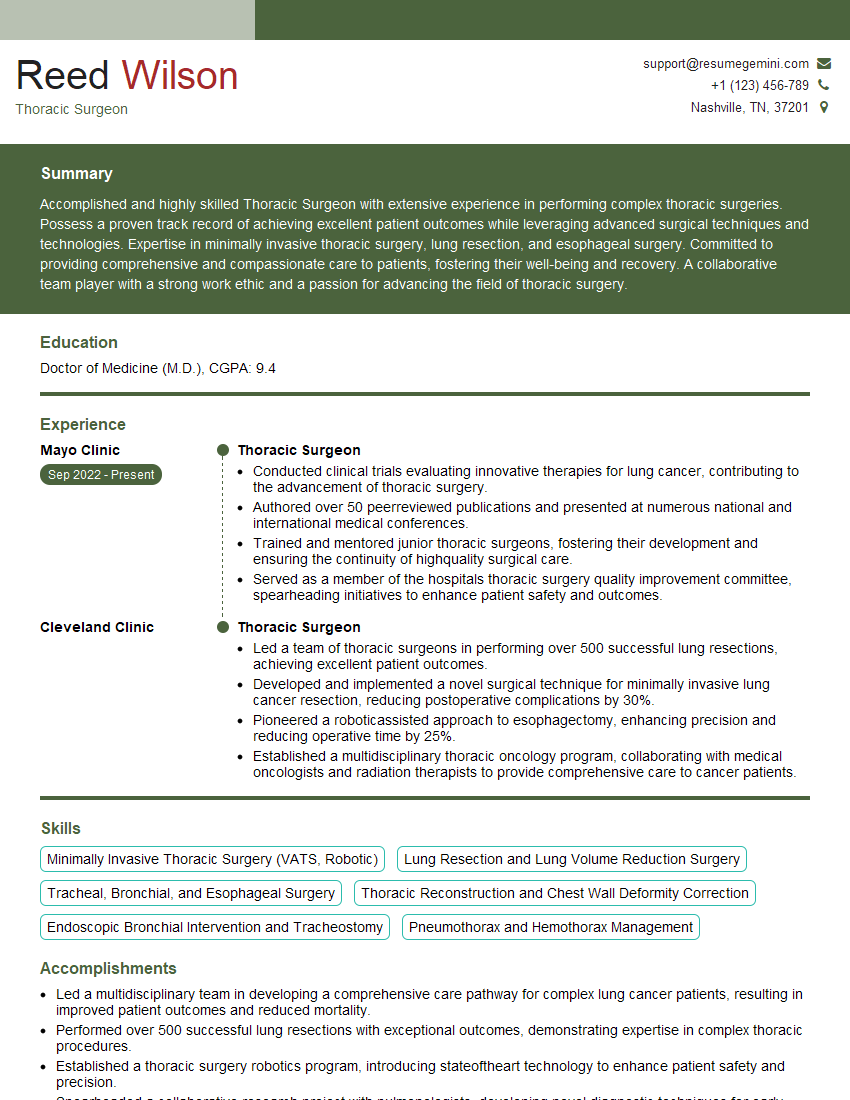
Next Steps
Mastering pleural procedures significantly enhances your career prospects in respiratory medicine and related specialities, opening doors to advanced roles and leadership opportunities. To maximize your chances of landing your dream job, it’s essential to create a compelling and ATS-friendly resume that showcases your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume tailored to the specific requirements of your target positions. We offer examples of resumes specifically tailored to highlight experience in Pleural Procedures, helping you present your qualifications in the best possible light. Invest in your future – build the resume that lands you the interview.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.